Abstract
Purpose
The amount of blood on computed tomography (CT) has been shown to be a predictor of cerebral vasospasm after subarachnoid hemorrhage (SAH). However, the influence of the location of the blood on the incidence of vasospasm remains unclear. We retrospectively assessed the association of the blood volumes in the individual components (cisterns and fissures) of CT scans with angiographic vasospasm after SAH.
Methods
One hundred forty-nine SAH patients scheduled for cerebral aneurysm clipping were enrolled. The amount of subarachnoid blood was classified using the Fisher CT grade . The amounts of subarachnoid blood in 5 cisterns or 3 fissures were also evaluated using SAH scores ranging from 0 to 3 (0, no blood; 3, completely filled with blood). Cerebral vasospasm was diagnosed by the results of angiography.
Results
Angiographic vasospasm developed in 51 of 149 patients (34%). Of those, 26 patients were symptomatic. The Fisher CT grade and SAH scores in the right and left sylvian fissures and suprasellar cisterns were significantly higher in patients with angiographic vasospasm than in those without it. Univariate logistic regression analysis revealed that a high Fisher CT grade and high SAH scores in the right and left sylvian fissures and suprasellar cisterns were predictors of angiographic vasospasm. Multivariate analysis indicated that the SAH score in the right sylvian fissure was an independent predictor of angiographic vasospasm (odds ratio, 3.6; 95% confidence interval (CI), 1.7–7.7; P = 0.01).
Conclusion
The results indicated that the amount of blood in the right sylvian fissure was significantly associated with the development of angiographic vasospasm after SAH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral vasospasm after subarachnoid hemorrhage (SAH) is one of the major devastating complications of this condition and is related to morbidity and death. Previous studies have demonstrated that 13%–30% of patients with SAH were reported to have suffered clinical deterioration due to an ischemic event secondary to cerebral vasospasm, and approximately 50% of these patients either had long-term morbidity or died as a result of such an event [1–5]. Angiographic vasospasm has been reported to occur in 50%–70% of patients with SAH [4–6]. A number of research efforts have been directed toward identifying early predictors of vasospasm after SAH, because such identification may be able to provide more effective prevention of vasospasm and subsequently result in better neurological outcomes. The amount of SAH on computed tomography (CT), intraventricular hemorrhage (IVH), neurological grade, hypertension and temperature on admission, aneurysm location, smoking, and age have been reported as predictors of vasospasm [6, 7]. Of these, the most powerful predictor has been considered to be the thickness of the subarachnoid clot on the admission CT scan [8–11].
Clinically, the Fisher CT grading scale has been used most commonly to assess SAH on CT and it has been advocated as a tool to predict the development of vasospasm [12, 13]. However, this scale only identifies the thickness of the blood or clot in any cisterns or fissures and the presence of IVH or an intraparenchymal clot. There is no information regarding the exact location of blood or clots in the Fisher CT grading scale. It is therefore unknown whether there are specific locations (fissures and cisterns) that are prominently related to the development of cerebral vasospasm. In the present study, we hypothesized that the laterality and location of SAH and its amounts may affect the development of postoperative vasospasm after intracranial ruptured aneurism surgery. We retrospectively assessed the predictors of angiographic vasospasm after SAH, including the amount of blood in individual components of CT scans, such as the interhemispheric fissure, sylvian fissures, quadrigeminal cistern, suprasellar cisterns, and ambient cisterns.
Methods
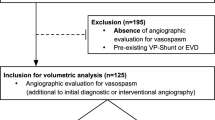
We retrospectively analyzed 149 patients who underwent cerebral aneurysm clipping for ruptured cerebral aneurysm at Nara Medical University between February 1999 and December 2007. Information regarding the patients’ demographic variables, pre- and intraoperative data, and postoperative course were examined from the medical records. Patients who died before the assessments for postoperative cerebral vasospasm by angiography were excluded.
The data collected included age; sex; weight; history of hypertension, diabetes, and coronary artery disease; location of cerebral aneurysm; severity of the neurological injury; preoperative electrocardiogram abnormality; the duration of operation and anesthesia; systolic blood pressure and heart rate on arrival at the operation room; blood glucose and body temperature after the induction of anesthesia; and postoperative angiographic and symptomatic vasospasm. The severity of neurological injury was graded using the Hunt and Kosnik and World Federation of Neurosurgical Societies (WFNS) classifications.
The amount of subarachnoid blood was classified using the Fisher CT grade: 1, none evident; 2, less than 1 mm thick; 3, more than 1 mm thick; and 4, any thickness with IVH or parenchymal extension. In addition, the amounts of subarachnoid blood in 5 cisterns or 3 fissures, including the interhemispheric fissure, quadrigeminal cistern and right and left sylvian fissures, suprasellar cisterns, and ambient cisterns on CT were also evaluated semiquantitatively as reported previously. Briefly, we used SAH scores ranging from 0 to 3 according to the criteria of Hijdra et al. [14]. Each cistern or fissure was graded separately according to the amount of extravasated blood: 0, no blood; 1, small amount of blood; 2, moderately filled with blood; or 3, completely filled with blood. One author of this report (Y.M.) blindly scored all of the CT scans performed immediately after admission.
In the postoperative period, a continuous infusion of diltiazem was routinely used to prevent cerebral vasospasm in all patients. The diagnosis of symptomatic vasospasm was made as an exclusion diagnosis, based on the onset of focal or global neurological deterioration not explained by other factors, including hydrocephalus, hemorrhage, surgical complications, metabolic abnormalities, or infection. The final diagnosis was performed according to the results of angiography with or without transcranial Doppler. Digital subtraction angiography was performed a week after the operation or at the time when the symptoms of delayed ischemic neurological deficits developed postoperatively. Angiographic vasospasm was diagnosed when a reduction of 50% or more of the normal diameter was demonstrated in the measurements of any cerebral arterial segment.
Statistical analysis
According to the angiographic findings, all patients were divided into two groups: spasm and non-spasm groups. Patients in the spasm group had angiographic vasospasm and those in the non-spasm group did not have angiographic vasospasm. Pre- and intraoperative variables associated with angiographic vasospasm were evaluated. Comparisons of demographic variables and clinical data between the groups were performed using unpaired t-test, χ2test, or Mann–Whitney U-test. Univariate and multivariate logistic regression analyses were performed to determine the predictors of postoperative spasm. Values of P < 0.05 were considered significant.
Results
Of 149 patients, 51 patients (34%) had angiographic vasospasm and 98 patients (66%) did not have it. Of the 51 patients with angiographic vasospasm, 26 patients (18% of all patients) had symptomatic vasospasm, whereas the vasospasm in 25 patients (16% of all patients) was asymptomatic. Table 1 shows the demographic variables in each group. There were no significant differences between the groups in demographic variables, including age, weight, sex, hypertension, diabetes, coronary artery disease, neurological grade, and location of the aneurysm. Table 2 shows the intraoperative variables in each group. There were no significant differences between the groups in intraoperative variables, including operation and anesthesia times, blood pressure and heart rate before anesthesia, temperature and glucose after the induction of anesthesia, and the incidence of re-rupture during the operation.
Table 3 shows the SAH scores in the individual components of CT scans and the Fisher CT grade in each group. The SAH scores in the right and left sylvian fissures and suprasellar cisterns and the Fisher CT grade were significantly higher in the spasm group than those in the nonspasm group (P < 0.05). Table 4 shows the results of univariate logistic regression analysis. Univariate logistic regression analysis revealed that the WFNS score (III–IV), Fisher CT grade (III–IV), SAH scores in the right and left sylvian fissures and suprasellar cisterns (score 3) were significantly associated with angiographic vasospasm. Table 5 shows the results of multivariate logistic regression analysis. Multivariate logistic regression analysis revealed that an SAH score of 3 in the right sylvian fissure was an independent variable associated with angiographic vasospasm. The sensitivity and specificity of an SAH score of 3 in the right sylvian fissure to predict the development of angiographic vasospasm were 58% and 69%, respectively.
Discussion
The results obtained in this retrospective study show that, whereas univariate logistic regression analysis revealed that the WFNS score, Fisher CT grade, and SAH scores in the right and left sylvian fissures and suprasellar cisterns were associated with angiographic vasospasm after SAH, multivariate logistic regression analysis indicated that a high SAH score in the right sylvian fissure was significantly associated with angiographic vasospasm in patients who underwent intracranial aneurismal surgery for ruptured cerebral aneurysm.
A number of studies have been performed to identify potential predictors of vasospasm after SAH. Reported predictors of cerebral vasospasm in patients with SAH include the amount of SAH on CT, IVH, neurological grade, hypertension and temperature on admission, aneurysm location, smoking, and age. Of these factors, a large blood volume or clots on CT is the only consistently demonstrated predictor of cerebral vasospasm. Fisher et al. [12] reported that 23 of 24 patients with subarachnoid blood clots larger than 5 × 3 mm developed serious symptomatic vasospasm, while symptomatic vasospasm occurred in only 1 of 18 patients with no blood or diffusely distributed blood in the subarachnoid space. The Fisher CT grading scale, which evaluates the amount of blood in any fissures or cisterns and the presence of IVH or intracerebral hemorrhage, has been widely used to identify patients at high risk for the development of cerebral vasospasm after SAH [12, 13]. However, because the Fisher CT grading scale does not evaluate the amount of blood in the specific fissures and cisterns, it is unknown whether there are specific fissures and cisterns that are prominently related to the development of cerebral vasospasm.
Hijdra et al. [14] evaluated the amount of subarachnoid blood in 10 cisterns or fissures, including the frontal interhemispheric fissure, the quadrigeminal cistern, both suprasellar cisterns, both ambient cisterns, both basal sylvian fissures, and both lateral sylvian fissures, by using semiquantitative scores, and they demonstrated that the sum of the scores in the 10 cisterns or fissures was associated with the development of cerebral vasospasm in patients with SAH. However, this method of summed scoring ignored the importance of localized accumulations of blood and, therefore, important information on the localization of the blood may have been missed in the process of the assessments. Recently, Claassen et al. [15] evaluated the effects of the locations of blood or clots on delayed cerebral ischemia and infarction after SAH, although they did not evaluate the laterality of the amount of blood. Their results indicated that a completely filled SAH in the anterior interhemispheric fissure was significantly associated with the development of delayed cerebral ischemia and those in the anterior interhemispheric fissure, lateral and basal sylvian fissures, and suprasellar cistern were significantly associated with the development of infarction. In the present study, we evaluated the influence of locations with a large amount of blood and their laterality on the development of angiographic vasospasm after SAH. The results of multivariate logistic regression analysis indicated that SAH completely filling the right sylvian fissure was significantly associated with the development of angiographic vasospasm after SAH. The reasons for the discrepancy between the results reported by Claassen et al. [15] and us are unknown. However, a possible reason for the difference might be that Claassen et al. did not evaluate the laterality of the amount of blood, although we did so. Another reason might be that Claassen et al. evaluated delayed cerebral ischemia or infarction, whereas we evaluated angiographic vasospasm.
The mechanisms by which the blood in the right sylvian fissure was related to the development of angiographic vasospasm in our study are unknown. Although these mechanisms remain undetermined, a variety of mechanisms are considered to be involved in the development of cerebral vasospasm [1]. Erythrocytes have been shown to be the blood component necessary for the development of vasospasm, and the most vasoactive substance within them is oxyhemoglobin. Oxyhemoglobin’s action can involve direct vasoconstriction, the release of arachidonic metabolites and endothelin from the arterial wall, inhibition of endothelium-dependent vasodilation through nitric oxide scavenging, damage to perivascular nerves, and the promotion of free radical reactions. In addition to these effectsbrought about by the blood located in the subarachnoid spaces, sympathetic activation has also been reported to be related to the development of vasospasm [16–20]. Peerless et al. [16] indicated the vessels remote from direct contact with blood showed reactive narrowing 1 week after SAH, suggesting that cerebral vasospasm may be mediated by a central control mechanism acting through the sympathetic nervous system. Bunc et al. [17] have demonstrated that the exclusion of sympathetic nervous system activity in rabbits prevented vasospasm in circumstances similar to SAH.
It is well known that brain stem cardiovascular centers are involved in the regulation of cardiac function via sympathetic and parasympathetic efferents. However, recent evidence has indicated that supratentorial centers may also be involved in cardiovascular regulation. Hirashima et al. [21] indicated that the amount of SAH in the right sylvian fissure was independently associated with abnormal ECG changes in patients with SAH and the grade of the amount of SAH in the right sylvian fissure was a better predictor of ECG changes than the Fisher CT grade. These authors suggested that, because the insular cortex is an important site of control of autonomic function with right-sided dominance in sympathetic cardiovascular effects, the blood in the right sylvian fissure possibly stimulates the insular cortex, resulting in sympathetic cardiovascular effects such as ECG changes. Although the level of sympathetic activation was not evaluated in the present study, a large volume of blood in the right sylvian fissure may have induced sympathetic activation. Sympathetic activation may activate inflammatory responses, including the activation of adhesion molecules and cytokines, which have been considered to be related to the development of vasospasm and a poor clinical outcome [1, 22]. Yoshimoto et al. [22] reported that SAH patients with systemic inflammatory response syndrome on admission had a higher likelihood of cerebral vasospasm. Recently, Kato et al. [23] demonstrated that inhibition of sympathetic activation using beta-adrenergic receptor antagonists attenuated the levels of proinflammatory cytokine in cerebrospinal fluid in a rat model of SAH. However, the premise of sympathetic activation being involved in angiographic vasospasm is speculative. Further studies will be required to clarify the mechanisms of the relation between blood in the right sylvian fissure and angiographic vasospasm.
There are several limitations in the present study. First, we evaluated angiographic vasospasm. The results might have been different if symptomatic vasospasm had been evaluated. Second, cerebral angiography was performed a week after the operation or at the time when the symptoms of delayed ischemic neurological deficits developed postoperatively. So we may have missed angiographic vasospasm that developed at different periods from our assessments, although the development of cerebral vasospasm can be most prevalent at around one week after the onset of SAH. Third, the number of patients enrolled in this study was relatively small, and so further studies with more patients will be required.
In summary, the predictors of angiographic vasospasm after SAH, including the amount of blood in individual components of CT scans, were retrospectively evaluated in patients with SAH using logistic regression analysis. Although univariate analysis indicated that the neurological score, Fisher CT grade, and the amount of blood in the individual components of CT scans were associated with angiographic vasospasm, multivariate analysis indicated that a high SAH score in the right sylvian fissure was most significantly associated with angiographic vasospasm. This finding may not be used clinically to predict symptomatic cerebral vasospasm, because it is a predictor of angiographic vasospasm. However, this phenomenon may be used to understand the pathogenesis of cerebral vasospasm in patients with SAH and to provide a key for the development of strategies for the prevention of cerebral vasospasm.
References
Kolias AG, Sen J, Belli A. Pathogenesis of cerebral vasospasm following aneurismal subarachnoid hemorrhage: putative mechanisms and novel approaches. J Neurosci Res. 2009;87(1):1–11.
Kassell NF, Torner JC, Haley EC Jr, Jane JA, Adams HP, Kongable GL. The International Cooperative Study on the Timing of Aneurysm Surgery. Part 1: Overall management results. J Neurosurg. 1990;73:18–36.
Macdonald RL. Management of cerebral vasospasm. Neurosurg Rev. 2006;29:179–93.
Gonzalez NR, Boscardin WJ, Glenn T, Vinuela F, Martin NA. Vasospasm probability index: a combination of transcranial Doppler velocities, cerebral blood flow, and clinical risk factors to predict cerebral vasospasm after aneurismal subarachnoid hemorrhage. J Neurosurg. 2007;107:1101–12.
Weir B, Grace M, Hansen J, Rothberg C. Time course of vasospasm in man. J Neurosurg. 1978;48:173–8.
Harrod CG, Bendok BR, Batjer HH. Prediction of cerebral vasospasm in patients presenting with aneurismal subarachnoid hemorrhage: a review. Neurosurgery. 2005;56:633–54.
Macdonald RL, Rosengart A, Huo D, Karrison T. Factors associated with the development of vasospasm after planned surgical treatment of aneurismal subarachnoid hemorrhage. J Neurosurg. 2003;99:644–52.
Gurusinghe NT, Richardson AE. The value of computerized tomography in aneurismal subarachnoid hemorrhage. J Neurosurg. 1984;60:763–70.
Mohsen F, Pomonis S, Illingworth R. Prediction of delayed cerebral ischaemia after subarachnoid haemorrhage by computed tomography. J Neurol Neurosurg Psychiatry. 1984;47:1197–202.
Brouwers PJ, Dippel DW, Vermeulen M, Lindsay KW, Hasan D, van Gijn J. Amount of blood on computed tomography as an independent predictor after aneurysm rupture. Stroke. 1993;24:809–14.
Reilly C, Amidei C, Tolentino J, Jahromi BS, Macdonald RL. Clot volume and clearance rate as independent predictors of vasospasm after aneurismal subarachnoid hemorrhage. J Neurosurg. 2004;101:255–61.
Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980;6:1–9.
Kistler JP, Crowell RM, Davis KR, Heros R, Ojemann RG, Zervas T, et al. The relation of cerebral vasospasm to the extent and location of subarachnoid blood visualized by CT scan: a prospective study. Neurology. 1983;33(4):424–36.
Hijdra A, van Gijn J, Nagelkerke NJ, Vermelen M, van Crevel H. Prediction of delayed cerebral ischemia, rebleeding, and outcome after aneurismal subarachnoid hemorrhage. Stroke. 1988;19:1250–6.
Claassen J, Bernardini GL, Kreiter K, Bates J, Du YE, Copeland D, et al. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the Fisher scale revisited. Stroke. 2001;32:2012–20.
Peerless SJ, Fox AJ, Komatsu K, Hunter IG. Angiographic study of vasospasm following subarachnoid hemorrhage in monkeys. Stroke. 1982;13:473–9.
Bunc G, Kovacic S, Strnad S. The influence of noradrenergic blockade on vasospasm and the quality of cerebral dopamine beta-hydroxylase following subarachnoid haemorrhage in rabbits. Wien Klin Wochenschr. 2003;115:652–9.
Morooka H. Cerebral arterial spasm. I. Adrenergic mechanism in experimental cerebral vasospasm. Acta Med Okayama. 1978;32:23–37.
Lobato R, Marin J, Salaices M, Burgos J, Rivilla F, Garcia AG. Effect of experimental subarachnoid hemorrhage on the adrenergic innervation of cerebral arteries. J Neurosurg. 1980;53:477–9.
Kovacic S, Bunc G, Ravnik J. Correspondence between the time course of cerebral vasospasm and the level of cerebral dopamine-beta-hydroxylase in rabbits. Auton Neurosci. 2006;130:28–31.
Hirashima Y, Takashima S, Matsumura N, Kurimoto M, Origasa H, Endo S. Right sylvian fissure subarachnoid hemorrhage has electrocardiographic consequences. Stroke. 2001;32:2278–81.
Yoshimoto Y, Tanaka Y, Hoya K. Acute systemic inflammatory response syndrome in subarachnoid hemorrhage. Stroke. 2001;32:1989–93.
Kato H, Kawaguchi M, Inoue S, Hirai K, Furuya H. The effects of beta-adrenoceptor antagonists on proinflammatory cytokine concentrations after subarachnoid hemorrhage in rats. Anesth Analg. 2009;108(1):288–95.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nomura, Y., Kawaguchi, M., Yoshitani, K. et al. Retrospective analysis of predictors of cerebral vasospasm after ruptured cerebral aneurysm surgery: influence of the location of subarachnoid blood. J Anesth 24, 1–6 (2010). https://doi.org/10.1007/s00540-009-0836-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-009-0836-2