Abstract
Background
Apnea testing is an essential step in the clinical diagnosis of brain death. Current international guidelines recommend placement of an oxygen (O2) insufflation catheter into the endotracheal tube to prevent hypoxemia, but use of a continuous positive airway pressure (CPAP) valve may be more effective at limiting arterial partial pressure of O2 (PO2) reduction.
Methods
We performed a multicenter study assessing consecutive apnea tests in 14 intensive care units (ICUs) in two cities utilizing differing protocols. In one city, O2 catheters are placed and arterial blood gases (ABGs) performed at intervals determined by the attending physician. In the other city, a resuscitation bag with CPAP valve is attached to the endotracheal tube, and ABGs performed every 3–5 min. We assessed arterial PO2, partial pressure of carbon dioxide (PCO2), pH, and blood pressure at the beginning and termination of each apnea test.
Results
Thirty-six apnea tests were performed using an O2 catheter and 50 with a CPAP valve. One test per group was aborted because of physiological instability. There were no significant differences in the degree of PO2 reduction (−59 vs. −32 mmHg, p = 0.72), rate of PCO2 rise (3.2 vs. 3.9 mmHg per min, p = 0.22), or pH decline (−0.02 vs. −0.03 per min, p = 0.06). Performance of ABGs at regular intervals was associated with shorter test duration (10 vs. 7 min, p < 0.0001), smaller PCO2 rise (30 vs. 26 mmHg, p = 0.0007), and less pH reduction (−0.20 vs. −0.17, p = 0.0012). Lower pH at completion of the apnea test was associated with greater blood pressure decline (p = 0.006).
Conclusion
Both methods of O2 supplementation are associated with similar changes in arterial PO2 and PCO2. Performance of ABGs at regular intervals shortens apnea test duration and may avoid excessive pH reduction and consequent hemodynamic effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
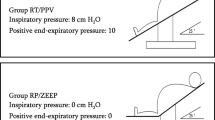
Apnea testing to document cessation of respiratory drive is an essential step in the clinical diagnosis of brain death [1–4]. International guidelines, including those of the American Academy of Neurology (AAN), recommend disconnection from mechanical ventilation with concomitant placement of a catheter into the endotracheal tube to deliver 100% oxygen (O2) at a flow rate of approximately 2–6 L/min (Fig. 1a) [1–3]. This method enables safe completion of apnea testing in the majority of cases [5–9]. Nevertheless, while the safety of apnea testing may have improved overtime with increasingly standardized approaches that incorporate appropriate precautions (e.g., pre-oxygenation), various complications such as hypoxemia, dysrhythmias, and hypotension still occur in a sizable proportion of patients [7–9]. Cases of iatrogenic pneumothorax have also been reported [10–13], which may be attributable to use of an insufflation catheter that is relatively large in relation to the inner diameter of the endotracheal tube, which in turn produces gas trapping, especially with comparatively high O2 flow rates [14, 15].
Alternative methods have been proposed to minimize the degree of lung de-recruitment and atelectasis, with resultant hypoxemia, that may occur during apnea testing. One common approach is to attach a continuous positive airway pressure (CPAP) valve to the opening of the endotracheal tube, using either a T-piece connector or a resuscitation bag to provide supplemental O2 at a flow rate of 10–15 L/min (Fig. 1b) [16–21]. Use of a resuscitation bag with CPAP valve has been reported in a relatively large clinical series to be effective at attenuating hypoxemia [19]. A prospective single-center study involving 20 brain-dead patients found use of a T-piece connector with CPAP valve to be associated with a less pronounced drop in the arterial partial pressure of O2 (PO2) compared with an O2 catheter [17]. However, this finding has not been confirmed in a larger and more heterogeneous patient population and has not been incorporated into major guideline documents [1–4].
We performed a multicenter, population-based cohort study of consecutive apnea tests performed in urban centers in the province of Alberta in order to compare the conventional O2 insufflation catheter method with use of a resuscitation bag with CPAP valve.
Methods
This study was performed as part of a Quality Improvement initiative by the Department of Critical Care Medicine at the University of Calgary. Based on criteria set out by the Alberta Research Ethics Community Consensus Initiative (available at www.aisolutions.ca), this study posed minimal risk to subjects and therefore did not require formal review by provincial research ethics boards.
In the province of Alberta, the vast majority of critically ill patients are cared for in either Calgary or Edmonton. Calgary has one neurosurgical center serving all of southern Alberta, with a total of six adult intensive care units (ICUs) and one pediatric ICU located at five hospitals. Edmonton has two neurosurgical centers servicing all of northern Alberta and the Northwest Territories and has six adult ICUs and one pediatric ICU located in four hospital complexes.
In both cities, written protocols for the diagnosis of brain death are in accordance with published Canadian Guidelines [4]. A checklist provided in the Canadian Guideline document, or a variation thereof, is regularly utilized in both cities. Apnea testing is performed only when the remainder of the neurological assessment is consistent with brain death and none of the following confounding factors are present: unresuscitated shock, temperature <34 °C, severe metabolic disturbances, significant peripheral nerve or muscle dysfunction that may account for unresponsiveness, or residual effects of drug intoxication or sedating drugs. It is also recommended that definitive clinical evaluation for brain death be delayed for at least 24 h after return of spontaneous circulation in the setting of hypoxic-ischemic encephalopathy following a cardiac arrest, since initially absent brainstem reflexes are known to sometimes return in this context [4].
In both cities, patients are pre-oxygenated for at least 10 min with 100% O2 and with positive end-expiratory pressure (PEEP) maintained at 5–15 mmHg. Ventilator settings are adjusted to achieve an arterial partial pressure of carbon dioxide (PCO2) of 35–45 mmHg. In Calgary, apnea tests are performed in accordance with AAN recommendations, using an O2 insufflation catheter with a diameter small enough to avoid occlusion of the endotracheal tube, with the flow set at 5–8 L/min [1]. In Edmonton, apnea tests are performed using a resuscitation bag with a CPAP valve, set at either 10 cm H2O or to match the preexisting PEEP level, whichever is higher. In Calgary, the timing of arterial blood gases (ABGs) is left to the discretion of the attending critical care physician, with the initial ABG usually obtained after 5–10 min of apnea. In Edmonton, ABGs are performed regularly every 3–5 min. As per national guidelines, apnea tests are considered consistent with brain death if patients do not breathe despite reaching each of the following criteria: pH ≤7.28, PCO2 ≥60 mmHg, and a PCO2 increment ≥20 mmHg relative to the baseline level [2]. Of note, these criteria are slightly different than AAN recommendations, which require either a PCO2 ≥60 mmHg or an increment ≥20 mmHg, with no specific pH criterion [1]. Criteria to terminate an apnea test included hypoxemia (PO2 <60 mmHg or a peripheral O2 saturation <90%), hypotension (systolic blood pressure <90 mmHg), or arrhythmias (tachyarrhythmias other than sinus tachycardia and second- or third-degree heart block).
ICUs across the province of Alberta share a common clinical information system (Meta-Vision; iMDsoft, Dedham, MA) that records minute-by-minute physiological data. This system has been gradually introduced across the province, beginning with ICUs in Calgary in 2012–2013, followed by ICUs in Edmonton in 2013–2014.
We identified consecutive apnea tests that were performed in Calgary since introduction of the provincial clinical information system, and in Edmonton since mid-2014. We determined the duration of each apnea test, the number and time interval of arterial blood gas (ABG) assessments; baseline arterial pH, PO2, and PCO2, and pH, PO2, and PCO2 at the time when criteria for brain death were met. We recorded mean arterial pressure and heart rate during the apnea test, as well as use of vasopressors or inotropes. Our primary outcome of interest was the reduction in PO2 during the apnea test, which we hypothesized would be less with use of the CPAP method [17], as well as the proportion of apnea tests needing to be aborted due to significant hypoxemia, hypotension, or arrhythmias, as defined above. Apart from preventing completion of the apnea test, thereby precluding a clinical diagnosis of brain death, these complications are important because they could lead to cardiac arrest if not rapidly reversed.
Secondary outcomes included the rates of PCO2 elevation and pH decline, changes in hemodynamic parameters, and development of pneumothoraces. We also sought to identify variables that are associated with changes in PO2, PCO2, pH, and blood pressure.
Continuous variables were expressed as medians with interquartile ranges and compared using Wilcoxon rank sum tests. Categorical variables were expressed as proportions and compared using Chi-square analysis or Fisher’s exact test, as appropriate. Mixed models using generalized estimating equations were developed to compare the effects of apnea testing methodology on changes in PO2, PCO2, pH, mean arterial pressure, and heart rate over time and to identify variables predictive of the magnitude of change. Such models are a variation of generalized linear models, which may be used to accommodate correlated, longitudinally measured data with repeated measures. Predictor variables with p <0.10 in univariate analysis were incorporated into multivariable analyses. Analyses were performed using SAS (version 9.3; Cary, NC). Figures were created using GraphPad Prism (Version 7; La Jolla, CA). P values <0.05 were considered statistically significant.
Results
The cohort consisted of 33 patients from Calgary, who underwent 36 apnea tests using the O2 insufflation technique and 44 patients from Edmonton, who underwent 50 apnea tests using the CPAP method. Baseline characteristics, including age, sex, weight, cause of brain injury, and temperature at the start of the apnea test, were similar between cities (Table 1). There were no significant differences in baseline PO2:FIO2 ratio, O2 index (fraction of inspired oxygen (FIO2) × mean airway pressure/PO2) and PCO2, but baseline arterial pH was slightly lower in Calgary patients, attributable to more patients having metabolic acidosis (p = 0.03). Heart rate, mean arterial pressure, and vasopressor use at the start of the apnea test were also similar between groups, although there was more use of milrinone in Calgary.
In Calgary, with the timing of ABGs left to the discretion of attending physicians, the median time interval between onset of the apnea test and an ABG meeting criteria for brain death was 10 (7–12) min, with an ABG performed a median of every 7 (5–9) min. In Edmonton, with a protocol stipulating routine performance of ABGs at set intervals, apnea tests were significantly shorter [7 (5–9) min; p = 0.0004], with ABGs performed more often [every 4 (3–5) min; (p <0.0001)]. The proportion of cases that had apnea tests longer than 10 and 15 min was significantly greater in Calgary (36 vs. 14%, p = 0.02 and 14 vs. 2%, p = 0.03, respectively).
Using the O2 insufflation technique, one out of 36 apnea tests (3%) needed to be discontinued because of hypoxemia and hypotension, but this patient had already reached pH and PCO2 levels sufficient to diagnose brain death. Using the CPAP technique, one out of 50 apnea tests (2%) needed to be discontinued because of hypoxemia, but the patient had again reached criteria to declare brain death. Two additional apnea tests in Edmonton were terminated prior to meeting pH criteria for declaration of brain death (pH 7.31 and 7.35, although PCO2 had risen by more than 20 mmHg in both cases), despite the absence of any overt physiological instability, for reasons that are unclear (both patients also underwent ancillary testing that was consistent with brain death).
With the O2 insufflation method, the PO2 changed a median of −59 (−143 to +3) mmHg, compared with −32 (−90 to 0) mmHg when the CPAP method was used [Table 2; β = 8.3 (−36.9 to 53.6), p = 0.72]. When the analysis was restricted to patients with baseline PO2:FIO2 ratio ≤300 mmHg or an O2 Index ≥4, there was again no statistically significant difference in the degree of PO2 reduction between the two groups (p = 0.68 and p = 0.47, respectively). Similarly, there was no difference when the PO2 reduction was divided by the duration of the apnea test (p = 0.66), or in the final PO2 at the time that criteria for brain death were met [305 (141–410) vs. 299 (173–433) mmHg, p = 0.63] (Table 2). The only baseline variable of those listed in Table 1 to be associated with a larger degree of PO2 reduction during apnea testing was higher baseline temperature [β = 32.6 (10.5–54.7), p = 0.004] (Fig. 2). There was a similar trend for greater patient weight [β = 0.9 (−0.1 to 1.8), p = 0.08]. After adjustment for these potential confounders, the method of apnea testing was still not associated with magnitude of PO2 reduction (p = 0.62).
With the O2 catheter method, the PCO2 increased by a median of 30 (25–35) mmHg, compared with 26 (24–28) mmHg using the CPAP method (p = 0.0007) (Table 2). However, this relationship was no longer statistically significant when adjusted for the duration of the apnea test, which was longer with the O2 catheter method (p = 0.21). When expressed as mmHg per min, the rate of PCO2 rise was slightly slower with the O2 catheter technique compared with the CPAP method, although the difference was not statistically significant [3.2 (2.2–5.0) mmHg per min vs. 3.9 (3.0–4.8) mmHg per min; p = 0.22]. Similarly, although the overall pH drop was larger with the O2 insufflation method [−0.20 (−0.22 to −0.17) vs. −0.17 (−0.19 to −0.16), p = 0.0012], this was no longer significant with adjustment for apnea test duration, and there was an opposing trend toward slower pH reduction with an O2 catheter compared with a CPAP valve [0.02 (0.02–0.03) vs. 0.03 (0.02–0.03) per min, p = 0.06] (Table 2). The only variable to be associated with a greater PCO2 increment was younger age [β = −0.2 (−0.3 to −0.1), p = 0.01]. After adjustment for patient age and duration of the apnea test, the O2 insufflation method was not associated with a significantly different rate of PCO2 rise (p = 0.15) or pH reduction (p = 0.17).
Heart rate did not change significantly during apnea testing in either city [median difference +1 (−3 to +5.5) vs. +1.5 (−1 to +5) beats per min; p = 0.99]. Mean arterial pressure decreased by a median of 8.5 (−18 to +1) mmHg with an O2 catheter, compared with only 1 (−8 to +5) mmHg with the CPAP method (p = 0.02). The mean arterial pressure at the time of meeting criteria for brain death was 85 (69–92) and 90 (83–105) mmHg, respectively (p = 0.03). The dose of vasopressor(s) was increased during 14% of apnea tests using an O2 catheter, compared with 2% using the CPAP method (p = 0.07). The magnitude of blood pressure reduction during the apnea test was associated with the degree of pH reduction (p = 0.03) (Fig. 3). After adjustment for the duration of the apnea test and pH reduction, the method of apnea testing was no longer associated with the degree of blood pressure reduction (p = 0.20).
Twenty-one apnea tests in Calgary (58%) and 32 in Edmonton (64%) were followed by a chest X-ray, and there was no pneumothorax detected in either group.
Discussion
In this “comparative effectiveness” study of two protocols for apnea testing in the diagnosis of brain death, we made the following observations: (1) Apnea tests only rarely needed to be discontinued because of physiological instability (hypoxemia, hypotension, or arrhythmias), regardless of the method of O2 supplementation; (2) Use of the CPAP method was associated with a slightly smaller reduction in PO2, but this difference was not statistically (or clinically) significant. This was true also among patients with more severe baseline hypoxemia; (3) Although there was no statistically significant difference in the rate at which PCO2 increased and pH decreased, the proportion of patients with relatively slow PCO2 increments (apnea tests requiring longer than 10–15 min) was larger with the O2 catheter method; (4) More frequent performance of ABGs at fixed intervals permits earlier completion of an apnea test, with less dangerous degrees of respiratory acidosis. Although we found no evidence of major complications associated with greater increments in PCO2, a lower pH at the completion of the apnea test was predictive of a greater drop in blood pressure; (5) The magnitude of PO2 reduction was associated higher body temperature, while the rate of PCO2 elevation was greater in younger patients.
Our finding that apnea tests only rarely need to be aborted, regardless of the method of O2 supplementation, is consistent with other recently published literature. In a single-center series of 228 patients, only 3% of patients who received O2 supplementation using an insufflation catheter required premature termination of the apnea test [3]. Similarly, in a series of 169 patients that underwent apnea testing with a resuscitation bag and PEEP valve, severe hypoxemia was encountered in only 3% of tests [18]. The incidence of major physiological derangements has likely decreased over time with increasing use of standardized protocols [6].
In a previous prospective study comparing three methods of apnea testing in 20 brain-dead patients, Levesque and colleagues reported that use of a T-piece setup with a CPAP valve was more effective at minimizing reductions in PO2 than the O2 catheter technique [17]. The trends in our study were in the same direction, although the absolute differences were smaller and not statistically significant. Our median reduction in PO2 using a resuscitation bag and CPAP valve was larger than the mean reduction reported by Levesque and colleagues (32 vs. 22 mmHg), while that using the O2 catheter technique was less pronounced (59 vs. 99 mmHg). The degree of de-recruitment and atelectasis over time with the O2 catheter method is likely to vary based on multiple factors, such as the O2 flow rate, the relative size of the catheter in relation to the endotracheal tube, and the presence of lung disease.
We found increased body temperature to be predictive of a greater drop in PO2. This observation has never previously been described during apnea testing and requires confirmation. Although lower systemic consumption of O2, with higher mixed venous oxygen levels, may be a contributing factor, hypothermia is generally not protective against hypoxemia. However, a previous animal study found that hypothermia might raise PO2 specifically in the setting of hypercapnia, with data suggesting that this may be in part because hypothermia attenuates the rightward shift of the oxygen-hemoglobin dissociation curve that occurs in the setting of acidemia [22]. Increasing body weight had a possible, albeit statistically insignificant effect on PO2 reduction during apnea testing. This is not surprising, since obesity reduces respiratory system compliance, with higher pleural pressure and lower lung volumes producing a predisposition to atelectasis [23, 24].
Our finding that the rate of PCO2 elevation was not significantly different based on the method of apnea testing is also consistent with previous literature [17]. However, there was a trend toward slower decline in pH with the O2 catheter method, and there were more patients requiring long periods of apnea before reaching the target PCO2 and pH. In some patients, the PCO2 rise was as low as 1 mmHg per min. It is possible that O2 insufflation into the distal trachea results in some degree of CO2 elimination, particularly at higher flow rates. Inadequate documentation in our database precluded the possibility of evaluating the relationship between O2 flow rate and PCO2 rise. If clinicians using the O2 catheter method encounter a relatively slow PCO2 rise, they should consider lowering the O2 flow rate. We found that younger age predicted a faster rise in PCO2. This finding may relate to higher metabolic rate and CO2 production in younger individuals.
The duration of apnea testing tended to be longer when ABGs were performed less frequently. When ABGs are performed at fixed intervals, it enables clinicians to estimate the rate of PCO2 rise during the apnea test and identify criteria for brain death as soon as possible once these are reached. This, in turn, avoids unnecessarily large degrees of PCO2 elevation and severe acidemia, which could conceivably result in unanticipated hemodynamic complications in some patients [5–8].
Although we did not find an association between longer apnea test duration and hemodynamic complications, there was a relationship between a lower pH at the end of the apnea test and a greater reduction in mean arterial pressure over time. In a previous study, apnea testing was performed with pulmonary artery catheters in situ, with some patients also having measurements of plasma concentrations of catecholamines. During apnea testing, levels of epinephrine and norepinephrine increased slightly, as did cardiac output, but these effects were significantly attenuated compared with a normal response [25]. The authors concluded that although mild PCO2 elevation and pH reduction are generally well tolerated, a blunted sympathetic response makes patients with brain death more vulnerable to hemodynamic effects resulting from severe hypercapnia and acidemia [25]. Major reduction in blood pressure precludes completion of an apnea test [1–3]. Although rare, cardiac arrest or imminent cardiac arrest has been described in the setting of apnea testing [7, 26]. Mild reduction in blood pressure during an apnea test is likely to be of limited clinical importance. Current guidelines recommend maintenance of a mean arterial pressure of 60–70 mmHg in brain-dead potential organ donors, but brief reductions below this threshold are unlikely to compromise graft function [27].
We did not encounter any pneumothoraces with either method of apnea testing. Based on our experience, as well as that in other large cohort studies, pneumothorax is likely to be a very rare event [5–8]. A recent systematic review of pneumothorax during apnea testing found that eight of 10 (80%) patients had an O2 flow rate ≥8 L/min, which is higher than guideline recommendations [10]. Institutional protocols should ensure that the O2 insufflation catheter is not inappropriately large for the diameter of the endotracheal tube and should limit the flow rate to ≤6–8 L/min.
The strengths of our study include the multicenter and population-based design, with inclusion of consecutive and diverse (including pediatric) patients, with availability of minute-by-minute physiological data. An important limitation is that the proportion of patients with severe baseline hypoxemia or very large doses of inotropes or vasopressors was relatively small. In such patients, a full apnea test is often not attempted, with clinicians instead opting to perform an ancillary test if all other criteria for brain death are met [1–4]. With a relatively modest sample size, our study may have lacked statistical power to detect a significant difference in the degree of PO2 reduction between the two apnea testing methods. Allocation to the two methods of apnea testing was not randomized, such that there may have been other unknown procedural differences between cities that were not recognized and assessed in this study.
In conclusion, apnea testing can be safely performed with both methods assessed in this study, including the O2 catheter technique that is recommended in major guideline documents [1–3]. Contrary to some previous research, we could not confirm the superiority of apnea testing using a CPAP valve [17]. We believe that clinicians should perform regular ABGs at fixed intervals of 3–5 min in order to avoid severe respiratory acidosis, and terminate the apnea test as soon as accepted criteria for brain death are met to help avoid significant hemodynamic complications. If the O2 catheter method is used, limiting flow rate to no more than 6–8 L/min may minimize the risk of pneumothorax and avoid any CO2 elimination that could conceivably slow the rise of PCO2 in some patients. Clinicians should be aware that the PCO2 may rise faster in younger patient. The PO2 may drop to a greater degree among patients with higher body temperature.
References
Wijdicks EF, Varelas PN, Gronseth GS, Greer DM. Evidence-based guideline update: determining brain death in adults—Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74:1911–8.
Intensive Care Society: guidelines for adult organ and tissue donation. http://www.ics.ac.uk. Accessed 18 Dec 2016.
The ANZICS statement on death and organ donation. Edition 3.2. 2013. http://www.anzics.com.au. Accessed 18 Dec 2016.
Shemie SD, Doig C, Dickens B, et al. Severe brain injury to neurological determination of death: Canadian forum recommendations. Can Med Assoc J. 2006;174:S1–13.
Wijdicks EF, Rabinstein AA, Manno EM, Atkinson JD. Pronouncing brain death: contemporary practice and safety of the apnea test. Neurology. 2008;71:1240–4.
Datar S, Fugate J, Rabinstein AA, Couillard P, Wijdicks EF. Completing the apnea test: decline in complications. Neurocrit Care. 2014;21:392–6.
Saposnik G, Rizzo G, Vega A, et al. Problems associated with the apnea test in the diagnosis of brain death. Neurol India. 2004;52:342–5.
Goudreau JL, Wijdicks EF, Emergy SF. Complications during apnea testing in the determination of brain death: predisposing factors. Neurology. 2000;55:1045–8.
Melano R, Adum ME, Scarlatti A, et al. Apnea test in diagnosis of brain death: comparison of two methods and analysis of complications. Transplant Proc. 2002;34:11–2.
Gorton LE, Dhar R, Woodworth L, et al. Pneumothorax as a complication of apnea testing for brain death. Neurocrit Care. 2016;25:282–7.
Burns JD, Russell JA. Tension pneumothorax complicating apnea testing during brain death evaluation. J Clin Neurosci. 2008;15:580–2.
Vivien B, Haralambo MS, Riou B. Barotrauma during apnea testing for the determination of brain death. Ann Fr Anesth Reanim. 2001;20:370–3.
Bar-Joseph G, Bar-Lavie Y, Zonis Z. Tension pneumothorax during apnea testing for the determination of brain death. Anesthesiology. 1998;89:1250–1.
Henry NR, Marshall SG. Apnea testing: the effects of insufflation catheter size and flow on pressure and volume in a test lung. Respir Care. 2014;59:406–10.
Denny JT, Burr A, Tse J, et al. A new technique for avoiding barotrauma-induced complications in apnea testing for brain death. J Clin Neurosci. 2015;22:1021–4.
Perel A, Berger M, Cotev S. The use of continuous flow of oxygen and PEEP during apnea in the diagnosis of brain death. Intensive Care Med. 1983;9:25–7.
Levesque S, Lessard MR, Nicole PC, et al. Efficacy of a T-piece system and a continuous positive airway pressure system for apnea testing in the diagnosis of brain death. Crit Care Med. 2006;34:2213–6.
Gianni M, Scaravilli V, Colombo SM, et al. Apnea test during brain death assessment in mechanical ventilated and ECMO patients. Intensive Care Med. 2016;42:72–81.
Solek-Pastuszaka J, Sawicki M, Iwanczuk W, Bohatyrewicz R. Ventilator-delivered continuous positive airway pressure for apnea test in the diagnosis of brain death in patient with extremely poor baseline lung function: case report. Transplant Proc. 2016;48:2471–2.
Hocker S, Whalen F, Wijdicks EF. Apnea testing for brain death in severe acute respiratory distress syndrome: a possible solution. Neurocrit Care. 2014;20:298–300.
Shreshtha GS, Shreshtha PS, Acharya SP, et al. Apnea testing with continuous positive airway pressure for the diagnosis of brain death in a patient with poor baseline oxygenation status. Indian J Crit Care Med. 2014;18:331–3.
Wetterberg T, Sjobert T, Steen S. Effects of hypothermia in hypercapnia and hypercapnic hypoxemia. Acta Anesthesiol Scand. 1993;37:296–302.
Pelosi P, Ravagnan I, Giurati G, et al. Positive end-expiratory pressure improves respiratory system function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology. 1999;91:1221–31.
Behazin N, Jones SB, Cohen RI, Loring SH. Respiratory restriction and elevated pleural and esophageal pressures in morbid obesity. J Appl Physiol. 2010;108:212–8.
Ebata T, Watanabe Y, Amaha K, et al. Hemodynamic changes during the apnea test for diagnosis of brain death. Can J Anaesth. 1991;38:436–40.
Jeret JS, Benjamin JL. Risk of hypotension during apnea testing. Arch Neurol. 1994;51:595–9.
Kotloff R, Blosser S, Fulda G, et al. Management of the potential organ donor in the ICU: Society of Critical Care Medicine/American College of Chest Physicians/Association of Organ Procurement Organizations Consensus Statement. Crit Care Med. 2015;43:1291–325.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Kramer, A.H., Couillard, P., Bader, R. et al. Prevention of Hypoxemia During Apnea Testing: A Comparison of Oxygen Insufflation And Continuous Positive Airway Pressure. Neurocrit Care 27, 60–67 (2017). https://doi.org/10.1007/s12028-017-0380-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0380-0