Abstract
Cisplatin (CP) as a potent chemotherapeutic agent is restricted due to its hepatotoxicity, nephrotoxicity, and multiple organ toxicity. The current study investigates the possible mechanisms responsible for the hepatorenal protective effects of ginger extract (GE) against cisplatin-induced hepatorenal toxicity in rats. Thirty-two male albino rats (240–250 g) were divided into four equal groups (n = 8) as follows: control group (single i.p. saline dose 7.5 ml/kg at the 15th day of the study), CP-treated group (7.5 mg/kg single i.p. injection of CP at the 15th day of the study), GE-treated group (500 mg/kg/ p.o daily for 20 days), and GE + CP-treated group (GE 500 mg/kg/day, p.o daily for 15 days prior to CP injection and 5 days after CP injection). At day 21st of the experiment, blood samples were collected, and serum was isolated for biochemical assessments. Then, rats were euthanized, and hepatic and renal tissues were collected for tissue biochemical parameters, histopathology, and immunohistochemistry evaluations. Cisplatin-injected rats showed marked alterations in the serum liver and kidney functions, oxidant/antioxidant biomarkers, pro-inflammatory cytokines; tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and interleukin-6 (IL-6) and anti-inflammatory cytokine; interleukin-10 (IL-10). CP also induced overexpression of oxidative (INOS) and apoptotic (caspase-3) immunohistochemical markers in hepatic and renal tissues. Conversely, the combining administration of ginger extract before, with, and after CP treatment ameliorated the aforementioned biochemical, pathological, and immunohistochemical adverse effects induced by CP. In conclusion, ginger extract has protective effects against CP adverse effects, possibly via its antioxidant, anti-inflammatory, and anti-apoptotic properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cisplatin (CP) is one of the most effective front-line chemotherapies in the treatment of several solid tumors as well as some hematological malignancies (Ishikawa 2009). Clinical use of CP is limited due to its toxic side effects and severe cytotoxicity to normal tissue of liver, kidney, ear, and brain (Abdel-Daim et al. 2019; Abuzinadah and Ahmad 2020; El-Sheikh 2020), resulting in a reduction in dose or discontinuation of treatment (Yao et al. 2007). CP exerts its action through inhibition of DNA transcription and replication, apoptosis, and necrosis of the cancer cells which underlies the antitumor effect of the drug (Ishikawa 2009). During the intensive treatment protocols, higher doses of CP may be required for effective tumor suppression, inducing toxicity that is also encountered during low-dose repeated CP therapy (Dkhil et al. 2013).
The exact mechanism of CP-induced toxicities is not fully understood (Hong et al. 2005), but oxidative stress has been linked with CP toxicity in many experimental models (Beagloo et al. 2019). CP can cause production of reactive oxygen species (ROS) [hydrogen peroxide (H2O2), superoxide anions (O2−), and hydroxyl radicals (OH−)]. The OH− is capable of abstracting a hydrogen atom from cell membrane lipids causing lipid peroxidation (Antunes et al. 2000).
Two theories for CP inducing ROS have been proposed. The first mechanism CP enters into cells by organic cation transporter 2 which then undergoes hydrolysis to generate positively charged electrophile. This electrophile accumulates in negatively charged mitochondria and reduces the activity of mitochondrial respiratory complexes, resulting in ROS generation. The second one is CP inside the body converted into a highly reactive form, which causes depletion of glutathione (GSH), and inactivation of antioxidant enzymes leads the accumulation of ROS in the cells (Malik et al. 2015). Also, CP has been reported to decrease antioxidant enzyme activities such as SOD, GPx, and CAT and to cause an increase in the level of lipid peroxidation end-product, MDA (Abdel-Daim et al. 2019). Free radicals can massively damage tissue through reacting with various cellular components such as membrane lipids, proteins, and cell DNA, thus impairing the cellular structure (Ma et al. 2017).
Moreover, other various mechanisms, including inflammation, hypoxia, vascular injury, and activation of apoptotic pathways with an increase in the pro-apoptotic proteins and a decrease in the anti-apoptotic proteins, are thought to be involved in cisplatin toxicity (Kandemir et al. 2019).
Many preclinical trials have been performed to evaluate the protective effects of some antioxidants on antagonizing the side effects related with cisplatin. In this regard, natural antioxidants mainly found in medical plants, fruit, and vegetables are very popular among the consumers, which seem to prevent some diseases (Wojcik et al. 2010).
The rhizome of Zingiber officinale, commonly called as ginger, is consumed in many parts of the world as a flavoring agent and spice plant (Grant and Lutz 2000). Also, ginger has many medical uses such as anti-cancer (Pan et al. 2008), anticlotting, free radical removal, anti-inflammatory, and analgesic (Yiming et al. 2012). Ginger extract is rich with plenty of active substances as zingerone, paradols, shagaols, and gingerols. These components exhibit anti-inflammatory, anti-oxidant, and anti-carcinogenic proprieties both in vivo and in vitro (Surh 2002; Kandemir et al. 2019). Zingerone is reported to have therapeutic effects such as antiapoptotic, antioxidant, anti-vomiting, anti-inflammatory, and anti-nausea agent after chemotherapy (Ahmad et al. 2015). Gingerols has the anti-oxidative, anti-serotonergic, the inhibition of prostaglandin production, and anti-inflammatory effects (Aimbire et al. 2007).
Several studies tested the protective effect of various substances to counteract the cisplatin-induced toxicity. Therefore, we aimed to investigate the protective effects of ginger extract against cisplatin-induced hepatorenal injuries in rats. Moreover, to investigate the potential anti-oxidative, anti-inflammatory, and anti-apoptotic properties of ginger against CP via investigating serum biochemical and tissue oxidative/antioxidant parameters, in addition to assessment of pro-inflammatory and anti-inflammatory cytokines, histopathological alterations and immunohistochemical expressions of INOS and caspase-3 in hepatic and renal tissues.
Materials and methods
Chemicals
Cisplatin (Cisplatin®) vial was purchased as a clinical formulation from a local pharmacy manufactured by Merck Co. (Lyon, France); each vial contains 50 mg/50 ml saline. Diagnostic kits for assaying serum liver and kidney function biomarkers (alanine transaminase, aspartate transaminase, alkaline phosphatase, total protein, urea and creatinine), oxidative stress parameters (malondialdehyde and nitric oxide), and antioxidant enzymatic parameters (super oxide dismutase and total antioxidant capacity) were purchased from Biodiagnostic Company (Dokki, Giza, Egypt). The pro-inflammatory cytokines (tumor necrosis factor-α, interleukin-1β, and interleukin-6) and the anti-inflammatory cytokine (interleukin-10) rat enzyme-linked immune sorbent assay (ELISA) kits which are Sandwich-based were purchased from (RayBiotech Company; Georgia, USA).
Preparation of aqueous extract of ginger
Ginger fresh roots were purchased from the local market of Sadat city, Egypt. Aqueous ginger extract was prepared from ginger roots as described by Al-Amin et al. (2006). Briefly, the ginger roots were peeled on crushed ice, and 50 g ginger was cut into small pieces and homogenized (2000 rpm for 10 min) in 75-ml cold, sterile 0.9% NaCl in the presence of some crushed ice. The homogenization was carried out in a blender at high speed using 2-min bursts for a total of 12 min. The homogenized mixture was filtered three times through cheesecloth. The clear supernatant fraction was separated and the volume made up to 100 ml with cold normal saline. The concentration of this ginger extract was measured and adjusted to 500 mg/ml. The prepared aqueous extract of ginger root was stored in small samples at −20 °C until use.
Animals
Male Wistar adult albino rats of (240–250 g) were obtained from the animal house of the National Central Institute, Dokki, Cairo, Egypt. They were clinically healthy and were acclimatized to the standard laboratory conditions for 2 weeks before start of the experiment. During this period, the rats were housed in plastic cages with galvanized iron filter tops in quiet place with natural ventilation and natural daily 12:12 h light–dark cycle. Rats were provided with standard commercial diet and clean tap water ad libitum throughout the experimental period.
Experimental design and animal grouping
After acclimatization for 2 weeks, the rats were randomly divided into four groups, with eight rats in each group, as shown:
-
Group I: (C) control received single intraperitoneal (i.p.) injection of normal saline (7.5 ml/kg i.p. injection)
-
Group II: (CP) received single dose of CP dissolved in normal saline (7.5 mg/kg i.p. injection) according to El-Sheikh (2020) at day 15 of the study
-
Group III: (GE) received ginger extract dissolved in distilled water (500 mg/kg/day, orally by gavage) according to Al-Shathly et al. (2020) for 20 days
-
Group IV: (GE + CP) received ginger extract as group III and CP as group II
-
At the day of CP injection (at day 15th), rats were given a single i.p. dose of CP 1 h after ginger extract administration
Collection of blood and tissue samples
By the end of the experiment, all rats were overnight fasted, and blood samples collection was done 24 h after the last GE dose administration. Rats were anesthetized under inhalation anesthesia of isoflurane. Blood samples were collected from the medial canthus of the eye of each rat and were left to coagulate at room temperature for 20 min then in the refrigerator for clot retraction then centrifuged at 3000 rpm for 15 min. The clean supernatant non-hemolyzed serum was harvested and kept frozen at −20 °C until used. Immediately after blood collection, rats were sacrificed by cervical dislocation, and tissue specimens from liver and kidney were collected. Hepatic and renal tissue samples were collected, washed several times with normal saline, and then kept at −80 °C until tissue biochemical analysis performed. Another part of tissue samples was fixed in 10% neutral buffered formalin solution for histopathological and immunohistochemical examinations.
Serum biochemical analysis
Serum liver function biomarkers (ALT, AST, ALP, and total protein levels)
Commercial kits (Biodiagnostic Company, Dokki, Giza, Egypt) were used to determine hepatic serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) and alkaline phosphatase (ALP). Serum total protein was measured according to Lowry et al. (1951), and the results were expressed as g/dl.
Serum kidney function biomarkers (urea and creatinine levels)
The serum urea and creatinine levels were measured using available commercial kits (Biodiagnostic Company, Dokki, Giza, Egypt). The results were expressed as mg/dL.
Determination of pro/anti-inflammatory markers
Serum concentrations of pro-inflammatory cytokines (tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), interleukin-6 (IL-6)) and anti-inflammatory cytokine marker (interleukin-10 (IL-10)) were measured using quantitative sandwich ELISA commercial kits according to the manufacturer’s instructions.
Biochemical tissue analysis
Preparation of tissue homogenate
The liver and kidney tissues were weighed and prepared for analysis by adding ice-cold phosphate-buffered saline (0.01 M, pH = 7.4) and volume added based on the sample weight (1/10 (w/v) ratio). Then, place on ice, homogenized to disrupt the cell wall, and release the cell contents using an ultrasonic sonicator (Qsonica, Newtown, CT, USA), and then centrifuged at speed of 4000 rpm for 20 min in a cooling centrifuge to obtain supernatant. The supernatant was collected in new Eppendorf tubes and stored at −80 °C until use for biochemical analysis of oxidant/antioxidant biomarkers.
Determination of oxidant/antioxidant biomarkers in tissue homogenate
Oxidative stress biomarkers and antioxidant enzyme activities were measured by colorimetric techniques using commercially available kits (Bio-diagnostic, Dokki, Giza, Egypt) by following kit instructions. The level of malondialdehyde (MDA), nitric oxide (NO), reduced GSH content, SOD activity, and total antioxidant capacity (TAC) was measured.
Histopathological examination
The formalin-fixed specimens of liver and kidney were trimmed, washed, and dehydrated in ascending grades of ethyl alcohol, cleared in methyl benzoate and embedded in paraffin after having completed the routine follow-up steps and processed for paraffin Sects. (4 μm thick) using a microtome (LEICA RM 2135) then routinely stained with hematoxylin and eosin stain (H&E) according to Bancroft and Layton (2013). Histopathological examination and photographing were done using a digital Leica photomicroscope (LEICA DMLB Germany).
Semi-quantitative analysis of H&E staining sections
A semi‑quantitative evaluation of hepatic and renal tissues parameters of the following: vascular (congestion, hemorrhage, edema), degenerative (necrosis, apoptosis), and inflammatory changes were accomplished by scoring the degree of severity of histopathological characteristics according to the 5-point semi-quantitative scale adopted by Allen (1992) as follows: (0): normal appearance and absence of pathological lesions 0%, grade (I): mild changes (< 25% tissue damage), grade (II): moderate changes (25–50% tissue damage), grade (III): severe changes (51–75% tissue damage), and grade (IV): very severe changes (> 75% tissue damage). All evaluations were made on 5 tissue sections per group and 5 fields per tissue section (n = 25) as previously described by Hsu et al. (2006). A frequency and severity grade as described by Nežić et al. (2019) shown as hepatic damage score (HDS) and renal damage score (RDS) of lesions were determined for all fields (n = 25) of each organ, and a mean hepatic and renal HDS and RDS were determined, respectively. The exact method of calculation is shown in Tables 5 and 6, respectively.
Immunohistochemical investigation
The immune-staining method for localization of inducible nitric oxide synthase (iNOS) and caspase-3 was performed following the method described by Yang et al. (2020). Immunohistochemical staining of the samples was performed on 4-μm thick formalin-fixed paraffin-embedded sections. Following deparaffinization in xylene and rehydration in degrading series of ethanol, the sections were washed with phosphate-buffered saline (PBS, 0.1 M, pH 7.4). Antigen retrieval of the tissues was performed by microwave treatment in 0.1 M sodium citrate solution, pH 6.0 at 600 W for 10 min. The sections were then treated with 0.3% hydrogen peroxide for 30 min to block endogenous peroxidase activity. The sections were incubated with primary anti-rat polyclonal antibodies against iNOS (diluted 1:100, Santa Cruz Biotechnology, Santa Cruz, CA, USA) and caspase-3 (diluted 1:200, Abcam, Cambridge, MA, USA) for 1 h at room temperature. Following the primary antibody incubation, the sections were washed with phosphate-buffered saline, then incubated with the appropriate biotinylated secondary antibodies according to the Vecta stain Elite ABC Kit (Vector Laboratories, Burlingame, CA, USA) for 30 min at room temperature. Visualization of immune reaction was performed using 3, 3′-diaminobenzidine (DAB, Sigma Chemical Co, St. Louis, Missouri, USA) until dark brown color development detected by light microscopy and then washed by distilled water and counterstained with Mayer’s hematoxylin (Sigma-Aldrich, St. Louis, MO, USA) dehydrated in ascending grades of alcohol, cleared in xylene, and mounted with using the Aquatex fluid (Merk KGaA, Darmstadt, Germany) under a cover slip. A cell with a brown cytoplasm or a brown nucleus was considered immune positive.
Semi-quantitative analysis of immunohistochemical staining sections
Twenty-five different randomly selected fields were selected to estimate the immune index of INOS and caspase-3 staining sections under high power magnification (× 40). Semi‑quantitative analysis of INOS and caspase-3 were evaluated using a semi-quantitative scoring method described by Zhang (2017) with little modification. The average values of 25 fields were calculated to obtain the hepatic and renal tubular immune index and given a score from 0 to IV as follows: none (0): no hepatic or renal tubular cells immunostaining, mild (I): hepatic or renal tubular cells had brown signals affecting < 25% of the examined sections, moderate (II); hepatic or renal tubular cells had brown signals affecting 25–50% of the examined sections, severe (III): hepatic or renal tubular cells had brown signals affecting 50–75% of the examined sections and very severe (IV): hepatic or renal tubular cells had brown signals affecting > 75% of the examined sections.
Statistical analysis
Results were expressed as mean ± standard error. Statistical analysis of data was carried out using analysis of variance by one-way ANOVA test followed by Duncan’s multiple comparison tests. All data were statistically analyzed using statistical software program SPSS (Statistical package for Social Sciences) Version 16 released on 2007. Statistical significance was considered at probability (P ≤ 0.05) according to Sendecor and Cochran (1987).
Results
-
1.
Clinical signs
All rats in control and ginger extract treated group were bright, active, alert, and did not exhibit any disease manifestations during the whole experimental period. The cisplatin-treated group showed signs of toxicity like decreased food intake, dullness, depression, lethargy, rough hair coat, dehydration, and diarrhea accompanied by death of one rat (mortality rate 12.5%) at the 19th day of the experiment. The ginger- and CP-treated group had less severe clinical manifestations compared with the CP-treated group alone. Moreover, no mortality was recorded in this group.
-
2.
Serum liver and kidney functions biomarkers
The results are summarized in Table 1. Compared with C group, the CP-treated rats had significant (p ≤ 0.05) increase of liver enzymes (ALT, AST, and ALP) and decrease in serum total protein. Administration of GE for 15 days before CP treatment and 5 days after CP treatment ameliorated CP-induced elevations of liver enzymes and serum total protein. Administration of GE alone had no significant effects on the mentioned parameters, and the results were similar to the control. Regarding the kidney function biomarkers, CP-treated rats had significant (p ≤ 0.05) increase in serum urea and creatinine compared to C group. Administration of GE for 15 days before CP treatment and 5 days after CP injection ameliorated CP-induced urea and creatinine elevations (p ≤ 0.05). Administration of GE alone protected the kidney and kept serum urea and creatinine levels within normal value of control rats.
-
3.
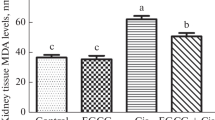
Hepatic and renal oxidant/antioxidant biomarkers
The results are summarized in Table 2. Compared to the C group, CP-treated rats had significant (p ≤ 0.05) elevation of lipid peroxidation biomarkers (MDA and NO) levels along with significant (p ≤ 0.05) reduction of the concentration of the antioxidant biomarker (GSH, SOD, and TAC) concentrations in hepatic and renal tissue. Conversely, administration of GE for 15 days before CP treatment and 5 days after CP treatment showed marked improvement of these parameters represented by significant reduction in MDA and NO levels with an increase of GSH, SOD, and TAC content when compared with the CP-treated group. On the other hand, rats treated with GE alone had no significant change of the oxidant parameters and total anti-oxidant capacity, but there was significant increase in reduced glutathione and superoxide dismutase compared with C group.
-
4.
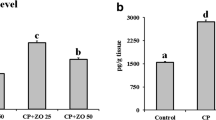
Serum pro-inflammatory cytokines (tumor necrosis factor-α, interleukin-6, and interleukin-1β) and anti-inflammatory cytokine (interleukin-10)
The results are summarized in Table 3. Compared to the C group, the CP-treated group had significant increase (P ≤ 0.05) of pro-inflammatory cytokines (TNF-α, IL-6, and IL-1β). Conversely, administration of GE for 15 days before CP treatment and 5 days after CP treatment showed marked improvement represented by significant reduction in these biomarkers compared to CP group. The ginger extract–treated group alone did not show any significant change in these parameters compared to the C group. Correspondingly, the anti-inflammatory cytokine Il-10 was dramatically diminished in the CP-treated group as compared to the C and GE groups. Conversely, administration of GE for 15 days before CP treatment and 5 days after CP treatment showed significant increase (P ≤ 0.05) in IL-10 biomarker level compared to the CP-treated group alone.
-
5.
Histopathological results
Summary of histopathology examination of hepatic tissues is showed in Table 4. Liver sections from C- and GE-treated rats revealed normal histological architecture of liver tissues including hepatocytes, central vein, and hepatic sinusoids (Fig. 1 (A, C)). Conversely, liver from CP-treated rats had marked injury characterized by marked vascular changes including congestion of central vein and hepatic sinusoids, associated with degenerative changes characterized by multifocal to coalescing hepatic necrosis, inflammatory cell infiltration, and apoptotic hepatocytes (Fig. 1 (B1, B2, and B3)). In contrast, administration of GE to CP treated rats attenuated their hepatic injury as indicated by nearly normal hepatic tissue except for congestion of central vein and small focal areas of necrosis infiltrated by inflammatory cells (Fig. 1 (D)).
The summary of histopathology examination of renal tissues is presented in Table 5. Kidney sections from C and GE rats revealed normal architecture of kidney tissues in Fig. 2 (A, C). Cisplatin-treated rats showed marked renal injury characterized by marked vascular changes including congestion, perivascular and interstitial edema, and degenerative changes proved by necrosis of glomerular tuft and renal tubular cells, inflammatory cell infiltrations, and formation of hyaline casts and epithelial casts (Fig. 2 (B1, B2, and B3)). Administration of GE- to CP-treated rats attenuated renal damage induced by CP as indicated by less vascular, degenerative, and inflammatory alterations (Fig. 2 (D)).
-
6.
Immunohistochemical expression of INOS and caspase-3
Semi-quantitative scoring of INOS and caspase-3 in hepatic and renal sections is presented in Table 6. Hepatic tissues from C and GE groups had negative immune-staining for INOS and caspase-3 as shown in Figs. 3A, C and 4A, C, respectively. CP-treated group had strong positive immune-staining of INOS and caspase-3 as shown in Figs. 3B and 4B, respectively. Treatment with GE before and after CP induced marked downregulation of INOS and xaspase-3 expressions (Figs. 3D and 4D), respectively.
Renal tissues from C and GE groups had negative immune-staining of INOS and caspase-3 as shown in Figs. 5A, C and 6A, C, respectively. The CP-treated group had strong positive immune-staining of INOS and caspase-3 as shown in Figs. 5B and 6B, respectively. Treatment with GE before and after CP-induced downregulation of INOS and caspase-3 expressions is shown in Figs. 5D and 6D, respectively.
Representative photomicrographs of histopathological alterations in liver sections of different groups (H&E stain X20 except B2, B3 X40; scale bar = 50 μm; star: congestion, black arrows: coagulative necrosis of hepatocytes with nuclear pyknosis and more eosinophilic cytoplasm, blue arrows: different stages of apoptosis (cell shrinkage, fragments, collapse and formation of apoptotic body) in hepatic cells, yellow arrow: margination of inflammatory cells in central vein, green arrows: inflammatory cell infiltrations in hepatic parenchyma, CV: central vein. (A) Control group. (B) CP group. (C) GE group and (D) GE + CP group
Representative photomicrographs of histopathological alterations in kidney sections of different groups (H&E stain X20; scale bar = 50 μm; head arrow: congestion, star: edema, black arrows: renal casts, yellow arrows: necrotic cells with pyknotic nuclei, green arrows: inflammatory cell infiltrations in the interstitial tissue, infiltration, G glomeruli, P proximal convoluted tubules, D distal convoluted tubules. (A) Control group. (B) CP group. (C) GE group and (D) GE + CP group
Representative photomicrographs of immunohistochemical localization of inducible nitric oxide synthase (INOS) in liver sections of different groups (INOS IHC; scale bar = 50 μm), yellow arrows: cytoplasmic immune expression in hepatic sinusoids, black arrows: immune expression in hepatic cells. A Control group. B CP group. C GE group and D GE + CP group
Representative photomicrographs of immunohistochemical localization of inducible nitric oxide synthase (INOS) in kidney sections of different groups (INOS IHC; scale bar = 50 μm), black arrows: cytoplasmic immune expression in renal tubular cells. A Control group. B CP group. C GE group and D GE + CP group
Representative photomicrographs of immunohistochemical localization of caspase-3 in kidney sections of different groups (caspase-3 IHC; scale bar = 50 μm), yellow arrows: nuclear immune expression in renal tubular cells. A Control group. B CP group showing widespread brown immunoreactivity for caspase-3 of most renal tubular cells. C GE group and D GE + CP group
Discussion
Despite its clinical value, the application of cisplatin is limited by its severe side effects on normal tissues, especially hepatic and renal tissues. We have studied the possible protective effect of ginger extract against cisplatin hepatorenal toxicity in rats. The obtained results showed that ginger extract alone did not induce any adverse effects on all tested parameters but partially offered significant protection against CP-induced hepatic and renal dysfunction via modulation of oxidative stress, inflammation, and apoptosis. The apparent protective effects of GE against CP-induced toxicity were attributed to its scavenging properties or its anti-inflammatory and anti-apoptotic properties.
In the current study, the obtained data of rats treated with CP showed impairment of hepatic and renal functions. CP-induced hepatotoxicity was evidenced by significant elevation in the serum liver enzyme activities (ALT, AST, and ALP), accompanied with a significant reduction in the serum total protein level when compared with the control group. Elevated activities of blood transaminases especially ALT indicate liver dysfunction induced by cisplatin, where hepatocellular damage causes leakage of intracellular ALT into the blood stream due to loss of hepatocyte membrane integrity which correlates well with the damage degree and consequent leakage out membranes (Farid et al. 2021). This result may be attributed to the metabolism of CP in liver. Mohamed and Badawy (2019) reported that CP is significantly taken up by the liver and accumulated in the hepatocyte, causing its damage leading to an increase of the liver enzyme activities.
The marked reduction in the serum total protein indicates disturbance in protein metabolism induced by cisplatin due to a reduction in protein synthesis as plasma protein, especially albumin synthesis primarily occurs in the liver. Also, CP disturbs protein synthesis in hepatocytes as it binds to cellular proteins, resulting in alterations in a high number of hepatocyte enzymes. Moreover, reduction in the serum total protein indicates liver dysfunction following liver damage and alteration of functional integrity in the kidney leading to proteinuria, so, their plasma level decreases in hepatotoxic/nephrotoxic conditions (Sen et al. 2013). In line with these findings, a high degree of hepatic vascular, degenerative, and inflammatory histopathological alterations of the liver tissue was observed in CP-treated rats.
Also, cisplatin-induced renal damage was indicated by the recorded elevation of serum urea and creatinine levels which are confirmed by previous investigators (Sadeghi et al. 2020). In association with these findings, vascular, degenerative, and inflammatory histopathological alterations of a high degree were observed in renal tissue of CP-treated rats including congestion, and dilatation of interstitial blood vessels, degeneration and desquamation of the tubular epithelium, and presence of eosinophilic hyaline casts in most renal tubules as reported by Elkomy et al. (2020). Nephrotoxicity of cisplatin also has been reported by Kandemir et al. (2019) who indicate that CP-induced nephrotoxicity in female rats was associated with the oxidative stress, oxidative DNA damage, apoptosis, inflammation, and decreasing kidney AQP1 protein level and Sun et al. (2019) who concluded that pretreatment with scutellarin-ameliorated cisplatin-induced nephrotoxicity in mice via suppression of apoptosis and inflammation and activation of autophagy.
The increment in liver and kidney function biomarkers may be attributed to CP-induced oxidative stress that considers one of the major possible explanations of CP-induced hepatic and renal damage. Over-generation of ROS ultimately elevates lipid peroxidation and reduces the cellular antioxidant enzymatic activities as confirmed by pronounced elevation of the MDA and NO levels in the hepatic and renal homogenates with a significant reduction in GSH, SOD, and TAC activities in both tissues compared to the control group. This elevation of oxidative stress biomarkers (MDA and NO) could explain the cause of cellular damage in both hepatocytes and renal tubular epithelial cells in cisplatin-treated rats. In accordance with our findings, previous studies have shown that oxidative stress is implicated as a major mechanism of CP-induced hepatorenal toxicity either by enhancement of free radical generation and lipid peroxidation or depletion of antioxidant enzyme system (Abdel-Daim et al. 2020; Abuzinadah and Ahmad 2020; Elkomy et al. 2020). In association with these results, there were vascular, degenerative, and inflammatory histopathological alterations observed in hepatic and renal tissue of CP-treated rats.
Inducible nitric oxide synthase (INOS) is a major downstream mediator of inflammation in various cell types and also is an enzyme used to produce NO (Caglayan et al. 2018). Excess NO reacts with superoxide anion to generate peroxynitrite radical that causes organ injury and protein nitration. Also, excess NO decreases intracellular GSH thus increasing the susceptibility to ROS (Kandemir et al. 2017).
The immunohistochemical results showed increased number of immune-stained cells by inducible nitric oxide synthase (INOS) and caspase-3 in both hepatic and renal tissues; this suggests that the oxidative stress from the released free radicals is considered as one of the possible mechanisms in pathology of cisplatin-induced hepatorenal toxicity. These results are compatible with previous investigators (Beagloo et al. 2019; Elkomy et al. 2020) who also reported an increase in lipid peroxidation and decrease in the activities of antioxidant enzymes upon similar cisplatin treatment (7.5 mg/kg BW single ip injection) in rat liver and kidney.
Inflammation, an oxidative stress complication, is characterized by excessive production of cytokines (Ingawale et al. 2014). Cytokines are glycoproteins produced by a variety of cells and are secreted into the extracellular space to participate in the immune response and inflammatory regulation. Previous studies have demonstrated that inflammatory markers such as TNF-α and IL-1β were released by tissue macrophages and monocytes in response to any noxious events (Singh and Agarwal 2002). Moreover, stimulated leukocytes were documented to produce free radicals, which in turn trigger the intensity of inflammation and lipid peroxidation (Lazarenko et al. 2014).
TNF-α is a multifunctional cytokine most often referred to as a potent pro-inflammatory cytokine and is recognized as a major effector of macrophage-mediated host defense and tissue injury, also playing a crucial role in innate and adaptive immunity, cell proliferation, and apoptotic processes (Pober and Min 2006). In pathological processes, tissue-fixed macrophages, such as Langerhan’s cells, Kupffer cells, and astroglia, are believed to be major sources of TNF-α. However, other cell types, including endothelial cells, epithelial cells, monocytes, T-cells, smooth muscle cells, adipocytes, and fibroblasts, secrete significant amounts of TNF-α when exposed to the appropriate stimuli (Luster et al. 1999) and used to reflect injury severity (Knoblach et al. 1999). TNF-α as an inflammatory biomarker has been suggested to be involved in the generation of ROS and free radicals that cause cisplatin toxicity and initiate inflammation (Ramesh and Reeves 2002). Also, TNF-α can activate caspases and therefore trigger apoptosis through a multitude of molecular mechanisms (Babu et al. 2015).
Interleukin-1β (IL-1β) is thought to be the most important cytokine, with a strong pro-inflammatory activity by stimulating the production of multiple pro-inflammatory mediators such as cytokines, chemokines, prostaglandins, and the activation of cyclooxygenase-2 and matrix metalloproteinases (Dinarello 2009). In addition, IL-1β promotes oxidative stress and accelerates the degradation of extracellular matrix by inducing cell senescence apoptosis, thereby accelerating degeneration (Yang et al. 2015). Furthermore, IL-1β has also been shown to play a role in adhesion of leukocytes to endothelial cells (Bevilacqua et al. 1985) and edema formation (Holmin and Mathiesen 2000). Concerning interleukin-6 (IL-6), a multifunctional cytokine involved in cell proliferation and differentiation, maintaining immune homeostasis, macrophage function, and other key functions (Kishimoto et al. 1995; Romano et al. 1997) can be used as a pro‑inflammatory cytokine, which may cause secondary injury (Gruol et al. 2011). Conversely, IL-10 is anti-inflammatory cytokine produced by monocytes and lymphocytes and is known to have a major role in the anti‑inflammatory response having a potent inhibitory effect on the production of pro-inflammatory mediators (Knoblach and Faden 1998).
Several cytokines, such as TNF-α and IL-6, were elevated during the inflammatory cascade induced by cisplatin (El-Sheikh 2020). Furthermore, TNF-α and IL-10 play a crucial role in mediating the interplay between inflammatory, oxidative stress, and apoptotic pathways (Tadagavadi and Reeves 2010; Shaw et al. 2011). Similarly, a potent inflammatory response accompanied with lipid peroxidation after cisplatin treatment was shown in CP-treated rats in this study, and this situation aggravates hepatic and renal tissue damage. This was noted by marked increase of pro-inflammatory cytokine profile (TNF-α, IL-6, and IL-1β) and significance decrease of interleukin-10 (IL-10). It is also indicated by mononuclear cellular infiltrations in liver and kidney sections stained by H&E stain. The observed mononuclear cellular infiltration after cisplatin injection was in consistence with other investigators (Faubel et al. 2007; Ozkok and Edelstein 2014) who reported that cisplatin evoked an inflammatory response with cell infiltration of renal tissue mainly mast cells, T cells, macrophages, and neutrophils.
In addition to inflammation, cisplatin-induced apoptosis has been reported as a major mechanism contributing to cisplatin toxicity (Kandemir et al. 2019; Sun et al. 2019). Cell death can result from naturally occurring apoptosis (physiological apoptosis) or from irreparable cell injury (pathological apoptosis) as described by Farber (1994). Cisplatin is thought to kill cells primarily by forming DNA adducts, causing G2 arrest in the cell cycle, triggering apoptosis (Kishimoto et al. 2000). CP binds DNA through the interaction of platinum atom and N7 position of purine bases leading to formation of inter strand crosslinks and intra strand crosslinks causing DNA double-helix disruption and blockage of DNA transcription and replication (Zhu et al. 2015). CP reacts not only with DNA but also with cytoplasmic proteins that induced apoptosis (Perez 1998).
CP administration shifts the balance between anti/and pro-apoptotic proteins toward pro-apoptotic pathway. It causes decreases Bcl-2, an antiapoptotic protein, and activation of Bax, a pro-apoptotic protein. It also induces translocation of Bax from cytosol to mitochondria releasing cytochrome c to cytosol. Cytochrome c also activates caspase-3, -8, and -9 and induces apoptosis in renal tubular cells (Malik et al. 2015). Among caspase enzymes, caspase-3 activates other caspase enzymes and initiates the apoptosis (Eldutar et al. 2017). Caspase-3 is the most important member of caspase family, which is responsible for many biochemical manifestations of apoptosis that lead to cleavage of nuclear and cytosolic substrates, chromatin condensation, fragmentation of DNA, and apoptotic body (Karadeniz et al. 2011). Moreover, activation of caspase-3, an apoptotic marker, indicates irreversible cell death (Yu et al. 2014) and thought to be one of the main cellular mechanisms for induction of apoptosis in renal tubular cells in CP-induced nephrotoxicity (Malik et al. 2015).
It is well known that oxidative stress and generation of large amount of ROS is often responsible for the mitochondria-mediated signaling pathway of apoptosis (Yiran et al. 2013) that promotes the activation of caspase-3 leading to apoptotic cell death (Rana 2008). The observed different stages of apoptosis in liver hepatocytes in tissues stained by hematoxylin and eosin was confirmed by the observed widespread positive caspase-3 immunoreactivity of most hepatocytes and renal tubular cells of cisplatin-treated rats pointing to abundant apoptotic cells. These results were in agreement with another study that reported involvement of cisplatin‑induced tubular epithelial cells is in caspase‑3 activation (El-Kordy 2019).
On the other hand, regarding the cytoprotective effects of GE (500 mg/kg b.wt.) 15 days before and 5 days after cisplatin treatment, we observed that GE could significantly provide protection against cisplatin-induced hepatorenal toxicity as there was marked improvement of liver and kidney functions throughout reduction of ALT, AST, AlP, urea, and creatinine compared to the cisplatin group. Also, there was marked improvement in all parameters of oxidative stress. GE was effective in suppressing MDA and NO production back to normal level, which may offer protection against hepatic and renal damages by cisplatin. This protective effect of GE may be related to the anti-oxidant properties of GE. These results are in agreement with Ajith et al. (2007) who focused on the protective effects of the alcoholic extract of ginger root against cisplatin-induced nephrotoxicity and suggested that this extract plays a protective role against cisplatin by reducing the oxidative stresses. Additionally, it decreases the amount of malondialdehyde and increases the amount of reduced glutathione and the activity of antioxidant defense system enzymes like superoxide dismutase, catalase, and glutathione peroxidase. Concerning the pro-inflammatory and anti- inflammatory cytokines, GE-treated rats showed marked reduction in all markers of pro-inflammatory cytokines and enhancement of interleukin-10 level indicating the potent anti-inflammatory effects of GE by affecting the balance between pro-inflammatory and anti-inflammatory cytokines. The anti-inflammatory property of GE has been demonstrated by Lantz et al. (2007). These biochemical obtained data are in harmony and came hand by hand with histopathological and immune-histochemical observations. The beneficial effects of ginger can result from the antioxidant effects of ingredients in ginger extract (Franciscoa et al. 2009). With regard to the beneficial therapeutic effects of ingredients in ginger, especially the antioxidant effects, this herb seems to protect the liver (Beagloo et al. 2019) and kidney (Ali et al. 2015) against the oxidative toxic effects of cisplatin.
Conclusion
The present study suggests that ginger extract is a potential hepatorenal protective agent against cisplatin-induced hepatotoxicity and nephrotoxicity when administered before, during, and after use of cisplatin. This protection is mediated either by decreasing of pro-oxidants (MDA and NO) and enhancement of the endogenous antioxidant molecules in hepatic and renal tissues (GSH, SOD, and TAC) or by their direct free radical scavenging activity, antioxidant, and anti-inflammatory activities. The protective effect of GE also involved the suppression of the pro-inflammatory cytokines (TNF-α, IL-1β and IL-6), elevation of anti- inflammatory cytokine IL-10 level, and downregulation of the expressions of INOS and caspase-3 in liver and kidney. These results substantiate the use of ginger extract against CP-induced hepatorenal toxicity in rats.
References
Abdel-Daim MM, Aleya L, El-Bialy BE, Abushouk AI, Alkahtani S, Alarifi S, Alkahtane AA, AlBasher G, Ali D, Almeer RS, Al-Sultan NK, Alghamdi J, Alahmari A, Bungau SG (2019) The ameliorative effects of ceftriaxone and vitamin E against cisplatin-induced nephrotoxicity. Environ Sci Pollut Res Int 26(15):15248–15254. https://doi.org/10.1007/s11356-019-04801-2
Abdel-Daim MM, Abdel-Rahman HG, Dessouki AA, El-Far AH, Khodeer DM, Bin-Jumah M, Alhader MS, Alkahtani S, Aleya L (2020) Impact of garlic (Allium sativum) oil on cisplatin-induced hepatorenal biochemical and histopathological alterations in rats. Sci Total Environ 710:136338. https://doi.org/10.1016/j.scitotenv.2019.136338
Abuzinadah MF, Ahmad A (2020) Pharmacological studies on the efficacy of a thymoquinone-containing novel polyherbal formulation against cisplatin induced hepatorenal toxicity in rats. J Food Biochem 44(2):e13131. https://doi.org/10.1111/jfbc.13131
Ahmad B, Rehman MU, Amin I, Arif A, Rasool S, Bhat SA, Afzal I, Hussain I, Bilal S (2015) A review on pharmacological properties of zingerone (4-(4-hydroxy-3-methoxyphenyl)-2-butanone). Sci World J 2015:816364. https://doi.org/10.1155/2015/816364
Aimbire F, Penna SC, Rodrigues M, Rodrigues KC, Lopes-Martins RA, Sertié JAA (2007) Effect of hydroalcoholic extract of Zingiber officinalis rhizomes on LPS-induced rat airway hyperreactivity and lung inflammation. Prostaglandins Leukot Essent Fatty Acids 77(3–4):129–138. https://doi.org/10.1016/j.plefa.2007.08.008
Al-Amin ZM, Thomson M, Al-Qattan KK, Peltonen-Shalaby R, Ali M (2006) Anti-diabetic and hypolipidaemic properties of ginger (Zingiber officinale) in streptozotocin-induced diabetic rats. Brit J Nutr 96(4):660–666. https://doi.org/10.1079/bjn20061849
Ali DA, Abdeen AM, Ismail MF, Mostafa MA (2015) Histological, ultrastructural and immunohistochemical studies on the protective effect of ginger extract against cisplatin-induced nephrotoxicity in male rats. Toxicol Ind Health 31(10):869–880. https://doi.org/10.1177/0748233713483198
Allen CT (1992) Hematoxylin and eosin. In: Prophet EB, Mills B, Arrington JB, Sobin LH (ed) Laboratory methods in histochemistry. Washington, DC: Armed Forced Institute of Pathology, American Registry of Pathology, p. 53
Al-Shathly MR, Ali SS, Ayuob NN (2020) Zingiber officinale preserves testicular structure and the expression of androgen receptors and proliferating cell nuclear antigen in diabetic rats. Andrologia 52:e13528. https://doi.org/10.1111/and.13528
Antunes GLM, Darin JD, Bianchi MD (2000) Protective effects of vitamin C against cisplatin-induced nephrotoxicity and lipid peroxidation in adult rats: a dose-dependent study. Pharmacol Res 41(4):405–411. https://doi.org/10.1006/phrs.1999.0600
Ajith TA, Nivitha V, Usha S (2007) Zingiber officinale Roscoe alone and in combination with alpha-tocopherol protect the kidney against cisplatin-induced acute renal failure. Food Chem Toxicol 45(6):921–927. https://doi.org/10.1016/j.fct.2006.11.014
Babu D, Leclercq G, Goossens V, Remijsen Q, Vandenabeele P, Motterlini R, Lefebvre RA (2015) Antioxidant potential of CORM-A1 and resveratrol during TNF-alpha/cycloheximide-induced oxidative stress and apoptosis in murine intestinal epithelial MODE-K cells. Toxicol Appl Pharmacol 288(2):161–178. https://doi.org/10.1016/j.taap.2015.07.007
Bancroft JD, Layton C (2013) The hematoxylins and eosin (chapter 10). In: Suvarna SK, Layton C, and Bancroft JD (2013) Bancroft’s Theory and Practice of Histological Techniques, 7th edn. UK: Churchill, Living Stone, Elsevier, Ebook (Online) ISBN: 978–0–7020–5032–9. Available from: https://books.google.com.eg/books. p 173–186
Beagloo IE, Valilu MR, Motiei M, Rahbar M, Hejazi A (2019) The antioxidant and hepatoprotective effect of alcoholic extract of ginger against the cisplatin induced oxidative stress in rats. Biomed J Sci Tech Res 19(2):14240–14245. https://doi.org/10.26717/BJSTR.2019.19.003283
Bevilacqua MP, Pober JS, Wheeler ME, Cotran RS, Gim-brone MA (1985) Interleukin 1 acts on cultured human vascular endothelium to increase the adhesion of poly morpho nuclear leukocytes, monocytes, and related leukocyte cell lines. J Clin Invest 76(5):2003–2011. https://doi.org/10.1172/JCI112200
Caglayan C, Kandemir FM, Yıldırım S, Kucukler S, Kılınc MA, Saglam YS (2018) Zingerone ameliorates cisplatin-induced ovarian and uterine toxicity via suppression of sex hormone imbalances, oxidative stress, inflammation and apoptosis in female Wistar rats. Biomed Pharmacother 102:517–530. https://doi.org/10.1016/j.biopha.2018.03.119
Dinarello CA (2009) Immunological and inflammatory functions of the interleukin 1 family. Annu Rev Immunol 27(519):550. https://doi.org/10.1146/annurev.immunol.021908.132612
Dkhil MA, Al-Quraishy S, Aref AM, Othman MS, El-Dieb KM, Moniem A (2013) The potential role of Azadirachta indica treatment on cisplatin-induced hepatotoxicity and oxidative stress in female rats. Oxid Med Cell Longev 741817. https://doi.org/10.1155/2013/741817
Eldutar E, Kandemir FM, Kucukler S, Caglayan C (2017) Restorative effects of Chrysin pretreatment on oxidant–antioxidant status, inflammatory cytokine production, and apoptotic and autophagic markers in acute paracetamol-induced hepatotoxicity in rats: an experimental and biochemical study. J Biochem Mol Toxicol 31:e21960. https://doi.org/10.1002/jbt.21960
Elkomy A, Abdelhiee EY, Fadl SE, Emam MA, Gad F, Sallam A, Alarifi S, Abdel-Daim MM, Aboubakr M (2020) L-carnitine mitigates oxidative stress and disorganization of cytoskeleton intermediate filaments in cisplatin-induced hepato- renal toxicity in rats. Front Pharmacol 11:574441. https://doi.org/10.3389/fphar.2020.574441
El-Kordy EA (2019) Effect of suramin on renal proximal tubular cells damage induced by cisplatin in rats (histological and immunohistochemical study). J Microsc Ultrastruct 79(4):153–164. https://doi.org/10.4103/JMAU.JMAU_21_19
El-Sheikh AAK (2020) P-glycoprotein/ABCB1 might contribute to morphine/cisplatin-induced hepatotoxicity in rats. Sci Pharm 88(1):14. https://doi.org/10.3390/scipharm88010014
Farber E (1994) Programmed cell death: necrosis versus apoptosis. Mod Pathol 7(5):605–609
Farid AS, El Shemy MA, Nafie E, Hegazy AM, Abdelhiee EY (2021) Anti-inflammatory, anti-oxidant and hepatoprotective effects of lactoferrin in rats. Drug Chem Toxicol 44(3):286–293. https://doi.org/10.1080/01480545.2019.1585868
Faubel S, Lewis EC, Reznikov L, Ljubanovic D, Hoke TS, Somerset H, Oh DG, Lu L, Klein CL, Dinarello CA, Edelstein CL (2007) Cisplatin-induced acute renal failure is associated with an increase in the cytokines interleukin (IL)-1beta, IL-18, IL-6, and neutrophil infiltration in the kidney. J Pharmacol Exp Ther 322(1):8–15. https://doi.org/10.1124/jpet.107.119792
Franciscoa M, Morenob DA, Carteaa ME, Ferreres F, García-Viguera C, Velasco P (2009) Simultaneous identification of glucosinolates and phenolic compounds in a representative collection of vegetable Brassica rapa. J Chromatogr A 1216(38):6611–6619. https://doi.org/10.1016/j.chroma.2009.07.055
Grant KL, Lutz RB (2000) Ginger Am J Health System Pharm 57(10):945–947. https://doi.org/10.1093/ajhp/57.10.945
Gruol DL, Puro A, Hao C, Blakely P, Janneke E, Vo K (2011) Neuroadaptive changes in cerebellar neurons induced by chronic exposure to IL-6. J Neuroimmunol 239(1–2):28–36. https://doi.org/10.1016/j.jneuroim.2011.08.009
Holmin S, Mathiesen T (2000) Intra cerebral administration of interleukin-1beta and induction of inflammation, apoptosis, and vasogenic edema. J Neurosurg 92(1):108–120. https://doi.org/10.3171/jns.2000.92.1.0108
Hong KO, Hwang JK, Park KK, Kim SH (2005) Phosphorylation of c-Jun N-terminal Kinases (JNKs) is involved in the preventive effect of xanthorrhizol on cisplatin-induced hepatotoxicity. Arch Toxicol 79(4):231–236. https://doi.org/10.1007/s00204-004-0623-7
Hsu BG, Lee RP, Yang FL, Harn HJ, Chen HI (2006) Post-treatment with N-acetylcysteine ameliorates the endotoxin shock-induced organ damage in conscious rats. Life Sci 79(21):2010–2016. https://doi.org/10.1016/j.lfs.2006.06.040
Ingawale DK, Mandlik SK, Naik SR (2014) Models of hepatotoxicity and the underlying cellular, biochemical and immunological mechanism(s): a critical discussion. Environ Toxicol Pharmacol 37(1):118–133. https://doi.org/10.1016/j.etap.2013.08.015
Ishikawa T (2009) Future perspectives on the treatment of hepatocellular carcinoma with cisplatin. World J Hepatol 1(1):8–16. https://doi.org/10.4254/wjh.v1.i1.8
Kandemir FM, Kucukler S, Caglayan C, Gur C, Batil AA, Gülçin İ (2017) Therapeutic effects of silymarin and naringin on methotrexate-induced nephrotoxicity in rats: biochemical evaluation of anti-inflammatory, antiapoptotic, and antiautophagic properties. J Food Biochem 41:e12398. https://doi.org/10.1111/jfbc.12398
Kandemir FM, Yildirim S, Caglayan C, Kucukler S, Eser G (2019) Protective effects of zingerone on cisplatin-induced nephrotoxicity in female rats. Environ Sci and Pollut Res Int 26(22):22562–22574. https://doi.org/10.1007/s11356-019-05505-3
Karadeniz A, Simsek N, Karakus E, Yildirim S, Kara A, Can I, Kisa F, Emre H, Turkeli M (2011) Royal jelly modulates oxidative stress and apoptosis in liver and kidneys of rats treated with cisplatin. Oxid Med Cell Longev 2011:981793. https://doi.org/10.1155/2011/981793
Kishimoto S, Miyazawa K, Terakawa Y, Ashikari H, Ohtani A, Fukushima S, Takeuchi Y (2000) Cytotoxicity of cis-[((1R,2R)-1,2-cyclohexanediamine-N, N’)bis(myristato)]-platinum (II) suspended in Lipiodol in a newly established cisplatin-resistant rat hepatoma cell line. Jpn J Cancer Res 91(12):1326–1332. https://doi.org/10.1111/j.1349-7006.2000.tb00921.x
Kishimoto T, Akira S, Narazaki M, Taga T (1995) Interleukin‑6 family of cytokines and gp130. Blood 86:1243–1254. https://doi.org/10.1182/blood.V86.4.1243.bloodjournal8641243
Knoblach SM, Faden AI (1998) Interleukin-10 improves outcome and alters pro-inflammatory cytokine expression after experimental traumatic brain injury. Exp Neurol 153(1):143–151. https://doi.org/10.1006/exnr.1998.6877
Knoblach SM, Fan L, Faden AI (1999) Early neuronal expression of tumor necrosis factor-alpha after experimental brain injury contributes to neurological impairment. J Neuroimmunol 95(1–2):115–125. https://doi.org/10.1016/S0165-5728(98)00273-2
Lantz RC, Chena GJ, Sarihana M, Solyomb M, Joladb SD, Timmermannb BN (2007) The effect of extracts from ginger rhizome on inflammatory mediator production. Phytomedicine 14(2–3):123–128. https://doi.org/10.1016/j.phymed.2006.03.003
Lazarenko VA, Lyashev YD, Shevchenko NI (2014) Effect of a synthetic indolicidin analogue on lipid peroxidation in thermal burns. Bull Exp Biol Med 157(4):447–449. https://doi.org/10.1007/s10517-014-2587-9
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193(1):265–275
Luster MI, Simeonova PP, Gallucci R, Matheson J (1999) Tumor necrosis factor alpha and toxicology. Crit Rev Toxicol 29(5):491–511. https://doi.org/10.1080/10408449991349258
Ma P, Xiao H, Yu C, Liu J, Cheng Z, Song H, Zhang X, Li C, Wang J, Gu Z, Lin J (2017) Enhanced cisplatin chemotherapy by iron oxide nanocarrier-mediated generation of highly toxic reactive oxygen species. Nano Lett 17(2):928–937. https://doi.org/10.1021/acs.nanolett.6b04269
Malik S, Suchal K, Gamad N, Dinda AK, Arya DS, Bhatia J (2015) Telmisartan ameliorates cisplatin-induced nephrotoxicity by inhibiting MAPK mediated inflammation and apoptosis. Eur J Pharmacol 748:54–60. https://doi.org/10.1016/j.ejphar.2014.12.008
Mohamed HE, Badawy MM (2019) Modulatory effect of zingerone against cisplatin or y-irradiation induced hepatotoxicity by molecular targeting regulation. Appl Radiat Isot 154:108891. https://doi.org/10.1016/j.apradiso.2019.108891
Nežić L, Amidžić L, Škrbić R, Gajanin R, Nepovimova E, Vališ M, Kuca K, Jacević V (2019) Simvastatin inhibits endotoxin- induced apoptosis in liver and spleen through up-regulation of survivin/NF-_B/p65 expression. Front Pharmacol 10:54. https://doi.org/10.3389/fphar.2019.00054
Ozkok A, Edelstein CL (2014) Pathophysiology of cisplatin-induced acute kidney injury. Biomed Res Int 2014:967826. https://doi.org/10.1155/2014/967826
Pan MH, Hsieh MC, Kuo JM, Lai CS, Wu H, Sang Sh, Ho CT (2008) 6-Shogaol induces apoptosis in human colorectal carcinoma cells via ROS production, caspase activation, and GADD 153 expression. Mol Nutr Food Res 52(5):527–537. https://doi.org/10.1002/mnfr.200700157
Perez RP (1998) Cellular and molecular determinants of cisplatin resistance. Eur J Cancer 34(10):1535–1542. https://doi.org/10.1016/s0959-8049(98)00227-5
Pober JS, Min W (2006) Endothelial cell dysfunction, injury and death. Handb Exp Pharmacol (176 Pt 2):135–156. https://doi.org/10.1007/3-540-36028-x_5
Ramesh G, Reeves WB (2002) TNF-alpha mediates chemokine and cytokine expression and renal injury in cisplatin nephrotoxicity. J Clin Invest 110(6):835–842. https://doi.org/10.1172/JCI15606
Rana SVS (2008) Metals and apoptosis: recent developments. J Trace Elem Med Biol 22(4):262–284. https://doi.org/10.1016/j.jtemb.2008.08.002
Romano M, Sironi M, Toniatti C, Polentarutti N, Fruscella P, Ghezzi P, Luini W, Hinsbergh V, Sozzani S, Bussolino F, Poli V, Ciliberto G, Mantovani A (1997) Role of IL-6and its soluble receptor in induction of chemokines and leukocyte recruitment. Immunity 6(3):315–325. https://doi.org/10.1016/s1074-7613(00)80334-9
Sadeghi H, Mansourian M, PanahiKokhdan E, Salehpour Z, Sadati I, Abbaszadeh-Goudarzi K, Asfaram A, Doustimotlagh AH (2020) Antioxidant and protective effect of Stachys pilifera Benth against nephrotoxicity induced by cisplatin in rats. J Food Biochem 44(5):e13190. https://doi.org/10.1111/jfbc.13190
Sen S, De B, Devanna N, Chakraborty R (2013) Cisplatin induced nephrotoxicity in mice: protective role of Leea asiatica leaves. Renal Fail 35(10):1412–1417. https://doi.org/10.3109/0886022X.2013.829405
Sendecor GW, Cochran WG (1987) The comparison of two samples. Statistical methods, 4th ed. Iowa State University, p 91–110
Shaw J, Chen B, Huang WH, Lee AR, Media J, Valeriote FA (2011) The small-molecule TNF-alpha modulator, UTL-5g, reduces side effects induced by cisplatin and enhances the therapeutic effect of cisplatin in vivo. J Exp Ther Oncol 9(2):129–137
Singh RP, Agarwal R (2002) Flavonoid antioxidant silymarin and skin cancer. Antioxid Redox Signal 4(4):655–663. https://doi.org/10.1089/15230860260220166
Sun C, Nie J, Zheng Z, Zhao J, Wu L, Zhu Y, Su Z, Zheng G, Feng B (2019) Renoprotective effect of scutellarin on cisplatin-induced renal injury in mice: impact on inflammation, apoptosis, and autophagy. Biomed Pharmacother 112:108647. https://doi.org/10.1016/j.biopha.2019.108647
Surh YJ (2002) Anti-tumor promoting potential of selected spice ingredients with antioxidative and anti-inflammatory activities: a short review. Food and Chem Toxicol 40(8):1091–1097. https://doi.org/10.1016/s0278-6915(02)00037-6
Tadagavadi RK, Reeves WB (2010) Endogenous IL-10 attenuates cisplatin nephrotoxicity: role of dendritic cells. J Immunol 185(8):4904–4911. https://doi.org/10.4049/jimmunol.1000383
Wojcik M, Burzynska Pedziwiatr I, Wozniak LA (2010) A review of natural and synthetic antioxidants important for health and longevity. Curr Med Chem 17(28):3262–3288. https://doi.org/10.2174/092986710792231950
Yao X, Panichpisal K, Kurtzman N, Nugent K (2007) Cisplatin nephrotoxicity: a review. Am J Med Sci 334(2):115–124. https://doi.org/10.1097/MAJ.0b013e31812dfe1e
Yiming L, Van HT, Colin CD, Basil DR (2012) Preventive and protective properties of Zingiber officinale (Ginger) in diabetes mellitus, diabetic complications, and associated lipid and other metabolic disorders: a brief review. Evid Based Complement and Alternat Med 516870:1–10. https://doi.org/10.1155/2012/516870
Yang W, Yu XH, Wang C, He WS, Zhang SJ, Yan YG, Zhang J, Xiang YX, Wang WJ (2015) Interleukin-1β in intervertebral disk degeneration. Clin Chim Acta 450:262–272. https://doi.org/10.1016/j.cca.2015.08.029
Yang R, Guo P, Ma Z, Chang C, Meng Q, Gao Y, Khan I, Wang X, Cui Z (2020) Effects of simvastatin on iNOS and caspase-3 levels and oxidative stress following smoke inhalation injury. Mol Med Rep 22(4):3405–3417. https://doi.org/10.3892/mmr.2020.11413
Yiran Z, Chenyang J, Jiajing W, Yan Y, Jianhong G, Jianchun B, Zongping L (2013) Oxidative stress and mitogen-activated protein kinase pathways involved in cadmium-induced BRL 3A cell apoptosis. Oxid Med Cell Longev 2013:516051. https://doi.org/10.1155/2013/516051
Yu ZQ, Jia Y, Chen G (2014) Possible involvement of cathepsin B/D and caspase-3 in deferoxamine-related neuro protection of early brain injury after subarachnoid haemorrhage in rats. Neuropathol Appl Neurobiol 40(3):270–283. https://doi.org/10.1111/nan.12091
Zhang QF (2017) Ulinastatin inhibits renal tubular epithelial apoptosis and interstitial fibrosis in rats with unilateral ureteral obstruction. Mol Med Rep 16(6):8916–8922. https://doi.org/10.3892/mmr.2017.7692
Zhu S, Pabla N, Tang C, He L, Dong Z (2015) DNA damage response in cisplatin-induced nephrotoxicity. Arch Toxicol 89(12):2197–2205. https://doi.org/10.1007/s00204-015-1633-3
Acknowledgements
The authors would like to thank the laboratory technician at the Department of Veterinary Pathology, Faculty of Veterinary Medicine, for their great help during preparation of histopathological slides.
Author information
Authors and Affiliations
Contributions
All the listed authors have made substantial contributions to the research design and acquisition, analysis, or interpretation of the data. ET and AE performed histopathology and IHC examination; GE performed chemical examination. All the authors have shared in writing the manuscript and approved the final submitted version.
Corresponding author
Ethics declarations
Ethics approval
The Research Ethical Committee of Animal Experiments of faculty of veterinary medicine at University of Sadat city, Egypt has approved our experimental protocol (VUSC-017–5-20).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tahoun, E., Elgedawy, G. & El-Bahrawy, A. Cytoprotective effect of ginger extract on cisplatin-induced hepatorenal toxicity in rats via modulation of oxidative stress, inflammation and apoptosis: histopathological, biochemical and immunohistochemical study. Comp Clin Pathol 30, 647–663 (2021). https://doi.org/10.1007/s00580-021-03256-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-021-03256-7