Abstract
Background
SLC25A13 gene mutations cause citrin deficiency, which leads to neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD). Information on the mutation spectrum of SLC25A13 in the Chinese population is limited. The aim of this study was to explore the mutation spectrum of the SLC25A13 gene in Chinese infants with intrahepatic cholestasis and various forms of aminoacidemia.
Methods
Sequence analyses were performed on 39 infants with intrahepatic cholestasis and various forms of aminoacidemia. Novel mutations were subjected to homology and structural analyses. Western blots were performed when liver specimens available.
Results
Genetic testing revealed the presence of SLC25A13 gene mutations (9 heterozygotes, 6 homozygotes and 13 compound heterozygotes) in 28 infants. Subsequent Western blot analysis revealed 22 cases of citrin deficiency, accounting for 56.4% of the 39 patients. Twelve types of mutations, including nine known mutations and three novel mutations, were found. Of the 49 mutated alleles, known ones include 851del4 (26 alleles, 53.1%), 1638ins23 (6 alleles, 12.2%), IVSl6ins3kb (3 alleles, 6.1%), IVS6+5G>A (2 alleles, 4.1%), E601K (2 alleles, 4.1%) and IVS11+1G>A, R184X, R360X and R585H (1 allele each, 2.0%). The three novel mutations were a splice site change (IVS6+1G>A), a deletion mutation (1092_1095delT) and a missense mutation (L85P), each in one allele.
Conclusions
The mutation spectrum of the SLC25A13 gene in a Chinese population of infants with intrahepatic cholestasis with various forms of aminoacidemia was found to be different from that of other population groups in East Asia. The SLC25A13 gene mutation is the most important cause of infantile intrahepatic cholestasis with various forms of aminoacidemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Citrin protein, consisting of 675 amino acid residues with a molecular weight of 74 kDa and harboring four EF-hands and six mitochondrial transmembranous (TM) spanners, has been identified as a mitochondrial aspartate–glutamate carrier protein [1, 2]. Citrin deficiency causes not only adult-onset type II citrullinemia (CTLN2, MIM #603471) [1] but also neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD, MIM #605814) [3, 4]. The symptoms of NICCD include intrahepatic cholestasis, mild liver dysfunction, an elevated aspartate aminotransferase/alanine aminotransferase ratio, failure to thrive, fatty liver, multiple forms of aminoacidemia, including citrullinemia, hypoproteinemia, hypoglycemia, coagulation disorders, and/or high levels of plasma α-fetoprotein [5–13]. Although the symptoms of most NICCD patients may spontaneously disappear by 12 months of age or after dietary adjustment, liver failure may occur, necessitating liver transplantation in a small proportion of such patients in early life [6, 14]. In less fortunate cases, CTLN2 may develop one or more decades later and may lead to death if treated inappropriately [15]. Early diagnosis of NICCD may prevent progression to CTLN2 by dietary adjustment or prevent serious consequences by close follow-up and timely treatment before the onset of symptoms; hence, early detection is extremely important in such patients [16]. Because the symptoms of NICCD are transitory and complex, it is not so easy to establish definite clinical diagnostic criteria, and the best diagnostic test for NICCD is a genetics test.
Citrin is encoded by the SLC25A13 gene located on chromosome 7q21.3 [1, 17]. This gene, 160 kb in length, consists of 18 exons and encodes a 3.4-kb transcript. It is expressed ubiquitously, but most abundantly in the liver. To date, more than 50 mutations have been identified [18], and all, with the exception of P632L, are pathogenic.
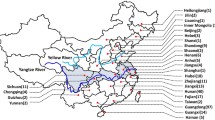
Citrin deficiency was thought to be restricted to the Japanese population when it was first reported in Japan [1, 19]. However, recent studies have indicated that the disease may be distributed worldwide [12, 20–24], especially in the East Asian region [25]. More than 100,000 individuals may be homozygous for SLC25A13 mutations in the total population of East Asia [23]. Only a few cases of NICCD have been reported in the Chinese population to date [9, 13, 18, 23, 25–27]. Details on the spectrum of the SLC25A13 gene mutation in Chinese infants with intrahepatic cholestasis is still under investigation. In this study, the SLC25A13 gene mutation spectrum was studied in Chinese infants with neonatal intrahepatic cholestasis and various forms of aminoacidemia.
Materials and methods
Definition of intrahepatic cholestasis
In this study, conjugated hyperbilirubinemia was defined as serum total bilirubin (TBil) >5 mg/dL, with a conjugated fraction that accounted for more than 20% of the total or conjugated bilirubin >1 mg/dL where total serum bilirubin <5 mg/dL. Intrahepatic cholestasis was defined as conjugated hyperbilirubinemia following the exclusion of diseases affecting the extrahepatic biliary system, such as biliary atresia, choledochal cyst, tumor, inspissated bile, or hemangioma, among others, by imaging of the hepatobiliary system. The imaging procedures included ultrasound scan and hepatobiliary iminodiacetic acid (HIDA) scintigraphy in each case and laparotomic cholangiography in selected cases.
Definition of aminoacidemia
The plasma amino acid spectrum was analyzed by tandem mass spectrometry (MS/MS). The concentrations of 19 amino acids, including alanine, valine, leucine, methionine, phenylalanine, tyrosine, aspartic acid, glutamic acid, glycine, ornithine, citrulline, arginine, serine, proline, threonine, tryptophan, cysteine, asparagine, and histidine, were determined. Aminoacidemia was defined as either of the following two conditions: (1) an elevation in the concentration of any one of the screened amino acids to twofold higher than the upper normal reference point; (2) elevation of multiple amino acids, with the concentration of at least one of the amino acids being 1.5-fold higher than the upper limit of normal.
Subjects
Patients who were referred to the Children’s Hospital of Fudan University, a tertiary referral pediatric hospital in eastern China, for investigation of conjugated hyperbilirubinemia before 1 year of age between June 2003 and September 2009 were eligible for enrollment if both of the definitions of intrahepatic cholestasis and aminoacidemia (see above) were satisfied. The exclusion criteria were:
-
1.
Patients with persistent cholestasis and low γ-glutamyl transpeptidase (GGT; no more than 50 U/L), which may be indicative of progressive familiar intrahepatic cholestasis or bile salt synthesis defects [28, 29].
-
2.
Patients with low free T4 and elevated thyroid stimulating hormone.
-
3.
Patients with obvious extrahepatic abnormalities, such as abnormal facies, heart disease, butterfly vertebrae, etc.
-
4.
Patients with positive serology that may indicate infection of hepatitis B, hepatitis C, hepatitis A and E, toxoplasmosis, rubella, herpes simplex, human immunodeficiency virus-1 or syphilis. Patients with cytomegalovirus (CMV) infection were not excluded because it is highly prevalent in Chinese infants, and patients infected with CMV have the same outcome as those without the infection [30, 31]. The presence of CMV infection has been found not to rule out other causes of intrahepatic cholestasis [26].
-
5.
Patients whose parents were unwilling to take part in the study.
In total, 39 patients (22 male and 17 female infants) fulfilled the above inclusion and exclusion criteria (Table 1) and were enrolled in the study. With the except of one patient, who was born of consanguineous parents (P2394, Table 1), no consanguinity was found among the parents of the enrolled infants.
An additional 50 infants with intrahepatic cholestasis but a normal plasma amino acid profile served as controls for the screening of the novel mutations using direct sequencing or real time fluorescent (RTD)-PCR with dual-labeled probes.
Mutation detection
The study protocol conforms to the ethical guidelines of the Declaration of Helsinki of 1975 and was approved by the Ethics Committee on human research of the Children’s Hospital of Fudan University. Informed consent was obtained from the parents or guardian of every participant. About 1 ml whole blood from each participant was obtained. Genomic DNA of peripheral blood leucocytes was extracted using routine methodology. The entire 18 coding exons together with its flanking sequence of the SLC25A13 gene of all 39 patients were amplified by PCR and directly sequenced. A list of primers is available upon request. Purified PCR products were detected by laser-induced fluorescence on an ABI Prism 3730 Genetic Analyzer (Applied Biosystems, Foster City, CA). Sequence analysis was performed using BIOEDIT software (North Carolina State University, Raleigh, NC) and double-checked by two of the investigators. All sequences were blasted to the gene bank. Genomic sequences were obtained at the National Center for Biotechnology Information (NCBI), and sequence RefSeq NG_012247.1 was used as the SLC25A13 gene reference. Possible mutations were confirmed by direct sequencing from both ends of a second independent PCR fragment. The known large fragment mutations Ex15dup (IVS14_15), IVS16ins3kb, and Ex16+74_IVS17-32del516 were tested as reported previously [20, 23, 32].
Homology and structural predictions
MaxEntScan was used to evaluate the role of splice site mutations (http://genes.mit.edu/burgelab/maxent/Xmaxentscan_scoreseq.html). The homology between human citrin protein and that of other species was surveyed using software Clustal X (European Bioinformatics Institute, Hinxton, Saffron Walde, UK). Secondary structures were predicted with YASPIN secondary structure prediction (http://www.ibi.vu.nl/programs/yaspinwww/). The program Polyphen (Polymorphism Phenotyping), available at: http://genetics.bwh.harvard.edu/pph/, was used to predict the possible impact of an amino acid substitution on the structure and function of citrin proteins. Polyphen calculates PSIC (position-specific independent counts) scores for two amino acid variants in the polymorphic position. A PSIC score difference of less than 0.5 denote benign variants, PSIC scores that differ by between 1.5 and 2 indicate the possibility of damaging variants, and PSIC scores that differ by >2 indicate the probability of damaging variants [33].
Western blot analysis
Western blot analysis was performed on the biopsied liver specimens of nine patients. Liver tissues were homogenized in radio-immunoprecipitation assay (RIPA) lysis buffer (Beyotime Institute of Biotechnology, Jiangsu, China) and the proteins extracted routinely. Western blotting was performed using anti-citrin immunoglobulin G as the first antibody [34] and horseradish peroxidase (HRP)-conjugated goat anti-rabbit antibodies as the secondary antibody. Fluorescence was effected with ECL+Plus kit (Thermo Fisher Scientific, Waltham, MA). HRP-conjugated monoclonal mouse anti-glyceraldehyde-3-phosphate dehydrogenase (GAPDH; KangChen Bio-tech Inc., China) was used served as loading control (detecting band at approx. 36 kDa).
Statistical analysis
The frequency of citrullinemia among the three groups, including patients with definite diagnosis of citrin deficiency, with probable citrin deficiency and patients without mutation were assessed using Fisher’s exact test. A two-tailed P value of <0.05 was considered to be significant.
Results
The incidence of citrin deficiency
Among the 39 cases of intrahepatic cholestasis and various forms of aminoacidemia, SLC25A13 gene mutations were found in 28 patients cases, including six patients with a homozygous mutation 13 patients with a compound heterozygous mutation, and nine patients with a heterozygous mutation (Table 1).
Western blotting were performed on the biopsied liver specimens from nine patients, of whom six had homozygous or compound heterozygous mutations (P2509, P2394, P1541, P2078, P3163, and P3174) and three had heterozygous mutations (P3156, P2625, and P2434). Citrin protein was absent in all specimens except that from the patient with homozygous mutation IVS6+1G>A (P2394), in which approximately 63- and 68-kDa immunoreactive bands were detected (Fig. 1). Western blot analysis was not performed for the other patients due to the lack of a liver specimen.
When the results of the Western blot of citrin protein and the genetic tests were analyzed together, at least 22 cases of citrin deficiency could be diagnosed, accounting for 56.4% of all the subjects. The other six patients in whom only a mutation was detected in an allele were diagnosed as probable citrin deficiency, although there is a possibility that some of these are really carriers. The diagnosis of citrin deficiency is unlikely in the 11 patients for whom no mutation was found because all 18 exons were tested.
SLC25A13 gene mutation spectrum
Twelve mutations (49 mutated alleles) were detected, of which three mutations were novel. These three novel mutations were splice site change IVS6+1G>A in one allele and missense mutation L85P and frameshift mutation 1092_1095delT in one allele each. Two other mutations, R585H and IVS11+1G>A, each in one allele, were detected in Chinese patients for the first time. The remaining seven mutations identified were: 851del4 (26 alleles, 53.1%), 1638ins23 (6 alleles, 12.2%), IVSl6ins3kb (3 alleles, 6.1%), IVS6+5G>A (2 alleles, 4.1%), E601K (2 alleles, 4.1%), and R184X and R360X (each in 1 allele, account for 2.0%, respectively).
The effect of novel mutations
The splice-site mutation IVS6+1G>A identified in P2394 represents a base substitution from G to A at the first position of the 5′-end in intron 6. The patient with homozygous mutation IVS6+1G>A/IVS6+1G>A (P2394) was born of parents who were second-generation cousins. Genetic tests on the parents indicated that both were heterozygotes of IVS6+1G>A. The scores of predicted splicing sites decreased significantly compared with the wild sequence (Table 2). Western blot analysis of the liver protein of this patient revealed the disappearance of the normal band but the appearance of two size-decreased bands (about 63 and 68 kDa in Fig. 1b).
The mutation L85P, which represents a T>C substitution at position 254 in exon 4 and an amino acid change from leucine to proline at position 85, was found in P3174. Analysis on the alignment of amino acids residual reservation in different species showed that the locative amino acid is highly conserved (Fig. 2). L85P was found in a compound heterozygote with E601K (Table 1). Western blot analysis with anti-human citrin antibody revealed the absence of citrin protein in the liver specimen (Fig. 1c), indicating that this mutation leads to citrin deficiency.
R585H, first reported in two Japanese patients with CTLN2 or NICCD [18, 35] with no detailed description, represents a G>A substitution at position 1754 in exon 17 and leads to an arginine to histidine substitution at position 585. Conservation analysis in different species indicated that the amino acid in this position is highly conserved [23], except in Danio rerio (Fig. 2). This is the first report of a Chinese patient with the R585H mutation.
Secondary structural prediction of the two missense mutations, L85P and R585H, using YASPIN showed that these variations in amino acids did not affect the secondary structure of citrin protein. The PSIC for the normal amino acid L85 and R585 is 1.54 and 2.133, respectively, and for the variant amino acid 85P and 585H, −1.007 and −0.335, respectively; thus, the absolute difference between the two profile scores is 2.547 and 2.468, respectively, indicating that both missense mutations have a high chance of affecting protein function.
The mutation 1092_1095delT (one of 4 conjoint bases of T deletion within nt 1092–1095 in exon 11) found in P3013, predicting a frame shift and the introduction of a stop codon at position 407, may lead to premature truncation of the citrin protein.
Mutation 1092_5delT and IVS6+1G>A were detected by PCR and the direct sequencing method. Mutation L85P was screened by RTD-PCR with dual-labeled probes L85P-FP 5′-AATATCTTTTCAAGAATTTGTTGCC-3′, L85P-RP 5′-GGTAGCCTTTCAGCTGTTTGAC-3′; fluorescence-labeled probes are MAR-TCTGTCCCGTGTGCCC-MAR and JUP-TCTGTCCTGTGTGCCC-JUP. Each of the above mutations was screened in 50 control infants, and none was detected in the 100 control alleles.
Aminoacidemia and the incidence of SLC25A13 gene mutations
To explore the relationship between SLC25A13 mutations and citrullinemia, we compared the data among three patient subgroups. Citrulline elevated more than 1.5-fold the upper normal limit (UNL) was found in 28 patients, including 19 of the 22 cases that could be definitely diagnosed as citrin deficiency, five of the six patients with probable citrin deficiency, and four of the 11 infants with unlikely citrin deficiency (no mutation was detected) (Table 1). Citrullinemia was more frequently found in patients with a definite diagnosis of citrin deficiency than in those in whom citrin deficiency was unlikely (definite diagnosis vs. unlikely, P = 0.006; probable vs. unlikely, P = 0.131).
Among the 11 patients with normal levels of plasma citrulline (P4129, P4115, P4487, P2338, P4542, P2769, P4684, P2516, P4068, P3013, P4163), the homozygous mutation was found in one patient (P4163) and the compound heterozygous mutation was found in two patients (P3013 and P4068).
Discussion
To the best of our knowledge, this is the first study on the SLC25A13 gene mutation spectrum in infants with intrahepatic cholestasis and various forms of aminoacidemia in mainland China. The design is different from those of the previous studies in which mutation analysis was generally only carried out on individuals for whom a diagnosis of citrin deficiency is highly suspected based on citrullinemia detected by MS analysis [6, 20, 32–39]. In contrast, we tested all cases of various forms of aminoacidemia, including those patients with citrulline in normal range and those who were given a possible diagnosis of tyrosinemia or aminoacidemia secondary to liver diseases on the basis of MS amino acid analysis. More than one half of the patients were given a definitive prognosis of citrin deficiency, including not only those with citrullinemia but also those with forms of aminoacidemia other than citrullinemia. This means that the SLC25A13 gene mutation is the most important cause of infantile intrahepatic cholestasis and various forms of aminoacidemia in this region.
Mutations 851del4 and IVS11+1G>A are two of the most prevalent mutations in Japan and Korea [25]. However, mutation IVS11+1G>A has never been reported in the Chinese population [23, 25], and we found only one mutant allele with IVS11+1G>A (P4405) in our study. Among our patients, mutations 851del4 and 1638ins23 were the two most common mutations. Mutation IVS6+5G>A, which had been identified to be the second most common mutation in the south area of China [23, 25], was found in only two patients (P4554 and P4068) of our study from the south area of China. This result suggests that mutation types have regional specificity within China.
Mutation IVS6+1G>A has not been reported in other countries to date. However, mutation IVS6+1G>C at the same site (named mutation XIV), but not G>A, has been reported [25]. Theoretically, the deduced product of mutation IVS6+1G>A should be much smaller than approximately the 63- and 68-kDa products revealed by Western blot analysis. The size difference may be caused by abnormal splicing, leading to the deletion of exons 7, 8, and 9 (total 318 nt, about 11 kDa) or the deletion of exon 6 (147 nt, about 6 kDa).
The presence of mutation L85P indicates a base substitution in exon 4, located in the middle part between the second and the third EF-hand domain (http://srs.ebi.ac.uk/cgi-bin/wgetz?-id+newId+-e+[SWALL-ACC:Q9UJS0]#Features), which is conserved in calcium-binding proteins [1]. To date, no mutation has been reported in this exon [18]. Western blot analysis on this patient (P3174; see Fig. 1c), with compound heterozygote E601K/L85P showing no detectable peptide, indicated that the mutation led to citrin deficiency. R585H is located in the sixth TM spanning one of the most functional domains of citrin protein. Mutations in this area may cause the abnormal function of citrin protein and result in clinical manifestations. 1092_1095delT leads to a premature truncated protein.
NICCD is a complicated metabolic disorder that is difficult to distinguish from other causes of hepatic disease. Aminoacidemia is one of the more important features of NICCD, but the diagnosis is difficult without early monitoring of amino acid levels [24]. MS to detect citrin deficiency is useful in identifying the clinical course, treatment, and prevention of this disease [38]. In this study, citrin deficiency was not only found in patients with citrullinemia, but also in patients with aminoacidemia other than citrullinemia, suggesting that although citrullinemia is a very useful parameter for the diagnosis of citrin deficiency, the diagnosis cannot be ruled out even if the level of citrulline is within normal range.
Based on amino acid profile, there were three suspected cases of possible tyrosinemia (P3013, P4068 and P2769). However, fumarylaceteoacetic acid hydrolase (FAH) gene sequencing did not reveal any mutation (data not shown). The SLC25A13 compound heterozygote was found in two patients (P3013 and P4068), and patient P2769 had no mutation (Table 1). Therefore, citrin deficiency should be considered in patients with any form of aminoacidemia, including tyrosinemia.
No mutation was detected in 11 patients with aminoacidemia. The amino acid profile of these patients is significantly different from that of patients with a definite diagnosis of citrin deficiency (Table 1). These 11 patients may have other metabolic disturbances, such as tyrosinemia, galactosemia [40] or just secondary to liver diseases other than citrin deficiency. Hence, the diagnosis of NICCD cannot be made based solely on the various forms of aminoacidemia, similar to the diagnosis of NICCD not being established based only on clinical manifestations and biochemical changes [13].
One limitation of this study was that we did not perform Western blotting on lymphocytes. We did attempt this in a previous study [41], but unfortunately failed. Consequently, we were unable to determine whether those patients that carried only one mutation allele were carriers or citrin-deficiency patients. Another limitation to our study was that direct sequencing may miss the mutation occurring in the primers and that the deletion/insertions of a large fragment also could be determined. This may explain why the second mutation was not find in patients cases with citrin deficiency (P3156, P2625 and P2434).
In conclusion, the results of this study indicate that SLC25A13 gene mutations play an important role in Chinese infants with intrahepatic cholestasis and various forms of aminoacidemia. 851del4 and 1638ins23 are the most common mutation types. Three novel mutations were found in our cohort of patients, which has expanded the SLC25A13 gene mutation spectrum.
References
Kobayashi K, Sinasac DS, Iijima M, Boright AP, Begum L, Lee JR, et al. The gene mutated in adult-onset type II citrullinaemia encodes a putative mitochondrial carrier protein. Nat Genet. 1999;22:159–63.
Palmieri L, Pardo B, Lasorsa FM, del Arco A, Kobayashi K, Iijima M, et al. Citrin and aralar1 are Ca(2+)-stimulated aspartate/glutamate transporters in mitochondria. EMBO J. 2001;20:5060–9.
Tazawa Y, Kobayashi K, Ohura T, Abukawa D, Nishinomiya F, Hosoda Y, et al. Infantile cholestatic jaundice associated with adult-onset type II citrullinemia. J Pediatr. 2001;138:735–40.
Yamaguchi N, Kobayashi K, Yasuda T, Nishi I, Iijima M, Nakagawa M, et al. Screening of SLC25A13 mutations in early and late onset patients with citrin deficiency and in the Japanese population: identification of two novel mutations and establishment of multiple DNA diagnosis methods for nine mutations. Hum Mutat. 2002;19:122–30.
Tomomasa T, Kobayashi K, Kaneko H, Shimura H, Fukusato T, Tabata M, et al. Possible clinical and histologic manifestations of adult-onset type II citrullinemia in early infancy. J Pediatr. 2001;138:741–3.
Tamamori A, Okano Y, Ozaki H, Fujimoto A, Kajiwara M, Fukuda K, et al. Neonatal intrahepatic cholestasis caused by citrin deficiency: severe hepatic dysfunction in an infant requiring liver transplantation. Eur J Pediatr. 2002;161:609–13.
Ohura T, Kobayashi K, Abukawa D, Tazawa Y, Aikawa J, Sakamoto O, et al. A novel inborn error of metabolism detected by elevated methionine and/or galactose in newborn screening: neonatal intrahepatic cholestasis caused by citrin deficiency. Eur J Pediatr. 2003;162:317–22.
Tazawa Y, Kobayashi K, Abukawa D, Nagata I, Maisawa S, Sumazaki R, et al. Clinical heterogeneity of neonatal intrahepatic cholestasis caused by citrin deficiency: case reports from 16 patients. Mol Genet Metab. 2004;83:213–9.
Song YZ, Hao H, Ushikai M, Liu GS, Xiao X, Saheki T, et al. A difficult and complicated case study: neonatal intrahepatic cholestasis caused by citrin deficiency (in Chinese with English abstract). Zhongguo Dang Dai Er Ke Za Zhi. 2006;8:125–8.
Ko JS, Song JH, Park SS, Seo JK. Neonatal intrahepatic cholestasis caused by citrin deficiency in Korean infants. J Korean Med Sci. 2007;22:952–6.
Ohura T, Kobayashi K, Tazawa Y, Abukawa D, Sakamoto O, Tsuchiya S, et al. Clinical pictures of 75 patients with neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD). J Inherit Metab Dis. 2007;30:139–44.
Dimmock D, Maranda B, Dionisi-Vici C, Wang J, Kleppe S, Fiermonte G, et al. Citrin deficiency, a perplexing global disorder. Mol Genet Metab. 2009;96:44–9.
Song YZ, Li BX, Chen FP, Liu SR, Sheng JS, Ushikai M, et al. Neonatal intrahepatic cholestasis caused by citrin deficiency: clinical and laboratory investigation of 13 subjects in mainland of China. Dig Liver Dis. 2009;41:683–9.
Shigeta T, Kasahara M, Kimura T, Fukuda A, Sasaki K, Arai K, et al. Liver transplantation for an infant with neonatal intrahepatic cholestasis caused by citrin deficiency using heterozygote living donor. Pediatr Transplant. doi: 10.1111/j.1399-3046.2009.01172.x.
Yazaki M, Takei Y, Kobayashi K, Saheki T, Ikeda S. Risk of worsened encephalopathy after intravenous glycerol therapy in patients with adult-onset type II citrullinemia (CTLN2). Intern Med. 2005;44:188–95.
Saheki T, Kobayashi K, Terashi M, Ohura T, Yanagawa Y, Okano Y, et al. Reduced carbohydrate intake in citrin-deficient subjects. J Inherit Metab Dis. 2008;31(3):386–94.
Sinasac DS, Crackower MA, Lee JR, Kobayashi K, Saheki T, Scherer SW, Tsuiet L-C. Genomic structure of the adult-onset type II citrullinemia gene, SLC25A13, and cloning and expression of its mouse homologue. Genomics 62:289–92.
Kobayashi K, Ushikai M, Song Y, Gao H, Sheng J, Tabata A, et al. Overview of citrin deficiency: SLC25A13 mutations and the frequency. J Appl Clin Pediatr. 2008;23:1553–7.
Ohura T, Kobayashi K, Tazawa Y, Nishi I, Abukawa D, Sakamoto O, et al. Neonatal presentation of adult-onset type II citrullinemia. Hum Genet. 2001;108:87–90.
Ben-Shalom E, Kobayashi K, Shaag A, Yasuda T, Gao HZ, Saheki T, et al. Infantile citrullinemia caused by citrin deficiency with increased dibasic amino acids. Mol Genet Metab. 2002;77:202–8.
Luder AS, Tabata A, Iijima M, Kobayashi K, Mandel H. Citrullinaemia type 2 outside East Asia-Israeli experience. J Inherit Metab Dis. 2006;29:59.
Dimmock D, Kobayashi K, Iijima M, Tabata A, Wong LJ, Saheki T, et al. Citrin deficiency: a novel cause of failure to thrive that responds to a high-protein, low-carbohydrate diet. Pediatrics. 2007;119:773–7.
Tabata A, Sheng JS, Ushikai M, Song YZ, Gao HZ, Lu YB, et al. Identification of 13 novel mutations including a retrotransposal insertion in SLC25A13 gene and frequency of 30 mutations found in patients with citrin deficiency. J Hum Genet. 2008;53:534–45.
Hutchin T, Preece MA, Hendriksz C, Chakrapani A, McClelland V, Okumura F, et al. Neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD) as a cause of liver disease in infants in the UK. J Inherit Metab Dis. doi:10.1007/s10545-009-1116-x
Lu YB, Kobayashi K, Ushikai M, Tabata A, Iijima M, Li MX, et al. Frequency and distribution in East Asia of 12 mutations identified in the SLC25A13 gene of Japanese patients with citrin deficiency. J Hum Genet. 2005;50:338–46.
Yeh JN, Jeng YM, Chen HL, Ni YH, Hwu WL, Chang MH. Hepatic steatosis and neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD) in Taiwanese infants. J Pediatr. 2006;148:642–6.
Song YZ, Sheng JS, Ushikai M, Hwu WL, Zhang CH, Kobayashi K. Identification and diagnosis of three novel mutations in SLC25A13 gene of neonatal intrahepatic cholestasis caused by citrin deficiency (in Chinese with English abstract). Zhonghua Er Ke Za Zhi. 2008;46:411–5.
Liu LY, Wang XH, Wang ZL, Zhu QR, Wang JS. Characterization of ATP8B1 gene mutations and a hot-linked mutation found in Chinese with progressive intrahepatic cholestasis and low GGT. J Pediatr Gastroenterol Nutr. 2010;50(2):179–83. doi:10.1097/MPG.0b013e3181c1b368.
Liu LY, Wang ZL, Wang XH, Zhu QR, Wang JS. ABCB11 gene mutations in Chinese children with progressive intrahepatic cholestasis and low γ glutamyltransferase. Liver Int. 2010;30(6):809–15. doi:10.1111/j.1478-3231.2009.02112.x.
Chang MH, Hsu HC, Lee CY, Wang TR, Kao CL. Neonatal hepatitis: a follow-up study. J Pediatr Gastroenterol Nutr. 1987;6:203–7.
Wang JS, Wang ZL, Wang XH, Zhu QR, Zheng S. The prognostic value of serum gamma glutamyltransferase activity in Chinese infants with previously diagnosed idiopathic neonatal hepatitis HK. J Paediatr. 2008;13:39–45.
Takaya J, Kobayashi K, Ohashi A, Ushikai M, Tabata A, Fujimoto S, et al. Variant clinical courses of 2 patients with neonatal intrahepatic cholestasis who have a novel mutation of SLC25A13. Metabolism. 2005;54:1615–9.
Ramensky V, Bork P, Sunyaev S. Human non-synonymous SNPs: server and survey. Nucleic Acids Res. 2002;30:3894–900.
Yasuda T, Yamaguchi N, Kobayashi K, Nishi I, Horinouchi H, Jalil MA, et al. Identification of two novel mutations in the SLC25A13 gene and detection of seven mutations in 102 patients with adult-onset type II citrullinemia. Hum Genet. 2000;107:537–45.
Song YZ, Ushikai M, Sheng JS, Iijima M, Kobayashi K. SLC25A13 gene mutation analysis in a pedigree of neonatal intrahepatic cholestasis caused by citrin deficiency. Zhonghua Er Ke Za Zhi. 2007;45:408–12.
Naito E, Ito M, Matsuura S, Yokota IE, Saijo T, Ogawa Y, et al. Type II citrullinaemia (citrin deficiency) in a neonate with hypergalactosaemia detected by mass screening. J Inherit Metab Dis. 2002;25:71–6.
Kobayashi K, Bang LY, Xian LM, Nishi I, Hsiao KJ, Choeh K, et al. Screening of nine SLC25A13 mutations: their frequency in patients with citrin deficiency and high carrier rates in Asian populations. Mol Genet Metab. 2003;80:356–9.
Tamamori A, Fujimoto A, Okano Y, Kobayashi K, Saheki T, Tagami Y, et al. Effects of citrin deficiency in the perinatal period: feasibility of newborn mass screening for citrin deficiency. Pediatr Res. 2004;56:608–14.
Hachisu M, Oda Y, Goto M, Kobayashi K, Saheki T, Ohura T, et al. Citrin deficiency presenting with ketotic hypoglycaemia and hepatomegaly in childhood. Eur J Pediatr. 2005;164:109–10.
Feillet F, Merten M, Battaglia-Hsu SF, Rabier D, Kobayashi K, Straczek J, et al. Evidence of cataplerosis in a patient with neonatal classical galactosemia presenting as citrin deficiency. J Hepatol. 2008;48:517–22.
Tokuhara D, Iijima M, Tamamori A, Ohura T, Takaya J, Maisawa S, et al. Novel diagnostic approach to citrin deficiency: analysis of citrin protein in lymphocytes. Mol Genet Metab. 2007;90(1):30–6.
Acknowledgments
We thank MSc Ms. LJ Fang and R Chen for carrying out the mutation test for IVSl6ins3kb, and Prof. YK Leung for the revision and editing of the manuscript. We also thank the patients and their parents for their kind cooperation as well as the physicians who referred the patients. This paper was partly supported by two grants (Nos. 30672257 and 30973230) from the National Natural Science Foundation of China and a grant for Shanghai Public Health Key Subject Construction (08GWZX0102), and was supported in part by a Grant for Asia-Africa Scientific Platform Program from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fu, HY., Zhang, SR., Wang, XH. et al. The mutation spectrum of the SLC25A13 gene in Chinese infants with intrahepatic cholestasis and aminoacidemia. J Gastroenterol 46, 510–518 (2011). https://doi.org/10.1007/s00535-010-0329-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-010-0329-y