Abstract
Background
Little is known about the specific risks of metastasis in esophageal adenocarcinoma in relation to invasion depth or other pathologic factors.
Methods
We conducted a multicenter retrospective study in 13 high-volume centers in Japan from January 2000 to October 2014 to elucidate the risk of metastasis of esophageal adenocarcinoma. A total of 458 patients (217 surgically resected and 241 endoscopically resected) with esophageal adenocarcinoma or esophagogastric adenocarcinoma involving the esophagus were included. Metastasis was considered positive if there was histologically confirmed metastasis in the surgical specimen or clinically confirmed metastasis during follow-up. Metastasis was considered negative if no metastasis was identified in resected specimens and during follow-up in patients treated surgically or no metastasis during follow-up for >5 years in patients treated by endoscopic resection.
Results
Metastasis was identified in 72 patients. Multivariate analysis confirmed lymphovascular involvement [odds ratio (OR) 6.20; 95 % confidence interval (CI) 3.12–12.32; p < 0.001], a poorly differentiated component (OR 3.69; 95 % CI 1.92–7.10; p < 0.001), and lesion size >30 mm (OR 3.12; 95 % CI 1.63–5.97; p = 0.001) as independent risk factors for metastasis. No metastasis was detected in patients with mucosal cancer without lymphovascular involvement and a poorly differentiated component (0/186 lesions) or in patients with cancer invading the submucosa (1–500 µm) without lymphovascular involvement, a poorly differentiated component, and ≤30 mm (0/32 lesions).
Conclusions
Mucosal and submucosal cancers (1–500 µm invasion) without risk factors have a low incidence of metastasis and may thus be good candidates for endoscopic resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal adenocarcinoma is an aggressive disease with a steadily increasing incidence in the Western world [1–3]. Although no equivalent data are available for Eastern countries, it is suggested that the rate of esophageal adenocarcinoma will increase in Asia because of the decreasing prevalence of Helicobacter pylori infection and Westernization of the diet [4, 5].
Survival of patients with esophageal adenocarcinoma correlates with disease stage. Locally advanced disease has a 5-year survival rate of ~20 % [6]. The poor survival of patients with advanced cancer means that surveillance and early detection of esophageal adenocarcinoma have become critical issues, [7, 8], and rigorous surveillance of Barrett’s esophagus (BE) and a systematic biopsy protocol have improved the detection of early cancer [9].
Early esophageal adenocarcinoma has traditionally been treated by surgery; however, endoscopic resection (ER) has recently emerged as a potential alternative to surgery. ER can eliminate cancers that are confined to the esophagus [10–12], but it cannot cure cancers that have metastasized to the lymph nodes and is therefore only suitable for cancers with a very low risk of metastasis.
To identify suitable candidates for ER, it is therefore necessary to understand the associations between early esophageal adenocarcinomas and metastasis. Studies of surgical specimens have indicated that mucosal carcinomas are associated with a low risk of metastasis (0.0–7.4 %), while cancers that have invaded the submucosa (SM) have a higher risk (17.5–46 %) [13–25]. However, little is known about the specific risks associated with invasion into each part of the mucosa or SM. To determine the indications for ER, it is necessary to establish a detailed metastasis-risk profile in relation to invasion depth and other pathologic factors. We therefore elucidated the metastasis-risk factors in patients with esophageal adenocarcinomas, including esophagogastric cancer involving the esophagus.
Methods
Patients
This was a retrospective, multicenter study conducted at 13 high-volume centers in Japan, comprising 5 university hospitals and 8 tertiary care hospitals. Records for all patients who underwent surgery or ER for adenocarcinoma of the esophagus from January 2000 to October 2014 were extracted from the database and reviewed. Patients were included if they met the following criteria: (1) histologically diagnosed adenocarcinoma, (2) histologically diagnosed mucosal or SM cancer, or (3) esophageal cancer or esophagogastric cancer involving the esophagus. The exclusion criteria were: (1) chemotherapy or radiation before surgery, (2) chemotherapy or radiation before or after ER, (3) deeper invasion (SM invasion ≥500 µm) in the cardia than in the esophagus, and (4) any other primary invasive cancer that had been treated within the preceding 5 years. This study was approved by the institutional review board and was performed in accordance with the Declaration of Helsinki.
Standard handling of resected specimens
Pathologic examinations were performed according to the standard methods proposed by the Japan Esophageal Society [26]. Resected specimens were stretched and pinned to boards and fixed in formalin. After fixation, all resected specimens were cut into 2-mm-wide longitudinal slices for ER specimens and 5 mm wide for surgical specimens. The tissue specimens were embedded in paraffin, sectioned at 4 µm, and stained with hematoxylin and eosin.
Macroscopic appearance was classified as protruding type or flat type, and cancer invasion depth was classified based on the Japanese Classification of Esophageal Cancer [26]. BE includes new muscularis mucosa just under the columnar epithelium. The primary muscularis mucosa is called the deep muscularis mucosa (DMM), and the new muscularis mucosa, which is frequently observed in BE, is called superficial muscularis mucosa (SMM). Cancer arising in Barrett’s epithelium without invasion through the basement membrane (carcinoma in situ) or cancer extending beyond the basement membrane into the SMM was classified as SMM (Table 1). Cancers extending beyond the SMM into the lamina propria were classified as LPM, and those with the deepest invasion were defined as DMM [26]. If no new muscularis mucosa was identified, cancer invasion depth was classified as follows: cancer arising in Barrett’s epithelium without invasion through the basement membrane and cancers extending into the lamina propria were classified as LPM, and cancers with deepest invasion into the muscularis mucosa were defined as DMM.
SM invasion depth was measured in micrometers from the deepest muscularis mucosa to the deepest tumor invasion in the SM. The width of muscularis mucosa invasion and SM invasion were assessed in each slice, and the maximum width was measured in micrometers. Cancer differentiation was evaluated, and lesions were judged positive for a poorly differentiated component if it was identified in the part invading the DMM or SM. An infiltrative growth pattern was defined as follows: type a, expansive growth of tumor nests with a well-demarcated border from surrounding tissue; type b, intermediate growth pattern, between type a and c; type c, infiltrative growth of tumor nests with an ill-defined border with the surrounding tissue. Cancer differentiation and an infiltrative growth pattern were evaluated in DMM and SM cancers. Pathologic diagnosis was conducted by the pathologists at the individual facilities. An expert pathologists’ review was conducted in selected patients with metastasis diagnosed at their facilities with mucosal cancer or SM invasion ≤2000 µm and negative for lymphovascular involvement.
Data collection
Lesion characteristics and details of ER or surgery were obtained from the database or medical records. Follow-up patient data were obtained from medical records, and in the case of patients who moved away from the hospital, we attempted to obtain outcome details by questionnaire or by telephone conversation with the patient or the patient’s family or referring physician.
The histologic features of the lesions were obtained from the pathology reports and review of the resected specimens, and they included size, macroscopic appearance, location of the tumor, SM invasion depth, invasion width, histologic type, lymphovascular involvement, and resection margin.
Definition of metastatic status
Metastasis was considered positive if one of following criteria was fulfilled: (1) histologically confirmed metastasis in surgical specimen or (2) clinically confirmed metastasis during follow-up after surgery or ER. Metastasis was considered negative if: (1) no metastasis was identified in resected specimens and during follow-up for patients treated by surgery or (2) no metastasis was identified during follow-up longer than 5 years for patients treated by ER.
Statistical analysis
The results were expressed as median (range). Continuous variables were compared using Mann-Whitney U tests. Categorical baseline data were compared using Yates χ 2 tests. In multivariate analysis, independent factors were determined by the Cox regression hazards model using variables with significant or marginally significant differences in univariate analysis. Receiver-operating characteristic (ROC) curves were used to evaluate the predictive accuracy of lesion size for assessing metastasis [27]. To calculate this curve, the threshold value was varied systematically over the whole range of lesion sizes. The sensitivity for metastasis (sensitivity on the y-axis) of each of these threshold values was plotted against the specificity for metastasis (1—specificity on the x-axis). The optimal threshold value for differentiating between patients who did and did not develop metastasis was determined by the point of the ROC curve near the specificity and sensitivity values of 1.0. Differences were considered significant at values of p < 0.05. Analyses were conducted using SPSS version 11.0J (SPSS, Chicago, IL, USA).
Results
Patient characteristics
A total of 516 patients with no history of other primary invasive cancers received surgery or ER for mucosal or SM adenocarcinoma of the esophagus. Only the deepest lesion was included for four patients who had two or more lesions. Fifty-eight patients were excluded for the following reasons: (1) chemotherapy before surgery or after ER in 4 patients; (2) details of histologic findings missing in 4 patients; (3) deeper invasion (SM invasion ≥500 µm) in the cardia than in the esophagus in 4 patients; (4) 5-year follow-up data after ER not obtained in 31 patients; (5) death from other diseases within 5 years after ER in 15 patients. Data for 241 patients initially treated by ER and 217 patients initially treated by surgery were analyzed. BE was evident in 311 patients, including 247 with short-segment and 64 with long-segment BE. In cases of short-segment BE, the centers of tumors were located below the esophagogastric junction in 18 patients, 0–1 cm above the junction in 182 patients, 1 < −2 cm above the junction in 33 patients, and 2 cm< above the junction in 14 patients. In cases of long-segment BE, the centers of tumors were located below the esophagogastric junction in 1 patients, 0–1 cm above the junction in 8 patients, 1 < −2 cm above the junction in 5 patients, and 2 cm < above the junction in 50 patients. Of the 241 patients treated by ER, 202 were treated by endoscopic submucosal dissection and 39 by endoscopic mucosal resection; 225 lesions were treated by en bloc resection and 16 by piecemeal resection. Of patients initially treated by ER, 41 had lymphovascular involvement, of whom 31 were treated by additional surgery, 1 by radiation and 1 by chemotherapy. The other eight patients received no additional treatment, mainly because of their condition or because of patient refusal. Details of surgery for 217 patients were as follows: proximal gastrectomy and distal esophagectomy in 101 patients, subtotal esophagectomy in 59 patients, total or proximal gastrectomy with partial resection of distal esophagus in 39 patients, middle and lower esophagectomy in 3 patients, and others in 15 patients.
Metastasis and risk factors in patients treated by surgery
Of the 217 cancers treated by surgery, 14 were SMM cancers, 14 were LPM cancers, 24 were DMM cancers, 23 were SM cancers with 1–500 µm invasion [SM cancer (1–500 µm)], and 142 were SM cancers (≥501 µm). Metastases were confirmed in surgical specimens from 47 patients, and metastases developed in 10 patients after a median (range) follow-up period of 9 (2–24) months. The initial sites of metastases were lymph nodes in 52 patients, lymph nodes and bone in one patient, liver in three patients, and peritoneum in one patient. Survival analysis was performed in patients treated before 1 January 2010. Of 91 patients, 9 died of esophageal cancer and 13 died of other diseases. The overall 1-, 3-, and 5-year survival rates were 97, 88, and 81 %, respectively.
Metastasis and risk factors in all patients
Metastases were confirmed in surgical specimens from 54 patients, including 7 patients who received surgery after ER. Metastases developed in 18 patients (10 patients after surgery and 8 patients after ER) after a median (range) follow-up period of 12 (2–44) months. The initial sites of metastases were lymph nodes in 64 patients, lymph nodes and other organs in 2 patients, liver in 3 patients, bone in 1 patient, lung in 1 patient, and peritoneum in 1 patient. According to univariate analysis (Table 2), metastasis was predicted by lesion size, macroscopic appearance, invasion depth of cancer, invasion depth to SM, invasion width to SM, lymphovascular involvement, infiltrative growth pattern, and a poorly differentiated component. Metastasis was identified in significantly more patients with lymphatic involvement (50/95) than with vascular involvement (32/87) (p = 0.032).
Based on the advice of a statistician (T.M.), multivariate analysis was divided into two steps because some factors, such as SM invasion depth or width, were only available for SM cancers. The initial analysis was conducted in SM cancers. This showed that SM invasion depth (p = 0.76) and width (p = 0.14) were not significant, and these factors were excluded from further analysis. The second multivariate analysis (Table 3) included DMM and SM cancers and confirmed lymphovascular involvement [odds ratio (OR) 6.20; 95 % confidence interval (CI) 3.12–12.32; p < 0.001], a poorly differentiated component (OR 3.69; 95 % CI 1.92–7.10; p < 0.001), and lesion size (OR 3.12; 95 % CI 1.63–5.97; p = 0.001) as independent risk factors for metastasis.
Optimal threshold value for lesion size
The ROC curve, based on all 458 lesions, demonstrated that the highest accuracies for predicting metastasis were achieved by applying cutoff values of 20, 30, or 40 mm (Fig. 1). A cutoff value of a 20 mm correctly identified 57 of 72 lesions with metastasis and 217 of 386 cancers without metastasis, providing a sensitivity of 79.2 % and a specificity of 56.2 %. A cutoff value of 30 mm correctly identified 35 of 72 lesions with metastasis and 312 of 386 cancers without metastasis, providing a sensitivity of 48.6 % and a specificity of 80.8 %. A cutoff value of a 40 mm correctly identified 26 of 72 lesions with metastasis and 352 of 386 cancers without metastasis, providing a sensitivity of 36.1 % and a specificity of 91.2 %. Considering the clinical application of these results and comparing them with other predictors (Table 4), a specificity of 56.2 % for the cutoff value of 20 mm was too low, and we judged 30 mm to be the optimal cutoff value and 40 mm a suboptimal cutoff value to ensure high sensitivity and acceptable specificity (>75 %).
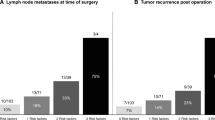
Subgroup analysis
When we subdivided SM cancers based on invasion depths of 500-µm increments (Table 5), SM cancer (1–500 µm) had a low risk (6.8 %) of metastasis, while SM cancers (≥501 µm) had a 22.9–50 % risk of metastasis. When we subdivided cancers based on metastasis risk factors (Table 6), mucosal cancer without lymphovascular involvement and a poorly differentiated component had no risk of metastasis (0/186 lesions), and SM cancer (1–500 µm) without lymphovascular involvement, a poorly differentiated component, and ≤30 mm also had no metastasis risk (0/32 lesions).
Discussion
In this study, we analyzed the metastatic risk of mucosal and SM esophageal adenocarcinomas and identified a subgroup of cancers with low metastatic risk.
Metastasis was observed in 4.4 % of patients with mucosal cancer in this study. This incidence was higher than that for gastric mucosal cancer (2.2 %) [28] and colonic mucosal cancer (0 %) [29]. Unlike elsewhere, the esophagus contains a rich plexus of lymphatic ducts near the muscularis mucosa, [30–33], and invasion of the cancer into the muscularis mucosa increases exposure to the lymphatic ducts and enhances lymphatic involvement. The higher rate of lymphovascular involvement of esophageal adenocarcinoma (7.8 %) compared with gastric mucosal cancer (0.6 %) [28] or colon cancer may have been responsible for the higher incidence of metastasis in esophageal mucosal cancer in this study. According to our data, lymphovascular involvement, a poorly differentiated component, and lesion size were independent predictors of metastasis. Although these factors have been identified previously [13, 22, 24, 34], the current study confirmed the involvement of these three factors by multivariate analysis and also confirmed their importance in a Japanese population.
The frequency of metastasis is known to increase with the depth of tumor invasion into the SM [13, 22, 23]. The SM1 area remains the most controversial, and some studies have reported a relevant incidence of lymph node metastasis even in SM1 cancers [23, 35, 36]. However, if the rate of metastasis is stratified by pathologic findings, SM1 cancers without risk factors such as lymphovascular involvement and a poorly differentiated component have very low rates [12, 21, 37]. Accordingly, some studies [38, 39] have suggested that a subgroup of SM cancers could be treated sufficiently by ER. SM1 cancer is commonly defined as cancer involving the upper third of the SM. However, this division cannot be applied in ER specimens because not all the SM is resected by ER, and absolute measurement may thus be a more pragmatic way of subdividing the SM layer in ER specimens. In this study, we compared cutoff values of 500-µm increments (1–500, 501–1000, 1001–1500 µm, etc.) and identified ≤500 µm as the most effective depth for dividing the risk of metastasis: the risk of metastasis in SM cancers with 1–500 µm invasion was 6.8 % and that for SM cancers 1–500 µm without risk factors was 0 %. Although the sample size for SM cancers (1–500 µm) was not large enough to draw definite conclusions, these results nevertheless provide important information regarding the indications of ER.
Previous studies that investigated the risk of metastasis mainly included surgical cases [13–19, 23, 24]. Lesions treated surgically may mainly include lesions with high metastatic risk (SM cancer and larger lesions), while lesions treated by ER may mainly include lesions with lower metastatic risk (mucosal cancer and smaller lesions). The overall metastatic risk of mucosal and SM cancers thus cannot be estimated precisely on the basis of surgical specimens alone because of selection bias. We therefore included both patients treated by ER and surgery to reduce selection bias and evaluate the risk of metastasis in whole mucosal and SM cancers. In this study, metastasis was considered negative if no metastasis was identified during follow-up longer than 5 years for patients treated by ER. Although we cannot completely exclude the possibility that metastasis may develop after 5 years, previous reports showed that most tumor recurrences presented during the first 2 years of follow-up [13, 40]. Moreover, all 18 metastases in the current study occurred within 44 months during follow-up, and no metastases were identified in 289 patients who were followed up for longer than 5 years. We therefore consider that our definition of a metastasis-negative group was reasonable.
One of the strengths of this study was the quality of the ER and detailed histologic investigation. ER series from the West included 48.3–50.8 % piecemeal resected specimens [11, 41], and there is some concern regarding the accuracy of histologic diagnosis of cancer invasion depth assessed in piecemeal resection specimens. However, given that 93.4 % (225/241) of the lesions in this study were resected en bloc, the reliability in terms of invasion depth may be high. We also conducted detailed histologic investigations, including measurements of the vertical and horizontal extents of SM invasion and infiltrative growth pattern, to investigate all the possible factors contributing to metastasis. Investigation of many factors allowed us to select the important risk factors for metastasis by multivariate analysis, providing results that are simple enough for use in clinical settings.
This study was limited by its retrospective style, which includes the potential for recall bias in patient selection. However, patients were extracted from the database in all facilities, and the recall bias for patient selection may have been small. The quality of histologic assessment was a limitation of this study. Immunostaining, e.g., for D2-40, CD31, or CD34, was not mandatory in all patients, and no central review of pathologic findings was performed, mainly because of restrictions arising from the study’s retrospective design. Further well-designed and well-organized prospective studies including more detailed pathologic examinations are needed to confirm the present results. Another limitation was the potential for discrepancies between Japanese and Western pathologists in the diagnosis of mucosal cancer [42, 43], which may also have caused bias. However, such discrepancies are usually evident in neoplasias limited to the epithelium and decline with invasion into the lamina propria, such that most cancers invading into the DMM or deeper would be diagnosed accurately. Considering that the risk of metastasis was limited to cancers invading into the DMM or deeper, bias in the risk of metastasis for DMM and SM cancer may have been low.
In conclusion, lymphovascular involvement, a poorly differentiated component, and lesion size were independent risk factors for metastasis in patients with esophageal adenocarcinoma. Mucosal cancer and SM cancer (1–500 µm) without such risk factors were not associated with metastasis and would thus be good candidates for ER.
References
DeMeester SR. Adenocarcinoma of the esophagus and cardia: a review of the disease and its treatment. Ann Surg Oncol. 2006;13:12e30.
Shaheen NJ, Richter JE. Barrett’s oesophagus. Lancet. 2009;373:850–61.
Brown LM, Devesa SS, Chow WH. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J Natl Cancer Inst. 2008;100:1184–7.
Wu JC. Gastroesophageal reflux disease: an Asian perspective. J Gastroenterol Hepatol. 2008;23:1785–93.
Hongo M, Nagasaki Y, Shoji T. Epidemiology of esophageal cancer: orient to occident. Effects of chronology, geography and ethnicity. J Gastroenterol Hepatol. 2009;24:729–35.
Gillison EW, Powell J, Mcconkey CC, et al. Surgical workload and outcome after resection for carcinoma of the oesophagus and cardia. Br J Surg. 2002;89:344–8.
Inadomi JM, Sampliner R, Lagergren J, et al. Screening and surveillance for Barrett esophagus in high-risk groups: a cost-utility analysis. Ann Intern Med. 2003;138:176–86.
Sharma P, Sidorenko EI. Are screening and surveillance for Barrett’s oesophagus really worthwhile? Gut. 2005;54:i27–32.
Abela JE, Going JJ, Mackenzie JF, et al. Systematic four-quadrant biopsy detects Barrett’s dysplasia in more patients than nonsystematic biopsy. Am J Gastroenterol. 2008;103:850–5.
Nakagawa K, Koike T, Iijima K, et al. Comparison of the long-term outcomes of endoscopic resection for superficial squamous cell carcinoma and adenocarcinoma of the esophagus in Japan. Am J Gastroenterol. 2014;109:348–56.
Pech O, May A, Manner H, et al. Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus. Gastroenterology. 2014;146:652–60.
Manner H, Pech O, Heldmann Y, et al. Efficacy, safety, and long-term results of endoscopic treatment for early stage adenocarcinoma of the esophagus with low-risk sm1 invasion. Clin Gastroenterol Hepatol. 2013;11:630–5.
Westerterp M, Koppert LB, Buskens CJ, et al. Outcome of surgical treatment for early adenocarcinoma of the esophagus or gastro-esophageal junction. Virchows Arch. 2005;446:497–504.
Stein HJ, Feith M, Bruecher BL, et al. Early esophageal cancer: pattern of lymphatic spread and prognostic factors for long-term survival after surgical resection. Ann Surg. 2005;242:566–73.
Barbour AP, Jones M, Brown I, et al. Risk stratification for early esophageal adenocarcinoma: analysis of lymphatic spread and prognostic factors. Ann Surg Oncol. 2010;17:2494–502.
Lee L, Ronellenfitsch U, Hofstetter WL, et al. Predicting lymph node metastases in early esophageal adenocarcinoma using a simple scoring system. J Am Coll Surg. 2013;217:191–9.
Altorki NK, Lee PC, Liss Y, et al. Multifocal neoplasia and nodal metastases in T1 esophageal carcinoma: implications for endoscopic treatment. Ann Surg. 2008;247:434–9.
Pennathur A, Farkas A, Krasinskas AM, et al. Esophagectomy for T1 esophageal cancer: outcomes in 100 patients and implications for endoscopic therapy. Ann Thorac Surg. 2009;87:1048–54.
Dubecz A, Kern M, Solymosi N, et al. Predictors of lymph node metastasis in surgically resected T1 esophageal cancer. Ann Thorac Surg. 2015;99:1879–86.
Prasad GA, Wu TT, Wigle DA, et al. Endoscopic and surgical treatment of mucosal (T1a) esophageal adenocarcinoma in Barrett’s esophagus. Gastroenterology. 2009;137:815–23.
Alvarez HL, Pouw RE, van Vilsteren FG, et al. Risk of lymph node metastasis associated with deeper invasion by early adenocarcinoma of the esophagus and cardia: study based on endoscopic resection specimens. Endoscopy. 2010;42:1030–6.
Buskens CJ, Westerterp M, Lagarde SM, et al. Prediction of appropriateness of local endoscopic treatment for high-grade dysplasia and early adenocarcinoma by EUS and histopathologic features. Gastrointest Endosc. 2004;60:703–10.
Sepesi B, Watson TJ, Zhou D, et al. Are endoscopic therapies appropriate for superficial submucosal esophageal adenocarcinoma? An analysis of esophagectomy specimens. J Am Coll Surg. 2010;210:418–27.
Leers JM, DeMeester SR, Oezcelik A, et al. The prevalence of lymph node metastases in patients with T1 esophageal adenocarcinoma a retrospective review of esophagectomy specimens. Ann Surg. 2011;253:271–8.
Dunbar KB, Spechler SJ. The risk of lymph-node metastases in patients with high-grade dysplasia or intramucosal carcinoma in Barrett’s esophagus: a systematic review. Am J Gastroenterol. 2012;107:850–62.
Japan Esophageal Society. Japanese Classification of Esophageal Cancer, tenth edition: part I. Esophagus. 2009;6:1–58.
Metz CE. Basic principles of ROC analysis. Semin Nucl Med. 1978;8:283–98.
Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–25.
Morson BC, Whiteway JE, Jones EA, et al. Histopathology and prognosis of malignant colorectal polyps treated by endoscopic polypectomy. Gut. 1984;25:437–44.
Goseki N, Koike M, Yoshida M. Histopathologic characteristics of early stage esophageal carcinoma. A comparative study with gastric carcinoma. Cancer. 1992;69:1088–93.
Bogomoletz WV, Molas G, Gayet B, et al. Superficial squamous cell carcinoma of the esophagus. A report of 76 cases and review of the literature. Am J Surg Pathol. 1989;13:535–46.
Sugimachi K, Ikebe M, Kitamura K, et al. Long-term results of esophagectomy for early esophageal carcinoma. Hepatogastroenterology. 1993;40:203–6.
Sabik JF, Rice TW, Goldblum JR, et al. Superficial esophageal carcinoma. Ann Thorac Surg. 1995;60:896–902.
Davison JM, Landau MS, Luketich JD, et al. A model based on pathologic features of superficial esophageal adenocarcinoma complements clinical node staging in determining risk of metastasis to lymph nodes. Clin Gastroenterol Hepatol. 2016;14:369–77.
Griffin SM, Burt AD, Jennings NA. Lymph node metastasis in early esophageal adenocarcinoma. Ann Surg. 2011;254:731–6.
Bollschweiler E, Baldus SE, Schroder W, et al. High rate of lymph-node metastasis in submucosal esophageal squamous cell carcinomas and adenocarcinomas. Endoscopy. 2006;38:149–56.
Manner H, Pech O, Heldmann Y, et al. The frequency of lymph node metastasis in early-stage adenocarcinoma of the esophagus with incipient submucosal invasion (pT1b sm1) depending on histological risk patterns. Surg Endosc. 2015;29:1888–96.
Greene CL, Worrell SG, Attwood SE, et al. Emerging concepts for the endoscopic management of superficial esophageal adenocarcinoma. J Gastrointest Surg. 2016;20:851–60.
Mohiuddin K, Dorer R, El Lakis MA, et al. Outcomes of surgical resection of T1bN0 esophageal cancer and assessment of endoscopic mucosal resection for identifying low-risk cancers appropriate for endoscopic therapy. Ann Surg Oncol. 2016;23:2673–8.
Dresner SM, Griffin SM. Pattern of recurrence following radical oesophagectomy with two-field lymphadenectomy. Br J Surg. 2000;87:1426–33.
Sgourakis G, Gockel I, Lang H. Endoscopic and surgical resection of T1a/T1b esophageal neoplasms: a systematic review. World J Gastroenterol. 2013;19:1424–37.
Schlemper RJ, Itabashi M, Kato Y, et al. Differences in diagnostic criteria for gastric carcinoma between Japanese and Western pathologists. Lancet. 1997;349:1725–9.
Stolte M, Kirtil T, Oellig F, et al. The pattern of invasion of early carcinomas in Barrett’s esophagus is dependent on the depth of infiltration. Pathol Res Pract. 2010;206:300–4.
Acknowledgments
We thank Tomoki Shimizu, Yasutaka Kuribayashi, Yuko Hara, Hiroki Kikuchi, Yuichi Sato, Mitsuhiro Fujishiro, and Taku Yamagata for help with data collection, Yasuo Ohkura, Tomio Arai and Atsusi Ochiai for help with pathologic examination, and Junya Oguma, Takayuki Nishi for general advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Saku Central Hospital Ethics Committee.
Funding
Supported by a grant from the Japanese Gastroenterological Association.
Rights and permissions
About this article
Cite this article
Ishihara, R., Oyama, T., Abe, S. et al. Risk of metastasis in adenocarcinoma of the esophagus: a multicenter retrospective study in a Japanese population. J Gastroenterol 52, 800–808 (2017). https://doi.org/10.1007/s00535-016-1275-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1275-0