Abstract
Background
A nationwide survey of autoimmune hepatitis (AIH) patients was performed in Japan in 2015. The aims of this study were to elucidate the trends and characteristics of AIH in Japan, in addition to identifying differences in AIH between acute hepatitis and chronic hepatitis.
Methods
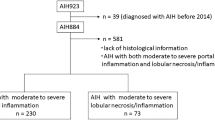
Questionnaires about patients with AIH diagnosed from 2009 to 2013 were sent to 437 hospitals or clinics with hepatology specialists.
Results
A total of 1682 patients were enrolled. The mean age at diagnosis was 60.0 years, and 87.1 % of patients were female. Serum immunoglobulin G levels were high, peaking at 1.5–2.0 g/dL. Histological diagnoses of chronic hepatitis, acute hepatitis, and cirrhosis were seen in 79.6, 11.7, and 6.7 % of patients respectively. In addition to elevation of aminotransferase levels, the frequencies of emperipolesis and human leukocyte antigen (HLA)-DR2 positivity were higher in patients with acute hepatitis than in those with chronic hepatitis. Approximately 80 % of patients were treated with corticosteroids, and in 97.7 % of them, their condition improved. Steroid pulse therapy was more frequently given to patients with acute hepatitis than to those with chronic hepatitis.
Conclusions
In the present nationwide survey of AIH patients in Japan, patients with acute hepatitis had clinical features different from those of patients with chronic hepatitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autoimmune hepatitis (AIH) is caused by an immune disorder that is characterized by hypergammaglobulinemia, autoantibodies, and chronic active hepatitis on liver histology. Associations between AIH and numerous immune mechanism disorders, including those with a genetic background, have been elucidated, but the precise mechanisms remain unknown. Specific serum markers or liver histological findings of AIH remain to be established, and diagnostic criteria for AIH have improved with time. The International Autoimmune Hepatitis Group (IAIHG) proposed diagnostic criteria for AIH in 1993 [1]. The IAIHG revised the criteria in 1999 [2] and proposed simplified criteria in 2008 [3]. Simplified criteria solve the complexity of modified criteria and make possible easy diagnosis of AIH in daily clinical situations. However, the diagnosis of nonclassic phenotypes of AIH has remained difficult.
In Japan, a national survey of AIH has been conducted several times since 1975 [4–7]. The most recent survey was conducted in 2009 and was based on 1056 patients with AIH diagnosed from 2006 to 2008 [7]. The survey showed an increase in the incidence of acute hepatitis and aging and lowering of serum immunoglobulin G (IgG) levels in comparison with the previous survey in 1995. Japanese diagnostic criteria were proposed and revised on the basis of the results of the nationwide survey. Japanese guidelines for AIH were developed in 2013 on the basis of the results of the nationwide survey conducted in 2009 and recent research findings [8, 9]. AIH with an acute presentation is also mentioned in the new Japanese guidelines, but differences between AIH with acute hepatitis and AIH with chronic hepatitis remain unclear. Changes in diagnostic criteria and guidelines for AIH have gradually disseminated to general clinicians, as well as liver specialists; therefore, the characteristics of AIH and treatment of AIH may have changed even in the relatively short term. The purpose of the present study was to determine the characteristics of recent patients with AIH in Japan, and to elucidate differences in AIH with acute hepatitis and AIH with chronic hepatitis.
Materials and methods
Participants
This nationwide survey was conducted by the Autoimmune Hepatitis Group, a subgroup of the Intractable Hepato-Biliary Disease Study Group supported by the Ministry of Health, Labour and Welfare of Japan. This survey was approved by the Ethics Committee of Fukushima Medical University (protocol number 2170). Questionnaires were sent to 437 hospitals and clinics with at least one board-certified physician and surgeon in January 2015. The survey also asked about patients newly diagnosed with AIH from 2009 to 2013, excluding patients previously registered in whom AIH had previously been diagnosed, and respondents were asked to return the questionnaires by June 2015. Finally, the questionnaires about 1682 AIH patients from 105 hospitals or clinics were collected and analyzed. The diagnostic criteria for AIH were not specified, and the diagnosis of AIH depended on each hospital and clinic.
Questionnaire
The questionnaire was composed of topics based on the previous survey, as follows: age at diagnosis, sex, history and family history, alcohol and medication history, laboratory and liver histological findings at diagnosis, presence of other autoimmune or malignant diseases, treatment, and outcome. Basic histological findings were graded as follows: interface hepatitis, portal inflammation, plasma cell infiltration, and lobular necrosis or inflammation (0, absent; 1, mild; 2, moderate to severe); fibrosis (0, absent, 1; mild, 2, moderate; 3, severe; 4, cirrhosis); bile duct injury, hepatocyte rosette formation, centrilobular necrosis, emperipolesis, and fatty change (0, absent; 1, present).
Statistical analysis
The results are presented as the mean ± standard deviation or the median and the interquartile range for continuous variables and the percentage for categorical variables. Statistical analysis was performed with SPSS Statistics for Windows version 17.0 (SPSS, Chicago, IL, USA). If there were missing values, statistical analysis was performed with available data. The two groups were compared with the χ 2 test and Fisher’s exact test for categorical variables and the Mann–Whitney U test for continuous variables.
Results
Characteristics of patients with AIH
The mean age at diagnosis was 60.0 ± 13.8 years, and the male-to-female ratio was 1:6.7. The distribution of the age at diagnosis had a single peak in the 60s in both males and females (Fig. 1). The χ 2 test showed no significant difference in male rates between 904 elderly patients (65 years or older) and 674 younger patients (younger than 65 years) (14.7 % vs 12.6 %, P = 0.451). Twenty-two (1.6 %) of 1401 patients with AIH had a family history of AIH. Among 1573 patients, 674 (42.8 %) had a medication history, and major kinds of drugs were a calcium blocker (126/674, 18.7 %), an angiotensin II receptor blocker (75/674, 11.1 %), and hydroxymethylglutaryl-CoA reductase (70/674, 10.4 %). Among the 1682 patients, 294 (17.5 %) had a history of alcohol intake and 120 (40.8 %) of them drank less than 20 g ethanol per day.
Laboratory findings
Laboratory findings at diagnosis are shown in Table 1, and the distributions of the levels of alanine aminotransferase (ALT), total bilirubin (TB), IgG, and antinuclear antibody (ANA) are shown in Fig. 2. ALT level elevation was mostly mild, with 50.2 % of patients having ALT levels below 200 U/L and 9.9 % of patients having ALT levels greater than 1000 U/L. The distribution of serum TB levels had an incidence peak around mild elevation and a small peak at severe elevation. IgG concentration showed a single peak at 1.5–2.0 g/dL. With respect to serum autoimmune antibodies, ANA was present in 1499 (90.7 %) of 1653 patients, anti-smooth muscle antibody (ASMA) was present in 215 (40.9 %) of 526 patients, and ASMA was also present in 29 (50 %) of 58 patients who tested negative for ANA. There were no significant differences in the positivity ratio for ANA (89.1 % in 2009), ASMA (42.5 % in 2009), human leukocyte antigen (HLA)-DR4 (present 67.1 % vs 60 % in 2009), and HLA-DR2 (present 9.3 % vs 10 % in 2009) between the present survey and the 2009 survey.
Liver histological findings
Liver histological assessment was performed in 1457 patients; 79.6 % of patients had chronic hepatitis, and 11.7 % of patients had acute hepatitis. There were no significant differences in the proportions between the present survey and the 2009 survey (Table 2). Regarding the basic histological characteristics of AIH, portal inflammation (96.7 %) and interface hepatitis (95.8 %) had the highest frequency, whereas emperipolesis had the lowest frequency (Table 3). The prevalences of hepatocyte rosette formation and centrilobular necrosis were 41.5 and 35.4 % respectively.
Complications
Other autoimmune diseases were present in 401 (24.2 %) of 1659 patients with AIH (Table 4). In the 401 patients with other autoimmune diseases, chronic thyroiditis was the most frequent complication (7.5 %), followed by Sjögren syndrome (5.7 %), primary biliary cholangitis (3.6 %), and rheumatoid arthritis (3.4 %). Malignancy was seen in 116 (7.1 %) of 1645 patients with AIH. In the 116 patients with malignancy, hepatocellular carcinoma was the most frequent complication (1.8 %), followed by breast cancer (1.2 %) and gastric cancer (0.8 %). The frequency of male patients was significantly higher in AIH patients with malignant diseases than in those with autoimmune diseases (12.9 % vs 6.7 %; P = 0.012). There was no significant difference in the frequency of other autoimmune diseases between patients with HLA-DR2 and patients without HLA-DR2 (15.4 % vs 25.0 %; P = 0.271).
Treatment
Among 1664 patients, 1336 (80.3 %) were treated with prednisolone, and of these, 387 patients (29.0 %) were treated with prednisolone alone and 737 patients (55.2 %) were treated with a combination of prednisolone and ursodeoxycholic acid (UDCA). Moreover, 159 patients (11.9 %) were treated by steroid pulse therapy. Administration of prednisolone was effective in reducing the activity of AIH in 1190 (97.7 %) of 1218 patients treated with prednisolone. Overall, 285 (24.3 %) of 1172 patients relapsed despite continuous administration of prednisolone. Azathioprine was administered to 146 patients (8.7 %). Among 328 patients who did not receive prednisolone treatment, 257 patients (78.4 %) were treated with UDCA alone, and 37 patients (11.3 %) were followed up without any treatment. Figure 3 shows the distributions of the initial and maintenance dosages of prednisolone. For the initial dosage, 30–40 mg daily and 40–50 mg daily accounted for 39.0 and 28.7 % of 1292 patients respectively. As a maintenance dosage, 5–7.5 mg daily was given to 50.6 % of patients. The serum levels of AST, ALT, TB, and IgG at diagnosis were significantly higher in patients treated with prednisolone alone than in those treated with UDCA alone (data not shown).
Characteristics of patients with acute hepatitis and patients with chronic hepatitis
Serum levels of AST, ALT, ALP, and TB at diagnosis were significantly higher in patients with acute hepatitis than in patients with chronic hepatitis (Table 5). Serum IgG levels and ANA titers were significantly lower in patients with acute hepatitis than in patients with chronic hepatitis. Moreover, the frequency of HLA-DR2 positivity was higher in patients with acute hepatitis than in patients with chronic hepatitis (14.0% vs 3.7 %; P = 0.022). For treatment, the initial dosage of prednisolone and the frequency of steroid pulse therapy were greater in patients with acute hepatitis than in patients with chronic hepatitis (23.4 % vs 10.1 %; P < 0.005). Liver histological findings such as interface hepatitis, portal/lobular inflammation, plasma cell infiltration, and fibrosis were severer in patients with chronic hepatitis than in patients with acute hepatitis. The frequencies of centrilobular necrosis and emperipolesis were higher in patients with acute hepatitis than in patients with chronic hepatitis.
Outcome
Sixty-five patients (3.9 %) died of liver-related causes during the 4-year survey period. The male-to-female ratio was approximately 1:3.3, and the mean age at diagnosis was 68.9 years. Three patients received liver transplants, and one patient died after liver transplant.
Discussion
The clinical characteristics of patients with AIH have shown a broad spectrum by country (Table 6) [10–13]. The results of the present nationwide survey present the clinical characteristics of recent patients with AIH in Japan. The proportion of females slightly increased compared with the proportion in the nationwide survey in 2009, even though the proportion had gradually decreased in previous studies (male-to-female ratio 1:12 [4], 1:9.5 [5], 1:7.0 [6], and 1:6.0 [7]). Both the mean age at diagnosis (59.9 ± 14.7 years) and the distribution showing a single peak in the 60s were similar to those in the nationwide survey in 2009 [7].
Each laboratory finding tended to be similar to its counterpart in the nationwide survey in 2009. Although the serum IgG levels were almost the same as in the last survey (2398.8 ± 1015.1 mg/dL) [7], the IgG concentration peak shifted from 2.0–2.5 g/dL to 1.5–2.0 g/dL in the present survey. One of the reasons for this shift is that some atypical characteristics such as acute hepatitis and lower serum IgG levels have been broadly accepted as one aspect of AIH since the nationwide survey in 2009. Japanese diagnostic criteria have also been revised with respect to the definition of an increased IgG level from 2000 mg/dL to 1.1 times the upper limit of normal on the basis of the results of the nationwide survey in 2009 [8]. New diagnostic criteria may also affect the diagnosis of AIH in male patients.
The prevalences of chronic hepatitis (present 79.6 % vs 81.6 % in 2009 ), acute hepatitis (present 11.7 % vs 10.9 % in 2009), and liver cirrhosis (present 6.7 % vs 6.4 % in 2009) were close to those in the nationwide survey in 2009. Emperipolesis has been reported in 65–78 % of patients with AIH in Western countries [14], although it had been an unfamiliar histological finding of AIH in Japan until the simplified IAIHG criteria were proposed. The frequency of emperipolesis was therefore evaluated for the first time in the present nationwide survey in Japan. Emperipolesis was more frequent in patients with acute hepatitis than in patients with chronic hepatitis. The presence of emperipolesis indicates the interaction of lymphocytes and hepatocytes. Emperipolesis, in addition to elevation of aminotransferase levels may reflect a stronger immune interaction in acute hepatitis than in chronic hepatitis. Emperipolesis is frequently observed in hepatocytes around the interface hepatitis of AIH with severe hepatic changes. Interface hepatitis was predominant in patients with chronic hepatitis; on the other hand, emperipolesis was frequently seen in patients with acute hepatitis in the present survey. The causes of this discrepancy are unknown, but emperipolesis may be overlooked in patients with chronic hepatitis, because it is difficult to distinguish emperipolesis from apoptotic-body-laden macrophages and differentiate whether lymphocytes are located inside or outside hepatocytes [15]. In fact, the prevalence of emperipolesis in the present survey was lower than in Western countries. Moreover, acute hepatitis in the present survey was the acute presentation of AIH including acute exacerbation, because acute hepatitis contained fibrosis from F0 to F3. However, the frequency of emperipolesis (22.9 %, 8/35) in AIH patients with acute hepatitis without fibrosis (F0) had a tendency to be higher than that of patients with chronic hepatitis (11.6 %, 44/378) (P = 0.056). Detailed evaluations are necessary to determine the clinical significance of emperipolesis.
HLA is the most well-described disease-specific susceptibility gene complex in patients with AIH. HLA-DR4 is the most frequent HLA in Japanese patients [6, 7]. HLA-DR3 is the most frequent HLA, followed by HLA-DR4, in Caucasian patients [16]. Patients with HLA-DR4 are older than middle-aged and have mild disease activity, whereas patients with HLA-DR3 are young and have severe disease activity [16]. The genetic backgrounds associated with an acute presentation of AIH have not yet been clarified. Thus, the present survey is the first report showing that HLA-DR2 is predominant in patients with acute hepatitis and occurs more frequently than in patients with chronic hepatitis. The HLA-DR2 gene is the second most frequent susceptibility gene in Japanese patients [6]. Although it was not possible to confirm this in the present survey, Japanese patients with HLA-DR2 have been reported to have a lower frequency of concurrent autoimmune disease [17]. More detailed study is needed to elucidate the association between HLA-DR2 and the clinical features of AIH.
Immunosuppressive therapy for AIH patients with a definitive diagnosis was recommended by the Japanese treatment guideline [8]. Although both corticosteroid and azathioprine were proposed as basic immunosuppressants by the American Association for the Study of Liver Diseases in 2010 [18], corticosteroid alone or in combination with UDCA is the basic treatment for AIH in Japan because azathioprine is not covered by National Health Insurance in Japan. The frequencies of patients with AIH treated with prednisolone (present 80.6 % vs 74.5 % in 2009) and the efficacy of prednisolone (present 97.7 % vs 93.7 % in 2009) were both increased compared with those in the nationwide survey in 2009, whereas the initial dosage of prednisolone was similar to that in the nationwide survey in 2009. The rate of administration of azathioprine was also slightly increased from 5.6 to 8.7 %. These results may be attributed to a broad understanding of immunosuppressive therapy for AIH. Moreover, steroid pulse therapy was frequently performed in AIH patients with higher activity or acute hepatitis. The efficacy of pulse therapy in patients with AIH should be evaluated in the future. Only few patients were treated with UDCA alone or had no treatment. The various treatments mentioned for patients with AIH reflect a broad spectrum of AIH.
Complications are serious problems in AIH because they affect treatment and prognosis. The frequencies of concomitant autoimmune diseases and malignancies were quite similar to those in the nationwide survey in 2009. A previous mega survey showed that hepatocellular carcinoma developed in 5.1 % of patients with AIH in Japan [19]. The reason for the high frequency of malignancy in male patients is unknown, however, alcohol intake or smoking may be associated with the finding. Concomitant malignancy, including hepatocellular carcinoma, should always be considered, especially in patients with risk factors such as cirrhosis, old age, and alcohol intake.
There are some limitations of this survey. First, the revised or simplified AIH score could not be evaluated because of some missing values and questionnaires without scoring. However, the questionnaires were sent to liver specialists, and, thus the results of the present survey reflect patients with a diagnosis of AIH. Second, basic liver histological findings may not be enough. As mentioned above, acute hepatitis in the present survey actually contained both acute hepatitis and acute exacerbation. Patients with acute hepatitis in the present survey included those with histological findings of chronic active hepatitis, such as portal inflammation with interface hepatitis and fibrosis. Moreover, emperipolesis was less often evaluated than other classic basic findings of AIH. A histological definition of acute hepatitis and improved skills of pathologists for evaluation of emperipolesis will solve these problems in the future. Third, the incidence and prevalence of AIH in Japan could not be determined from this survey. Despite a narrow region of Japan being studied, increases in the incidence and prevalence of AIH have recently been reported [20]. Annual registration of all AIH patients in Japan will be needed to elucidate the precise incidence and characteristics of AIH.
In conclusion, the characteristics of AIH have changed in the relatively short term in parallel with a proposal for diagnostic criteria and understanding of new clinical and histological findings. The present nationwide survey showed that AIH patients with an acute presentation have clinical features different from those of patients with chronic hepatitis in Japan.
References
Johnson PJ, McFarlane IG. Meeting report: International Autoimmune Hepatitis Group. Hepatology. 1993;18:998–1005.
Alvarez F, Berg PA, Bianchi FB, et al. International Autoimmune Hepatitis Group report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929–38.
Hennes EM, Zeniya M, Czaja AJ, et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;48:169–76.
Monna T, Kuroki T, Yamamoto S. Autoimmune hepatitis: the present status in Japan. Gastroenterol Jpn. 1985;20:260–72.
Onji M, Nonaka T, Horiike N, et al. Present status of autoimmune hepatitis in Japan. Gastroenterol Jpn. 1993;28(Suppl 4):134–8.
Toda G, Zeniya M, Watanabe F, et al. Present status of autoimmune hepatitis in Japan-correlating the characteristics with international criteria in an area with a high rate of HCV infection. J Hepatol. 1997;26:1207–12.
Abe M, Mashiba T, Zeniya M, et al. Present status of autoimmune hepatitis in Japan: a nationwide survey. J Gastroenterol. 2011;46:1136–41.
Onji M, Zeniya M, Yamamoto K, et al. Autoimmune hepatitis: diagnosis and treatment guide in Japan, 2013. Hepatol Res. 2014;44:368–70.
Ohira H, Abe K, Takahashi A, et al. Recent advances in the pathogenesis and new diagnostic guidelines in Japan. Intern Med. 2015;54:1323–8.
Wong RJ, Gish R, Frederick T, et al. The impact of race/ethnicity on the clinical epidemiology of autoimmune hepatitis. J Clin Gastroenterol. 2012;46:155–61.
van Gerven NM, Verwer BJ, Witte BI, et al. Epidemiology and clinical characteristics of autoimmune hepatitis in the Netherlands. Scand J Gastroenterol. 2014;49:1245–54.
Delgado JS, Vodonos A, Malnick S, et al. Autoimmune hepatitis in southern Israel: a 15-year multicenter study. J Dig Dis. 2013;14:611–8.
Kim BH, Kim YJ, Jeong SH, et al. Clinical features of autoimmune hepatitis and comparison of two diagnostic criteria in Korea: a nationwide, multicenter study. J Gastroenterol Hepatol. 2013;28:128–34.
Tiniakos DG, Brain JG, Bury YA. Role of histopathology in autoimmune hepatitis. Dig Dis. 2015;33(Suppl 2):53–64.
Harada K. Histological findings of autoimmune hepatitis. In: Ohira H, editor. Autoimmune liver disease: perspectives from Japan. Tokyo: Springer Japan; 2014. p. 45–65.
Czaja AJ, Doherty DG, Donaldson PT. Genetic bases of autoimmune hepatitis. Dig Dis Sci. 2002;47:2139–50.
Miyake Y, Iwasaki Y, Takaki A, et al. Human leukocyte antigen DR status and clinical features in Japanese patients with type 1 autoimmune hepatitis. Hepatol Res. 2008;38:96–102.
Manns MP, Czaja AJ, Gorham JD, et al. Diagnosis and management of autoimmune hepatitis. Hepatology. 2010;51:2193–213.
Ohira H, Abe K, Takahashi A, et al. Clinical features of hepatocellular carcinoma in patients with autoimmune hepatitis in Japan. J Gastroenterol. 2013;48:109–14.
Yoshizawa K, Joshita S, Matsumoto A, et al. Incidence and prevalence of autoimmune hepatitis in the Ueda area, Japan. Hepatol Res. 2016;46:878–83.
Acknowledgments
This study was conducted and supported by Health Labor Science Research grants from Research on Measures for Intractable Diseases, the Intractable Hepato-Biliary Diseases Study Group in Japan.
In addition to the authors, the hepatology specialists who participated in this study and the contributors to this study were as follows: Masahito Minami (Aiseikai Yamashina Hospital), Hikaru Nagahara (Aoyama Hospital Tokyo Women’s Medical University), Shiro Yokohama (Asahikawa Medical Center), Koji Sawada (Asahikawa Medical University), Takato Ueno (Asakura Medical Association Hospital), Yuki Haga (Chiba University), Chiharu Miyabayashi (Chikuma Central Hospital), Masaya Tamano (Dokkyo Medical University Koshigaya Hospital), Yasuaki Takeyama (Fukuoka University), Kenji Imai (Gifu University Hospital), Yuichi Yamazaki (Gunma University Hospital), Kazuhito Kawata (Hamamatsu University School of Medicine), Hiroshi Aikata (Hiroshima University Hospital), Koji Ogawa (Hokkaido University), Shuhei Nishiguchi (Hyogo College of Medicine), Akihide Masumoto (Iizuka Hospital), Toshihiko Mizuta (Imari Arita Kyoritsu Hospital), Kojiro Kataoka (Iwate Medical University School of Medicine), Chitomi Hasebe (Japanese Red Cross Asahikawa Hospital), Hiroshi Watanabe (Japanese Red Cross Fukuoka Hospital), Hideki Fujii (Japanese Red Cross Kyoto Daiichi Hospital), Hiroo Fukada (Juntendo University Nerima Hospital), Kazuyoshi Kon (Juntendo University School of Medicine),Takuya Genda (Juntendo University Shizuoka Hospital), Takako Nomura (Kagawa University Hospital), Mikihiro Tsutsumi (Kanazawa Medical University), Miki Murata (Kansai Medical University Medical Center), Kazuya Kitamura (Kanazawa University Hospital), Nobuko Koyama (Kawasaki Medical School), Shinji Iwasaki (Kochi University), Takeshi Kawasaki (Kumamoto University Hospital), Kouju Kobayashi (Kurihara Central Hospital), Hitoshi Takagi (Kusunoki Hospital), Yuya Seko (Kyoto Prefectural University of Medicine), Yuki Bekki (Kyushu University), Shinji Shimoda (Kyushu University Hospital), Hisashi Takayama (Maebashi Red Cross Hospital),Yasuyuki Nagao (Matsushita Memorial Hospital), Toshie Mashiba (Matsuyama Red Cross Hospital), Kiyohiko Kishi (Meiwa General Hospital), Naoya Murashima (Mishuku Hospital), Motoshige Nabeshima (Mitsubishi Kyoto Hospital), Akihiro Obora (Murakami Memorial Hospital Asahi University), Atsumasa Komori (Nagasaki Medical Center), Hidetaka Shibata (Nagasaki University Hospital), Yasuyo Morita (Nagata Hospital), Saiyu Tanaka (Nara City Hospital), Kei Moriya (Nara Medical University), Kengo Tomita (National Defense Medical Colledge Hospital), Toshiki Yamamoto (Nihon University Hospital), Kentarou Igarashi (Niigata City General Hospital), Satoshi Yamagiwa (Niigata University), Daisuke Watanabe (Noshiro Yamamoto Medical Association Hospital), Akira Kaneko (NTT Osaka Hospital), Shinya Yokoyama (Ogaki Municipal Hospital), Tomohiko Suzuki (Ohkubo Hospital), Shinichi Fujioka (Okayama Saiseikai General Hospital), Mie Arakawa (Oita University Hospital), Kazunori Noguchi (Omuta City Hospital), Norifumi Kawada (Osaka City University Graduate School of Medicine), Takatoshi Nawa (Osaka Medical Center for Cancer and Cardiovascular Diseases), Hideko Ohama (Osaka Medical College Hospital), Kunimaro Furuta (Osaka University), Shiro Takami (Otsu Municipal Hospital), Taiga Otsuka (Saga University Hospital), Atsushi Nakazawa (Saiseikai Central Hospital), Morikazu Onji (Saiseikai Imabari Hospital), Shigeru Matsui (Saiseikai Kawaguchi General Hospital), Fujimasa Tada (Saiseikai Matsuyama Hospital), Sumiko Nagoshi (Saitama Medical Center), Mie Inao (Saitama Medical University), Yoshinori Horie (Sanno Medical Center), Tomoaki Nakajima (Sapporo-Kosei General Hospital), Hideyasu Takagi (Sapporo Medical University Hospital), Takeji Umemura (Shinshu University School of Medicine), Toshiyuki Baba (Showa University Northern Yokohama Hospital), Naoki Yamashita (Steel Memorial Yawata Hospital), Hiroshi Okano (Suzuka General Hospital), Atsushi Naganuma (Takasaki General Medical Center), Kentaro Kikuchi (Teikyo University Hospital, Mizonokuchi), Kazuhiko Koike (The Jikei University Daisan Hospital), Yoshio Aizawa (The Jikei University Katsushika Medical Center), Shougo Ohkoshi (The Nippon Dental University), Ryo Nakagomi, Tomohiro Tanaka (The University of Tokyo Hospital), Mie Shinohara (Toho University Omori Medical Center), Yutaka Miyazaki (Tohoku Kosai Hospital), Yu Nakagome (Tohoku University Hospital), Mitsunori Morimatsu (Tokuyama Medical Association Hospital), Tadashi Ikegami (Tokyo Medical University Ibaraki Medical Center), Naoaki Hashimoto (Tokyo Teishin Hospital), Masahiko Koda (Tottori University Hospiital), Tomoyuki Nemoto (University of Fukui Hospital), Masami Minemura (Toyama University Hospital), Yoshiyuki Mori (Wakayama Medical University), Kazuo Okumoto (Yamagata University), Yasuhiro Funayama (Yamagata City Hospital SAISEIKAN), Isao Hidaka (Yamaguchi University), Noriyuki Ono (Yame General Hospital), Takaaki Ikeda (Yokosuka Kyosai Hospital).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Yoshiyuki Suzuki received lecture fees from Bristol-Myers Squibb. The other authors declare that they have no conflict of interest.
Additional information
The authors in the Autoimmune Hepatitis Study Group, a subgroup of the Intractable Hepato-Biliary Disease Study Group in Japan, are listed in “Acknowledgments.”
Rights and permissions
About this article
Cite this article
Takahashi, A., Arinaga-Hino, T., Ohira, H. et al. Autoimmune hepatitis in Japan: trends in a nationwide survey. J Gastroenterol 52, 631–640 (2017). https://doi.org/10.1007/s00535-016-1267-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1267-0