Abstract
Ulcerative colitis and Crohn’s disease are the two main forms of inflammatory bowel disease (IBD). The study of immunological pathways involved in the onset of IBD is of fundamental importance to identify potential biological markers of disease activity and specific targets for therapy. Removing excess and activated circulating leukocytes with adsorptive cytapheresis has been shown to be a potentially effective treatment for patients with an inflamed bowel. Adsorptive cytapheresis is a non-pharmacological approach for active IBD, in which known sources of inflammatory cytokines such as activated myeloid lineage leucocytes are selectively depleted from the circulatory system. The decrease in inflammatory load caused by removing these cells is thought to enhance drug therapy and thereby promote disease remission. The benefit of cytapheresis appears to rest upon its ability to reduce levels of certain immune cell populations; however, whether this depletion results in further changes in lymphocyte populations and cytokine production needs further clarification. In this review, we aim to summarize existing evidence on the role of cytapheresis in patients with IBD, its effect on cytokine levels and cellular populations, and to discuss its potential impact on disease activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ulcerative colitis (UC) and Crohn’s disease (CD) are the two main forms of inflammatory bowel disease (IBD). Both conditions are characterized by chronic inflammation of the gastrointestinal tract, which affects millions of individuals throughout the world, severely impairing quality of life and reducing the life expectancy of those with the disease [1]. Despite the relatively high incidence of IBD, the underlying causes of UC and CD remain unknown [2, 3]. However, recent hypotheses suggest an altered response in the host’s immune system toward self-antigens and commensal bacteria in association with environmental triggers that are yet to be identified [4, 5].
The study of the immunological pathways involved in the onset of IBD is of fundamental importance to identify potential biological markers of disease activity and specific targets for therapy. Traditionally, most research efforts have focused on acquired immunity, mainly due to the detection of an unusually high activation of CD4+ Th1 lymphocytes and the resulting increase in TNF-α expression that can be found in these patients [6]. In fact, blocking this pathway with anti-TNF-α treatments has become pivotal in the management of the disease [7]. The discovery of a novel class of CD4+ T-helper cells (Th17) with pro-inflammatory activity has also been the subject of research; however, a clear therapeutic target has not yet been identified [8]. Recently, the spotlight has shifted toward a potential deregulation of innate immunity and a loss of immunological tolerance to gut microbiota, which in turn results in abnormal activation and migration of granulocytes and monocytes/macrophages to the intestinal mucosa, with the ensuing overexpression of inflammatory cytokines [7]. In fact, one of the most recent therapies approved for IBD is a so-called anti-migration drug which hinders leukocyte migration to the gut mucosa by through selective inhibition of the α4β7 integrins [9].
Researchers worldwide are now interested in the expression patterns of cytokines and their role as potential triggers of mucosal inflammation in patients with IBD. Cytapheresis is a novel non-pharmacological approach for the treatment of active IBD, in which known sources of inflammatory cytokines such as activated myeloid lineage leucocytes are selectively depleted from the circulatory system, eliminating their inflammatory effect. In this review, we clarify the role of cytapheresis in patients with IBD, its effect on cytokine levels and cellular populations, and its potential impact on disease activity.
Role of Apheresis in IBD
Most IBD research to date has endeavored to determine the role of cytokines in mucosal inflammation and important progress has been made in this area. However, the recent identification of altered granulocyte subpopulations in patients with UC has led to an increased interest in the immunological effects derived from selectively adjusting these populations with cytapheresis and its potential impact on disease activity.
Changes in innate immunity and cytokine profiles are known to play a key pathophysiological role in IBD and are, therefore, the subject of extensive research [10, 11]. Recent studies have reported elevations—both in tissue and in peripheral blood—of certain monocyte subpopulations, particularly the CD4+ CD16+ phenotype, which constitutes a major source of inflammatory cytokines such as TNF-α, interleukin (IL)-1β, IL-6, IL-12, and IL-23 [9]. In line with these findings is the fact that patients with active IBD respond to anti-cytokine antibodies (notably, anti-TNF-α antibodies), which currently represent the main therapeutic breakthrough for the management of this disease [12]. Despite these advances, the development of biological agents has not necessarily led to a deeper understanding of their mode of action; furthermore, increasing concern about their long-term safety and efficacy makes research into other potential treatments of critical importance [13]. Biological therapies only appear to be effective in certain subgroups of patients. Even when anti-TNF therapies are effective, many patients suffer of loss of response which is not always explained by a mechanism of immunogenicity. This suggests that cytokine networks might be far more complex than initially suspected and, thus, that the blockade of a single cytokine can be compensated for by the development of alternative pro-inflammatory pathways [7, 9]. Furthermore, the mechanisms that drive mucosal inflammation are believed to differ among individuals, which explains why anti-cytokine therapy is not equally effective in all patients and why focusing on single cytokines might prove less effective than anticipated. Research on new therapies for IBD and new mechanisms of action are needed.
Types of Apheresis Systems
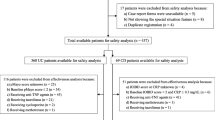
Selective depletion of soluble elements from the blood has been available since the early 20th century, but their efficacy as alternative or adjunct therapy in UC could not be adequately assessed until the recent development of safe and efficient extracorporeal cellular adsorption techniques [14]. Cytapheresis removes circulating activated myeloid lineage leukocytes and thereby provides a means to “reset” the immune system and enhance drug therapy. Two methods of adsorptive cytapheresis have been developed: granulocyte/monocyte apheresis (GMA) using Adacolumn (Japan Immunoresearch Laboratories, Takasaki, Japan) and leukocytapheresis (LCAP) using the Cellsorba E column (Asahi Medical, Tokyo, Japan; Fig. 1a, b) [14,15,16,17].
Adacolumn is the most commonly used system of adsorptive cytapheresis. It works by selectively removing granulocyte/monocyte populations from peripheral blood using extracorporeal circulation. This selective depletion has been found to alleviate intestinal inflammation and promote disease remission, thereby reducing the need for long-term treatment with potentially harmful medications such as corticosteroids and other immunosuppressive agents [18, 19]. The Adacolumn mechanism consists of a 335-mm column filled with specially designed cellulose acetate beads that act as the adsorptive carriers. These carriers adsorb immunoglobulin G and immune complexes from blood plasma, making their binding sites available for the fragment crystallizable gamma receptors (FcγR) on myelocytes and small subsets of B, T and natural killer cells. It must be noted that FcγRs are not as widely expressed on lymphocytes (2%) as they are on granulocytes (65%) and monocytes (55%); it is this particularity that lends Adacolumn its selectivity toward myeloid lineage cells. Whether this selective cellular depletion can induce secondary changes in lymphocyte populations and cytokine production and the extent to which these changes can influence the course of the disease has yet to be determined (Table 1) [14, 20]. The duration of each session is about 60 min and it is usually performed once per week for five consecutive weeks, though different protocols with 2+ sessions per week have also been tested.
Nonetheless, the clinical efficacy of GMA therapy cannot be fully explained by the effects of the procedure on peripheral cytokine levels per se; thus, efforts are being made to identify the specific cellular and biochemical mechanisms that underlie its effect on mucosal inflammation [21,22,23,24].
The LCAP is another method of therapeutic apheresis using the Cellsorba E column, consisting of polyester nonwoven fabric in a sterilized polycarbonate container that can remove leukocytes, including lymphocytes [25]. Leukocytes are removed by adhesion to the column fiber element after which the treated blood is returned to the patient. The adsorptive column removes 90–100% of granulocytes and monocytes, 30–60% of lymphocytes and a lower percentage of platelets from peripheral blood [26]. The anticoagulated blood is passed through a pre-filter made of 10–40 μm of fabric and then through the main filter made of finer fiber. LCAP with Cellsorba is performed once weekly for five consecutive weeks. The duration of each session is about 60 min, with 2–3 L of blood processed at a flow rate of 30–50 mL/min. Like with Adacolumn, the selective removal of leukocytes from peripheral blood with Cellsorba is probably not the only mechanism responsible for its clinical efficacy (Table 2). Other immunological mechanisms play an important role in the efficacy of apheresis in patients with active IBD. All these mechanisms seem to contribute to the clinical efficacy of Adacolumn and Cellsorba in the treatment of IBD. However, the transient lymphopenia observed during Cellsorba leukocytapheresis treatment could potentially represent a limit, as suggested by the evidence indicating that lymphopenia could promote autoimmunity development [27].
Efficacy of GMA in IBD
Despite the initial controversy regarding the use of apheresis in patients with IBD, a considerable number of studies have been conducted reporting clinical efficacy in patients with UC, with a smaller number investigating the changes in cellular populations and cytokine levels, which might be responsible for such outcomes [15,16,17, 20, 28]. Current data support its use, especially in steroid-dependent patients, and other suggested possible clinical predictors are summarized in Table 3. Several studies [17, 28, 29], including a large-scale postmarketing study with 656 patients [18], have reported that GMA is safe and effective for the treatment of active UC. This has also been reported in a subsequent meta-analysis; [19] however, some trials such as a pivotal sham-controlled trial conducted by Sands et al. [30] was offered negative results. One of the reasons for these contradicting results may be the fact that these studies include different patient populations. This fact is illustrated by a very recent publication of a post hoc analysis which, unlike the original study, revealed a significant therapeutic effect of adsorptive cytapheresis for active UC [31]. The authors conclude that this was likely due to strict selection of patients during post hoc analysis. Subsequent studies have shown efficacy of apheresis [20].
In another recent study, granulocyte/monocyte apheresis (GMA) provided significant clinical benefit to a large cohort of steroid-dependent UC patients with previous failure to immunosuppressant and/or biologic treatment, with a favorable safety profile [32]. These results are consistent with previous studies and support GMA use in this difficult-to-treat patient group.
Reports from clinical practice settings classically indicate that first-episode and steroid-naïve cases respond well to GMA and usually attain a favorable future clinical course; however, GMA seems to be most effective if applied immediately after a flare-up rather than after a lag time. Studies also seem to show that patients with extensive deep ulcers, long duration of UC, and those refractory to multiple drugs are unlikely to benefit from GMA; however, other scenarios need to be characterized. In therapeutic settings, identifying baseline features which predict response to GMA should help to stop futile use of this technique.
The majority of the studies with cytoaphereiss have been performed for UC patients and studies in patients with CD are scarce. GMA has shown efficacy in patients with refractory CD to conventional medication. In an open-label, prospective, randomized multicenter study, 104 patients with mild-to-moderately active CD received intensive GMA (two sessions per week) or standard GMA (one session per week) [33]. In both arms, GMA showed efficacy, was well-tolerated, and did not raise any safety concerns (Table 4).
Efficacy of LCAP in IBD
LCAP has been shown to be effective not only in the improvement of clinical symptoms but also in the induction of mucosal healing. However, the number of subjects in each of these studies is relatively small and no-large scale studies have been conducted to evaluate the efficacy and safety of LCAP. An open-label, multicenter, randomized control study [34] and a double-blind, prospective, case-controlled study with sham apheresis report that LCAP is effective and safe for treating UC [35]. Recently, a large-scale, prospective, observational study of 847 UC patients was conducted to evaluate the treatment outcomes of LCAP, including intensive LCAP, as it is currently used in clinical practice [36]. This study also reports safety and efficacy of LCAP in patients with active UC. The overall clinical remission rate and mucosal healing rate at 2 weeks after the last LCAP session were 68.9 and 62.5%, respectively.
Effects of GMA Therapy on Cytokines
Cytokines are small peptide proteins produced mainly by hematopoietic lineage cells that mediate a broad array of cellular interactions in adjacent or distant tissues. One of the primary consequences of the changes in immune cell populations observed in patients with IBD is a distorted cytokine expression pattern, with a clear upregulation of certain proinflammatory cytokines that promotes activation of leukocytes and, ultimately, perpetuates the inflammatory cycle [9, 10]. The identification and categorization of these biological mediators has been valuable not only in better defining the pathogenesis of IBD, but also for tailoring treatments by targeting specific cytokines [11]. Earlier studies have centered their attention on the impact of GMA therapy on individual cytokine levels while also evaluating any potential correlation with clinical, endoscopic and histological findings in patients with IBD [21, 22]; however, despite the high expectations, the effect on serial cytokine levels has been variable.
Few studies to date have found any clear association between GMA and a reduced concentration of proinflammatory cytokines in patients with active UC [23,24,25]. Studies such as those by Yamamoto et al. [22] and Muratov et al. [37] report a decrease in mucosal infiltration of myeloid leukocytes alongside considerable drops in the mucosal levels of inflammatory cytokines observed after GMA therapy. In particular, Muratov et al. [37] describes a downregulation of INF-γ found in peripheral blood samples of clinical responders to GMA. On the other hand, a study by Yamamoto et al. focused on the levels of mucosal cytokines before and after GMA therapy in patients with active UC. The mucosal tissue concentrations of IL-1β, IL-1 receptor antagonist (IL-1ra), IL-6, IL-8 and TNF-α observed in these patients were significantly higher than those found in the healthy control group, whereas the IL-1ra/IL-1β ratio was significantly lower. In line with these findings, patients who achieved clinical remission after GMA also exhibited lower mucosal concentrations of IL-1β, IL-1ra, IL-6, IL-8 and TNF-α, along with an increased IL-1ra/IL-1β ratio. In patients with no clinical or endoscopic remission, concentrations of these cytokines remained unchanged after GMA [22].
These results have been confirmed by other studies. Hanai et al. also report increased blood levels of IL-6, IL-10, IL-18 and IL-1ra in active UC with a subsequent decline after an 8-week GMA course. Interestingly, a correlation with the UC clinical activity index was only observed in the cases of IL-6, IL-10 and IL-18, but not with IL-1ra [38].
A subsequent study by Aoki et al. aimed to quantify and compare plasma levels of the proinflammatory cytokines TNF-α, IL-1β, IL-6 and IL-8 in patients with active UC in both pre- and post-GMA settings. Results show that only the IL-8 level was high enough to be assayed, with a significant drop in its concentration after GMA therapy. In addition to this finding, the authors observed a downregulation of the expression of Toll-like receptor 2 on granulocytes after incubation of blood samples belonging to healthy subjects compared with the Adacolumn patients [24].
Similarly, recent work by Toya et al. analyzes the effect of GMA on serum levels of 17 cytokines found in patients with active UC. Serum IL-10 and MIP-1β levels were significantly increased after GMA therapy, whereas concentrations of all other cytokines remained unchanged [23].
Effects of GMA Therapy on Cellular Populations
We have thus far reviewed the changes in cytokines observed after GMA therapy; however, these changes hardly provide a satisfying explanation for its clinical efficacy. For this and other reasons, research is beginning to focus on cellular subpopulations.
As mentioned above, the primary consequence of GMA therapy is a selective depletion of certain subsets of myeloid leukocytes, the most relevant of which is the CD14+ CD16+ DR++ phenotype, also known as the proinflammatory monocytes. This specific phenotype accounts for approximately 10% of total monocytes in healthy individuals, a proportion that can significantly increase in inflammatory conditions such as the ones found in patients with IBD [39]. This particular population is thought to play a key role in the pathogenesis of various inflammatory diseases due to their ability to release inflammatory cytokines, such as TNF-α, IL-1β, IL-6, IL-12 and IL-23 [7].
Surprisingly, in addition to depletion of CD14+ CD16+ DR++ monocytes, the procedure has also been associated with a sustained increase in absolute lymphocyte counts, notably the CD4+ CD25+ phenotype, known as regulatory T-cells (Treg), as well as an increase in the liberation of inflammatory mediators such as soluble cytokine receptors (sTNFR) I and II, IL-10, IL-1ra and hepatocyte growth factor [39, 40]. Treg cells express high levels of IL-2 receptor (CD25) and transcription factor forkhead box P3, and are involved in regulating the immune response by means of suppressing excess activation of immune cells, a feature that supports the use of GMA in diseases whose causes are related to a chronic over-activation of immunity [41].
Some recent data from flow cytometry analyses of peripheral blood after the GMA procedure with Adacolumn have also revealed a significant decrease in mature CD10+ neutrophils, followed by a stimulation of naïve CD10-neutrophils, the latter of which are believed to have a reduced proinflammatory effect [42, 43]. The extent to which this might contribute to reducing inflammation has yet to be assessed.
Given the novelty of this approach, the before-mentioned studies represent virtually all the available literature on the effects of GMA on cellular populations; however, as the use of Adacolumn and other GMA techniques becomes more widespread, we expect further abnormalities in these and other cellular subtypes to be revealed. Furthermore, systematic categorization of the cytokines produced by these specific cells will likely expose the mechanisms that underlie mucosal inflammation at a molecular level, allowing for more precise identification of the cytokines that should be subjected to further research.
Effects of LCAP Therapy on Cytokines
Adsorptive cytapheresis with Cellsorba is able to remove about 90–100% of granulocytes and monocytes, 30–60% of lymphocytes, and approximately 30% of platelets from peripheral blood in the first 30 min of session [25, 26]. Cellsorba is known to remove not only leukocytes but also activated platelets, monocyte-platelet aggregate (MPA), and leukocyte-platelet aggregates (LPA), all of which are known sources of proinflammatory cytokines [44]. In IBD patients who respond to cytapheresis with Cellsorba, baseline values of the proinflammatory cytokines TNF-α, IL-2, IL-8, and IFN-γ have been shown to be in the upper limit of normality [45]. These and other values such as those of C-reactive protein and erythrocyte tend to normalize after cytapheresis. Filter-passed lymphocytes have also shown a greater production of IL-4 with respect to pre-apheresis values [45].
Effects of LCAP Therapy on Cellular Populations
Flow cytometry also revealed the ability of Cellsorba to remove activated cells and adhesion molecule-positive cells [46]. Moreover, the average number of lymphocytes, both T and B cells, significantly decreases after Cellsorba. The CD4/CD8 ratio does not change after Cellsorba, while TH1/TH2 ratio seems to significantly decrease [47]. This technique also seems to be able to selectively remove CD14+ CD16+ DR++ monocytes from peripheral blood, both of which represent an important source of TNF-α and IL-12. All these mechanisms seem to contribute to the clinical efficacy of Cellsorba cytapheresis in the treatment of IBD [48].
In a recent study designed to examine the molecular dynamics which underlie the proliferation of intestinal epithelial cells after LCAP with Cellsorba, the authors pointed to an increase in the expression of caudal type homeobox 2 (CDX2) and hairy-related protein 1 (HES1) as a possible mechanism. In this study, patients with endoscopic improvement after LCAP exhibited an increase of CDX2 prior to LCAP, while those without endoscopic improvement did not [49, 50]. In both groups, expression of CDX2 was markedly increased after LCAP. The authors conclude that LCAP-induced CDX2 expression might be associated with mucosal healing in patients with active UC.
Concluding Remarks
The efficacy of anti-TNF-α biologics has provided evidence on the importance of inflammatory cytokines in the exacerbation and perpetuation of IBD. Cytokines control multiple aspects of the inflammatory response and play a fundamental role in the pathogenesis of IBD and other autoimmune diseases. In particular, the imbalance between proinflammatory and anti-inflammatory cytokines that occurs in IBD impedes the resolution of inflammation leading to disease perpetuation and tissue destruction. One of the major sources of inflammatory cytokines is myeloid lineage leucocytes, which also tend to be overly activated in individuals with IBD. This has led to the search for non-pharmacological strategies to reduce these leukocyte populations [51]. Activation of granulocytes and monocytes/macrophages such as the CD14+ CD16+ DR++ phenotype, represents a major source of proinflammatory cytokines in patients with UC; thus, these cellular populations appear to be logical targets of cytapheresis therapy. The benefit of cytapheresis seems to rest upon its ability to reduce the levels of specific immune cell populations; however, whether this depletion results in further changes in lymphocyte populations and cytokine production remains unclear. There is a pressing need to elucidate the mechanisms which underlie response to cytapheresis in order to accurately select the patients in which its use can offer the most benefit. This could be particularly important in patients who remain active in spite of being treated with double immunosuppressive therapy. In conclusion, current evidence seems to favor the use of adsorptive cytapheresis in selected IBD patients. Patients with extensive deep ulcers and with long duration of UC refractory to multiple drugs are unlikely to benefit from this treatment strategy. In therapeutic settings, identifying baseline features which predict response to cytapheresis should help to stop futile use of this technique.
Abbreviations
- GMA:
-
Granulocyte/monocyte apheresis
- UC:
-
Ulcerative colitis
- CD:
-
Crohn’s disease
- IBD:
-
Inflammatory bowel disease
- LCAP:
-
Leukocytapheresis
References
Jess T, Riis L, Vind I, et al. Changes in clinical characteristics, course, and prognosis of inflammatory bowel disease during the last 5 decades: a population-based study from Copenhagen, Denmark. Inflamm Bowel Dis. 2007;13:481–489.
Hendrickson BA, Gokhate R, Cho JH. Clinical aspects and pathophysiology of inflammatory bowel disease. Clin Microbiol Rev. 2002;15:79–94.
Neuman MG. Immune dysfunction in inflammatory bowel disease. Inflamm Bowel Dis. 2004;10:462–478.
Monteleone G, Fina D, Caruso R, Pallone F. New mediators of immunity and inflammation in inflammatory bowel disease. Curr Opin Gastroenterol. 2006;22:361–364.
Wallace KL, Zheng LB, Kanazawa Y, Shih DQ. Inmunopathology of inflammatory bowel disease. World J Gastroenterol. 2014;20:6–21.
Geremia A, Biancheri P, Allan P, Corazza GR, Di Sabatino A. Innate and adaptive immunity in inflammatory bowel disease. Autoimmun Rev. 2014;13:3–10.
Neurath MF. Cytokines in inflammatory bowel disease. Nat Rev Inmunol. 2014;14:329–342.
Waite JC, Skokos D. Th17 response and inflammatory autoimmune diseases. Int J Inflam. 2012;2012:819467.
Wang MC, Zhang LY, Han W, et al. PRISMA—efficacy and safety of vedolizumab for inflammatory bowel diseases: a systematic review and meta-analysis of randomized controlled trials. Medicine. 2014;93:e326.
Frankenberger M, Sternsdorf T, Pechumer H, et al. Differential cytokine expression in human blood monocyte subpopulations: a polymerase chain reaction analysis. Blood. 1996;87:373–377.
Sánchez F, Domínguez A, Yamamoto JK. Role of cytokines in inflammatory bowel disease. World J Gastroenterol. 2008;14:4280–4288.
Rutgeerts P, Sandborn WJ, Feagan BG. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462–2476.
Aaltonen KJ, Virkki LM, Malvimaara A, et al. Systematic review and meta-analysis of the efficacy and safety of existing TNF blocking agents in treatment of rheumatoid arthritis. PLoS ONE. 2012;7:e30275.
Hanai H, Takeda Y, Eberhardson M, et al. The mode of actions of the Adacolumn therapeutic leucocytapheresis in patients with inflammatory bowel disease: a concise review. Clin Exp Immunol. 2011;163:50–58.
Saniabiadi AR, Hanai H, Takeuchi K, et al. Adacolumn, an adsorptive carrier based granulocyte and monocyte apheresis device for the treatment of inflammatory and refractory diseases associated with leukocytes. Ther Apher Dial. 2003;7:48–59.
Saniabadi AR, Hanai H, Suzuki Y, et al. Adacolumn for selective leococytapheresis as a non-pharmacological treatment for patients with disorders of the immune system: an adjunct or an alternative to drug therapy? J Clin Apher. 2005;20:171–184.
Yamamoto T, Umegae S, Maysumoto K. Safety and clinical efficacy of granulocyte and monocyte adsorptive apheresis therapy for ulcerative colitis. World J Gastroenterol. 2006;12:7568–7577.
Hibi T, Sameshima Y, Sekiguchi Y, et al. Treating ulcerative colitis by Adacolumn therapeutic leucocytapheresis: clinical efficacy and safety based on surveillance of 656 patients in 53 centres in Japan. Dig Liver Dis. 2009;41:570–577.
Habermalz B, Sauerland S. Clinical effectiveness of selective granulocyte, monocyte adsorptive apheresis with Adacolumn device in ulcerative colitis. Dig Dis Sci. 2010;55:1421–1428.
Saniabadi AR, Tanaka T, Ohmori T, Swada K, Yamamoto T, Hanai H. Treating inflammatory bowel disease by adsorptive leucocytapheresis: a desire to treat without drugs. World J Gastroenterol. 2014;20:9699–9715.
Sacco R, Tanaka T, Yamamoto T, Bresci G, Saniabadi AR. Adacolumn leucocytapheresis for ulcerative colitis: clinical and endoscopic features of responders and unresponders. Expert Rev Gastroenterol Hepatol. 2014;27:1–7.
Yamamoto T, Saniabadi AR, Umegae S, Matsumoto K. Impact of selective leukocytapheresis on mucosal inflammation and ulcerative colitis: cytokine profiles and endoscopic Findings. Inflamm Bowel Dis. 2006;12:719–726.
Toya Y, Chiba T, Mizutani T, et al. The effect of granulocyte and monocyte adsorptive apheresis on serum cytokine levels in patients with ulcerative colitis. Cytokine. 2013;62:146–150.
Aoki H, Nakamura K, Yoshimatsu Y, et al. Adacolumn selective leukocyte adsorption apheresis in patients with ulcerative colitis: clinical efficacy, effects on plasma IL-8 and expression of toll-like receptor 2 on granulocytes. Dig Dis Sci. 2007;52:1427–1433.
Swada K, Ohnishi K, Fukui S, et al. Leukocytapheresis therapy, performed with leukocyte removal filter for inflammatory bowel disease. J Gastroenterol. 1995;30:322–329.
Sawada K, Ohnishi K, Kosaka Chikano S, et al. Leukocytapheresis with leukocyte removal filter as a new therapy for ulcerative colitis. Ther Apher. 1997;1:207–211.
King C, Ilic A, Koelsch K, Sarvetnick N. Homeostatic expansion of T cells during immune insufficiency generates autoimmunity. Cell. 2004;117:265–277.
Thanaraj S, Hamlin PJ, Ford AC. Systematic review: granulocyte/monocyte adsorptive apheresis for ulcerative colitis. Aliment Pharmacol Ther. 2010;32:1297–1306.
Cabriada JL, Domènech E, Ibargoyen N, et al. Leukocytapheresis for steroid-dependent ulcerative colitis in clinical practice: results of a nationwide Spanish registry. J Gastroenterol. 2012;47:359–365.
Sands BE, Sandborn WJ, Feagan B, et al. A randomized, double-blind, sham-controlled study of granulocyte/monocyte apheresis for active ulcerative colitis. Gastroenterology. 2008;135:400–409.
Kruis W, Nguyen P, Morgenstern J. Granulocyte/Monocyte Apheresis in moderate to severe ulcerative colitis—effective or not? Digestion. 2015;92:39–44.
Dignass A, Akbar A, Hart A, et al. Safety and efficacy of granulocyte/monocyte apheresis in steroid-dependent active ulcerative colitis with insufficient response or intolerance to immunosuppressants and/or biologics [the ART Trial]: 12-week interim results. J Crohns Colitis. 2016;10:812–820.
Yoshimura N, Yokoyama Y, Matsuoka K, et al. An open-label prospective randomized multicenter study of intensive versus weekly granulocyte and monocyte apheresis in active Crohn’s disease. BMC Gastroenterol. 2015;15:163.
Sawada K, Muto T, Shimoyama T, et al. Multicenter randomized controlled trial for the treatment of ulcerative colitis with a leukocytapheresis column. Curr Pharm Des. 2003;9:307–321.
Sawada K, Kusugami K, Suzuki Y, et al. Leukocytapheresis in ulcerative colitis: results of a multicenter double-blind prospective case–control study with sham apheresis as placebo treatment. Am J Gastroenterol. 2005;100:1362–1369.
Yokoyama Y, Matsuoka K, Kobayashi T, et al. A large-scale, prospective, observational study of leukocytapheresis for ulcerative colitis: treatment outcomes of 847 patients in clinical practice. J Crohns Colitis. 2014;8:981–991.
Muratov V, Lundahl J, Ulfgren AK, et al. Down-regulation of interferon-gamma parallels clinical response to selective leukocyte apheresis in patients with inflammatory bowel disease: a 12-month follow-up study. Int J Colorectal Dis. 2006;21:493–504.
Hanai H, Lida T, Yamada M, et al. Effects of adacolumn selective leukocytapheresis on plasma cytokines during active disease in patients with active ulcerative colitis. World J Gastroenterol. 2006;12:3393–3399.
Belge KU, Farshid D, Horelt A, et al. The proinflammatory CD14+ CD16++ DR++ monocytes are a major source of TNF. J Immunol. 2002;168:3536–3542.
Hanai H, Lida T, Takeuchi K, et al. Adsorptive depletion of elevated proinflamatory CD14+ CD16+ DR++ monocytes in patients with inflammatory bowel disease. Am J Gastroenterol. 2008;103:1210–1216.
Cuadrado E, Alonso M, De Juan MD, Echaniz P, Arenas JI. Regulatory T cells in patients with inflammatory bowel diseases treated with adacolumn granulocytapheresis. World J Gastroenterol. 2008;14:1521–1527.
Kashiwagi N, Sugimura K, Saniabadi AR, et al. Immunomodulatory effects of granulocyte and monocyte adsorption apheresis as a treatment for patients with ulcerative colitis. Dig Dis Sci. 2002;47:1334–1341.
Hanai H, Takeuchi K, Lida T, et al. Relationship between fecal calprotectin, intestinal inflammation, and peripheral blood neutrophils in patients with active ulcerative colitis. Dig Dis Sci. 2004;49:1438–1443.
Passacquale G, Vamadevan P, Pereira L, Hamid C, Corrigall V, Ferro A. Monocyte-platelet interaction induces a pro-inflammatory phenotype in circulating monocytes. PLoS ONE. 2011;6:e25595.
Andoh A, Ogawa A, Kitamura K, et al. Suppression of interleukin-1beta- and tumor necrosis factor-alpha-induced inflammatory responses by leukocytapheresis therapy in patients with ulcerative colitis. J Gastroenterol. 2004;39:1150–1157.
Noguchi M, Hiwatashi N, Hayakawa T, et al. Leukocyte removal filter-passed lymphocytes produce large amounts of interleukin-4 in immunotherapy for inflammatory bowel disease: role of bystander suppression. Ther Apher. 1998;2:109–114.
Andoh A, Tsujikawa T, Inatomi O, et al. Leukocytapheresis therapy modulates circulating T-cell subsets in patients with ulcerative colitis. Ther Apher Dial. 2005;9:270–279.
Kanai T, Makita S, Kavamura T, et al. Extracorporeal elimination of TNF-α producing CD14(dull)CD16+ monocytes in leukocytapheresis therapy for ulcerative colitis. Inflamm Bowel Dis. 2007;13:284–290.
Kanai T, Hibi T, Watanabe M. The logics of leukocyteapheresis as a natural biological therapy for inflammatory bowel disease. Expert Opin Biol Ther. 2006;6:453–466.
Tsuchiya K, Hayashi R, Fukushima K, et al. CDX2 expression induced by leukocytapheresis might be associated with mucosal healing in ulcerative colitis. J Gastroenterol Hepatol. 2016. doi:10.1111/jgh.13645.
Danese S, Angelucci E, Stefanelli T, et al. Cytapheresis in inflammatory bowel diseases: current evidence and perspectives. Digestion. 2008;77:96–107.
Author information
Authors and Affiliations
Contributions
ES-G, IM, DA-S, FCD-J, EC, MI, PN and BB: Literature search and manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
This article offers an extensive review of the available literature on the topic of adsorptive cytapheresis and its use in patients with IBD. Here, we discuss its potential role as a non-pharmacologic agent, the technology involved, potential mechanisms of action with regard to cytokine and cell population changes, and future perspectives.
Rights and permissions
About this article
Cite this article
Sáez-González, E., Moret, I., Alvarez-Sotomayor, D. et al. Immunological Mechanisms of Adsorptive Cytapheresis in Inflammatory Bowel Disease. Dig Dis Sci 62, 1417–1425 (2017). https://doi.org/10.1007/s10620-017-4577-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4577-z