Abstract
Background
It is still unknown whether laparoscopic liver resection is suitable for recurrent hepatocellular carcinoma (HCC) after previous curative hepatic resection.
Method
The perioperative outcomes of 40 patients treated with second surgery for recurrent HCC by partial hepatectomy were studied retrospectively. The second surgery was performed under laparotomy in 20 patients (laparotomy group) and under laparoscopy in 20 patients (laparoscopy group).
Results
Intraoperative blood loss (p < 0.0001) and the incidence of postoperative complications (p = 0.0004) were lower in the laparoscopy group than in the laparotomy group. The incidence rates of surgical site infection and intractable ascites were significantly higher in the laparotomy group than in the laparoscopy group (p = 0.0202, p = 0.0436, respectively). The proportion of patients classified as Clavien grade IIIa was higher in the laparotomy group than in the laparoscopy group (p = 0.0033). The duration of the postoperative hospital stay was significantly shorter in the laparoscopy group than in the laparotomy group (p < 0.0001).
Conclusions
Postoperative morbidity has been decreased by the introduction of laparoscopic liver resection in patients with recurrent HCC after curative hepatic resection. As a result, the duration of the postoperative stay is shorter.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although various therapeutic modalities, including percutaneous ablation therapy or transarterial chemoembolization (TACE), have been used for the treatment of recurrent hepatocellular carcinoma (HCC), repeated hepatectomy is a potentially curative therapy, and offers patients the possibility of long-term survival [1]. Repeated hepatectomy is more technically challenging than initial resection because of impaired liver function due to the progression of hepatitis, the presence of adhesions, and modifications in the anatomy due to the previous surgery. Laparoscopic liver resection has been gradually accepted as a choice of treatment for HCC, and previous studies [2, 3] have demonstrated the feasibility and safety of the procedure without increasing tumor dissemination. However, it is unknown whether laparoscopic liver resection is suitable for recurrent HCC after previous curative hepatic resection. The aim of this study is to compare the feasibility and safety of laparoscopic liver resection for recurrent HCC with those of liver resection under laparotomy during the same period. To the best of our knowledge, this report is the largest series of laparoscopic repeated liver resections for recurrent HCC in a single institution.
Patients and methods
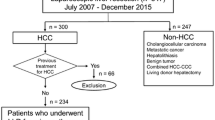
From 2006 to 2011, 65 patients underwent liver resection for recurrent HCC after curative hepatic resection in the Department of Hepato-Biliary-Pancreatic Surgery, Osaka City General Hospital, Osaka, Japan. To eliminate operative bias, patients receiving anatomical liver resection, non-curative resection or synchronous other organ resection were excluded. We retrospectively studied 40 patients divided into two groups according to whether the second operation was performed under laparotomy (laparotomy group, 20 cases) or under laparoscopy (laparoscopy group, 20 cases). Perioperative outcomes, including postoperative complications, were compared between these two groups. Blood loss was estimated using the volume of blood aspirated from the abdominal cavity during surgery. Operative time was defined as the time interval from the beginning of the skin incision until closure. Tumor location was divided into segments II–IV (so-called laparoscopic segments [4]), segments VII and VIII (non-laparoscopic segments), segment I, and bilober. Morbidity was graded according to Clavien classification [5]. Surgical site infection (SSI) was defined as a condition in which purulent discharge was observed from any incision or space that had been manipulated during an operation with or without microbiological evidence, as in the guidelines issued by the Centers for Disease Control and Prevention (CDC) [6], and was identified prospectively by direct observation of the surgical site. Intractable ascites was defined as a condition requiring use of diuretics or thoracocentesis, abdominal paracentesis on 2 or more occasions, or institution of continuous drainage or requiring skin suture of the drain site after the removal of the drain because of the continuous discharge of ascites. The variables identifying postoperative hepatic failure included hepatic coma with hyperbilirubinemia (total serum bilirubin concentration >5 mg/dl for more than 5 days) [7].
In patients who underwent laparoscopic repeated liver resection twice, the corresponding data were analyzed separately for each procedure.
Indications for liver resection
Patients with recurrent HCC after curative hepatic resection were evaluated before surgery according to a specified protocol including blood examinations, abdominal ultrasonography, multidetector row computed tomography (MDCT), esophagogastroduodenoscopy, and spirometry as well as before primary resection for HCC. Magnetic resonance imaging angiography or contrast-enhanced harmonic sonography was performed in selected patients. Patients were selected for surgery according to a published flow chart based on the presence of ascites, total serum bilirubin level and indocyanine green retention rate at 15 min (ICG-R15) [8]. We introduced laparoscopic repeated liver resection for patients with recurrent HCC in 2009 at our hospital. Since the introduction of laparoscopic repeated liver resection, we have increasingly chosen this procedure over the previously used open procedure.
Surgical procedure
Open repeated liver resection was performed through a subcostal (monolateral or bilateral) incision with an upward midline incision using the previous surgical scar. In some patients, a new location for skin incision was selected. After dissection of the intra-abdominal adhesions, intraoperative ultrasonography was performed routinely. Hepatic parenchymal transection was performed using an ultrasonic surgical aspirator and bipolar or monopolar forceps with soft coagulation (VIO System™) after a Pringle maneuver if possible.
For laparoscopic repeated liver resection, patients were placed in the supine (French) position with the main surgeon positioned on the right side of the patient and a endoscopist positioned between the legs. When lesions were located in the right lateral sector, patients were placed in the left lateral decubitus position. First, trocar for endoscope was inserted using an open technique avoiding the previous surgical scar and a continuous carbon dioxide pneumoperitoneum was induced at a pressure less than 10 mmHg to avoid gas embolism. After insertion of the second trocar into the abdominal cavity without peritoneal adhesion, meticulous dissection of the intra-abdominal adhesions was performed minimally around the area for repeated hepatectomy using a harmonic scalpel and bipolar scissors under a surgical flexible laparoscope. Standard diagnostic and staging laparoscopy was followed by intraoperative ultrasonography to evaluate tumor status and to assist liver resection. Hepatic transection was performed using a laparoscopic ultrasonic surgical aspirator and bipolar or monopolar forceps with soft coagulation. The Pringle maneuver using a temporary endoscopic clip was performed if necessary. If there was difficulty locating the tumor using laparoscopy alone due to limited visibility and the difficulty of controlling bleeding, we used hand-assisted laparoscopic surgery [9] or a hybrid procedure also called laparoscopy-assisted surgery [10].
The resected undivided specimen was placed in a plastic bag and removed through the slightly enlarged port site or small incision site in hand-assisted or laparoscopy-assisted liver resection. Just after taking out the resected specimen, we routinely checked the surgical margin of HCC during the laparoscopic liver resection. One or two closed drains were inserted close to the cut surface of the liver parenchyma before closing the abdominal wound in both groups. Before the subcutaneous tissue was closed, the wound was washed with saline. An absorbable suture material was used during abdominal wound closure. Intravenous cephazolin (CMZ) 1 g was administered 30 min before surgery and additional CMZ was administered every 3 h. Systemic antibiotics were used for 2 days after surgery. Drains were removed when no bleeding or bile leakage was observed within 3 days after surgery.
Statistical analysis
Continuous clinicopathological data were expressed as median (range). Differences between the two groups were analyzed using the Mann–Whitney U test. Categorical variables were analyzed by means of the Chi-square test or Fisher’s exact test. P values less than 0.050 were considered statistically significant.
Results
Patient and tumor characteristics of the two groups are summarized in Tables 1 and 2, respectively. No significant differences were observed in the characteristics of patients between the two groups: age, gender ratio, Child–Pugh grade, type of infected hepatitis, proportion of patients with histological liver cirrhosis (F4 by the New Inuyama classification system [11]) in the non-cancerous area of the resected liver, and laboratory test results. The median interval between the first hepatic resection and the second surgery for recurrent HCC in the laparoscopy group was 33 months which is not significantly different from that of the laparotomy group, 31 months (Table 1). Also, there were no significant differences in tumor size, resected liver weight, tumor number, or tumor location between the two groups (Table 2). Two cases were converted to hand-assisted liver resection although we had attempted pure laparoscopic liver resection first. In the laparotomy group, five types of long skin incision (right subcostal, reverse-T, right oblique, upper midline, and left subcostal) were selected according to the previous surgical scar and the location of the recurrent tumor. Intraoperative and postoperative outcomes of the two groups are summarized in Table 3. Although there were no significant differences in operating time between the two groups, intraoperative blood loss (p < 0.0001) and the rate of red cell concentrate (RCC) transfusion (p = 0.00471) were both lower in the laparoscopy group than in the laparotomy group. There were no significant differences in surgical margin between the two groups. In the laparotomy group, there was zero mortality and 13 patients had morbidity: 7 patients had ascites which were classified as 3 grade I and 4 grade IIIa requiring skin suture under local anesthesia at the leakage point of the ascites; and 6 patients had SSI (grade IIIa), including 3 incisional SSI requiring wound drainage under local anesthesia and 3 organ/space SSI requiring several surgical interventions under local anesthesia, one postoperative bleeding required re-operation for hemostasis (grade IIIb), one delayed gastric emptying (grade II) required placement of a nasogastric drainage tube for 10 days, and one renal failure (grade IVa) required transient hemodialysis. Thus, 13 patients suffered 16 morbidities in the laparotomy group. However, in the laparoscopy group, there was no mortality and only one patient had morbidity, ascites (grade IIIa). As a result, the morbidity rate in the laparoscopy group was significantly lower than that in the laparotomy group (p = 0.0004). The incidence rates of ascites and SSI were significantly higher in the laparotomy group than in the laparoscopy group (p = 0.0436, p = 0.0202, respectively). The bacteria isolated from the incisional site were Methicillin-sensitive Staphylococcus aureus, Methicillin-resistant Staphylococcus epidermidis, Enterococcus avium, and the bacteria from the organ/space site were Methicillin-sensitive Staphylococcus aureus (n = 3). The incidences of postoperative bleeding, delayed gastric emptying, renal failure, and hepatic failure were not different between the two groups. The proportion of patients classified as Clavien grade IIIa was higher in the laparotomy group than in the laparoscopy group (p = 0.0033, Table 4). As a result, the duration of the postoperative hospital stay was significantly shorter in the laparoscopy group than in the laparotomy group (p < 0.0001).
We studied the operative outcomes of cases in the laparoscopy group without regard to whether previous hepatic resection had been performed under laparotomy or laparoscopy (Table 5). Although the operating time for these five patients was shorter than that for the other 15 patients (p = 0.00495), there were no significant differences in the rates of liver cirrhosis (F4), conversion rates to hand-assisted laparoscopic liver resection (HALS), intraoperative blood loss, postoperative mortality, morbidity, or hospital stay.
Discussion
Laparoscopic hepatectomy after open liver resection is as difficult as repeated open hepatectomy because of the vascular-rich adhesions between the abdominal wall at the original large surgical scar and the resected portion of the liver. We think that the long skin incision may induce several disadvantages for patients in addition to cosmetic outcome. First, the larger skin incision and larger dissection area may increase the postoperative complications. A larger wound may give rise to more wound pain, possibly resulting in impaired kinetics of the diaphragm followed by respiratory complications. Increased damage to the collateral circulation or lymphatic circulation around the liver may cause intractable ascites postoperatively. A larger wound or wider dissection area of previous surgical adhesion appears to increase the risk of SSI or incisional hernia. In this study, the incidences of intractable ascites, SSI and Clavien grade IIIa complications were significantly higher in the laparotomy group than in the laparoscopy group. The incidence of SSI in this study was 30 % in the laparotomy group which is greater than the previously reported incidence of SSI: 20–25 % in patients who underwent liver resection [12, 13]. SSI did not develope in the laparoscopy group. Many studies have shown that the incidence of incisional SSI is lower after laparoscopic surgery than after conventional open surgery in patients who undergo colon resection [14]. These differences in colon surgery in this study are thought to be related directly to the size of the incisional wound. In the laparotomy group, the abdominal wall of the wound was often dry during surgery, which may decrease its ability to protect against infection. Because the bacteria isolated from the surgical infection site were skin flora in 5 of the 6 SSI patients, the small surgical wound created during laparoscopic liver resection may have the advantage of reducing SSI compared with conventional open surgery. In the laparoscopy group, meticulous dissection of the intra-abdominal adhesions can be performed by pneumoperitoneal pressure with its improvement in visual field and therefore the region of damage to the collateral circulation (i.e. the dissection area) could be minimized and the collateral circulation could be preserved. Consequently, the development of postoperative ascites may be suppressed, and this may lead to a lower incidence of postoperative ascites. The low incidence rates of intractable ascites and SSI results in a decreased number of patients who need invasive procedures for postoperative complications and a shortened postoperative hospital stay. Secondly, a large skin incision for hepatic resection would cause a disturbance in the treatment for recurrent HCC. Postoperative portal hypertension caused by damaging the collateral circulation may impair the function of the remnant liver postoperatively. In addition, intestinal adhesion to the surgical wound on the site of HCC recurrence may disturb ablation therapy, and developing collateral arteries to the recurrent HCC from the abdominal wall of the surgical scar may disturb TACE in some patients. Our study revealed that the operating time for five patients receiving laparoscopic liver resection for primary surgery for HCC was significantly shorter than that for patients who were treated by open liver resection for primary HCC (p = 0.00495, Table 5). However, there were no significant differences for conversion rate to HALS, blood loss, morbidity rate, or postoperative hospital stay. Therefore, a laparoscopic approach for the first treatment of HCC would seem to be advisable if possible. Intra-abdominal adhesion after repeated hepatectomy for recurrent HCC after laparoscopic liver resection was slight and located only at the small surgical wound for removing the resected specimen and port site. This means that adhesiolysis is minimizied. Therefore, laparoscopic liver resection appears to have important advantages, providing a better opportunity and situation for repeated hepatectomy for recurrent HCC. However, a larger series is needed to confirm this.
Conclusion
Even in cases of recurrent HCC, laparoscopic liver resection reduces intraoperative blood loss and leads to fewer cases of postoperative ascites, SSI, and Grade IIIa complications, and consequently shortens the length of hospitalization. Laparoscopic liver resection is also a safe and feasible procedure for treating patients with recurrent HCC.
References
Minagawa M, Makuuchi M, Takayama T, Kokudo N. Selection criteria for repeat hepatectomy in patients with recurrent hepatocellular carcinoma. Ann Surg. 2003;238:703–10.
Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, et al. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg. 2005;189:190–4.
Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, et al. Laparocsopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg. 2006;243:499–506.
Dagher I, Proske JM, Carloni A, Richa H, Tranchart H, Franco D. Laparoscopic liver resection: results for 70 patients. Surg Endosc. 2007;21:619–24.
Dindo D, Demartines N, Clavien P. Classifiction of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999;20:250–278;quiz 279–80.
Kubo S, Tsukamoto T, Hirohashi K, Tanaka H, Shuto T, Takemura S, et al. Correlation between preoperative serum concentration of type IV collagen 7s domain and hepatic failure following resection of hepatocellular carcinoma. Ann Surg. 2004;239:186–93.
Makuuchi M, Kosuge T, Takayama T, Yamazaki S, Kakazu T, Miyagawa S. Surgery for small liver cancers. Semin Surg Oncol. 1993;9:298–304.
Fong Y, Jarnagin W, Conlon KC, DeMateo R, Dougherty E, Blumagart LH. Hand-assisted laparoscopic liver resection: lessons from an initial experience. Arch Surg. 2000;135:854–9.
Nitta H, Sasaki A, Fujita T, Itabashi H, Hoshikawa K, Takahara T, et al. Laparoscopy-assisted major liver resections employing a hanging technique. Ann Surg. 2011;251:450–3.
Ichida F, Tsuji T, Omata M, Ichida T, Inoue K, Kamimura T. New Inuyama classification; new criteria for histological assessment of chronic hepatitis. Int Hepatol Commun. 1996;6:112–9.
Togo S, Matsuo K, Tanaka K, Matsumoto C, Shimizu T, Ueda M, et al. Perioperative infection control and its effectiveness in hepatectomy patients. J Gastroenterol Hepatol. 2007;22:1942–8.
Wu CC, Yeh DC, Lin MC, Liu TJ, P’eng FK. Prospective randomized trial of systemic antibiotics in patients undergoing liver resection. Br J Surg. 1998;85:489–93.
Murray BW, Cipher DJ, Pham T, Anthony T. The impact of surgical site infection on the development of incisional hernia and small bowel obstruction in colorectal surgery. J Am Coll Surg. 2010;211:812–22.
Conflict of interest
All authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kanazawa, A., Tsukamoto, T., Shimizu, S. et al. Laparoscopic liver resection for treating recurrent hepatocellular carcinoma. J Hepatobiliary Pancreat Sci 20, 512–517 (2013). https://doi.org/10.1007/s00534-012-0592-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-012-0592-9