Abstract
Background
This prospective study was to assess the safety and feasibility of daily granulocyte and monocyte adsorptive apheresis (GMA) therapy in patients with active ulcerative colitis (UC).
Methods
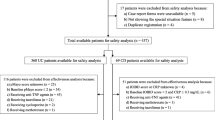
Thirty consecutive patients with moderately or severely active UC received daily GMA treatment (5 sessions over 5 consecutive days) with the Adacolumn. Adverse events (AE), patient tolerability, and clinical symptoms were monitored daily.
Results
Sixteen patients (53%) experienced AE during at least one GMA session. The most frequent AE was mild headache followed by fatigue and fever. None of the AE was serious, and all patients completed the 5 consecutive GMA sessions. Clinical symptoms (stool frequency and/or rectal bleeding) were improved in 21 patients (70%) during the course of GMA therapy. Clinical remission defined as normal stool frequency and no rectal bleeding was achieved in 7 patients (23%) after 5 GMA sessions. Seven of 20 patients (35%) with moderately active disease achieved clinical remission, whereas none of the 10 patients with severely active disease achieved clinical remission. Total and differential leukocyte counts, platelet count, and hemoglobin level did not significantly change, but C-reactive protein level significantly decreased during the course of GMA therapy.
Conclusions
This is the first report on daily GMA in the treatment of patients with UC. Daily GMA was safe and well tolerated without serious AE. Furthermore, daily GMA was associated with rapid improvement of clinical symptoms in patients with moderately active UC. However, controlled trials are warranted to assess a definite efficacy for daily GMA therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Active ulcerative colitis (UC) is frequently associated with infiltration of large numbers of leukocytes of the myeloid lineage (granulocytes and monocytes) into the bowel mucosa. Removal of the circulating activated leukocytes by apheresis has the potential to alleviate the inflammation in patients with UC and promote disease remission. In Japan, since April 2000, granulocyte and monocyte adsorptive apheresis (GMA) has been approved by the Japan Ministry of Health and Welfare as one treatment option for active UC [1, 2]. Several clinical trials have shown that GMA is safe and effective for patients with active UC [3–8]. A recent meta-analysis found that adverse events (AE) were much less frequent in patients treated with GMA as compared with those treated with steroids [9]. Similarly, homogeneous evidence from randomized controlled trials (RCTs) has shown that GMA induces clinical remission in a higher proportion of patients as compared to conventional medical therapy [9].
However, the optimal treatment regimen in terms of the number and frequency of GMA sessions during a given treatment time course remains to be established. Theoretically, intensive treatment may be more effective, in a shorter time, but the risk of serious AE may increase. Two RCTs [10, 11] comparing the safety and efficacy of weekly and twice-a-week regimens for active UC found that the rate of clinical remission was higher in the twice-a-week treatment group. Likewise, the mean time to remission was shorter in the twice-a-week treatment group as compared with the once-a-week regimen [10, 11]. Furthermore, the twice-a-week treatment was well tolerated without any serious AE [10, 11]. We were interested to see the safety and efficacy of a more intensive GMA treatment frequency like daily regimen. This was a prospective study in patients with moderately or severely active UC with a major focus on safety, tolerability, and patient compliance.
Patients and methods
Study design
This prospective, single-center study was undertaken at the Yokkaichi Social Insurance Hospital, a referral center treating a large number of patients with inflammatory bowel disease in the Mie Prefecture of Japan. The study was conducted in accordance with the principle of good clinical practice and the Declaration of Helsinki. Our study protocol was reviewed and approved by the ethics committee of our institution.
Patients
Patient inclusion criteria were: (1) age between 12 and 75 years; (2) endoscopic and histologic diagnosis of UC, not having indeterminate colitis; (3) endoscopic inflammation in the colon and the rectum at entry; (4) a disease activity index (DAI) [12] score of at least 6; and (5) receiving one or more of the following medications: sulphasalazine, mesalazine, corticosteroids, or immunosuppressants, which had started well in advance of entry to this study. Exclusion criteria were: (1) patients with evidence of toxic megacolon or fulminant colitis; (2) malignancy; (3) serious cerebral, pulmonary, cardiac, hepatic, or renal disease; (4) laboratory abnormalities like leukocyte count less than 2,000/mm3 or hemoglobin (Hb) less than 7.0 g/dL; (5) a known bleeding disorder or receiving anticoagulant therapy other than for the GMA procedure; and (6) a history of hypersensitivity reaction during an extracorporeal procedure. In the case of an underage patient, consent from one of the patient’s parents was sought. Thirty consecutive patients who met the inclusion criteria were treated in this study. Baseline demographic characteristics of the 30 patients are shown in Table 1.
GMA therapy
Twenty of the 30 patients were treated in our outpatient facility, the other 10 were treated as inpatients. GMA therapy was done with the Adacolumn (JIMRO, Takasaki, Japan), which is an adsorptive-type extracorporeal granulocyte and monocyte apheresis device with a volume of 335 mL, filled with about 220 g cellulose acetate beads of 2-mm diameter as the column adsorptive leukocytapheresis carriers [1, 2]. Blood was drawn into the column from the antecubital vein of one arm and returned to the patient via the antecubital vein of the contralateral arm. After completion of each GMA session, the residual blood in the column void volume and the circuit lines (approximately 200 mL) was returned to the patients by infusing physiological saline at the blood inflow line. Vital signs were continuously monitored during the GMA procedure. GMA was administered daily, every 24 ± 3 h. The total number of scheduled GMA sessions during this study was 5. The GMA session time was 90 min/session, at 30 mL/min. It was decided that when a patient develops a serious AE or a serious abnormality in hematology during the daily treatment, the GMA therapy should be stopped at that time. In patients who were receiving corticosteroids at entry, the steroid dose was to be tapered or discontinued in line with clinical improvement. Patients receiving sulphasalazine, mesalazine, or immunosuppressants at entry could continue at the same dosage.
Assessment of safety and efficacy
Adverse events experienced during and after every GMA session were recorded, and feasibility of the procedure was assessed. As clinical symptoms, stool frequency, consistency, presence or absence of abdominal pain, tenesmus, rectal bleeding, and mucus discharge were recorded daily. Stool frequency and rectal bleeding were scored according to the DAI system [12]. Stool frequency score 0, normal number of stools; score 1, 1–2 stools/day above normal; score 2, 3–4 stools/day above normal; score 3, 5 or more stools/day above normal. Rectal bleeding score 0, no blood; score 1, streaks of blood with stools less than half of the time; score 2, obvious blood with stools most of the time; score 3, blood alone passed. The stool frequency and rectal bleeding scores were recorded every 24 h after each GMA session. Clinical remission was defined as normal stool frequency (i.e., score 0) and no rectal bleeding (i.e., score 0) during 24 h after the fifth GMA session.
At entry (immediately before the first GMA session) and after the treatment (1–3 days after the fifth session), hematology data were obtained for all patients, including total and differential leukocyte counts, Hb, platelet count, C-reactive protein (CRP), total protein, albumin, creatinine, urea, sodium, potassium, chloride, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), lactic dehydrogenase (LDH), total bilirubin, and blood cholesterol. Furthermore, the total and differential leukocyte counts, platelet counts, and Hb level were measured immediately before each GMA session in all patients. The changes in hematology data during the treatment were monitored as part of AE evaluation.
Statistics
Comparison of frequencies was by using the chi-square test with Yates’ correction. Continuous data are presented as the mean ± SE values. The mean values between two groups were compared by using the unpaired t test. The change in values with time was evaluated by the paired t test. P < 0.05 was considered statistically significant. A StatView-J 5.0 was used for the statistical analyses of the data.
Results
Adverse events and patient compliance
All AE experienced during and after every GMA session are presented in Table 2. Sixteen patients (53%) experienced AE during at least one GMA session. Several patients experienced more than one AE during one session. The rate of AE did not significantly increase during subsequent GMA sessions. The most common AE was mild headache, observed during 15 of 150 sessions followed by feeling of fatigue (10 of 150 sessions) and fever, 37–38°C (9 of 150 sessions). None of these AE during this study was judged to be serious, and all patients completed the 5 GMA sessions according to the protocol.
Clinical efficacy outcomes
Figure 1 shows that the scores for both stool frequency and rectal bleeding significantly decreased during the course of GMA therapy. The stool frequency and/or rectal bleeding score decreased after 5 GMA sessions in 21 patients (70%). Clinical remission defined as normal stool frequency and no rectal bleeding was achieved in 7 patients (23%) after 5 GMA sessions. Seven of 20 patients (35%) with moderately active disease (6 ≤ DAI score < 9) achieved clinical remission, whereas none of the 10 patients with severely active disease (DAI score ≥9) achieved clinical remission (P = 0.09). Other potential factors that could impact clinical remission during the course of daily GMA therapy were investigated (Table 3). Age, gender, duration of UC, duration of current exacerbation, medications for the current exacerbation, and the extent of UC did not appear to affect the likelihood of clinical remission.
Hematology data
Table 4 shows a significant fall in serum CRP during the course of GMA therapy. Daily GMA potentially might impact patients’ blood counts. However, there was no significant change in hematology data including total and differential leukocyte counts, platelet count, or Hb.
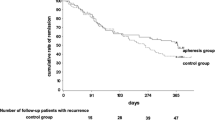
Follow-up data
Figure 2 shows a flow diagram of the patients’ follow-up treatment and outcomes. All patients were followed for at least 2 months after the last GMA session. The 7 patients who achieved clinical remission during the daily GMA treatment maintained remission. Among 23 patients without clinical remission, 1 patient was treated with twice-a-week GMA (5 sessions), 11 were given another course of 5 once-a-day GMA sessions, and 11 were treated with high-dose steroids, immunosuppressants, and/or infliximab. Five of the 11 patients who received further daily GMA sessions achieved clinical remission, the other 6 required conventional medication, or colectomy. Seven of the 11 patients treated with high-dose steroids, immunosuppressants, and/or infliximab achieved clinical remission. In 3 patients, UC symptoms continued and 1 patient underwent colectomy.
Discussion
Currently, intensive GMA regimen (twice-a-week) is applied to patients with active UC. However, this is the first time that daily GMA has been used in UC patients. Our major interest in this prospective study was to see if daily GMA was feasible, safe, and well tolerated by the patients. We found that 53% of the patients experienced AE during at least one GMA session. In our previous trial in which weekly or twice-a-week GMA was applied for moderate or severe UC, the overall AE rate was 24% [13]. Compared to weekly or twice-a-week GMA, the rate of AE in this trial was higher. However, in our daily treatment, the rate of AE did not significantly increase with the number of sessions. The higher AE rate may be related to our rigorous assessment process in this safety and feasibility study. The most frequent AE was transient mild headache, followed by feeling of fatigue and mild fever, which are commonly observed during extracorporeal therapy [14]. In several patients, headache could be prevented with common painkillers before starting the scheduled GMA session. None of the events was serious, and all patients completed the 5 GMA sessions according to the treatment schedule, i.e., patient compliance was 100%. Our experience indicated that daily GMA is safe and well tolerated. Furthermore, we did not experience any technical problem; feasibility was better than anticipated.
In Japan, a filtration-type leukocytapheresis (LCAP) device, which does not use cellulose acetate beads, has also been approved for treating active UC patients [15]. The filter removes up to 100% of granulocytes and monocytes, up to 60% of lymphocytes, and some platelets [15], but also significant red cells [16]. Recently, Tsujikawa et al. [17] investigated the safety and efficacy of daily LCAP therapy (5 sessions over 5 consecutive days) in 6 patients with moderately active UC. The Hb level in each patient gradually decreased as well as the platelet count and by the fifth session reached half of the value before the first session. The clinical activity index in only 2 patients reached remission level.
The GMA carriers of the Adacolumn we used in this study adsorb most of the granulocytes and monocytes, a significant fraction of platelets, and less than 2% of lymphocytes from the blood in the column; red blood cells are spared [1, 2, 18]. We were aware that despite these adsorption rates, leukocyte counts in the systemic circulation of the patients are not significantly affected during or immediately after a GMA session in weekly or twice-a-week protocols. However, we were concerned that granulocyte and monocyte counts may significantly decrease when patients receive daily GMA sessions. However, in this trial, we found that total and differential leukocyte counts did not significantly fall during or immediately after the treatment. Similarly, the residual blood remaining in the Adacolumn and circuit lines at the end of a GMA session potentially can affect the Hb level. Therefore, we had to ensure that in the daily GMA protocol, Hb level remains stable. For this, the residual blood was returned to the patients as described above and no significant fall in Hb level was observed in any patient during this study. Also, platelet count remained within the normal range.
In the present study, stool frequency and rectal bleeding were mainly assessed according to the DAI system [12]. The clinical outcomes might be summarized as follows. The stool frequency and rectal bleeding scores were recorded every 24 h after each GMA session. In 70% of the patients, stool frequency and/or rectal bleeding improved during the treatment. Clinical remission defined as normal stool frequency and no rectal bleeding during 24 h after the fifth GMA session was observed in 23% of the patients. The rate of clinical remission was 35% for moderate UC versus 0% for severe UC. In our previous trial in which weekly GMA was applied to treat moderate UC and twice-a-week regimen for severe UC, the overall clinical remission rate was 45% after 5–10 GMA sessions [13]. Following the present experience, we believe that daily GMA might produce similar effects, but in a shorter time.
In this study, no patient with severe UC achieved clinical remission. The remission rate was lower than those in previous studies with weekly or twice-a-week GMA [3–6]. This difference may be related to the duration of interventions and the timing of efficacy assessment. In this trial, the efficacy was assessed immediately after a 5-day treatment course. In contrast, in weekly or twice-a-week GMA regimen, adjunct medications may affect the efficacy of GMA during several weeks of the treatment.
In this trial, endoscopic examination was not done after the treatment because we were aware that it can take significant time before endoscopic improvement is observed [13]. We believe that further GMA sessions after the daily schedule (a total of 5 additional daily sessions) might induce endoscopic remission (mucosal healing) along with an increased clinical remission rate. We are planning to investigate the relationship between the endoscopic findings and the therapeutic effect of daily GMA in a future study with a longer follow-up time.
In this study, 11 patients were treated with another course of daily GMA (5 sessions), which was started 3 days after the initial daily treatment. The second course of daily GMA therapy was also well tolerated without serious AE in all the 11 patients. Throughout the study, patients were willing to receive daily GMA, up to 10 sessions or even more. Accordingly, we are planning to investigate whether another 5 daily GMA sessions (total 10 sessions) is safe and produces better efficacy rate in a large cohort of patients.
In conclusion, this is the first report on daily GMA in the treatment of patients with active UC. Daily GMA was safe and well tolerated without any serious AE. Daily GMA was associated with rapid improvement of clinical symptoms in patients with moderately active UC. However, controlled trials are warranted to assess a definite efficacy for daily GMA therapy. With a longer follow-up period, the full efficacy of daily GMA therapy may show up because mucosal healing is time-dependent even when a treatment is very effective. Therefore, in the future, it would be better to assess the efficacy of daily GMA after a longer follow-up time.
References
Shimoyama T, Sawada K, Hiwatashi N, Sawada T, Matsueda K, Munakata A, et al. Safety and efficacy of granulocyte and monocyte adsorption apheresis in patients with active ulcerative colitis: a multicenter study. J Clin Apher. 2001;16:1–9.
Saniabadi AR, Hanai H, Takeuchi K, Umemura K, Nakashima M, Adachi T, et al. Adacolumn, an adsorptive carrier based granulocyte and monocyte apheresis device for the treatment of inflammatory and refractory diseases associated with leukocytes. Therap Apher Dial. 2003;7:48–59.
Hanai H, Watanabe F, Takeuchi K, Iida T, Yamada M, Iwaoka Y, et al. Leukocyte adsorptive apheresis for the treatment of active ulcerative colitis: a prospective, uncontrolled, pilot study. Clin Gastroenterol Hepatol. 2003;1:28–35.
Suzuki Y, Yoshimura N, Saniabadi AR, Saito Y. Selective granulocyte and monocyte adsorptive apheresis as a first-line treatment for steroid naïve patients with active ulcerative colitis: a prospective uncontrolled study. Dig Dis Sci. 2004;49:565–71.
Naganuma M, Funakoshi S, Sakuraba A, Takagi H, Inoue N, Ogata H, et al. Granulocytapheresis is useful as an alternative therapy in patients with steroid-refractory or -dependent ulcerative colitis. Inflamm Bowel Dis. 2004;10:251–7.
Hanai H, Watanabe F, Yamada M, Sato Y, Takeuchi K, Iida T, et al. Adsorptive granulocyte and monocyte apheresis versus prednisolone in patients with corticosteroid-dependent moderately severe ulcerative colitis. Digestion. 2004;70:36–44.
Yamamoto T, Umegae S, Kitagawa T, Yasuda Y, Yamada Y, Takahashi D, et al. Granulocyte and monocyte adsorptive apheresis in the treatment of active distal ulcerative colitis: a prospective, pilot study. Aliment Pharmacol Ther. 2004;20:783–92.
Yamamoto T, Saniabadi AR, Maruyama Y, Umegae S, Matsumoto K. Factors affecting clinical and endoscopic efficacies of selective leucocytapheresis for ulcerative colitis. Dig Liver Dis. 2007;39:626–33.
Habermalz B, Sauerland S. Clinical effectiveness of selective granulocyte, monocyte adsorptive apheresis with the Adacolumn device in ulcerative colitis. Dig Dis Sci. 2010;55:1421–8.
Sakuraba A, Motoya S, Watanabe K, Nishishita M, Kanke K, Matsui T, et al. An open-label prospective randomized multicenter study shows very rapid remission of ulcerative colitis by intensive granulocyte and monocyte adsorptive apheresis as compared with routine weekly treatment. Am J Gastroenterol. 2009;104:2990–5.
Sakuraba A, Sato T, Naganuma M, Morohoshi Y, Matsuoka K, Inoue N, et al. A pilot open-labeled prospective randomized study between weekly and intensive treatment of granulocyte and monocyte adsorption apheresis for active ulcerative colitis. J Gastroenterol. 2008;43:51–6.
Sutherland LR, Martin F, Greer S, Robinson M, Greenberger N, Saibil F, et al. 5-Aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology. 1987;92:1984–8.
Yamamoto T, Umegae S, Matsumoto K. Mucosal healing in patients with ulcerative colitis during a course of selective leukocytapheresis therapy: a prospective cohort study. Inflamm Bowel Dis. 2010;16:1905–11.
Norda R, Berséus O, Stegmayr B. Adverse events and problems in therapeutic hemapheresis. A report from the Swedish registry. Transfus Apher Sci. 2001;25:33–41.
Kanai T, Hibi T, Watanabe M. The logics of leukocytapheresis as a natural biological therapy for inflammatory bowel disease. Expert Opin Biol Ther. 2006;6:453–66.
Sakata Y, Iwakiri R, Amemori S, Yamaguchi K, Fujise T, Otani H, et al. Comparison of the efficacy of granulocyte and monocyte/macrophage adsorptive apheresis and leucocytapheresis in active ulcerative colitis patients: a prospective randomized study. Eur J Gastroenterol Hepatol. 2008;20:629–33.
Tsujikawa T, Andoh A, Ogaẃa A, Sonoda A, Yagi Y, Hata K, et al. Feasibility of five days of consecutive leukocytapheresis for the treatment of ulcerative colitis: a preliminary study. Ther Apher Dial. 2009;13:14–8.
Saniabadi AR, Hanai H, Fukunaga K, Sawada K, Shima C, Bjarnason I, et al. Therapeutic leukocytapheresis for inflammatory bowel disease. Transfus Apher Sci. 2007;37:191–200.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamamoto, T., Umegae, S. & Matsumoto, K. Daily granulocyte and monocyte adsorptive apheresis in patients with active ulcerative colitis: a prospective safety and feasibility study. J Gastroenterol 46, 1003–1009 (2011). https://doi.org/10.1007/s00535-011-0428-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0428-4