Abstract
Purpose
Failed airway is the anesthesiologist’s nightmare. Although conventional preoxygenation can provide time, atelectasis occurs in the dependent areas of the lungs immediately after anesthetic induction. Therefore, alternatives such as positive end-expiratory pressure (PEEP) and head-up tilt during preoxygenation have been explored. We compared the conventional preoxygenation technique (group C) with 20º head-up tilt (group H) and 5 cmH2O PEEP (group P) in non-obese individuals for non-hypoxic apnea duration.
Methods
A total of 45 patients were enrolled (15 in each group). After 5 min of preoxygenation, intubation was performed after induction of anesthesia with thiopentone and succinylcholine. After confirming the tracheal intubation by esophageal detector device and capnogram, all patients were administered vecuronium to maintain neuromuscular blockade and midazolam to prevent awareness. Post-induction, patients in all groups were left apneic in supine position with the tracheal tube exposed to atmosphere till the SpO2 dropped to 93% or 10 min of safe apnea was achieved.
Results
The demographic data were comparable. Non-hypoxic apnea duration was higher with group H (452 ± 71 s) compared to group C (364 ± 83 s, P = 0.030). Group P did not show significant increase in the duration of non-hypoxic apnea (413 ± 86 s). There were no adverse outcomes or events.
Conclusions
Preoxygenation is clinically and statistically more efficacious and by inference more efficient in the 20º head-up position than with conventional technique in non-obese healthy adults. Although application of 5 cmH2O PEEP provides longer duration of non-hypoxic apnea compared to conventional technique, it is not statistically significant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preoxygenation, which is the routine administration of 100% oxygen to the conscious individual before induction of general anesthesia, has now become an integral part of the safe conduct of general anesthesia [1, 2]. It is now described as a new “minimum standard of care” because the benefits incurred by it far outweigh the disadvantages [3]. Every individual receiving a general anesthetic is at potential risk for developing a “cannot intubate–cannot ventilate” situation following anesthetic induction. Building up of oxygen reserves assumes great significance as this provides a longer duration of non-hypoxic apnea should one be faced with an unanticipated difficult airway. The traditional period advised for preoxygenation has usually been 3–5 min, although mass spectrometry studies have shown that denitrogenation is almost 80% complete within 60 s of breathing 100% oxygen [4–6]. Studies have proved that by prolonging preoxygenation beyond 1 min or a few vital capacity breaths, the additional time it provided in terms of the ability to maintain hemoglobin arterial oxygen saturation (SpO2) in the face of prolonged apnea was very important [7, 8].
It is well documented that atelectasis occurs in the dependent areas of the lungs as soon as anesthesia is induced [9]. Gas-exchange abnormalities setting in after induction of anesthesia and muscle paralysis can be reversed to an extent by the application of positive end-expiratory pressure (PEEP) [10]. Studies have shown that application of PEEP during preoxygenation helps in increasing the duration of non-hypoxic apnea [11–13].
Despite adequate preoxygenation in the supine position, obese individuals have been found to be more prone for a shorter period of non-hypoxic apnea because they have reduced functional residual capacity (FRC). A decrease in FRC with change of position from the erect to supine position has also been well documented [14]. Studies have shown that placing the patient in a head-up position during preoxygenation results in prolongation of the duration of non-hypoxic apnea [15–18]. Drop in oxygen saturation during apnea can be slowed by placing these patients 45º head-up during preoxygenation [16]. However, this positioning can also create practical difficulties during intubation. Providing a lesser degree of head-up position may help to achieve intubation in the same position.
Although the beneficial effects of application of PEEP and the head-up position during preoxygenation are well documented, there are no studies reported in the literature that have compared the relative efficacy of these two techniques against conventional preoxygenation. This study compares the efficacy of these two techniques with conventional preoxygenation on the duration of non-hypoxic apnea.
Materials and methods
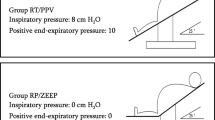
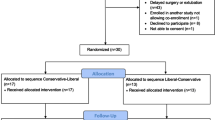
After obtaining approval from the Institutional Ethics Committee, Kasturba Hospital, 45 patients scheduled to undergo general anesthesia gave written informed consent to be recruited in this study. Individuals with significant cardiorespiratory or cerebrovascular disease, difficult intubation, history of epilepsy, requiring rapid sequence induction, body mass index >25 kg/m2, hemoglobin <8 g/dl, and those who had been non-ambulant for >24 h were excluded from the study. Patients were randomly assigned to one of the three groups by using random number draws. Oxygen was administered to all patients at 5 l/min for a period of 5 min using a Mapleson A breathing circuit with a tight-fitting face mask. In the control group (group C), patients were kept in supine position; in the PEEP group (group P), a 5 cmH2O PEEP valve was attached to the expiratory port; and in the head-up group (group H) patients were placed supine with the torso tilted 20º head-up from the hip upward.
The following parameters were monitored: electrocardiogram lead II and V5, noninvasive blood pressure, SpO2 monitored simultaneously from two pulse oximeters placed in two different digits (the Welch Allyn PIC50 biphasic defibrillator pulse oximeter and a second pulse oximeter as available in the operating location), arterial blood gases, end-tidal carbon dioxide (ETCO2), fraction of inhaled oxygen (FIO2), and end-tidal oxygen (ETO2). Hartmann’s solution (10 ml/kg) was administered after securing an intravenous access in the upper limb. In the same limb, the radial artery was cannulated and was kept locked with heparinized saline. Baseline values of heart rate, blood pressure, and SpO2 were recorded, and a sample of arterial blood (ABG1) was taken with the patient breathing room air. Patients were excluded from the study if ETO2 of 0.85 was not achieved at the end of the 5 min of preoxygenation. A sample of arterial blood was obtained after 5 min of preoxygenation (ABG2) and SpO2 recorded at this point. While continuing oxygenation, anesthesia was induced intravenously (IV) with fentanyl 2 μg/kg followed by thiopentone 5 mg/kg. Immediately after the patient lost consciousness, and without checking the ability to “mask ventilate,” succinylcholine was given in a dose of 2 mg/kg. Midazolam 2 mg IV was administered soon after to ensure amnesia during the apneic period following intubation. Sixty seconds later, intubation was performed by conventional laryngoscopy. Immediately following intubation, the patients in the head-up group were returned to supine position and PEEP was removed for patients in the PEEP group. The cuvette of a sidestream capnometer was attached via an angled connector to the end of the endotracheal tube. The endotracheal tube position was confirmed by visual observation of the tube passing between the vocal cords, the esophageal detector device (EDD), and the ETCO2 trace that was formed when the EDD was used. Then, the patient was paralyzed with vecuronium bromide in a dose of 0.08 mg/kg. Patients were left apneic with the endotracheal tube open to room air. The non-hypoxic apneic period was recorded as the time (in seconds) taken for the drop in arterial saturation to 93% in either of the two pulse oximeters or an apneic period of 10 min elapsed, whichever was earlier. An arterial blood gas sample was drawn at this point (ABG3). To keep the study conditions constant, patients were not ventilated either manually or mechanically during the study period. Following the period of study, patients were ventilated with 100% oxygen until the arterial oxygen saturation returned to baseline values. NIBP was recorded at 1-min intervals, and 3-mg boluses of mephentermine were given IV if mean pressure was <70 mmHg. Patients were questioned for any incidence of intraoperative awareness in the immediate postoperative period and 24 h after the surgery. Any other adverse events during the study period were also noted.
Statistical methods
The sample size was calculated for a power of 80% and an α error of 0.05 from a pilot study that we conducted with three patients in each group. The maximum standard deviation obtained for non-hypoxic apnea duration was 45 s (for the head-up group). The approximate per group sample size was calculated to be 14 using the formula: 22 s 2/d 2 + 1 where s is the maximum standard deviation among the three groups to be compared and d is the desired difference between means, which was considered to be 60 s for our study. We included 15 patients per group in this study.
The following statistical tests were used in the analysis of results. We applied one-way analysis of variance (ANOVA) for intergroup comparisons. The Tukey’s post hoc test was used for further analysis.
Results
Demographic data
Demographic parameters, hemoglobin values, ASA PS distribution, and smoking status were comparable between the groups (Table 1).
Safe duration of apnea
Drop in saturation to 93% before 10 min after induction occurred only in 12 of 15 patients in each group (Table 2). The duration of apnea was found to be statistically and clinically longer in the 20º head-up group (452 ± 71 s) as compared to the control group (364 ± 83 s). Although the duration of apnea was found to be clinically longer in PEEP group as compared to control group (413 ± 86 vs. 364 ± 83 s), the difference was not statistically significant.
Arterial blood gases
The partial pressure of arterial oxygen (PaO2), partial pressure of arterial carbon dioxide (PaCO2), and pH at the start of preoxygenation and following preoxygenation were comparable in the three groups (Tables 3, 4). However, at the end of the non-hypoxic apnea (or 10 min in some cases), a higher PaCO2 was observed in the 20º head-up group as compared to the control (P = 0.023; Table 4). Intergroup comparison of PaO2 and pH were comparable in the three groups (Tables 3, 4). The arterial blood gas values of three patients each (who did not desaturate below SpO2 of 93% at the end of 10 min of apnea) in the three groups are presented in Table 5.
Three patients in the head-up group developed hypotension necessitating treatment. None of the 45 patients experienced any episode of intraoperative awareness.
Discussion
The main aim of our study was to find the preoxygenation technique that could provide at least 60 s longer duration of non-hypoxic apnea than the other techniques. Three patients in each group maintained their saturation >93% until 10 min after induction. In the remaining 36 patients, the duration of non-hypoxic apnea was found to be statistically and clinically longer in the 20º head-up group (452 ± 71 s) as compared to the control group (364 ± 83 s) with a corresponding increase in the PaCO2 in the head-up group compared to the control group (66.52 ± 7.68 and 58.13 ± 9.26; P = 0.023). Although the duration of apnea was found to be clinically longer in the PEEP group as compared to the control group (413 ± 86 vs. 364 ± 83 s), the difference was not statistically significant. None of the 45 patients experienced any episode of intraoperative awareness. There were no major adverse events in any of the patients studied.
We evaluated for a non-hypoxic apnea duration of 10 min in our study, as the time to 90% twitch recovery at the adductor pollicis was found to be 9.3 ± 1.2 min with a succinylcholine dose of 1 mg/kg [19]. We planned to discontinue the study at this point as continuing further would have resulted in unreasonable CO2 buildup and unacceptable pH, which might have put the patients at risk. Because elective surgical patients were involved in the study and the methodology involved attempting intubation without attempting mask ventilation after induction and paralysis, there was a possibility of facing an unanticipated difficult airway. Hence, keeping patient safety in mind, we used succinylcholine as a muscle relaxant for aiding in laryngoscopy and intubation.
Three patients out of 15 in each group did not desaturate below the “safe limit” of SpO2 of 93% until the end of the study period of 10 min. Analysis of the remaining 12 patients in each group revealed that the duration of non-hypoxic apnea was significantly prolonged both statistically and clinically (approximately 90 s; P = 0.030) with the application of 20º head-up as compared to the conventional preoxygenation. This result explains why the PaCO2 was significantly higher in the head-up group compared to conventional preoxygenation (66.52 ± 7.68 and 58.13 ± 9.26 mmHg; P = 0.023) at the end of the study period. Our review of the literature showed three studies that have compared the effects of head-up (ranging from 20º to 60º) on the duration of non-hypoxic apnea in comparison with conventional preoxygenation and have drawn conclusions similar to ours [15, 17, 18]. Although the duration of non-hypoxic apnea was longer by 40 s with the 20º head-up position as compared to application of PEEP, we did not find a statistically significant difference between the two.
Application of PEEP during preoxygenation resulted in prolongation of non-hypoxic apnea by approximately 50 s compared to conventional preoxygenation. This finding, although clinically important, was not found to be statistically significant. There are few studies that compared the effects of application of PEEP of 6–10 cmH2O with conventional preoxygenation [12, 13, 20]. There was statistically and clinically significant increase in the duration of non-hypoxic apnea with PEEP compared to conventional preoxygenation in these studies. One notable difference in the methodology here is that patients in the PEEP group continued to receive PEEP with intermittent positive pressure ventilation with the mask for a duration of 5 min following induction and paralysis in their studies. As per our understanding, the objective of preoxygenation is to safeguard the patient against hypoxia in the event of inability to ventilate and/or intubate following induction of anesthesia and muscle paralysis. Therefore, the intention of our study was to determine whether the duration of non-hypoxic apnea could be usefully extended by the application of PEEP during preoxygenation. In essence, our study effectively simulated a “cannot intubate/cannot ventilate” situation. This change in methodology explains why our results were different from those of other such studies [12, 13, 20]. One study that evaluated the effect of PEEP with a methodology similar to ours, albeit in morbidly obese women, has shown results similar to ours [11].
Application of PEEP to awake patients can be discomforting, and hence we decided to use only 5 cmH2O PEEP, which was well tolerated by all the patients. Higher levels of continuous positive airway pressure (CPAP)/PEEP can also cause adverse hemodynamic effects. Because we used only 5 cmH2O CPAP/PEEP in our study, we did not encounter any hemodynamic disturbances. Patients in our study were intubated following succinylcholine and were not given positive pressure breaths before and immediately after intubation. Maintaining the 20º head-up tilt can exacerbate the hypotensive effects of anesthetic induction agents. In addition to preloading, we lowered the patient to the supine position immediately following tracheal intubation. Hypotension occurred in 3 of the 15 patients in the 20º head-up group.
Preoxygenation in a head-up position is believed to theoretically increase the risk of aspiration should regurgitation occur, although the risk of regurgitation per se is lower with the head-up position [18]. Increased difficulty in intubation can be encountered because of the unconventional position adopted, necessitating a footstool for facilitating intubation. Some anesthesiologists perceive that the head-up position provides better positioning of the head for optimal intubation and better access to the airway by gravitational retraction of the breast tissue in female patients. In our study, we did not encounter any difficulty in intubation, nor was any incident of regurgitation or aspiration noted. Arterial oxygen saturation and FRC have been found to decrease when obese patients assume a supine position; this may be further exacerbated by induction of anesthesia as a result of weakening of the tone of the diaphragm [21]. The same explanation might be true for non-obese patients, as evidenced by the results of our study.
Confirmation of tube position following intubation has been done by various techniques in different studies. Some of the techniques used include fibreoptic bronchoscopy, by providing a single positive pressure breath of lower volume, and by observing the capnographic trace. We believe that the use of positive pressure breaths could open up atelectatic areas, thereby interfering with our study conditions. We therefore confirmed correct placement of the endotracheal tube by using the modified EDD as it does not rely on use of positive pressure breaths for its performance. This method was additionally supported by visual observation of passage of the tube between the vocal cords and ETCO2 trace that appeared because of drawing some air from trachea while the EDD was applied. Our methodology thus provided controlled conditions aimed at avoiding alveolar recruitment in the immediate period following tracheal intubation.
The maximum PaCO2 noted was 82.5 mmHg and the minimum pH observed was 7.18 at the end of the study period, both of which were clinically acceptable as hyperventilation can correct these parameters immediately. Discontinuation of anesthetic agents after intubation for a variable period of up to 10 min might predispose to the risk of awareness under anesthesia. In the absence of target controlled infusion devices and bispectral index device (BIS) for preventing and monitoring awareness, we chose to administer 2 mg midazolam intravenously after intubation to all our patients. None of the patients reported awareness in the immediate postoperative period or 24 h later.
The main limitation to our study was that this was only single blinded, although the standardized anesthetic induction technique and observer-independent criteria for defining the duration of non-hypoxic apnea were used to limit possibility of bias.
Conclusion
In non-obese individuals, preoxygenation is clinically and statistically more efficacious and by inference more efficient in a 20º head-up position than either in supine position or with application of 5 cmH2O PEEP. Application of 5 cmH2O PEEP provides a clinically longer duration of non-hypoxic apnea, although this was not statistically significant.
References
Drummond GB, Park GR. Arterial oxygen saturation before intubation of the trachea. An assessment of oxygenation techniques. Br J Anaesth. 1984;56:987–93.
Thorpe CM, Gauntlett IS. Arterial oxygen saturation during induction of anaesthesia. Anaesthesia. 1990;45:1012–5.
Bell MD. Routine pre-oxygenation: a new ‘minimum standard’ of care? Anaesthesia. 2004;59:943–5.
Campbell IT, Beatty PC. Monitoring preoxygenation. Br J Anaesth. 1994;72:3–4.
Berthoud M, Read DH, Norman J. Pre-oxygenation—how long? Anaesthesia. 1983;38:96–102.
Russell GN, Smith CL, Snowdon SL, Bryson TH. Pre-oxygenation and the parturient patient. Anaesthesia. 1987;42:346–51.
Berthoud MC, Peacock JE, Reilly CS. Effectiveness of preoxygenation in morbidly obese patients. Br J Anaesth. 1991;67:464–6.
Valentine SJ, Marjot R, Monk CR. Preoxygenation in the elderly: a comparison of the four-maximal-breath and three-minute techniques. Anesth Analg. 1990;71:516–9.
Lundquist H, Hedenstierna G, Strandberg A, Tokics L, Brismar B. CT-assessment of dependent lung densities in man during general anesthesia. Acta Radiol. 1995;36:626–32.
Tokics L, Hedenstierna G, Strandberg A, Brismar B, Lundquist H. Lung collapse and gas exchange during general anesthesia: effects of spontaneous breathing, muscle paralysis, and positive end-expiratory pressure. Anesthesiology. 1987;66:157–67.
Cressey DM, Berthoud MC, Reilly CS. Effectiveness of continuous positive airway pressure to enhance pre-oxygenation in morbidly obese women. Anaesthesia. 2001;56:680–4.
Gander S, Frascarolo P, Suter M, Spahn DR, Magnusson L. Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg. 2005;100:580–4.
Herriger A, Frascarolo P, Spahn DR, Magnusson L. The effect of positive airway pressure during pre-oxygenation and induction of anaesthesia upon duration of non-hypoxic apnoea. Anaesthesia. 2004;59:243–7.
Nunn JF. Nunn’s applied respiratory physiology. 3rd ed. London: Butterworth Heinemann; 1987. p. 350–70.
Altermatt FR, Munoz HR, Delfino AE, Cortinez LI. Pre-oxygenation in the obese patient: effects of position on tolerance to apnoea. Br J Anaesth. 2005;95:706–9.
Baraka AS, Hanna MT, Jabbour SI, Nawfal MF, Sibai AA, Yazbeck VG, Khoury NI, Karam KS. Preoxygenation of pregnant and nonpregnant women in the head-up versus supine position. Anesth Analg. 1992;75:757–9.
Dixon BJ, Dixon JB, Carden JR, Burn AJ, Schachter LM, Playfair JM, Laurie CP, O’Brien PE. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology. 2005;102:1110–5.
Lane S, Saunders D, Schofield A, Padmanabhan R, Hildreth A, Laws D. A prospective, randomised controlled trial comparing the efficacy of pre-oxygenation in the 20 degrees head-up vs. supine position. Anaesthesia. 2005;60:1064–7.
Kopman AF, Zhaku B, Lai KS. The “intubating dose” of succinylcholine: the effect of decreasing doses on recovery time. Anesthesiology. 2003;99:1050–4.
Rusca M, Proietti S, Schnyder P, Frascarolo P, Hedenstierna G, Spahn DR, Magnusson L. Prevention of atelectasis formation during induction of general anesthesia. Anesth Analg. 2003;97:1835–9.
Pelosi P, Croci M, Calappi E, Mulazzi D, Cerisara M, Vercesi P, Vicardi P, Gattinoni L. Prone positioning improves pulmonary function in obese patients during general anesthesia. Anesth Analg. 1996;83:578–83.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ramkumar, V., Umesh, G. & Philip, F.A. Preoxygenation with 20º head-up tilt provides longer duration of non-hypoxic apnea than conventional preoxygenation in non-obese healthy adults. J Anesth 25, 189–194 (2011). https://doi.org/10.1007/s00540-011-1098-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1098-3