Abstract
Background
The prevalence of diabetes mellitus (DM) has been increasing. The present study was carried out to examine the relationship between this increase and fatty liver.
Methods
Japanese participants who underwent regular health examinations in 1991, 1996, 2001, 2006, and 2011 were enrolled. Fatty liver was diagnosed using ultrasonography. DM was defined as requiring the use of medication for DM, having a fasting blood glucose level ≥126 mg/dl, or hemoglobin A1c level ≥6.5 %.
Results
Logistic regression analysis on data from 11,235 participants (6,882 men and 4,271 women) in 2011 revealed that the association between fatty liver and DM was independent of age, body composition, and other confounders [odds ratio (OR) 1.97, 95 % confidence interval (95 % CI) 1.66–2.32 in men, and OR, 3.12; 95 % CI, 2.29–4.26 in women]. In 2006, 5,318 participants did not have DM and were able to be followed up in 2011. Fatty liver in 2006 was an independent predictor of DM in 2011 [OR 1.73 (95 % CI 1.20–2.50) in men, 4.13 (2.16–8.10) in women]. The prevalence of DM increased significantly during the 20-year period examined among both men (6.0, 8.9, 10.0, 10.8, 12.0 %, P < 0.001) and women (3.3, 4.5, 4.2, 4.1, 5.1 %, P = 0.004), accompanied with an increased prevalence of fatty liver among both men (10.8, 26.3, 33.8, 36.7, and 38.0 %, P < 0.001) and women (6.5, 16.7, 22.2, 21.3, and 20.8 %, P < 0.001).
Conclusion
Fatty liver independently predicts both present and future DM. Fatty liver may play an important role in the recent increases in the prevalence of DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The increasing prevalence of diabetes mellitus (DM) is a worldwide problem that is also occurring in Japan [1]. Obesity is recognized as the major driving force in the development of DM [2, 3]. However, in Japan, the prevalence of obesity has been increasing at a slower rate in men and has started to decline in women recently [4].
The liver plays a central role in nutrient homeostasis, because it stores glucose after a meal as glycogen or converts excess glucose to fatty acids, and oxidizes fatty acids to provide energy for gluconeogenesis during fasting to maintain a stable blood glucose level. Exaggerated gluconeogenesis in the liver is one of the major causes of hyperglycemia in type 2 DM patients [5]. Accumulating evidence suggests that fatty liver predicts the presence of DM cross-sectionally [6] and longitudinally [7–10]. Further, it has been reported that hepatokines such as fetuin-A [11, 12] and selenoprotein P [13, 14] are associated with insulin resistance and type 2 DM. Thus, the liver has attracted great attention as a key player in the pathogenesis of DM.
In the present study, we examined the relationship between DM and candidate factors such as fatty liver in a Japanese population during a 20-year timeframe, with the goal of identifying the association between fatty liver and DM.
Materials and methods
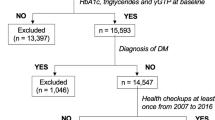
Japanese participants aged 30–79 years who received regular health checkups in 1991, 1996, 2001, 2006, or 2011 were enrolled in this study. This study was conducted at Kagoshima Kouseiren Medical Health Care Center, and was approved by the ethics committee of the Kagoshima Prefectural Federation of Agricultural Cooperatives for Health and Welfare, and the Kagoshima University Graduate School of Medical and Dental Sciences.
The diagnosis of fatty liver was made using ultrasonography (SSA-250A in 1991, 1996, and 2001; SSA-700A in 2006 and 2011; SSA-680 in 2011; and SSA-790 in 2011, Toshiba, Ibaraki, Japan; Logic 400 in 2001 and 2006, GE Yokogawa, Tokyo, Japan) based on the presence of a bright liver (increased echogenicity) with liver–kidney contrast (increased echogenicity of the liver compared to the right kidney). Subjects were classified into five brackets according to age: 30–39, 40–49, 50–59, 60–69, and 70–79. Body mass index (BMI) was calculated using the standard equation: body weight (kg)/height2 (m2). Body composition was categorized according to the Western Pacific Region of WHO criteria pertaining to obesity (WPRO criteria): BMI <18.5 kg/m2 (underweight), 18.5–22.9 kg/m2 (normal weight), 23.0–24.9 kg/m2 (overweight), and ≥25 kg/m2 (obese). Venous blood samples were obtained from all subjects before 9:00 a.m. after an overnight fast and analyzed immediately. Serum concentrations of total cholesterol (TC), triglycerides (TG), and blood glucose levels were measured using standard laboratory procedures. HDL-C levels were determined using detergents and direct homogeneous assays of serum samples (Daiichi Chemicals, Takaoka, Japan). To express hemoglobin A1c values using the National Glycoprotein Standardization Program (NGSP) format, hemoglobin A1c values were calculated using the following regression equations using values based on the standardization program of the Japan Diabetes Society (JDS): NGSP-value (%) = 1.02 × JDS-value (%) + 0.25 (%) [15]. Serological testing for hepatitis B surface antigen (HBsAg) and hepatitis C virus antibodies (HCV-Ab) was performed using an enzyme immunoassay and an enzyme-linked immunosorbent assay, respectively.
Hypertension was defined by the use of medication for hypertension, systolic blood pressure ≥130 mmHg, or diastolic blood pressure ≥85 mmHg. Dyslipidemia was defined by the use of medication for dyslipidemia, TC ≥220 mg/dl, TG ≥150 mg/dl, or HDL-C <40 mg/dl. DM was defined by the use of medication for DM, fasting blood glucose ≥126 mg/dl, or hemoglobin A1c ≥6.5 %.
Statistical analysis
Continuous variables were analyzed using t-tests or one-way analysis of variance (ANOVA). Categorical variables were examined using the chi-square test or the Cochran–Armitage test for trend. We used the Cochran–Mantel–Haenszel test to compare categorical variables across age brackets and body composition categories. The maximum likelihood estimates of the odds ratios (ORs) for the risk of fatty liver and 95 % confidence intervals (95 % CIs) were calculated using logistic regression models. All P values are two-sided. P values <0.05 were considered statistically significant. Statistical analyses were performed using JMP version 7 (SAS Corp., Cary, NC, USA) and R version 2.13.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Fatty liver predicts present DM
The association between DM and components of the metabolic syndrome was examined in the participants (6,882 men and 4,271 women) from 2011. In this population, serological testing for HBsAg and HCV-Ab was performed in 9,064 subjects. Among them, 147 subjects (98 men and 49 women) were positive for HbsAg and negative for HCV-Ab; 165 subjects (84 men and 81 women) were negative for HBsAg and positive for HCV-Ab, and four subjects (three men and one woman) were positive for both. For this analysis, DM was defined as treatment for DM, fasting blood glucose ≥126 mg/dl, or hemoglobin A1C ≥6.5 %.
Baseline characteristics and differences between the DM (−) and DM (+) groups are summarized in Table 1. The prevalence of DM was 13.3 % in men and 6.1 % in women. Mean age was significantly higher in the DM (+) group than in the DM (−) group among both men and women (both Ps < 0.001). For men and women, mean BMI and the prevalence of obesity were significantly higher in the DM (+) group than in DM (−) group (all Ps < 0.001). In addition, the prevalence of hypertension, dyslipidemia, and fatty liver in DM (+) subjects was significantly higher than in DM (−) subjects.
As for smoking status, DM (+) men had a significantly higher proportion of former smokers. Significant differences were not detected in women. DM (+) women had a significantly higher percentage of patients with no alcohol consumption. However, a significant difference was not detected in men.
As shown in Table 2, logistic regression analysis revealed that DM is independently associated with aging, obesity, hypertension, dyslipidemia, and fatty liver for both men and women. ORs (95 % CI) for fatty liver were 1.97 (1.66–2.32) in men and 3.12 (2.29–4.26) in women. This significant association between fatty liver and DM was detected even when subjects were limited to those who were HBsAg (−), HCV-Ab (−), and not on medication for hypertension and dyslipidemia [men, OR (95 % CI), 2.33 (1.78–3.05); women, 4.25 (2.51–7.20)]. In addition, positive associations between DM and former [OR (95 % CI), 1.22 (1.02–1.46)] and current smoking [1.42 (1.16–1.74)] were detected among men, but not among women [former smoking, OR (95 % CI), 1.46 (0.77–2.61); current smoking, 0.65 (0.19–1.64)]. Further, there was a negative association between DM and drinking alcohol ≥20 g/day [OR (95 % CI), 0.76 (0.60–0.96)] among men.
Fatty liver predicts future DM
The association between fatty liver and future DM was estimated (Table 3). Of 5,318 subjects (3,351 men and 1,967 women) who participated in both 2006 and 2011, 4,842 did not have DM in 2006. Of this group, 631 subjects (496 men and 135 women) were diagnosed with DM as of 2011. When the risk for DM in 2011 was estimated by logistic regression analysis using the variables in Table 3 and age as co-variables, only fatty liver [OR (95 % CI), 1.64 (1.13–2.41) in men, 2.83 (1.51–5.46) in women] and obesity [OR (95 % CI), 4.12 (2.53–6.93) in men, 4.89 (2.19–11.80) in women] in 2006 independently predicted the presence of DM in 2011. In this population, serological testing for HBsAg and HCV-Ab was performed in 4,480 subjects, and 93 subjects (60 men and 33 women) were positive for HbsAg and negative for HCV-Ab, while 93 subjects (45 men and 49 women) were negative for HBsAg and positive for HCV-Ab, and one subject (male) was positive for both in 2006. When subjects were limited to those who were HBsAg (−), HCV-Ab (−), and not on medication for hypertension and dyslipidemia, similar results were obtained: fatty liver and obesity in 2006 independently predicted the presence of DM in 2011. ORs (95 % CI) for fatty liver were 1.76 (1.11–2.80) in men and 1.84 (0.85–4.22) in women, respectively.
The prevalence of both fatty liver and DM increased in the past 20 years
Characteristic features of subjects in 1991, 1996, 2001, 2006, and 2011 are summarized in Table 4 and Fig. 1. In this analysis, DM was defined as patients under treatment for DM, fasting blood glucose ≥126 mg/dl, or both. The mean age of enrolled subjects gradually rose among both men and women (Table 4, P < 0.001 for both). There was a significant difference in BMI across the five groups among men (Table 4, P < 0.001). The prevalence of obesity also increased significantly among men (Fig. 1a, P for trend <0.001). On the contrary, both BMI (Table 1, P < 0.001) and the prevalence of obesity (Fig. 1a, P for trend <0.001) decreased significantly among women.
Rates of change in the prevalence of fatty liver and the components of the metabolic syndrome. a All subjects. b Subjects who consumed ≤20 g of ethanol per day. Data are expressed as percentages relative to 1991 values. P* and P for trend** values were obtained using the chi-square test and the Cochran–Armitage test, respectively. In this analysis, diabetes mellitus (DM) was defined as patients undergoing treatment for DM or blood glucose ≥126 mg/dl. HT hypertension, DL dyslipidemia
The prevalence of DM approximately doubled during the past 20 years among both men (P for trend <0.001) and women (P for trend =0.003) (Fig. 1a). Differences were significant even after matching for the 10-year age bracket among both men (Mantel–Haenszel test, P < 0.001) and women (Mantel–Haenszel test, P = 0.044) or for body composition among both men and women (Mantel–Haenszel test, both Ps < 0.001). The prevalence of hypertension increased significantly among men (P for trend <0.001), but not women (P = 0.181). On the contrary, the prevalence of DL increased significantly among women (P for trend <0.001), but did not among men (P for trend =0.441) (Fig. 1a).
The prevalence of fatty liver increased significantly in both men and women (Fig. 1a, both Ps for trend <0.001). Significant differences were observed even after matching for age and body composition, respectively, among both men and women (Mantel–Haenszel test, all Ps < 0.001). The prevalence of current smokers decreased among men (P < 0.001), but the prevalence of non-smokers decreased among women (P < 0.001) (Table 4). The prevalence of light alcohol consumption (ethanol <20 g/day) increased significantly among both men and women (Table 4, both Ps < 0.001). As shown in Fig. 1b, only the prevalence of fatty liver and DM increased significantly among both men and women during the examined time frame, even when subjects were limited to those who did not consume more than 20 g of ethanol per day.
Discussion
The present study showed that the prevalence of DM had approximately doubled among both men and women during the examined period. A significant difference was observed even after matching by age bracket. Thus, the prevalence of DM certainly increased, even considering Japan's systemic problem of decreasing birthrate and aging society. Obesity has been recognized as the major driving force in the development of DM. However, the prevalence of obesity decreased significantly among women. Significant differences in the prevalence of DM were detected from 1991 to 2011, even after matching for body composition. It seems possible that some factor other than obesity is needed to explain the recent increasing prevalence of DM.
Obesity may play a central role in the pathogenesis of fatty liver [16, 17] and DM [2, 3]. On the other hand, Kantartzis et al. [18] reported that the amount of fat in the liver increases steeply as one moves from normal glucose tolerance towards isolated impaired fasting glucose (IFG), isolated impaired glucose tolerance (IGT), or both, even more so than with visceral fat. Previous epidemiological studies have reported that fatty liver is an independent predictor of DM [6–10]. In the present study, we also demonstrated this relationship using cross-sectional (Table 2) and longitudinal (Table 3) analyses. In addition, we provided evidence from a viewpoint that differs from previous studies in that the prevalence of only fatty liver and DM increased significantly among both men and women during the long time period examined (Fig. 1). Considering our results in an integrated fashion, we strongly suspect that the prevalence of DM has increased in association with an increasing prevalence of fatty liver.
Empirically, it is recognized that some lifestyle conditions exacerbate both fatty liver and DM, even without body weight gain. Late-night snacking is an example. Recently, when the unique mechanism of insulin receptor substrate (IRS)-2 expression in the liver was revealed, it offered a possible explanation as to why late-night snacking is harmful. Late-night snacking may give rise to prolonged activation of sterol regulatory element binding protein (SREBP)-1c, which not only promotes de novo lipid synthesis but also suppresses the expression of IRS-2 protein [19, 20]. The action of insulin via hepatic IRS-2, including the suppression of gluconeogenesis, becomes inadequate, resulting in hyperglycemia. Unbalanced diets containing excess carbohydrates, especially fructose, may also cause both fatty liver and DM [21, 22]. One major mechanism may be that carbohydrates stimulate hepatic lipogenesis via the activation of carbohydrate response element binding protein and SREBP-1c. Cholesterol is also reported to activate the SREBP-1c pathway in the liver, resulting into hepatic steatosis even in non-obese individuals [23]. We consider that some lifestyle changes, such as diet, have been occurring in Japan, in which impaired liver metabolism results in not only hepatic steatosis but also in the progression of DM, regardless of obesity. In addition, an association between hepatokines, such as fetuin-A [11, 12], selenoprotein P [13, 14], and fibroblast growth factor 21 [24], insulin resistance, and type 2 DM has been reported. It is possible that hepatokines play a role in the scenario where the presence of fatty liver influences the development of DM.
We previously reported that cigarette smoking may be a risk factor for fatty liver [25]. In addition, it had been reported elsewhere that smoking is an independent predictor of DM [26]. In the present study, the risk for DM was significantly higher in men who are current and former smokers compared to men who have never smoked (Table 2). During the time frame examined, the prevalence of men who were current smokers decreased, and the number of men that were former smokers increased by the same amount. So the influence of smoking status seems to be small, if any, because the overall prevalence of current plus former smokers did not change. Among women, the prevalence of current plus former smokers increased. Therefore, it is possible that a change in smoking status influenced the prevalence of DM in women. In addition, it is well-known that smoking cessation can lead to substantial weight gain, which is associated with increases in both fatty liver [25] and DM [27]. Therefore, additional analysis is needed to clarify this issue.
Alcohol consumption is also a lifestyle factor that is relevant to the risk of fatty liver and DM. We previously reported an inverse association between alcohol consumption and fatty liver [28]. Several studies have reported a J-shaped or U-shaped association between alcohol consumption and DM [29]. Some investigators reported that moderate alcohol intake plays a protective role against fatty liver, but not the metabolic syndrome [30]. In the present study, similar results were obtained, whether the subjects included all enrolled individuals (Fig. 1a) or only those with less than or equal to 20 g of alcohol consumption daily (Fig. 1b). Although drinking habits may have changed during the past 20 years in Japan, it seems unlikely that trends in alcohol consumption contribute to the increasing prevalence of DM.
There are several limitations in the present study. First, fatty liver was diagnosed using ultrasonography. Diagnosis by ultrasonography may overlook a subset of advanced AFLD or NAFLD, sometimes called “burnt-out steatohepatitis,” in which there is less fatty steatosis. In addition, the diagnostic ability of ultrasonography had improved in the past 20 years. However, the prevalence of fatty liver in the present study was similar to those reported elsewhere in Japan [31]. Second, DM was defined by the presence of treatment for DM, fasting glucose levels (with or without hemoglobin A1C), or both, which may be insufficient to represent the whole spectrum of DM. Third, analyses were carried out using age, body composition based on BMI, smoking status, alcohol consumption, and the presence of hypertension, dyslipidemia, and fatty liver as parameters. It is possible that additional factors for which we did not adjust may have influenced the results. For example, it is insufficient to estimate the influence of visceral obesity only using BMI. In addition, weight gain or loss, rather than absolute body weight, may influence the development of fatty liver and DM. It might be important to gather information on physical activity and diet. However, this information was not available in our study. Finally, there is no information on medication use; some medicines, such as angiotensin II receptor blockers and pioglitazone, are known to reduce levels of hepatic steatosis and insulin resistance.
In conclusion, the prevalence of DM has been increasing during the last 20 years in a Japanese population, regardless of body composition. Fatty liver might play a pivotal role in this increasing prevalence of DM. In addition to measures against obesity, it seems worthwhile to explore a strategy against fatty liver. Further studies are needed to better understand the pathogenesis of DM and management strategies for DM with respect to fatty liver.
References
Kawamori R. Diabetes trends in Japan. Diabetes Metab Res Rev. 2002;18:S9–13.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
The Examination Committee of Criteria for. “Obesity disease” in Japan, Japanese Society for the Study of Obesity, New criteria for “obesity disease” in Japan. Circ J. 2002;66:987–92.
Gribble FM. Metabolism: a higher power for insulin. Nature. 2005;434:965–6.
Eguchi Y, Hyogo H, Ono M, Mizuta T, Ono N, Fujimoto K, et al. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study. J Gastroenterol. 2012;47:586–95.
Hanley AJ, Williams K, Festa A, Wagenknecht LE, D’Agostino RB Jr, Kemph J, et al. Elevation in Markers of Liver Injury and Risk of Type 2 Diabetes. The Insulin Resistance Atherosclerosis Study. Diabetes. 2004;53:2623–32.
Adams LA, Waters OR, Knuiman MW, Elliott RR, Olynyk JK. NAFLD as a risk factor for the development of diabetes and the metabolic syndrome: an eleven-year follow-up study. Am J Gastroenterol. 2009;104:861–7.
Yamada T, Fukatsu M, Suzuki S, Wada T, Yoshida T, Joh T. Fatty liver predicts impaired fasting glucose and type 2 diabetes mellitus in Japanese undergoing a health checkup. J Gastroenterol Hepatol. 2009;25:352–6.
Parl SK, Seo MH, Shin HC, Ryoo J-H. Clinical availability of nonalcoholic fatty liver disease as an early predictor of type 2 diabetes mellitus in Korean men; 5-year prospective cohort study. Hepatology. 2013;57:1378–83.
Mori K, Emoto M, Yokoyama H, Arali T, Teramura M, Koyama H, et al. Association of serum fetuin-A with insulin resistance in type 2 diabetic and nondiabetic subjects. Diabetes Care. 2006;29:468.
Pal D, Dasgupta S, Kundu R, Maitra S, Das G, Mukhopadhyay S, et al. Fetuin-A acts as an endogenous ligand of TLR 4 to promote lipid induced insulin resistance. Nat Med. 2012;18:1279–85.
Misu H, Takamura T, Takayama H, Hayashi H, Matuzawa-Nagata N, Kurita S, et al. A liver-derived secretory protein, selenoprotein P, causes insulin resistance. Cell Metab. 2010;12:483–95.
Takamura T, Misu H, Ota T, Kaneko S. Fatty liver as a consequence and cause of insulin resistance: lessons from type 2 diabetic liver. Endocr J. 2012;59:745–63.
Kashiwagi A, Kasuga M, Araki E, Oka Y, Hanafusa T, Ito H, et al. International clinical harmonization of glycerated hemoblobin in Japan. From Japan Diabetes Society to National Glycohemoglobin Standardization Program Values. Diabetol Int. 2012;3:8–10.
Eguchi Y, Eguchi T, Mizuta T, Ide Y, Yasutake T, Iwakiri R, et al. Visceral fat accumulation and insulin resistance are important factors in nonalcoholic fatty liver disease. J Gastroenterol. 2006;41:462–9.
Imamura Y, Uto H, Oketani M, Hosoyamada K, Sho Y, Hiwaki T, et al. Assocition between changes in body composition and the increasing prevalence of fatty liver in Japanese men. Hepatol Res. 2008;38:1083–6.
Kantartzis K, Machann J, Schick F, Fritsche A, Häring HU, Stefan N. The impact of liver fat vs visceral fat in determining categories of prediabetes. Diabetologia. 2009;53:882–9.
Shimano H. SREBP-1c and TFE3, energy transcription factors that regulate hepatic insulin signaling. J Mol Med. 2007;85:437–44.
Kubota N, Kubota T, Itoh S, Kumagai H, Kozono H, Takamoto I, et al. Dynamic functional relay between insulin receptor substrate 1 and 2 in hepatic insulin signaling during fasting and feeding. Cell Metab. 2008;8:49–64.
Ouyang X, Cirillo P, Sautin Y, MaCall S, Bruchette JL, Diehl AM, et al. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J Hepatol. 2008;48:993–9.
Stanfope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest. 2009;119:1322–34.
Enjoji M, Nakamuta M. Is the control of dietary intake sufficiently effective to ameliorate nonalcoholic fatty liver disease? World J Gastroentrol. 2010;16:800–3.
Cicione C, Deqirolamo C, Moschetta A. Emerging role of fibroblast groth factor 15/19 and 21 as metabolic integrators in the liver. Hepatology. 2012;56:2404–11.
Hamabe A, Uto H, Imamura Y, Kusano K, Mawatari S, Kumagai K, et al. Impact of cigarette smoking on onset of nonalcoholic fatty liver disease: a 10-year longitudinal study. J Gastroenterol. 2011;46:769–78.
Will JC, Galuska DA, Ford ES, Kokdad A, Calle EE. Cigarette smoking and diabetes mellitus: evidence of a positive association from a large prospective cohort study. Int J Epidemiol. 2001;30:540–6.
Yeh HC, Duncan BB, Schmidt MI, Wang NY, Brancati FL. Smoking, smoking cessation, and risk for type 2 diabetes mellitus: a cohort study. Ann Inter Med. 2010;152:10–7.
Hiramine Y, Imamura Y, Uto H, Koriyama C, Horiuchi M, Oketani M, et al. Alcohol drinking patterns and the risk of fatty liver in Japanese men. J Gastroenterol. 2011;46:519–28.
Koppes LL, Dekker JM, Hendriks HF, Bouter LM, Heine RJ. Moderate Alcohol Consumption Lowers the Risk of Type 2 Diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 2005;28:719–25.
Hamaguchi M, Kojima T, Ohbora A, Takeda N, Fukui M, Kato T. Protective effect of alcohol consumption for fatty liver but not metabolic syndrome. World J Gastroenterol. 2012;18:156–67.
Kojima S, Watanabe N, Numata M, Ogawa T, Matsuzaki S. Increase in the prevalence of fatty liver in Japan over the past 12 years. J Gastroenterol. 2003;38:954–61.
Acknowledgments
This work was supported in part by grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan (No. 23590981), and the Ministry of Health, Labour and Welfare of Japan (H20-Hepatitis-general-008).
Conflict of interest
HT holds endowed faculty positions in research for HGF tissue repair and regenerative medicine, and has received funds from Eisai Co., Ltd. The other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Imamura, Y., Uto, H., Hiramine, Y. et al. Increasing prevalence of diabetes mellitus in association with fatty liver in a Japanese population. J Gastroenterol 49, 1406–1413 (2014). https://doi.org/10.1007/s00535-013-0902-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-013-0902-2