Abstract
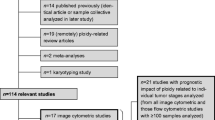
The biological characteristics of cancers depend mostly on genetic alterations in the cancer cells of individuals. Gastric cancers show a high frequency of DNA aneuploidy, a phenotype of chromosomal instability. Compared to diploid tumors, gastric carcinomas with aneuploidy have been shown to have high proliferative activity and high metastatic or invasive potential; these characteristics lead to a poor prognosis. It has been suggested that an abnormal spindle assembly checkpoint is involved in DNA aneuploidy, but the underlying mechanism is still unclear. This review, in order to determine whether gastric carcinomas that display aneuploidy are associated with a poorer prognosis than diploid tumors, and to discuss the biological mechanisms that induce aneuploidy, summarizes the results of studies on DNA ploidy in gastric cancer published in the English literature. Analysis of DNA ploidy in gastric cancer may provide clinically useful information from diagnostic, therapeutic, and prognostic standpoints. Further investigations may be needed to clarify the relationship between chromosome instability and DNA ploidy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is one of the most common causes of death among patients with malignant diseases around the world. DNA aneuploidy is one of the most frequent genetic aberrations in gastric cancer. However, the molecular mechanisms and roles of DNA aneuploidy are controversial topics. Because fresh biopsy samples or resected specimens can be obtained from gastric cancers, various genetic analyses have been conducted on samples collected worldwide. Gastric cancer is a chronic proliferative disease with multiple genetic and epigenetic alterations [1, 2]. This review summarizes the genetic and chromosomal alterations that have been found in gastric cancer. We focus on aneuploidy in particular, give an outline of the mechanisms involved in the development of aneuploidy, and discuss the significance and future of research on DNA aneuploidy in gastric cancer.
Genetic alterations in gastric cancer
Multiple genetic and epigenetic alterations in oncogenes, tumor suppressor genes, cell-cycle regulators, cell adhesion molecules, DNA repair genes, genetic instability factors, and telomerase activation are implicated in the multistep process of gastric carcinogenesis. The specific combination of alterations differs in the 2 histological types of gastric cancer, suggesting that intestinal-type and diffuse-type carcinomas have distinct carcinogenetic pathways. Chromosomal instability (CIN); in particular, loss of heterozygosity (LOH), genomic amplifications, and DNA aneuploidy, are frequently observed in intestinal-type gastric carcinoma [3, 4]. Numerical abnormalities in specific chromosomes have been reported for chromosomes 1, 7, 8, 9, 17, 20, X, and Y in gastric tumors [5]. Although the relationship between the numerical abnormality in each chromosome and gastric carcinogenesis has not been elucidated, several reports have demonstrated that aneuploidy is related to cancer progression. Alterations in chromosome 17 have been shown to be related to tumor progression and malignant potential in primary gastric cancer [6], and numerical abnormalities in chromosomes 3, 10, 11, 12, 17, and Y have also been shown to cause dramatic differences in outcomes [7]. Wu et al. [8], in a comparative genomic hybridization analysis, reported that frequent abnormalities were found in advanced cancers, including gains on the 8q chromosomal arm and losses on the 16q chromosomal arm. Other combinations of gains and losses have also been reported [9]. LOH is the deletion of one allele among paired chromosomes. LOH on chromosome 6 could be associated with an unfavorable prognosis [10]. Simultaneous alteration showing LOH on chromosome 16q and gains on 8q was also reported to result in poor outcomes [11].
Tumor suppressor gene mutations or LOH have been reported in over half of all human cancers, and they appear to occur in the early stages of cancer, indicating the important role that such mutations may play in the carcinogenesis of various organs [12]. LOH of the gene encoding phosphate and tensin homolog (PTEN) was observed in 17.1% of patients diagnosed with gastric cancer in our previous analysis [13]. p53 mutations were also found in more than 20% of gastric cancer samples, accompanied by LOH [12]. Genetic instability has long been considered an integral component of human neoplasias. In a small fraction of tumors, mismatch repair (MMR) deficiency leads to microsatellite instability (MSI) at the nucleotide sequence level [14]. In other tumors, an abnormal chromosome number (aneuploidy) has suggested genomic instability, but the nature and magnitude of the postulated instability are still matters of conjecture [15]. MSI is manifested as length variation in microsatellite sequences caused by MMR gene deficiency; MSI is found in around 20% of gastric cancer patients [16–20]. Gastric cancer with high-frequency MSI (MSI-H) represents a well-defined subset of carcinomas showing distinctive clinicopathological features. In colon cancer, tumors with MSI-H are characteristic of hereditary nonpolyposis colorectal cancer syndrome, which, in the majority of cases, is associated with an early age of onset and is caused by germline mutations in one of the MMR genes [21–24]. In contrast, the MSI-H phenotype in gastric cancer is predominantly caused by epigenetic hypermethylation of the hMLH1 MMR gene rather than being caused by germline mutations in one of the MMR genes [14, 25–27]. Aneuploidy is known to be associated with non-MSI tumors in both colon cancer and gastric cancer [28–31].
What is DNA aneuploidy?
DNA aneuploidy is a state in which cells have an abnormal number of chromosomes. Usually, CIN has been divided into numerical CIN and structural CIN forms. Numerical CIN includes DNA amplification and an abnormal number of chromosomes, and structural CIN includes DNA translocation and LOH. The term “DNA aneuploidy” means an abnormal number of chromosomes, but recently the term has been used to indicate both forms of CIN in a wide sense (Table 1). More than a century ago, David Paul Hansemann observed that cancer cells generally had an abnormal number of chromosomes [32]. In 1997, Lengauer et al. [15] reported that DNA aneuploidy was seen in 85% of colorectal cancers. This form of CIN is thought to reflect a continuing cellular defect that persists throughout the lifetime of the cancer cell and is independent of MSI, a recessive trait [15]. DNA aneuploidy is an important phenotypic characteristic of cancer cells; however, whether or not DNA aneuploidy may be a cause of carcinogenesis is still controversial. Recent evidence indicates that persistent missegregation of chromosomes results in gains and losses of chromosomes and may be an important cause of aneuploidy. This form of chromosome instability may contribute to tumor development and progression by facilitating LOH and the phenotypic expression of mutated tumor suppressor genes by favoring polysomy of chromosomes that harbor oncogenes [33]. Single nucleotide polymorphism array techniques can reveal all chromosomal alterations. DNA from aneuploid tumors shows alterations in almost all chromosomes, including DNA amplification and LOH (Fig. 1). Kawaguchi et al. [34] have reported that DNA aneuploidy is linked with gain of 8p23 and loss of 22q11 in gastric cancers. Gain or loss of specific chromosomal regions might have enough of an impact to generate the aneuploid phenotype. DNA aneuploidy is less frequent in early gastric cancer. Therefore, previous studies of early gastric cancers suggested that in pure diploid superficial carcinomas, genetic instability might lead to a cell clone that has undergone a ploidy shift, becoming more aggressive [35–37]. However, DNA ploidy in advanced gastric carcinoma is less heterogeneous than that in early gastric cancer. These observations suggest that gastric cancer tumor progression leads to the development of a dominant and more aggressive aneuploid cell clone [37]. Sasaki et al. [38] have shown that there is heterogeneity even in intramural gastric cancer. In addition, these results support the notion that aneuploid cells are generated from tumor stem cells, which selectively expand as aggressive tumors [39, 40].
Typical results of single nucleotide polymorphism arrays in gastric cancer. The left panel shows the result of single nucleotide polymorphism (SNP) arrays of DNA from diploid gastric cancers. The right panel shows the result of SNP arrays of DNA from aneuploid gastric cancers. There are numerous chromosomal changes in the left panel
Gastric cancer and DNA aneuploidy
DNA aneuploidy in gastric cancer has been reported since the 1980s [41]. Well-differentiated and moderately differentiated carcinomas display aneuploid patterns more frequently than poorly differentiated tumors [4, 42–45], though some reports have not agreed with that conclusion [36, 46].
Adenocarcinoma of the proximal portion of the stomach [gastroesophageal (GE) junction and cardia] is increasing in incidence. DNA aneuploidy is more common in GE-cardia tumors than in body-antrum tumors [47], and tumors displaying DNA aneuploidy have a greater proliferative activity, correlating with the Ki-67 index [44, 48]. Gastric adenoma, chronic gastritis, and intestinal metaplasia have also been investigated using flow cytometry [49], and these conditions show frequent chromosomal alterations [3], while none of the normal mucosae show aneuploidy [50]. DNA ploidy has also been reported in patients with primary gastric lymphoma. However, the impact of DNA ploidy on survival is still controversial [51, 52].
Is DNA aneuploidy a prognostic factor for gastric cancer?
Aneuploidy, as detected by flow cytometry, has been demonstrated as a useful prognostic marker during the progression of gastric carcinogenesis, due to the high proliferative activity associated with these tumors, leading to increased metastatic potential, poor prognosis, and shorter survival rates than rates in patients with diploid tumors [48, 53]. To date, numerous reports have been published that demonstrate the importance of DNA aneuploidy in gastric cancer (Table 2). Almost all of these reports have shown that DNA aneuploidy is associated with the prognosis of gastric cancer. However, the clinical impact of aneuploidy is debatable [54]. DNA aneuploidy is significantly correlated with lymph node metastasis, but not with tumor penetration [48, 55–57]. Although their case volume was low, Nesi et al. [58], in a prospective study, showed that aneuploidy was a prognostic factor in gastric cancer. Furthermore, even in multivariate analysis, DNA ploidy has been shown to be a prognostic factor [51, 59, 60]. However, some reports have demonstrated that DNA aneuploidy might be associated with a significantly shorter survival only in patients with intestinal-type tumors [61] or only in patients with diffuse-type cancer [62]. Taken together, this evidence strongly supports the hypothesis that aneuploidy is associated with the prognosis of gastric cancer.
Molecular mechanisms of DNA aneuploidy in gastric cancer
Defects in two distinct processes are considered to be the main causes of aneuploidy; namely, a failure in the centrosome-duplication cycle leading to multiple centrosomes, and a dysregulation of the cell division control machinery resulting in lagging chromosomes, mainly elicited by a weakened or an over-activated mitotic checkpoint also known as the spindle assembly checkpoint [63]. Figure 2 shows the spindle checkpoint kinases and chromosomal separation. This checkpoint is the mechanism that delays the separation of sister chromatids until all the chromosome kinetochores are correctly attached to the spindle.
Spindle checkpoint kinases and chromosomal separation. a In the mitotic stage, the spindle extends from both spindle poles to the kinetochore and adds tension to sister chromatids toward the 2 poles. If the tension applied to the sister chromatids is lacking in prometaphase, the mitotic checkpoint complex (MCC), formed by mitotic arrest deficient 2 (Mad2)-cell division cycle 20 (CDC20)-BUB-BUBR1, inactivates CDC20 and obstructs the separation of the chromosomes. b When there is equal tension, the MCC is removed, and CDC is activated. c Activated CDC20 stimulates the anaphase-promoting complex/cyclosome (APC/C), and activated APC/C polyubiquitylates and degrades securin, which inactivates separase. d Finally, separase cuts cohesin, which connects sister chromatids, and the chromosome is separated
BUB1 is a human homolog of the yeast mitotic checkpoint gene that plays an important role in chromosome segregation. Mutations in BUB1 have not been found in gastric cancer [64], but the protein encoded by BUB1, BUBR1, is overexpressed in gastric cancer [65–68]. We studied the expression of BUBR1 by immunohistochemistry in 181 gastric cancer samples. Ninety-one (50.3%) cases had high expression of BUBR1, and those cases were significantly correlated with the presence of DNA aneuploidy (P < 0.05). Also, high expression of BUBR1 was significantly correlated with deep invasion, lymph node metastasis, liver metastasis, and poor prognosis [65]. Transfection of gastric cancer cell lines with full-length BUBR1 resulted in changes to the ploidy pattern. BUBR1 forms a complex with Bub3, mitotic arrest deficient 2 (Mad2), and cell division cycle 20 (CDC20) at the spindle assembly checkpoint, thus inhibiting CDC20 activity [69]. In gastric cancer cells with high BUBR1 expression, the formation of this complex might be compromised, and the spindle assembly checkpoint may be overridden, resulting in DNA aneuploidy. In contrast, the overexpression of MAD2 in gastric cancer is not associated with aneuploidy or with any of the disease’s clinicopathological characteristics [70]. However, mutations in the MAD2 gene were reported in gastric cancer, and overexpression of mutant Mad2 in HeLa cells led to the appearance of aneuploid cells [66]. We investigated the relationship between Mad2 expression and aneuploidy. Aneuploidy in gastric cancer was significantly correlated with high expression of Mad2 protein (unpublished data), and Mad2 overexpression was found in gastric tumors harboring p53 mutations, indicating that p53 mutations may cause the upregulation of Mad2 and result in the generation of aneuploid cells within the tumor. The tumor-amplified kinase BTAK was cloned from breast cancer cells and mapped on chromosome 20q13 as a target gene for this amplification in human breast cancers. Transfection of BTAK in near-diploid gastric cancers induced the formation of another aneuploid cell population as well [71].
Helicobacter pylori infection
H. pylori infections have been reported to be associated with changes in DNA content and cellular proliferative activity [72, 73]. Chronic H. pylori infections were shown to be responsible for genomic instability in a subset of cases of H. pylori-positive chronic atrophic gastritis, and eradication of H. pylori infections might reverse genomic instability [74, 75]. Aneuploidy levels increased incrementally across the histological series from patients with gastritis to those with H. pylori-positive gastritis and those with atrophy/intestinal metaplasia (IM) [76, 77]. Methylation at E-cadherin was detected in patients with H. pylori infections, and H. pylori eradication therapy could reverse methylation in patients with chronic gastritis [78]. In diffuse gastric carcinoma, despite common E-cadherin gene (CDH1) mutations, CDH1 LOH was absent from most tumors [79–81]. CDH1 promoter methylation was found to be the second hit in more than half of the sporadic diffuse gastric carcinoma cases harboring CDH1 mutations [79]. E-cadherin methylation is an early event in gastric carcinogenesis and can be initiated by H. pylori infection. H. pylori eradication therapy could reverse the methylation [78, 82]. The relationship between p16 methylation and H. pylori infections in precancerous gastric lesions was also investigated in a population-based study in China. The study showed that p16 methylation was significantly associated with H. pylori infections in precancerous gastric lesions [83].
Relationship between p53 mutations and DNA aneuploidy
Tumor-suppressor proteins such as p53, APC, and RB have been described to combine key regulatory functions of signaling pathways with protection from CIN [63]. Aneuploidy and inactivation of p53 frequently coincide in human cancers, but increasing evidence has shown that loss of p53 by itself is not the primary cause of aneuploidy [84]. The relationship between DNA ploidy and p53 mutations is still controversial [85]. 17p (p53) LOH and increased 4N or aneuploidy are closely associated with the early stages of gastric carcinogenesis [86]. A significant association was also found between increased 4N or aneuploidy and 17p (p53) LOH in all precancerous gastric lesions. However, no association between H. pylori infection and 17p (p53) LOH or increased 4N/aneuploidy in precancerous gastric lesions was reported. Recent analysis showed that LOH without copy number changes at the p53 locus was observed in p53 mutant esophageal squamous cell carcinomas. This copy-neutral LOH might be the major mechanism for inactivation of the intact allele in esophageal squamous cell carcinogenesis associated with p53 mutations [87]. Our data suggest that copy-neutral LOH, occurring because of CIN, might be the major mechanism for inactivation of the intact allele in esophageal squamous cell carcinogenesis associated with p53 mutations. Crypt isolation has enabled the separation of tumor tissues from stromal tissues, and thus, the DNA content in tumor cells can be accurately assessed [88, 89]. Furthermore, S-phase fractions were found to be more useful indicators than DNA aneuploidy if the crypt isolation method was used [88]. Another report clearly showed that diploid tumors generally did not display LOH or MSI, whereas, using the crypt isolation technique, it was found that aneuploid and multiploid tumors were associated with LOH and MSI [28].
Future perspectives
DNA aneuploidy is associated with the carcinogenesis and prognosis of gastric cancer. Therefore, there has been considerable interest in targeting cell-cycle checkpoints, particularly in emerging and alternative anticancer strategies [90]. Several molecules that inhibit cell-cycle kinases have been developed and clinically screened as potential anticancer agents, but none of these agents has been approved for commercial use [90]. The development of selection markers that lead to the choice of appropriate therapies for patients will be the primary focus of future research. Such development may lead to new treatments for gastric cancer in the future.
References
Yasui W, Oue N, Aung PP, Matsumura S, Shutoh M, Nakayama H. Molecular-pathological prognostic factors of gastric cancer: a review. Gastric Cancer. 2005;8(2):86–94.
Yasui W, Oue N, Ito R, Kuraoka K, Nakayama H. Search for new biomarkers of gastric cancer through serial analysis of gene expression and its clinical implications. Cancer Sci. 2004;95(5):385–92.
Kim YH, Kim NG, Lim JG, Park C, Kim H. Chromosomal alterations in paired gastric adenomas and carcinomas. Am J Pathol. 2001;158(2):655–62.
Sugai T, Nakamura S, Uesugi N, Habano W, Yoshida T, Tazawa H, et al. Role of DNA aneuploidy, overexpression of p53 gene product, and cellular proliferation in the progression of gastric cancer. Cytometry. 1999;38(3):111–7.
Panani AD. Cytogenetic and molecular aspects of gastric cancer: clinical implications. Cancer Lett. 2008;266(2):99–115.
Terada R, Yasutake T, Yamaguchi E, Hisamatsu T, Nakamura S, Ayabe H, et al. Higher frequencies of numerical aberrations of chromosome 17 in primary gastric cancers are associated with lymph node metastasis. J Gastroenterol. 1999;34(1):11–7.
Kitayama Y, Igarashi H, Watanabe F, Maruyama Y, Kanamori M, Sugimura H. Nonrandom chromosomal numerical abnormality predicting prognosis of gastric cancer: a retrospective study of 51 cases using pathology archives. Lab Invest. 2003;83(9):1311–20.
Wu MS, Chang MC, Huang SP, Tseng CC, Sheu JC, Lin YW, et al. Correlation of histologic subtypes and replication error phenotype with comparative genomic hybridization in gastric cancer. Genes Chromosomes Cancer. 2001;30(1):80–6.
Hidaka S, Yasutake T, Kondo M, Takeshita H, Yano H, Haseba M, et al. Frequent gains of 20q and losses of 18q are associated with lymph node metastasis in intestinal-type gastric cancer. Anticancer Res. 2003;23(4):3353–7.
Koo SH, Jeong TE, Kang J, Kwon KC, Park JW, Noh SM. Prognostic implications for gastric carcinoma based on loss of heterozygosity genotypes correlation with clinicopathologic variables. Cancer Genet Cytogenet. 2004;153(1):26–31.
Suzuki S, Egami K, Sasajima K, Ghazizadeh M, Shimizu H, Watanabe H, et al. Comparative study between DNA copy number aberrations determined by quantitative microsatellite analysis and clinical outcome in patients with stomach cancer. Clin Cancer Res. 2004;10(9):3013–9.
Oki E, Zhao Y, Yoshida R, Egashira A, Ohgaki K, Morita M, et al. The difference in p53 mutations between cancers of the upper and lower gastrointestinal tract. Digestion. 2009;79(Suppl 1):33–9.
Oki E, Kakeji Y, Baba H, Tokunaga E, Nakamura T, Ueda N, et al. Impact of loss of heterozygosity of encoding phosphate and tensin homolog on the prognosis of gastric cancer. J Gastroenterol Hepatol. 2006;21(5):814–8.
Oki E, Kakeji Y, Zhao Y, Yoshida R, Ando K, Masuda T, et al. Chemosensitivity and survival in gastric cancer patients with microsatellite instability. Ann Surg Oncol. 2009;16(9):2510–5.
Lengauer C, Kinzler KW, Vogelstein B. Genetic instability in colorectal cancers. Nature. 1997;386(6625):623–7.
Falchetti M, Saieva C, Lupi R, Masala G, Rizzolo P, Zanna I, et al. Gastric cancer with high-level microsatellite instability: target gene mutations, clinicopathologic features, and long-term survival. Hum Pathol. 2008;39(6):925–32.
Lee HS, Choi SI, Lee HK, Kim HS, Yang HK, Kang GH, et al. Distinct clinical features and outcomes of gastric cancers with microsatellite instability. Mod Pathol. 2002;15(6):632–40.
Pinto M, Oliveira C, Machado JC, Cirnes L, Tavares J, Carneiro F, et al. MSI-L gastric carcinomas share the hMLH1 methylation status of MSI-H carcinomas but not their clinicopathological profile. Lab Invest. 2000;80(12):1915–23.
Wu CW, Chen GD, Jiang KC, Li AF, Chi CW, Lo SS, et al. A genome-wide study of microsatellite instability in advanced gastric carcinoma. Cancer. 2001;92(1):92–101.
Wu MS, Lee CW, Shun CT, Wang HP, Lee WJ, Chang MC, et al. Distinct clinicopathologic and genetic profiles in sporadic gastric cancer with different mutator phenotypes. Genes Chromosomes Cancer. 2000;27(4):403–11.
Cunningham JM, Christensen ER, Tester DJ, Kim CY, Roche PC, Burgart LJ, et al. Hypermethylation of the hMLH1 promoter in colon cancer with microsatellite instability. Cancer Res. 1998;58(15):3455–60.
Kang GH, Shim YH, Ro JY. Correlation of methylation of the hMLH1 promoter with lack of expression of hMLH1 in sporadic gastric carcinomas with replication error. Lab Invest. 1999;79(7):903–9.
Oki E, Oda S, Maehara Y, Sugimachi K. Mutated gene-specific phenotypes of dinucleotide repeat instability in human colorectal carcinoma cell lines deficient in DNA mismatch repair. Oncogene. 1999;18(12):2143–7.
Thibodeau SN, French AJ, Cunningham JM, Tester D, Burgart LJ, Roche PC, et al. Microsatellite instability in colorectal cancer: different mutator phenotypes and the principal involvement of hMLH1. Cancer Res. 1998;58(8):1713–8.
Bevilacqua RA, Simpson AJ. Methylation of the hMLH1 promoter but no hMLH1 mutations in sporadic gastric carcinomas with high-level microsatellite instability. Int J Cancer. 2000;87(2):200–3.
Fleisher AS, Esteller M, Wang S, Tamura G, Suzuki H, Yin J, et al. Hypermethylation of the hMLH1 gene promoter in human gastric cancers with microsatellite instability. Cancer Res. 1999;59(5):1090–5.
Leung SY, Yuen ST, Chung LP, Chu KM, Chan AS, Ho JC. hMLH1 promoter methylation and lack of hMLH1 expression in sporadic gastric carcinomas with high-frequency microsatellite instability. Cancer Res. 1999;59(1):159–64.
Sugai T, Habano W, Jiao YF, Suzuki M, Takagane A, Nakamura S. Analysis of genetic alterations associated with DNA diploidy, aneuploidy and multiploidy in gastric cancers. Oncology. 2005;68(4–6):548–57.
Sinicrope FA, Rego RL, Halling KC, Foster N, Sargent DJ, La Plant B, et al. Prognostic impact of microsatellite instability and DNA ploidy in human colon carcinoma patients. Gastroenterology. 2006;131(3):729–37.
Tang R, Changchien CR, Wu MC, Fan CW, Liu KW, Chen JS, et al. Colorectal cancer without high microsatellite instability and chromosomal instability—an alternative genetic pathway to human colorectal cancer. Carcinogenesis. 2004;25(5):841–6.
Toft NJ, Curtis LJ, Sansom OJ, Leitch AL, Wyllie AH, te Riele H, et al. Heterozygosity for p53 promotes microsatellite instability and tumorigenesis on a Msh2 deficient background. Oncogene. 2002;21(41):6299–306.
Bignold LP, Coghlan B, Jersmann H. David Paul Hansemann: chromosomes and the origin of the cancerous features of tumor cells. Cell Oncol. 2009;31(1):61.
Pihan GA, Doxsey SJ. The mitotic machinery as a source of genetic instability in cancer. Semin Cancer Biol. 1999;9(4):289–302.
Kawauchi S, Furuay T, Uchiyama T, Adachi A, Okada T, Nakao M, et al. Genomic instability and DNA ploidy are linked to DNA copy number aberrations of 8p23 and 22q11.23 in gastric cancers. Int J Mol Med. 2010;26(3):333–9.
Brito MJ, Filipe MI, Williams GT, Thompson H, Ormerod MG, Titley J. DNA ploidy in early gastric carcinoma (T1): a flow cytometric study of 100 European cases. Gut. 1993;34(2):230–4.
Kim JM, Lee DK, Kim YK, Baik SK, Lee CI, Kwon SO, et al. DNA analysis by flow cytometry in early gastric cancer. Korean J Intern Med. 1997;12(2):137–43.
Osterheld MC, Caron L, Demierre M, Laurini R, Bosman FT. DNA-ploidy in advanced gastric carcinoma is less heterogeneous than in early gastric cancer. Cell Oncol. 2004;26(1–2):21–9.
Sasaki O, Soejima K, Haraguchi Y. DNA ploidy in undifferentiated carcinomas of the human stomach-with special reference to its heterogeneity and the relation between its intratumor distribution pattern and prognosis. In Vivo. 1993;7(4):363–7.
Liang Y, Zhong Z, Huang Y, Deng W, Cao J, Tsao G, et al. Stem-like cancer cells are inducible by increasing genomic instability in cancer cells. J Biol Chem. 2009;285(7):4931–40.
Kusumbe AP, Bapat SA. Cancer stem cells and aneuploid populations within developing tumors are the major determinants of tumor dormancy. Cancer Res. 2009;69(24):9245–53.
Petrova AS, Subrichina GN, Tschistjakova OV, Lukina TA, Weiss H, Wildner G. Flow cytofluorometry, cytomorphology and histology in gastric carcinoma. Oncology. 1980;37(5):318–24.
Omejc M, Repse S, Bracko M. Is DNA aneuploidy a prognostic factor in gastric cancer? Acta Chir Hung. 1997;36(1–4):266–9.
Lee KH, Lee JS, Suh C, Ahn MJ, Kim SW, Doh BS, et al. DNA flow cytometry of stomach cancer. Prospective correlation with clinicopathologic findings. Cancer. 1993;72(6):1819–26.
Kim JY, Cho HJ. DNA ploidy patterns in gastric adenocarcinoma. J Korean Med Sci. 2000;15(2):159–66.
Oda N, Tsujino T, Tsuda T, Yoshida K, Nakayama H, Yasui W, et al. DNA ploidy pattern and amplification of ERBB and ERBB2 genes in human gastric carcinomas. Virchows Arch B Cell Pathol Incl Mol Pathol. 1990;58(4):273–7.
Tosi P, Leoncini L, Cintorino M, Vindigni C, Minacci C, Nuti S, et al. Flow cytometric analysis of DNA ploidy pattern from deparaffinized formalin-fixed gastric cancer tissue. Int J Cancer. 1988;42(6):868–71.
Nanus DM, Kelsen DP, Niedzwiecki D, Chapman D, Brennan M, Cheng E, et al. Flow cytometry as a predictive indicator in patients with operable gastric cancer. J Clin Oncol. 1989;7(8):1105–12.
Sasaki O, Kido K, Nagahama S. DNA ploidy, Ki-67 and p53 as indicators of lymph node metastasis in early gastric carcinoma. Anal Quant Cytol Histol. 1999;21(1):85–8.
Odegaard S, Hostmark J, Skagen DW, Schrumpf E, Laerum OD. Flow cytometric DNA studies in human gastric cancer and polyps. Scand J Gastroenterol. 1987;22(10):1270–6.
Yasa MH, Bektas A, Yukselen V, Akbulut H, Camci C, Ormeci N. DNA analysis and DNA ploidy in gastric cancer and gastric precancerous lesions. Int J Clin Pract. 2005;59(9):1029–33.
Belessi CJ, Parasi AS, Manioudaki HS, Laoutaris NP, Legakis NC, Peros GT, et al. Prognostic impact of DNA ploidy pattern, S-phase fraction (SPF), and proliferating cell nuclear antigen (PCNA) in patients with primary gastric lymphoma. J Surg Oncol. 2003;82(4):247–55.
Fernandez F, Rodriguez-Sanjuan JC, Mayorga M, Llorca J, Garcia RA, Trugeda S, et al. Prognostic value of flow cytometry in surgically treated primary gastric lymphoma. Rev Esp Enferm Dig. 2006;98(11):817–27.
Doak SH. Aneuploidy in upper gastro-intestinal tract cancers—a potential prognostic marker? Mutat Res. 2008;651(1–2):93–104.
Sanchez-Perez I, Garcia Alonso P, Belda Iniesta C. Clinical impact of aneuploidy on gastric cancer patients. Clin Transl Oncol. 2009;11(8):493–8.
Ohyama S, Yonemura Y, Miyazaki I. Prognostic value of S-phase fraction and DNA ploidy studied with in vivo administration of bromodeoxyuridine on human gastric cancers. Cancer. 1990;65(1):116–21.
Sakusabe M, Kodama M, Sato Y, Kikuchi T, Koyama K. Clinical significance of DNA ploidy pattern in stage III gastric cancer. World J Surg. 1996;20(1):27–31.
Shen KL, Chu CH. DNA ploidy and biologic aggressiveness of gastric adenocarcinoma in Chinese. World J Surg. 1994;18(3):433–9. discussion 439–40.
Nesi G, Bruno L, Saieva C, Caldini A, Girardi LR, Zanna I, et al. DNA ploidy and S-phase fraction as prognostic factors in surgically resected gastric carcinoma: a 7-year prospective study. Anticancer Res. 2007;27(6C):4435–41.
Abad M, Ciudad J, Rincon MR, Silva I, Paz-Bouza JI, Lopez A, et al. DNA aneuploidy by flow cytometry is an independent prognostic factor in gastric cancer. Anal Cell Pathol. 1998;16(4):223–31.
Santoro E, Carboni M, Catarci M, Carlini M, Carboni F, Zupi G, et al. DNA ploidy, proliferative index and EGF-R status in 130 cases of resected gastric cancer—a multivariate analysis. Hepatogastroenterology. 1997;44(15):826–37.
Wyatt JI, Quirke P, Ward DC, Clayden AD, Dixon MF, Johnston D, et al. Comparison of histopathological and flow cytometric parameters in prediction of prognosis in gastric cancer. J Pathol. 1989;158(3):195–201.
Setala LP, Nordling S, Kosma VM, Lipponen PK, Eskelinen MJ, Hollmen SM, et al. Comparison of DNA ploidy and S-phase fraction with prognostic factors in gastric cancer. Anal Quant Cytol Histol. 1997;19(6):524–32.
Thoma CR, Toso A, Meraldi P, Krek W. Mechanisms of aneuploidy and its suppression by tumour suppressor proteins. Swiss Med Wkly. 2011;141:w13170.
Mimori K, Inoue H, Alder H, Ueo H, Tanaka Y, Mori M. Mutation analysis of hBUB1, human mitotic checkpoint gene in multiple carcinomas. Oncol Rep. 2001;8(1):39–42.
Ando K, Kakeji Y, Kitao H, Iimori M, Zhao Y, Yoshida R, et al. High expression of BUBR1 is one of the factors for inducing DNA aneuploidy and progression in gastric cancer. Cancer Sci. 2010;101(3):639–45.
Kim HS, Park KH, Kim SA, Wen J, Park SW, Park B, et al. Frequent mutations of human Mad2, but not Bub1, in gastric cancers cause defective mitotic spindle checkpoint. Mutat Res. 2005;578(1–2):187–201.
Grabsch HI, Askham JM, Morrison EE, Pomjanski N, Lickvers K, Parsons WJ, et al. Expression of BUB1 protein in gastric cancer correlates with the histological subtype, but not with DNA ploidy or microsatellite instability. J Pathol. 2004;202(2):208–14.
Grabsch H, Takeno S, Parsons WJ, Pomjanski N, Boecking A, Gabbert HE, et al. Overexpression of the mitotic checkpoint genes BUB1, BUBR1, and BUB3 in gastric cancer–association with tumour cell proliferation. J Pathol. 2003;200(1):16–22.
Davenport J, Harris LD, Goorha R. Spindle checkpoint function requires Mad2-dependent Cdc20 binding to the Mad3 homology domain of BubR1. Exp Cell Res. 2006;312(10):1831–42.
Wu CW, Chi CW, Huang TS. Elevated level of spindle checkprotein MAD2 correlates with cellular mitotic arrest, but not with aneuploidy and clinicopathological characteristics in gastric cancer. World J Gastroenterol. 2004;10(22):3240–4.
Sakakura C, Hagiwara A, Yasuoka R, Fujita Y, Nakanishi M, Masuda K, et al. Tumour-amplified kinase BTAK is amplified and overexpressed in gastric cancers with possible involvement in aneuploid formation. Br J Cancer. 2001;84(6):824–31.
Abdel-Wahab M, Attallah AM, Elshal MF, Abdel-Raouf M, Zalata KR, el-Ghawalby N, et al. Cellular proliferation and ploidy of the gastric mucosa: the role of Helicobacter pylori. Hepatogastroenterology. 1997;44(15):880–5.
Melato M, Sidari L, Rizzardi C, Kovac D, Stimac D, Baxa P, et al. Gastric epithelium proliferation in early Hp+ and Hp− gastritis: a flow cytometry study. Anticancer Res. 2001;21(2B):1347–53.
Nardone G, Staibano S, Rocco A, Mezza E, D’Armiento FP, Insabato L, et al. Effect of Helicobacter pylori infection and its eradication on cell proliferation, DNA status, and oncogene expression in patients with chronic gastritis. Gut. 1999;44(6):789–99.
Rocco A, Staibano S, Ottini L, Mezza E, Somma P, Mariani-Costantini R, et al. Is there a link between environmental factors and a genetic predisposition to cancer? A lesson from a familial cluster of gastric cancers. Eur J Cancer. 2003;39(11):1619–24.
Williams L, Somasekar A, Davies DJ, Cronin J, Doak SH, Alcolado R, et al. Aneuploidy involving chromosome 1 may be an early predictive marker of intestinal type gastric cancer. Mutat Res. 2009;669(1–2):104–11.
Targa AC, Cesar AC, Cury PM, Silva AE. Apoptosis in different gastric lesions and gastric cancer: relationship with Helicobacter pylori, overexpression of p53 and aneuploidy. Genet Mol Res. 2007;6(3):554–65.
Chan AO, Peng JZ, Lam SK, Lai KC, Yuen MF, Cheung HK, et al. Eradication of Helicobacter pylori infection reverses E-cadherin promoter hypermethylation. Gut. 2006;55(4):463–8.
Machado JC, Oliveira C, Carvalho R, Soares P, Berx G, Caldas C, et al. E-cadherin gene (CDH1) promoter methylation as the second hit in sporadic diffuse gastric carcinoma. Oncogene. 2001;20(12):1525–8.
Guilford P, Hopkins J, Harraway J, McLeod M, McLeod N, Harawira P, et al. E-cadherin germline mutations in familial gastric cancer. Nature. 1998;392(6674):402–5.
Humar B, Blair V, Charlton A, More H, Martin I, Guilford P. E-cadherin deficiency initiates gastric signet-ring cell carcinoma in mice and man. Cancer Res. 2009;69(5):2050–6.
Chan AO, Lam SK, Wong BC, Wong WM, Yuen MF, Yeung YH, et al. Promoter methylation of E-cadherin gene in gastric mucosa associated with Helicobacter pylori infection and in gastric cancer. Gut. 2003;52(4):502–6.
Dong CX, Deng DJ, Pan KF, Zhang L, Zhang Y, Zhou J, et al. Promoter methylation of p16 associated with Helicobacter pylori infection in precancerous gastric lesions: a population-based study. Int J Cancer. 2009;124(2):434–9.
Duensing A, Duensing S. Guilt by association? p53 and the development of aneuploidy in cancer. Biochem Biophys Res Commun. 2005;331(3):694–700.
Ikeguchi M, Saito H, Kondo A, Tsujitani S, Maeta M, Kaibara N. Mutated p53 protein expression and proliferative activity in advanced gastric cancer. Hepatogastroenterology. 1999;46(28):2648–53.
Karaman A, Kabalar ME, Binici DN, Ozturk C, Pirim I. Genetic alterations in gastric precancerous lesions. Genet Couns. 2011;21(4):439–50.
Saeki H, Kitao H, Yoshinaga K, Nakanoko T, Kubo N, Kakeji Y, et al. Copy-neutral loss of heterozygosity at the p53 locus in carcinogenesis of esophageal squamous cell carcinomas associated with p53 mutations. Clin Cancer Res. 2011;17(7):1731–40.
Jiao YF, Sugai T, Suzuki M, Uesugi N, Habano W, Nakamura S, et al. Application of the crypt isolation technique to the flow cytometric analysis of DNA content in gastric carcinoma. Hum Pathol. 2004;35(5):587–93.
Kitayama Y, Sugimura H, Tanaka M, Nakamura S, Kino I. Expression of p53 and flow cytometric DNA analysis of isolated neoplastic glands of the stomach: an application of the gland isolation method. Virchows Arch. 1995;426(6):557–62.
Lapenna S, Giordano A. Cell cycle kinases as therapeutic targets for cancer. Nat Rev Drug Discov. 2009;8(7):547–66.
Korenaga D, Okamura T, Saito A, Baba H, Sugimachi K. DNA ploidy is closely linked to tumor invasion, lymph node metastasis, and prognosis in clinical gastric cancer. Cancer. 1988;62(2):309–13.
Korenaga D, Okamura T, Sugimachi K, Inokuchi K. Prognostic study of intramucosal carcinoma of the stomach with DNA aneuploidy. Jpn J Surg. 1985;15(6):443–8.
Sasaki K, Takahashi M, Hashimoto T, Kawachnino K. Flow cytometric DNA measurement of gastric cancers. Clinico-pathological implication of DNA ploidy. Pathol Res Pract. 1989;184(6):561–6.
Yonemura Y, Ooyama S, Sugiyama K, Kamata T, De Aretxabala X, Kimura H, et al. Retrospective analysis of the prognostic significance of DNA ploidy patterns and S-phase fraction in gastric carcinoma. Cancer Res. 1990;50(3):509–14.
Baretton G, Carstensen O, Schardey M, Lohrs U. DNA-ploidy and survival in gastric carcinomas: a flow-cytometric study. Virchows Arch A Pathol Anat Histopathol. 1991;418(4):301–9.
Haraguchi M, Watanabe A, Moriguchi S, Korenaga D, Maehara Y, Okamura T, et al. DNA ploidy is a major prognostic factor in advanced gastric carcinoma—univariate and multivariate analysis. Surgery. 1991;110(5):814–9.
Noguchi Y, Tsuburaya A, Makino T, Fukuzawa K, Nomura K, Yoshikawa T, et al. Predictive value of c-erbB-2 and DNA ploidy patterns in gastric carcinoma recurrence. Int Surg. 1993;78(2):107–11.
D’Agnano I, D’Angelo C, Savarese A, Carlini M, Garofalo A, Bottari L, et al. DNA ploidy, proliferative index, and epidermal growth factor receptor: expression and prognosis in patients with gastric cancers. Lab Invest. 1995;72(4):432–8.
Flyger HL, Christensen IJ, Thorup J, Hakansson TU, Norgaard T. DNA aneuploidy in gastric carcinoma. Flow cytometric data related to survival, location, and histopathologic findings. Scand J Gastroenterol. 1995;30(3):258–64.
Mizunuma H, Tsuchiya A, Ando Y, Kikuchi Y, Abe R. Flow cytometric DNA analysis of gastric cancer that is invading the muscularis propria. Eur J Surg. 1996;162(11):889–94.
Fujimaki E, Sasaki K, Nakano O, Chiba S, Tazawa H, Yamashiki H, et al. DNA ploidy heterogeneity in early and advanced gastric cancers. Cytometry. 1996;26(2):131–6.
Wang Z, Ikeguchi M, Maeta M, Kaibara N. The correlation between the expression of p53 protein and DNA ploidy in patients with gastric cancer that has invaded the serosa. Anticancer Res. 1997;17(5A):3701–5.
Hirose K, Iida A, Yamaguchi A, Onchi H, Awata H, Katayama K, et al. Prognostic value of DNA ploidy and proliferating cell nuclear antigen in gastric cancer. Oncology. 1998;55(4):300–6.
Furuya T, Uchiyama T, Murakami T, Adachi A, Kawauchi S, Oga A, et al. Relationship between chromosomal instability and intratumoral regional DNA ploidy heterogeneity in primary gastric cancers. Clin Cancer Res. 2000;6(7):2815–20.
Lee JH, Noh SH, Lee KY, Choi SH, Min JS. DNA ploidy patterns in advanced gastric carcinoma; is it a clinically applicable prognosticator? Hepatogastroenterology. 2001;48(42):1793–6.
Conflict of interest
None of the authors has anything to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oki, E., Hisamatsu, Y., Ando, K. et al. Clinical aspect and molecular mechanism of DNA aneuploidy in gastric cancers. J Gastroenterol 47, 351–358 (2012). https://doi.org/10.1007/s00535-012-0565-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-012-0565-4