Abstract
Purpose
Our intent was to identify whether cerebrovascular CO2 reactivity in diabetic patients is a risk factor for postoperative cognitive dysfunction after coronary artery bypass graft (CABG) surgery.
Methods
One hundred twenty-four diabetic patients undergoing elective CABG were studied and analyzed. Diabetic patients were divided into three groups: normal CO2 reactivity group (above 5%/mmHg), medium CO2 reactivity group (between 5 and 3%/mmHg), or impaired CO2 reactivity group (below 3%/mmHg). After the induction of anesthesia and before the start of surgery, cerebrovascular CO2 reactivity was measured for all patients. Hemodynamic parameters (arterial and jugular venous blood gas values) were measured during cardiopulmonary bypass. All patients underwent a battery of neurological and neuropsychological tests the day before surgery, 7 days after surgery, and 6 months after surgery.
Results
At 7 days, the rate of cognitive dysfunction in the impaired CO2 group was higher than in the other three groups (normal, 30%; medium, 25%; impaired, 57%; *P < 0.01 compared with the other groups). In contrast, at 6 months postoperatively, no significant difference in the rate of cognitive dysfunction was found among the three groups. Age, hypertension, CO2 reactivity, the duration for which jugular venous oxygen saturation (SjvO2) was less than 50%, ascending aorta atherosclerosis, diabetic retinopathy, and insulin therapy were independent predictors of short-term cognitive dysfunction in diabetic patients, and HbA1c, diabetic retinopathy, and insulin therapy were independent predictors of long-term cognitive dysfunction in diabetic patients.
Conclusions
We found that impaired cerebrovascular CO2 reactivity was associated with postoperative short-term cognitive dysfunction in diabetic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central nervous system (CNS) complications are a major cause of morbidity and mortality after cardiac surgery [1–4]. In fact, neuropsychological dysfunction after cardiopulmonary bypass (CPB) has been reported in as many as 79% of patients during the early postoperative period [2–5].
It is widely known that the presence of diabetes mellitus is a risk factor for stroke and cognitive dysfunction after cardiac surgery [2–5]. One possible mechanism of the more frequent occurrence of postoperative cognitive change in diabetic patients is reportedly their abnormal cerebral autoregulation during CPB. Croughwell et al. [6] reported that cerebral blood flow (CBF) in diabetic patients was constant despite an increase in temperature from 27° to 37°C, in contrast to an 83% CBF increase in nondiabetic patients during the rewarming period. In previous studies, we [7–12] and others [6] found that reduced jugular venous oxygen saturation (SjvO2 below 50%: estimated by the balance of cerebral oxygen supply and demand), was closely associated with short-term cognitive dysfunction in elderly or diabetic patients. Moreover, we [9] and Croughwell et al. [6] showed that diabetic patients more frequently experienced reduced SjvO2 during CPB.
Diabetic patients have impaired cerebrovascular CO2 reactivity, this being one of the factors related to reduced SjvO2 during CPB [13, 14]. Kessler et al. [15] showed that reduced cerebral vasomotor reactivity was a strong predictor for the occurrence of postoperative confusion. Thus, we hypothesized that reduced cerebrovascular CO2 reactivity in diabetic patients may be one of the risk factors for postoperative cognitive dysfunction after cardiac surgery. One of our recent studies identified the importance of the presence of preoperative depression on postoperative cognitive dysfunction [16]. However, no previous study has examined whether cerebrovascular CO2 reactivity in diabetic patients is a risk factor for postoperative cognitive dysfunction after cardiac surgery.
The purpose of this study, therefore, was to identify whether cerebrovascular CO2 reactivity in diabetic patients was associated with the risk of postoperative cognitive dysfunction after coronary artery bypass graft (CABG) surgery in diabetic patients.
Methods
Study population
A total of 131 diabetic patients scheduled for elective CABG were identified, 129 of whom agreed to participate in this study. All protocols used in this study were approved by the Ethics Committee of our institution, and written informed consent was obtained from all patients.
Preexisting diagnosis of diabetes mellitus was determined by a chart diagnosis of type 2 diabetes, and current hyperglycemic therapy, including diet, oral medications, or insulin therapy, was noted. Duration of disease was based on the time of initiation of medical therapy. Renal failure was defined by a creatinine concentration >2.0 mg/dl. Prior stroke was determined by a history of ischemic cerebrovascular disease with symptomatic neurological disorders and confirmed by preoperative brain computed tomography and magnetic resonance imaging (MRI). Presence of moderate to severe atherosclerotic lesions in the ascending aorta or carotid artery stenosis were diagnosed by preoperative ultrasonography and MRI. Major neurological defects were defined as clinical evidence of any combination of focal cerebral infarction, including hemiparesis, visual or gait disturbances, mental status changes (confusion, agitation, inability to interact with others), or a combination of these.
Operative procedure
All patients received diazepam (10 mg orally) 1 h before anesthesia. Anesthesia was induced with 0.2 mg/kg midazolam, 20 μg/kg fentanyl, and 0.2 mg/kg vecuronium, followed by tracheal intubation. After induction of anesthesia, a pulmonary arterial catheter (Vigilance; Swan-Ganz CCO Thermodilution Catheter; Baxter, Irvine, CA, USA) was inserted through the right internal jugular vein. For continuous monitoring of jugular venous oxygen saturation (SjvO2), a 4-Fr. fiberoptic oximetry catheter (dual-lumen oximetry catheter; Baxter) was inserted into the right jugular bulb using a modified Seldinger technique. This catheter was connected to an analysis system (Explorer system; Baxter) and calibrated in vivo by aspirating blood through the catheter. The position of the jugular bulb catheter was verified by standard radiography, and the catheter was repositioned until correctly situated (catheter tip cranial to the line extending from the atlanto-occipital joint space and caudal to the lower margin of the orbit). SjvO2 data were obtained and processed in a monitor–computer interface and displayed and stored every 5 s with an Apple computer (Apple Computer, Cupertino, CA, USA) [9].
The partial pressures of arterial and jugular venous blood gases were analyzed using Stat Profile Ultima (NOVA Biomedical, Boston, MA, USA) and CO oximeter (OSM3, HemoximeterR; Radiometer, Copenhagen, Denmark). All patients were ventilated with oxygen (50%) and nitrogen (50%). End-tidal CO2 was monitored (Ultima; Datex, Helsinki, Finland) and maintained between 35 and 40 mmHg. Following anesthesia induction, 5–10 mg/kg/h propofol was infused using a syringe pump and was continued until the patients arrived in the intensive care unit. Muscular relaxation was achieved by intermittent administration of vecuronium. No volatile anesthetic was administered. The tympanic temperature was continuously monitored by Mon-a-Therm (Mallinckrodt, St. Louis, MO, USA). PaO2 was maintained at 150–250 mmHg during the study.
The CPB was primed with a crystalloid, nonglucose-containing solution, and a nonpulsatile pump flow rate of 2.2–2.5 l/min/m2 was maintained. A membrane oxygenator and a 40-μm arterial line filter were used, and PaCO2, uncorrected for temperature, was adjusted to normocapnic levels (35–40 mmHg) by varying fresh gas flow to the membrane oxygenator (alpha-stat regulation). Target tympanic temperatures were 34.5°–36.0°C. The limit on maximal inflow temperature was set at 37.5°C. Hematocrit during CPB was maintained at >20% using blood transfusions as necessary. Phenylephrine infusions were used during CPB to maintain mean arterial pressure (MAP) at 50–80 mmHg. Insulin infusions were used during CPB to maintain blood sugar between 100 and 200 mg/dl. Distal and proximal coronary anastomoses were performed during a single aortic cross-clamp.
Hemodynamic parameters and arterial and jugular venous blood gases were measured at different time points, as previously described in detail [8]. The presence or absence of carotid artery stenosis, defined as narrowing >50% [7], was confirmed by preoperative ultrasonography and MRI. The presence of atherosclerotic lesions in the ascending aorta, defined as atherosclerotic lesions ≥3.0 mm thick with diffuse irregularities, large mobile or protruding atheromata, ulcerated plaques, or thrombi [7], was confirmed by intraoperative epiaortic ultrasonography.
Assessment of CO2 reactivity
Measurement of CO2 reactivity was performed during a stable hemodynamic period after the induction of anesthesia and before the start of surgery (approximately 15–20 min after the induction of anesthesia). A 2.5-MHz pulsed TCD probe was attached to the patient’s head at the right or left temporal window, and mean blood flow velocity in the middle cerebral artery (V mca) was measured continuously (SONOS 5500, 2.5 MHz transducer; Hewlett Packard, Andover, MA, USA). After the signals were identified at a depth of 45–60 mm, the probe was fixed using a probe folder so as not to change the insonating angle. The V mca value at end-expiration was recorded. After the measurement of baseline V mca and cardiovascular hemodynamic values, partial end-tidal CO2 pressure (PetCO2) was increased by reducing the ventilatory frequency by 2–5 breaths/min; this resulted in an increase in PetCO2 by approximately 6–9 mmHg within several minutes. All measurements were repeated when PetCO2 increased and remained stable for 5–10 min.
To confirm the accuracy of PetCO2 as an indicator of arterial CO2, arterial CO2 and PetCO2 were simultaneously measured in several patients, and an excellent correlation was found between PetCO2 and arterial CO2 in these patients (data not shown).
The cerebral vasodilatory response to hypercapnia in each patient was calculated as the percentage change in V mca (relative CO2 reactivity: percentage of baseline V mca/mmHg) per millimeter of mercury change in PaCO2 using the following formula [14]:
where ΔV mca is the difference between the flow velocity after PaCO2 elevation and the baseline flow velocity, and ΔPaCO2 is the difference between the final and baseline PaCO2.
V mca was calculated for all study participants using the following formula [13]:
Based on our previous study [13], we divided the diabetic patients into three groups: normal CO2 reactivity group (above 5%/mmHg), medium CO2 reactivity group (between 5 and 3%/mmHg), and impaired CO2 reactivity group (below 3%/mmHg).
Neurological and neuropsychological assessments
All patients underwent a battery of neurological and neuropsychological tests on the day before the operation, repeated at 7 days and at 6 months after the surgery. These tests were administered by trained specialists, and intra- and interobserver validity was ensured. The neuropsychological portion of the study design followed the consensus statements on the assessment of central nervous system (CNS) disorders after cardiac surgery [17]. Cognitive functioning was assessed using the following tests: (1) mini-mental state examination, (2) Rey auditory verbal learning test, (3) trail-making test (part A), (4) trail-making test (part B), (5) digit span forward, and (6) grooved pegboard.
Statistical analysis
All data are expressed as mean ± SD. After the study was performed, we evaluated the sample size. On the basis of our previous study [7], we considered a 20% reduction in cognitive function to be clinically important. The sample size provided 80% power to detect a 20% difference between diabetic patients with and without insulin therapy with a 5% probability of a type I error. To obtain an indicator of overall outcome, significant impairment was defined as a decline from preoperative testing of more than 1 SD on more than 20% of test measures (at least 2 of 6).
The data were examined by the Bartlett test to determine whether the variance was normally distributed between groups. Univariate comparisons between the three groups were performed using the chi-square test for dichotomous variables and analysis of variance (ANOVA) for ordered categorical and continuous variables. The latter analyses were performed nonparametrically when regression residuals suggested that the model fit was poor. Stepwise logistic regression was used to choose a best set of independent predictors of both short-term and long-term cognitive impairment. Variables entered into the initial logistic models were those with a univariate probability value of P < 0.2. The final model included all variables with an independent significant level of P < 0.1. The quality of the fit of the logistic model was tested with the Hosmer and Lemeshow goodness-of-fit test.
Statistical significance was set at P < 0.05. All calculations were performed on an Apple computer with SPSS (SPSS, Chicago, IL, USA) and Stat View 5.0 software packages (Abacus Concepts, Berkeley, CA, USA).
Results
All patients had easily detectable MCA flow velocities for assessment of CO2 reactivity. We were unable to perform neuropsychological assessments for one diabetic patient at 6 months after the surgery because the patient died within 6 months of the operation. Two diabetic patients (excluding patients with major neurological defects) had incomplete cognitive data, and 1 diabetic patient refused follow-up. Major neurological defects [defined as clinical evidence of focal cerebral infarction including hemiparesis, visual or gait disturbances, mental changes (confusion, agitation, inability to make contact with other people), or a combination of these] were observed in 3 diabetic patients after the operation. We thus performed neuropsychological assessments on 124 diabetic patients.
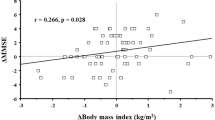
Table 1 shows the demographic data of the three groups. There were significant differences in age, weight, duration of SjvO2 ≤ 50%, HbA1c, fasting blood sugar (FBS), and insulin therapy among the three groups. Figure 1 shows the relationship between CO2 reactivity and duration of SjvO2 ≤ 50% during CPB; there was a close relationship between these two variables.
Table 2 shows the rate of cognitive dysfunction at 7 days and 6 months after the operation in the three groups. At 7 days, the rate of cognitive dysfunction in the impaired CO2 group was higher than in the other two groups (normal, 30%; medium, 25%; impaired, 57%; *P < 0.01 compared with the other groups). In contrast, no significant difference in the rate of cognitive dysfunction was found among the three groups at 6 months postoperatively.
Table 3 shows the independent predictors of cognitive dysfunction at 7 days or 6 months after cardiac surgery in diabetic patients. Age, hypertension, CO2 reactivity, duration of SjvO2 ≤ 50%, ascending aorta atherosclerosis, diabetic retinopathy, and insulin therapy were independent predictors of short-term cognitive dysfunction in diabetic patients, and HbA1c, diabetic retinopathy, and insulin therapy were independent predictors of long-term cognitive dysfunction in diabetic patients.
Discussion
The principal findings of this study were as follows: (1) reduced SjvO2 values during CPB were directly related to reduced cerebrovascular CO2 reactivity; and (2) reduced cerebrovascular CO2 reactivity was associated with short-term postoperative cognitive dysfunction.
Many studies have shown that diabetes is one of the key factors associated with postoperative cognitive dysfunction in diabetic patients undergoing cardiac surgery [1–6]. In fact, Hogue et al. [1] and Newman et al. [5] showed that diabetes was an independent predictor of postoperative neurological complications. One possible cause of postoperative cognitive dysfunction in diabetic patients is thought to be related to their impaired cerebrovascular circulatory and vasodilatory reserves. In a series of our studies [7, 10–12], we found that diabetic patients had a reduced SjvO2 during CPB. This reduced SjvO2 was associated with their cerebrovascular CO2 reactivity. During these previous studies, however, we did not examine the relationship between cerebrovascular CO2 reactivity and postoperative cognitive dysfunction in diabetic patients. The present study showed that reduced cerebrovascular CO2 reactivity in diabetic patients was associated with short-term cognitive dysfunction postoperatively.
Kessler et al. [15] examined the relationship between vasomotor reactivity and postoperative confusion states, and showed that reduced vasomotor reactivity was a strong predictor for the occurrence of postoperative confusion. They speculated that the etiology of this postoperative confusion is the critical, although temporary, reduction in brain perfusion resulting from fluctuations of systemic blood flow, which may induce reversible neuronal damage. The findings of Kessler et al. [15] suggest that cerebrovascular CO2 reactivity may be associated with postoperative cognitive dysfunction in diabetic patients. Our findings are consistent with their results.
Reduction of cerebrovascular CO2 reactivity in diabetic patients indicates the probable inability of the cerebral vasculature to meet oxygen demand and supply, especially under hypotensive conditions. Stratton et al. [18] reported that, in patients with type 2 diabetes, the risk of diabetic vascular complications was strongly associated with previous hyperglycemia. Pallas and Larson [19] noted that hyperglycemia led to impaired vascular function through endothelial cell dysfunction. The pathway that appears most affected by the diabetic state is that of nitric oxide. Loss of this pathway is accompanied by a loss of responsiveness to PaCO2 and by a lack of autoregulation related to the flow–pressure relationship. Although we did not demonstrate that the reduced SjvO2 values during CPB were directly caused by impaired CO2 reactivity in this study, we found a close relationship between HbA1c, indicative of previous hyperglycemic control, and reduced cerebrovascular CO2 reactivity (Fig. 1). From the aforementioned previous studies and from the present findings, we propose that the mechanisms for short-term cognitive dysfunction are associated with cerebral desaturation during the perioperative period, this cerebral desaturation being attributable to the impaired cerebral autoregulation in diabetic patients.
With regard to the factors related to long-term cognitive dysfunction, HbA1c, diabetic retinopathy, and insulin therapy were associated with short-term and long-term cognitive dysfunction in diabetic patients. This result is consistent with those of our previous report [7]. It is not known why cerebrovascular CO2 reactivity is not a predictor for long-term postoperative cognitive dysfunction. A possible cause for this, as has been mentioned in many previous studies, is that there are differential risk factors for short-term and long-term cognitive dysfunction [1, 4, 7]. Hypotension, cerebral desaturation as estimated by SjvO2, and use of sedative agents may be related to short-term cognitive dysfunction, whereas the presence of ascending aorta atherosclerosis or carotid artery stenosis may be related to long-term cognitive dysfunction. The implication of this finding for clinical practice is that physicians must be vigilant about maintaining adequate systemic and cerebral hemodynamics during the perioperative period to meet cerebral oxygen demand and supply.
We did not identify any relationship between postoperative cognitive dysfunction and ascending aorta atherosclerosis or carotid artery stenosis at 6 months after surgery. Several reports have shown that ascending aorta atherosclerosis and carotid artery stenosis represent major factors associated with cognitive dysfunction. As described in our previous report, the incidence of these diseases may have affected our results.
In this study, we divided the diabetic patients into three groups depending on CO2 reactivity. It is uncertain whether this division is really valid. However, our previous studies indicated that CO2 reactivity below 3%/mmHg is shown to be “an impaired response” to increased or decreased CO2 even under the influence of anesthetic agents that affect CO2 reactivity [13].
In conclusion, we found that impaired cerebrovascular CO2 reactivity was associated with postoperative short-term cognitive dysfunction in diabetic patients, and that impaired CO2 reactivity induced a reduction of SjvO2 during CPB.
References
Hogue CW, Murphy SF, Schechtman KB, Davila-Roman VG. Risk factors for early or delayed stroke after cardiac surgery. Circulation. 1999;100:642–7.
Newman MF, Wolman R, Kanchuger M, Marschall K, Mora-Mangano C, Roach G, Smith LR, Aggarwal A, Nussmeier N, Herskowitz A, Mangano DT. Multicenter prospective stroke risk index for patients undergoing coronary artery bypass graft surgery. Circulation. 1996;94(suppl II):74–80.
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K, Graham SH, Ley C. Adverse cerebral outcomes after coronary bypass surgery. N Engl J Med. 1996;335:1857–63.
Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344:395–402.
Newman MF, Croughwell ND, Blumenthal JA, Lowry E, White WD, Spillane W, Davis RD Jr, Glower DD, Smith LR, Mahanna EP. Predictors of cognitive decline after cardiac operation. Ann Thorac Surg. 1995;59:1326–30.
Croughwell N, Lyth M, Quill TJ, Newman M, Greeley WJ, Smith LR, Reves JG. Diabetic patients have abnormal cerebral autoregulation during cardiopulmonary bypass. Circulation. 1990;82(suppl):IV407–12.
Kadoi Y, Saito S, Fujita N, Goto F. Risk factors for cognitive dysfunction after coronary artery bypass graft surgery in patients with type 2 diabetes. J Thorac Cardiovasc Surg. 2005;129:576–83.
Kadoi Y, Saito S, Goto F, Fujita N. Decrease in jugular venous oxygen saturation during normothermic cardiopulmonary bypass predicts short-term postoperative neurologic dysfunction in elderly patients. J Am Coll Cardiol. 2001;38:1450–5.
Kadoi Y, Saito S, Kawahara F, Goto F, Owada R, Fujita N. Jugular venous bulb oxygen saturation in patients with preexisting diabetes mellitus or stroke during normothermic cardiopulmonary bypass. Anesthesiology. 2000;92:1324–9.
Kadoi Y, Saito S, Goto F, Someya T, Kamiyashiki S, Fujita N. Time course of changes in jugular venous oxygen saturation during hypothermic or normothermic cardiopulmonary bypass in patients with diabetic mellitus. Acta Anaesthesiol Scand. 2001;45:858–62.
Kadoi Y, Saito S, Yoshikawa D, Goto F, Fujita N, Kunimoto F. Increasing mean arterial blood pressure has no effect on jugular venous oxygen saturation in insulin-dependent patients during tepid cardiopulmonary bypass. Anesth Analg. 2002;95:266–72.
Kadoi Y, Saito S, Goto F, Fujita N. Slow rewarming has no effects on the decrease in jugular venous oxygen hemoglobin saturation and long-term cognitive outcome in diabetic patients. Anesth Analg. 2002;94:1395–401.
Kadoi Y, Hinohara H, Kunimoto F, Saito S, Ide M, Hiraoka H, Kawahara F, Goto F. Diabetic patients have an impaired cerebral vasodilatory response to hypercapnia under propofol anesthesia. Stroke. 2003;34:2399–403.
Miyoshi S, Morita T, Kadoi Y, Goto F. Analysis of the factors related to a decrease in jugular venous oxygen saturation in patients with diabetes mellitus during normothermic cardiopulmonary bypass. Surg Today. 2005;35:530–4.
Kessler C, Junge HM, Walker ML, Busack R, Albrecht DM, Ackeren KV. Reduced cerebral vasomotor reactivity as an indicator of postoperative confusion. Anaesthesia. 1997;52:433–7.
Kadoi Y, Kawauchi C, Ide M, Kuroda M, Takahashi K, Saito S, Mizutani A. Preoperative depression is a risk factor for postoperative short-term and long-term cognitive dysfunction in patients with diabetes mellitus. J Anesth. 2011;25:10–7.
Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59:1289–95.
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405012.
Pallas F, Larson DF. Cerebral blood flow in the diabetic patients. Perfusion. 1996;11:363–70.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kadoi, Y., Kawauchi, C., Kuroda, M. et al. Association between cerebrovascular carbon dioxide reactivity and postoperative short-term and long-term cognitive dysfunction in patients with diabetes mellitus. J Anesth 25, 641–647 (2011). https://doi.org/10.1007/s00540-011-1182-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1182-8