Abstract
Nephrotoxicity is a common adverse effect of treatment with cisplatin (CDDP). This study was performed to evaluate the antioxidant and nephroprotective efficacy of ceftriaxone (CTX) and vitamin E (Vit.E), alone and in combination against CDDP-induced acute renal injury. Fifty-six male albino rats were equally divided into seven groups, receiving (I) normal saline, (II) CTX (100 mg/kg, intraperitoneal [i.p] injection), (III) Vit.E (100 mg/kg orally), (IV) CDDP (5 mg/kg i.p injection), (V) CDDP plus CTX, (VI) CDDP plus Vit.E, and (VII) CDDP plus CTX in combination with Vit.E. All treatments were administered daily for 10 days except CDDP, which was given as a single dose at the sixth day of the study. Compared to normal control rats, CDDP-injected rats showed significantly (p < 0.05) higher serum levels of renal injury biomarkers (uric acid, urea, and creatinine) and tumor necrosis factor-α (TNF-α), as well as increased renal tissue concentrations of malondialdehyde, nitric oxide, and TNF-α. Moreover, CDDP administration was associated with significantly lower (p < 0.05) renal tissue levels of reduced glutathione and activities of endogenous antioxidant enzymes (glutathione peroxidase, superoxide dismutase, and catalase) and total antioxidant capacity. All these alterations were significantly ameliorated in CDDP-injected rats, receiving CTX and/or Vit.E, compared to rats receiving CDDP alone. Interestingly, the antioxidant and anti-inflammatory effects were more marked in the CTX-Vit.E combination group, compared to groups receiving either drug alone. In conclusion, CTX and Vit.E (especially in combination) could counteract the nephrotoxic effect of CDDP, probably through their antioxidant activities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
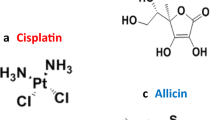
Cisplatin (cis-diamminedichloroplatinum II, CDDP) is a potent antineoplastic agent. However, its main dose-limiting side effects include nephrotoxicity, neurotoxicity, ototoxicity, allergic reactions, and hemorrhage (Dasari and Tchounwou 2014; Wang and Lippard 2005). Among these side effects, nephrotoxicity remains the most common, manifesting as acute kidney injury (AKI) in 20 to 30% of patients (Goldstein and Mayor 1983) and limiting the use of CDDP in cancer therapy (Thadhani et al. 1996). The mechanisms by which CDDP exerts its anti-carcinogenic or cytotoxic effects in normal tissues involve inflammation, oxidative stress, and apoptosis. Cisplatin can directly bind to DNA, forming inter- and intra-strand cross-links, which arrests DNA synthesis and replication, especially in rapidly proliferative cells (Jamieson and Lippard 1999; Zamble and Lippard 1995). The main nephrotoxic effect of CDDP occurs by generation of reactive oxygen species (ROS) (Arany and Safirstein 2003). Moreover, CDDP is bio-transformed by the microsomal cytochrome-P450 system into a highly reactive thiol form, depleting glutathione during this reaction. Further, it causes mitochondrial dysfunction, leading to exhaustion of the mitochondrial antioxidants and oxidative stress-mediated cytotoxicity (Siddik 2003).
Ceftriaxone (CTX) is a third-generation cephalosporin with a potent activity against several Gram-positive and Gram-negative bacteria (Bertram 2009). It is clinically used to treat acute bacterial otitis media, bone and joint infections, gonorrhea, intra-abdominal and urinary tract infections, and bacterial septicemia (Perry and Schentag 2001). The antibacterial activity of CTX is due to inhibition of the mucopeptide synthesis in the bacterial cell wall (Rothstein et al. 2005). Former studies reported that CTX protects against neurodegenerative disorders, including cerebral ischemia, amyotrophic lateral sclerosis, and epilepsy (Rothstein et al. 2005), and alleviates neuropathic pain in diabetic rats (Gunduz et al. 2011). Other authors showed that CTX can protect against the nephrotoxicity of tobramycin (Beauchamp et al. 1994), isepamicin (Yoshiyama et al. 1998), cyclosporine A (Yılmaz et al. 2011), and cadmium (Dwivedi et al. 2012) in rats.
Vitamin E (Vit.E) is a naturally occurring, fat-soluble molecule that has a potent, chain-breaking antioxidant activity. It can scavenge ROS and lipid peroxyl radicals (Arreola-Mendoza et al. 2006; Burton et al. 1982; Traber and Stevens 2011). Moreover, it protects the cell membrane integrity by inhibiting the peroxidation of polyunsaturated fatty acids (Ellie and Rolfes 2011). In a randomized controlled trial on cancer patients treated with CDDP, Vit.E supplementation significantly increased the plasma antioxidant enzymatic levels (Weijl et al. 2004). Further, high doses of Vit.E were shown able to protect against CDDP-induced oxidative damage to renal, hepatic (Nazıroǧlu et al. 2004), and neural tissues in rats (Younan and Rashed 2013).
To our knowledge, no previous studies investigated the chemopreventive effects of CTX against acute CDDP nephrotoxicity. Thus, this study was performed to evaluate the antioxidant and nephroprotective efficacy of CTX and/or Vit.E against CDDP-induced AKI.
Materials and methods
Animals
Fifty-six Wistar albino rats (males, weighing 170–200 g) were obtained from The Egyptian Organization for Biological Products and Vaccines (Giza, Egypt). The animals were acclimatized for 10 days in propylene cages with wire mesh cover and sawdust bedding and housed in a well-ventilated room with normal temperature (22 ± 2 °C) and light/dark cycle. They received balanced diet and tape water ad libitum. The Research Ethical Committee at Suez Canal University approved our experimental protocol (approval no. 20147). All animal stress conditions were taken into consideration and hardly avoided.
Chemicals
Cisplatin (Cisplatin® vial, CAS 15663-27-1) was purchased as a clinical formulation from Merck Co. (Lyon, France). Ceftriaxone (250 mg vial as crystalline powder) was obtained from Sandoz-Novartis, Egypt, while vitamin E was provided by Adwia Pharmaceuticals (Cairo, Egypt). The analytical kits were obtained from Biodiagnostics Co. (Dokki, Giza, Egypt) except for TNF-α assay kits (Assay Designs Inc., Ann Arbor, MI, USA). The other used chemicals in this study were of the highest analytical grade, available commercially.
Animal grouping and work design
After acclimatization, rats were randomly allocated into seven groups (n = 8 per group). Eight rats served as controls (group I) and were injected with normal saline. Group II rats received CTX (100 mg/kg bw intraperitoneal [i.p] injection) (Gunduz et al. 2011), while group III rats received Vit.E (100 mg/kg bw orally) (Stojiljkovic et al. 2018). Group IV rats received normal saline and cisplatin (5 mg/kg bw i.p injection) (de Oliveira et al. 2003), while rats in groups V and VI received CDDP plus CTX and CDDP plus Vit.E, respectively. Lastly, group VII rats received cisplatin plus CTX with Vit.E in combination. All treatments were administered daily for 10 days except CDDP [a single i.p. injection at the sixth day of the treatment schedule]. Each treatment was given at the same dose and via the same route in different groups.
Sample collection and preparation of tissue homogenate
After completing the dosing schedules, all rats were fasted overnight. Then, blood samples were obtained from the retro-orbital plexus under isoflurane anesthesia in centrifugation tubes without anticoagulants. The samples were allowed to clot at 25 °C and then centrifuged for 15 min (at 3000 rpm). The obtained sera were then stored at − 20 °C as aliquots for biochemical assays.
The animals were sacrificed by cervical dislocation. The kidneys were then removed, cleaned of connected tissue and blood clots, and washed with normal saline. Next, kidneys were perfused with sodium phosphate (Na2HPO4/NaH2PO4) buffer (50 mM, pH 7.4) mixed with heparin (0.16 mg/ml) to remove any blood clots. Following that, 1 g tissue was homogenized in 5–10 ml cold PBS (PH 7.4) in Teflon Dounce Tissue Grinder (Omni International, Kennesaw Georgia), surrounded by ice media then centrifuged at 4 °C, 10,000 rpm for 15 min in a cooling centrifuge. The resulting supernatant was collected in Eppendorf tubes and stored at − 80 °C.
Serum and tissue biochemical analyses
Serum creatinine, urea, and uric acid levels were measured according to Larsen (1972), Coulombe and Favreau (1963), and Whitehead et al. (1991), respectively. The renal tissue concentrations of malondialdehyde (MDA: lipid peroxidation biomarker) and nitric oxide (NO: nitrosative stress biomarker) were measured according to Mihara and Uchiyama (1978) and Green et al. (1982), respectively. The non-enzymatic antioxidant biomarker (reduced glutathione (GSH)) was assessed according to Beutler et al. (1963). While the enzymatic antioxidants superoxide dismutase (SOD), glutathione peroxidase (GPx), and catalase (CAT) were evaluated according to Nishikimi et al. (1972), Paglia and Valentine (1967), and Aebi (1984), respectively. Further, the total antioxidant capacity (TAC) was evaluated according to Koracevic et al. (2001). The serum and renal tissue concentrations of TNF-α were measured using commercial kits from R&D Systems (Minneapolis, MN, USA) according to the manufacturer’s protocol.
Statistical analysis
The obtained data were expressed as means ± standard error of means (SEM). The statistical significance of between-group differences was analyzed using the Statistical Package for Social Sciences (SPSS, version 22, IBM, Chicago, IL). For comparison, the ANOVA was used, followed by post hoc Tukey’s test. The statistical significance was set at p ≤ 0.05.
Results
Serum markers of renal injury
Biochemical analysis of renal injury biomarkers showed significant elevations in urea, uric acid, and creatinine levels by 186.4, 189.5, and 927.5%, respectively, in CDDP-intoxicated rats, compared to the untreated control group. Treatment with CTX (100 mg/kg bw i.p) and Vit.E (100 mg/kg bw oral) daily for 5 days before and after CDDP injection significantly reduced (p ≤ 0.05) serum uric acid, urea, and creatinine by about 26.7, 28.5, and 51%, respectively, in the CTX group and 44.1, 43.9, and 61.3%, respectively, in the Vit.E group, compared to the CDDP-intoxicated rats. The most significant reduction (p ≤ 0.05) in the serum levels of these parameters was obtained with CTX + Vit.E combination (57.4, 62.3, and 87.3%, respectively, in comparison to the CDDP group) (Figs. 1, 2, and 3).
Renal lipid peroxidation and antioxidant biomarkers
Compared to normal control rats, CDDP-intoxicated rats exhibited significant increases (p ≤ 0.05) in renal MDA and NO levels (273 and 104.9%, respectively), as well as significant decreases in renal GSH, GPx, SOD, CAT, and TAC (28.8, 38.7, 52.2, 52.2, and 31.4%, respectively). In contrast, treatment of CDDP-intoxicated rats with CTX or Vit.E significantly reduced renal MDA (24.6 and 50.4%, respectively) and NO (26.3 and 32.5%, respectively), as well as increased renal GSH (23.6 and 32.7%, respectively), GPx (34 and 52%, respectively), SOD (56.2 and 77.8%, respectively), CAT (31.9 and 61.3%, respectively), and TAC levels (25.6 and 38.5, respectively), compared to CDDP-intoxicated rats. The most significant improvements were recorded when CTX and Vit.E were given in combination with CDDP: reduction of renal MDA and NO levels (by 68.6 and 47.2%, respectively) and increase in GSH, GPx, SOD, CAT, and TAC levels (by 40, 59.8, 113.5, 97.4, and 44.9%, respectively) (Table 1).
Serum and renal TNF-α assays
Cisplatin intoxication was associated with significant increases (p ≤ 0.05) in serum and renal tissue TNF-α concentrations (339.6 and 371.4%, respectively), compared to control rats. Treatment with CTX or Vit.E was associated with significant reductions (p ≤ 0.05) in serum (45.7% and 53.9%, respectively) and renal TNF-α (66.3% and 70.7%, respectively) levels. Further, when CTX and Vit.E were administered together, more significant (p ≤ 0.05) reductions in serum and TNF-α levels were recorded (73.2 and 76.5%, respectively), compared to CDDP-intoxicated rats (Figs. 4 and 5).
In all investigated parameters, no significant changes were detected in rats that received CTX (second group) or Vit.E alone (third group) in comparison to normal control rats (first group), highlighting the safety of both agents at the tested doses, routes, and durations of administration.
Discussion
Cisplatin may be used alone or with radiotherapy to treat several solid tumors, especially treatment-resistant ones. The therapeutic potency of CDDP is dose-dependent; however, its clinical use is jeopardized by cumulative neurotoxicity and nephrotoxicity (O’Dwyer et al. 1999). Although other platinum-based drugs as carboplatin are non-nephrotoxic derivatives, CDDP remains the first choice in several platinum-based chemotherapeutic regimens. Various experiments were performed to identify novel agents that would mitigate CDDP nephrotoxicity without diminishing its anticancer efficacy. In this direction, this study was performed to investigate the chemoprotective effects of Vit.E and/or CTX against CDDP-induced acute renal injury.
Treatment of rats with a single i.p. dose of cisplatin induced oxidative stress-mediated renal injury as marked by (a) the significant elevation in serum urea, uric acid, and creatinine; (b) augmented renal tissue levels of lipid peroxidation (MDA) and nitrosative stress (NO) markers; (c) drop in tissue GSH concentration, TAC, and activities of antioxidant enzymes, indicating disturbed oxidant/antioxidant balance; and (d) elevated serum and renal tissue TNF-α concentrations. These results confirm those of previous studies on acute and sub-acute CDDP nephrotoxicity in mice and rats (Hassan et al. 2014; Ibrahim et al. 2016; Kawai et al. 2009).
Multiple mechanisms have been postulated for CDDP-induced renal cell injury; among them, oxidative stress and inflammation are the most important (Hanigan and Devarajan 2003; Miller et al. 2010). Proximal tubular cells express the transporters and enzymes, needed in each step of CDDP bio-activation into a more potent nephrotoxin (Park et al. 2002; Townsend et al. 2003). This metabolic activation process starts in the kidneys with the formation of glutathione conjugates, causing GSH depletion and formation of the reactive thiol nephrotoxin (Townsend et al. 2009). The latter induces oxidative stress and cellular apoptosis (Baliga et al. 1997). Moreover, CDDP significantly increases NADPH oxidase gene expression, a membrane-bound enzyme that generates high levels of O2·− (Babior 2004; Palipoch et al. 2014). The generated free radicals cause membrane lipid peroxidation and denaturation of DNA and proteins, which lead to enzymatic inactivation and mitochondrial dysfunction, enhancing ROS production via the disruption of the respiratory chain (Kruidering et al. 1997; Yilmaz et al. 2004). In addition, CDDP induces microsomal free radicals (superoxide anion (O2·), hydrogen peroxide (H2O2), and hydroxyl radical (·OH)) formation via the cytochrome-P450 (CYP) system, overwhelming the endogenous antioxidant mechanisms (Liu and Baliga 2003). Further, the renal injury, caused by CDDP, is partly mediated by a series of inflammatory changes and enhancement in renal expression of TNF-α (Deng et al. 2001). The latter can induce apoptosis and ROS generation and coordinate the activation of a large network of cytokines in the kidney (Ramesh and Reeves 2002, 2004).
Daily treatment with CTX antibiotic and Vit.E solely or in combination daily for 5 days before and after CDDP treatment significantly ameliorated all CDDP-induced alterations and relatively restored the normal cellular redox status. These findings confirm the results of previous studies, which examined the renoprotective effects of CTX against xenobiotics-induced nephrotoxicity (Beauchamp et al. 1994; Dwivedi et al. 2012; Yılmaz et al. 2011; Yoshiyama et al. 1998). Abdel-Daim and El-Ghoneimy (2015) referred the renoprotective effect of CTX against diazinon and deltamethrin-induced oxidative stress to its ability to scavenge ROS and enhance antioxidant enzymes’ activities. Moreover, cephalosporins can act as multidentate chelating agents and contain thio-ether groups, which prevent free radical-mediated oxidation (Anacona and Osorio 2008).
Vitamin E is an exogenous antioxidant that exerts its function through the GPx pathway (Wefers and Sies 1988). As a lipid-soluble antioxidant, it prevents the propagation of lipid peroxidation in the cell membrane by free radicals scavenging (Ellie and Rolfes 2011) and interference with oxidase enzymes, which initiate the production of free radicals (Palipoch et al. 2014). Previous studies proved that Vit.E can mitigate CDDP-induced ototoxicity and nephrotoxicity without interfering with its anti-tumor efficacy (Kalkanis et al. 2004; Leonetti et al. 2003). Moreover, Azzi et al. (2002) concluded that Vit.E reduced the production of NO and superoxide radicals (by endothelial cells and neutrophils, respectively) via inhibiting protein kinase C. In parallel, Vit.E was found to have anti-inflammatory effect beside its antioxidant effect. Several studies have shown that pre-treatment with Vit.E reduces TNF-α production in dichromate-induced nephrotoxicity (Mehany et al. 2013) and acetic acid colitis (Tahan et al. 2011). Future investigators are recommended to perform additional studies on urine osmolarity and chemical properties, histopathological studies of the kidneys, and exploration of the involved inflammatory pathways with the tested pharmacological compounds.
In conclusion, pre-treatment of rats with CTX and Vit.E, alone or in combination, can protect against CDDP nephrotoxicity and should be considered in future trials on nephroprotection against chemotherapeutic drugs.
Abbreviations
- CAT:
-
Catalase
- CDDP:
-
cis-diamminedichloroplatinum II
- CTX:
-
Ceftriaxone
- GPx:
-
Glutathione peroxidase
- GSH:
-
Reduced glutathione
- MDA:
-
Malondialdehyde
- NO:
-
Nitric oxide
- ROS:
-
Reactive oxygen species
- SOD:
-
Superoxide dismutase
- TAC:
-
Total antioxidant capacity
- TNF-α:
-
Tumor necrosis factor-α
- Vit.E:
-
Vitamin E
References
Abdel-Daim MM, El-Ghoneimy A (2015) Synergistic protective effects of ceftriaxone and ascorbic acid against subacute deltamethrin-induced nephrotoxicity in rats. Ren Fail 37:297–304
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126
Anacona JR, Osorio I (2008) Synthesis and antibacterial activity of copper (II) complexes with sulphathiazole and cephalosporin ligands. Transit Met Chem 33:517–521
Arany I, Safirstein RL (2003) Cisplatin nephrotoxicity. Semin Nephrol 23:460–464
Arreola-Mendoza L, Reyes JL, Melendez E, Martín D, Namorado MC, Sanchez E, Del Razo LM (2006) Alpha-tocopherol protects against the renal damage caused by potassium dichromate. Toxicology 218:237–246
Azzi A, Ricciarelli R, Zingg J-M (2002) Non-antioxidant molecular functions of α-tocopherol (vitamin E). FEBS Lett 519:8–10
Babior BM (2004) NADPH oxidase is a membrane-bound enzyme which has the ability to generate high levels of O2•- in response to stimulus. Curr Opin Immunol 16:42–47
Baliga R, Ueda N, Walker PD, Shah SV (1997) Oxidant mechanisms in toxic acute renal failure. Am J Kidney Dis 29:465–477
Beauchamp D, Thériault G, Grenier L, Gourde P, Perron S, Bergeron Y, Fontaine L, Bergeron MG (1994) Ceftriaxone protects against tobramycin nephrotoxicity. Antimicrob Agents Chemother 38:750–756
Bertram KA (2009) Basic and clinical pharmacology, Eleventh edn. McGraw-Hill, New York
Beutler E, Duron O, Kelly BM (1963) Improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Burton G, Joyce A, Ingold K (1982) First proof that vitamin E is major lipid-soluble, chain-breaking antioxidant in human blood plasma. Lancet 320:327
Coulombe J, Favreau L (1963) A new simple semimicro method for colorimetric determination of urea. Clin Chem 9:102–108
Dasari S, Tchounwou PB (2014) Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol 740:364–378
de Oliveira ML, Antunes LMG, Francescato HDC, Bianchi MLP (2003) The effects of oral glutamine on cisplatin-induced nephrotoxicity in rats. Pharmacol Res 47:517–522
Deng J, Kohda Y, Chiao H, Wang Y, Hu X, Hewitt SM, Miyaji T, Mcleroy P, Nibhanupudy B, Li S (2001) Interleukin-10 inhibits ischemic and cisplatin-induced acute renal injury. Kidney Int 60:2118–2128
Dwivedi VK, Bhatanagar A, Chaudhary M (2012) Protective role of ceftriaxone plus sulbactam with VRP1034 on oxidative stress, hematological and enzymatic parameters in cadmium toxicity induced rat model. Interdiscip Toxicol 5:192–200
Ellie WR, Rolfes SR (2011) In: Williams P (ed) Understanding nutrition, Twelfth edn. Wadsworth, Cengage Learning, California
Goldstein RS, Mayor GH (1983) The nephrotoxicity of cisplatin. Life Sci 32:685–690
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR (1982) Analysis of nitrate, nitrite, and [15N] nitrate in biological fluids. Anal Biochem 126:131–138
Gunduz O, Oltulu C, Buldum D, Guven R, Ulugol A (2011) Anti-allodynic and anti-hyperalgesic effects of ceftriaxone in streptozocin-induced diabetic rats. Neurosci Lett 491:23–25
Hanigan MH, Devarajan P (2003) Cisplatin nephrotoxicity: molecular mechanisms. Cancer Ther 1:47
Hassan HA, Edrees GM, El-Gamel EM, El-sayed EA (2014) Amelioration of cisplatin-induced nephrotoxicity by grape seed extract and fish oil is mediated by lowering oxidative stress and DNA damage. Cytotechnology 66:419–429
Ibrahim A, Eldaim MAA, Abdel-Daim MM (2016) Nephroprotective effect of bee honey and royal jelly against subchronic cisplatin toxicity in rats. Cytotechnology 68:1039–1048
Jamieson ER, Lippard SJ (1999) Structure, recognition, and processing of cisplatin− DNA adducts. Chem Rev 99:2467–2498
Kalkanis JG, Whitworth C, Rybak LP (2004) Vitamin E reduces cisplatin ototoxicity. Laryngoscope 114:538–542
Kawai Y, Satoh T, Hibi D, Ohno Y, Kohda Y, Miura K, Gemba M (2009) The effect of antioxidant on development of fibrosis by cisplatin in rats. J Pharmacol Sci 111:433–439
Koracevic D, Koracevic G, Djordjevic V, Andrejevic S, Cosic V (2001) Method for the measurement of antioxidant activity in human fluids. J Clin Pathol 54:356–361
Kruidering M, Van De Water B, De Heer E, Mulder GJ, Nagelkerke JF (1997) Cisplatin-induced nephrotoxicity in porcine proximal tubular cells: mitochondrial dysfunction by inhibition of complexes I to IV of the respiratory chain. J Pharmacol Exp Ther 280:638–649
Lausen K (1972) Creatinine assay in the presence of protein with LKB 8600 reaction rate Analyser. Clin Chim Acta 38:475–476
Leonetti C, Biroccio A, Gabellini C, Scarsella M, Maresca V, Flori E, Bove L, Pace A, Stoppacciaro A, Zupi G (2003) α-Tocopherol protects against cisplatin-induced toxicity without interfering with antitumor efficacy. Int J Cancer 104:243–250
Liu H, Baliga R (2003) Cytochrome P450 2E1 null mice provide novel protection against cisplatin-induced nephrotoxicity and apoptosis. Kidney Int 63:1687–1696
Mehany HA, Abo-youssef AM, Ahmed LA, Arafa E-SA, El-Latif HAA (2013) Protective effect of vitamin E and atorvastatin against potassium dichromate-induced nephrotoxicity in rats. Beni-Suef Univ J Basic Appl Sci 2:96–102
Mihara M, Uchiyama M (1978) Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal Biochem 86:271–278
Miller RP, Tadagavadi RK, Ramesh G, Reeves WB (2010) Mechanisms of cisplatin nephrotoxicity. Toxins 2:2490–2518
Nazıroǧlu M, Karaoğlu A, Aksoy AO (2004) Selenium and high dose vitamin E administration protects cisplatin-induced oxidative damage to renal, liver and lens tissues in rats. Toxicology 195:221–230
Nishikimi M, Appaji N, Yagi K (1972) The occurrence of superoxide anion in the reaction of reduced phenazine methosulfate and molecular oxygen. Biochem Biophys Res Commun 46:849–854
O’Dwyer PJ, Stevenson JP, Johnson SW (1999) Clinical status of cisplatin, carboplatin, and other platinum-based antitumor drugs. In: Cisplatin, B. L. (Ed.), Cisplatin: chemistry and biochemistry of a leading anticancer drug, 31–69
Paglia DE, Valentine WN (1967) Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J Lab Clin Med 70:158–169
Palipoch S, Punsawad C, Koomhin P, Suwannalert P (2014) Hepatoprotective effect of curcumin and alpha-tocopherol against cisplatin-induced oxidative stress. BMC Complement Altern Med 14:111
Park MS, De Leon M, Devarajan P (2002) Cisplatin induces apoptosis in LLC-PK1 cells via activation of mitochondrial pathways. J Am Soc Nephrol 13:858–865
Perry TR, Schentag JJ (2001) Clinical use of ceftriaxone. Clin Pharmacokinet 40(9):685–694
Ramesh G, Reeves WB (2002) TNF-α mediates chemokine and cytokine expression and renal injury in cisplatin nephrotoxicity. J Clin Invest 110:835–842
Ramesh G, Reeves WB (2004) Inflammatory cytokines in acute renal failure. Kidney Int 66:S56–S61
Rothstein JD, Patel S, Regan MR, Haenggeli C, Huang YH, Bergles DE, Jin L, Hoberg MD, Vidensky S, Chung DS (2005) β-Lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature 433:73–77
Siddik ZH (2003) Cisplatin: mode of cytotoxic action and molecular basis of resistance. Oncogene 22:7265–7279
Stojiljkovic N, Ilic S, Veljkovic M, Todorovic J, Mladenovic M (2018) α-Tocopherol reduces morphological changes and oxidative stress during gentamicin-induced acute renal failure. Bull Exp Biol Med 164:442–445
Tahan G, Aytac E, Aytekin H, Gunduz F, Dogusoy G, Aydin S, Tahan V, Uzun H (2011) Vitamin E has a dual effect of anti-inflammatory and antioxidant activities in acetic acid–induced ulcerative colitis in rats. Can J Surg 54:333–338
Thadhani RP, Pascual M, Bonventre JV (1996) Acute renal failure. N Engl J Med 334:1448–1460
Townsend DM, Deng M, Zhang L, Lapus MG, Hanigan MH (2003) Metabolism of cisplatin to a nephrotoxin in proximal tubule cells. J Am Soc Nephrol 14:1–10
Townsend DM, Tew KD, He L, King JB, Hanigan MH (2009) Role of glutathione S-transferase pi in cisplatin-induced nephrotoxicity. Biomed Pharmacother 63:79–85
Traber MG, Stevens JF (2011) Vitamins C and E: beneficial effects from a mechanistic perspective. Free Radic Biol Med 51:1000–1013
Wang D, Lippard SJ (2005) Cellular processing of platinum anticancer drugs. Nat Rev Drug Discov 4:307–320
Wefers H, Sies H (1988) The protection by ascorbate and glutathione against microsomal lipid peroxidation is dependent on vitamin E. FEBS J 174:353–357
Weijl N, Elsendoorn T, Lentjes E, Hopman G, Wipkink-Bakker A, Zwinderman A, Cleton F, Osanto S (2004) Supplementation with antioxidant micronutrients and chemotherapy-induced toxicity in cancer patients treated with cisplatin-based chemotherapy: a randomised, double-blind, placebo-controlled study. Eur J Cancer 40:1713–1723
Whitehead T, Bevan E, Miano L, Leonardi A (1991) Defects in diagnostic kits for determination of urate in serum. Clin Chem 37:879–881
Yilmaz HR, Iraz M, Sogut S, Ozyurt H, Yildirim Z, Akyol O, Gergerlioglu S (2004) The effects of erdosteine on the activities of some metabolic enzymes during cisplatin-induced nephrotoxicity in rats. Pharmacol Res 50:287–290
Yılmaz N, İlhan S, Nazıroğlu M, Oktar S, Nacar A, Arıca V, Tutanç M (2011) Ceftriaxone ameliorates cyclosporine A-induced oxidative nephrotoxicity in rat. Cell Biochem Funct 29:102–107
Yoshiyama Y, Yazaki T, Beauchamp D, KANKE M (1998) Protective effect of ceftriaxone against the nephrotoxicity of isepamicin administered once daily in rats. Biol Pharm Bull 21:520–523
Younan SM, Rashed LA (2013) Protective effect of vitamin E on nerve conduction and dorsal root ganglia against cisplatin-induced peripheral neurotoxicity in rats. Med J Cairo Univ 81:145–157
Zamble DB, Lippard SJ (1995) Cisplatin and DNA repair in cancer chemotherapy. Trends Biochem Sci 20:435–439
Acknowledgments
The authors would like to thank the Deanship of Scientific Research at King Saud University for funding this work through Research Group no. RGP-018.
Funding
This work was supported by the Deanship of Scientific Research at King Saud University, Saudi Arabia (Grant No: RGP-018).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The Research Ethical Committee at Suez Canal University approved our experimental protocol (approval no. 20147). All animal stress conditions were taken into consideration and hardly avoided.
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Responsible editor: Philippe Garrigues
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdel-Daim, M.M., Aleya, L., El-Bialy, B.E. et al. The ameliorative effects of ceftriaxone and vitamin E against cisplatin-induced nephrotoxicity. Environ Sci Pollut Res 26, 15248–15254 (2019). https://doi.org/10.1007/s11356-019-04801-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-019-04801-2








