Abstract
Background/purpose
The resectability of locally advanced pancreatic cancer depends upon, before anything else, the relationship between the tumor and the adjacent arterial structure. Pancreatic cancer that has developed at the caudal side of the pancreas can invade the common hepatic artery (CHA). Pancreatic cancers with CHA involvement can become candidates for surgery in selected cases. Pancreatic cancer arising at the caudal side of the pancreas head may sometimes invade the right and left hepatic arteries (RLHA) as well as the CHA. Pancreatic cancer with RLHA involvement may be assessed as unresectable unless complex vascular reconstruction is performed.
Methods
We have experienced 3 cases of successfully resected pancreatic cancer with RLHA and portal vein (PV) invasion. Pancreatectomy (including total pancreatectomy in two cases and pancreatoduodenectomy in one case) with RLHA and PV reconstruction was performed. Three different techniques of arterial reconstruction that were suitable for the individual cases were used. They were: (1) end-to-end anastomosis between the CHA and the left hepatic artery (LHA) and end-to-end anastomosis between the middle hepatic artery (MHA) and the right hepatic artery (RHA), (2) end-to-end anastomosis between the left gastric artery (LGA) and the RHA and end-to-end anastomosis between the right gastroepiploic artery and the LHA, and (3) end-to-side anastomosis between the splenic artery (SA) and the LHA and end-to-end anastomosis between the SA and the RHA.
Results
The mean operating time was 735 min (range 686–800 min) and the mean blood loss was 1726 ml (range 1140–2230 ml). Microscopic curative resection (R0) was possible in all cases even if their International Union Against Cancer (UICC) stage was IIb. There was one case of wound infection, although no serious complications, including hepatic artery thrombosis, liver failure, or biliary fistula were observed. By follow-up three-dimensional computed tomography (3D-CT) angiography, the patency of the anastomosed artery was confirmed to be maintained in all three cases.
Conclusions
R0 operation with 3 different arterial reconstruction techniques was able to be performed without presenting any risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The form of hepatic artery (HA) bifurcation is diverse and tumor invasion to the right and left hepatic arteries (RLHA) can occur depending upon the extent of the tumor. Cancers of the pancreatic head involving the RLHA are usually assessed as unresectable. Serious problems including the presence of arterial variants can happen when hepatic transplantation takes place. Various techniques of arterial reconstruction have thus been developed [1]. On the basis of experience in the use of these techniques, we performed pancreatectomy in 3 patients with cancers of the pancreatic head with RLHA and portal vein (PV) involvement. Techniques of reconstruction that were suitable for the individual cases are reported in the present article.
Surgical techniques
Case 1
Case 1 was a man 64 years of age in whom end-to-end anastomosis between the common hepatic artery (CHA) and the left hepatic artery (LHA), along with end-to-end anastomosis of the middle hepatic artery (MHA) and the right hepatic artery (RHA) was performed.
The RHA, the LHA, the MHA and the left lateral hepatic artery (LLHA) were exposed by dissection of the hepatoduodenal ligament. The celiac artery, the CHA, the splenic artery (SA) and the left gastric artery (LGA) were also dissected and exposed with care (Fig. 1). Despite the presence of tumor involvement in the RHA, the LHA, and the CHA, curative pancreatic resection with arterial resection was thought to be possible. As a usual procedure of pancreatoduodenectomy, the bile duct, the pancreas, and the duodenum were cut. The length between the cut ends of the CHA and the RHA was considered too long for end-to-end anastomosis, although it was thought that anastomosis between the CHA and the LHA could be performed without difficulty. The CHA, the LHA, and the RHA were ligated and divided at the dotted lines shown in Fig. 1, and the specimens were removed. The cut ends of the CHA and LHA were anastomosed with each other in an end-to-end fashion with 7-0 proline interrupted sutures (Fig. 2, green circle). After vascular control had been released, the back flow from the RHA was weak, so additional RHA reconstruction was considered necessary. Owing to sufficient intersegmental arterial communication between the medial and left lateral segments of the liver, no change was noted in the back flow of the RHA after a vascular clamp had been applied tentatively to the MHA. Therefore the MHA was ligated and divided at the blue dotted line shown in Fig. 1, and the cut ends of the MHA and RHA were anastomosed in an end-to-end fashion (Fig. 2, blue circle). Portal vein (PV) reconstruction was completed prior to the removal of specimens. Postoperative three-dimensional computed tomography (3D-CT) angiography showed that both the anastomosed arteries were patent, and visualization of the LLHA and RHA was achieved (Fig. 3). The green dotted circle in Fig. 3 shows the site of the CHA-LHA anastomosis and the blue dotted circle shows the site of the MHA-RHA anastomosis. The operating time was 686 min and blood loss was 1810 ml. R0 resection was possible.
Operative photograph of Case 1 showing dissection around the arteries. The right hepatic artery (RHA), the left hepatic artery (LHA), the middle hepatic artery (MHA), and the left lateral hepatic artery (LLHA) were dissected at the hepatoduodenal ligament. The celiac artery, the common hepatic artery (CHA), the splenic artery (SA), and the left gastric artery (LGA) were also dissected with care. The dotted lines show the planned resection lines
Operative photograph of Case 1 showing that reconstruction was completed. End-to-end anastomosis was performed between the common hepatic artery (CHA) and the left hepatic artery (LHA; green circle), and end-to-end anastomosis was performed between the middle hepatic artery (MHA) and the right hepatic artery (RHA; blue circle)
Case 2
Case 2 was a woman 75 years of age in whom end-to-end anastomosis between the LGA and the RHA was performed concomitantly with end-to-end anastomosis of the right gastroepiploic artery (RGEA) and the LHA. Pancreatoduodenectomy was performed for cancer of the pancreatic head and the CHA was divided at the origin of the celiac artery. The RGEA was obtained as a pedicle from the greater curvature of the stomach. End-to-end anastomosis was thus carried out between the LGA and the RHA. After declamping had been achieved, the back flow from the cut end of the LHA was weak, so end-to-end anastomosis between the RGEA and the LHA was carried out additionally (Fig. 4). The operating time was 800 min and blood loss was 1140 ml. R0 resection was possible.
Operative photograph of Case 2 showing that reconstruction was completed. End-to-end anastomosis was carried out between the left gastric artery (LGA) and the RHA, and end-to-end anastomosis was carried out between the right gastroepiploic artery (RGEA) and the LHA. SMA, Superior mesenteric artery; SA, splenic artery
Case 3
Case 3 was a man 57 years of age in whom end-to-side anastomosis between the splenic artery (SA) and the LHA was performed concomitantly with end-to-end anastomosis of the SA and RHA.
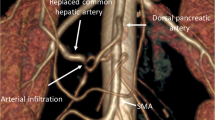
Total pancreatectomy was performed for pancreatic head-to-body cancer. Considering that there was no cancer involvement around the SA, the SA was reserved as a candidate blood vessel for RLHA reconstruction. Following the turnover of the SA to the right side, end-to-side anastomosis was performed between the SA and the LHA. Following declamping, the back flow from the cut end of the RHA was insufficient, so the SA and the RHA were anastomosed with each other in an end-to-end fashion (Fig. 5). The operating time was 720 min and blood loss was 2230 ml. R0 resection was possible.
Discussion
Due to the high frequency of arterial variants around the pancreas, some cases of arterial variants that are unfavorable for pancreatectomy may be assessed as unresectable or result in noncurative resection. Pancreatic cancer arising at the caudal side of the pancreatic head may occasionally invade the CHA. In patients in whom the RLHA have separated from each other at the origin of the CHA, tumor invasion may be observed in the RLHA. There are some opinions concerning the necessity for reconstruction of both the RLHA. For example, there is an opinion that no problems related to unilateral reconstruction will arise if both the RLHA have been divided. A rationale for this argument is based on the presence of a communicating arcade between the RLHA at the hepatic hilum [2, 3]. On the other hand, there is an argument that the presence of this communication may not necessarily mean that there is a sufficient amount of blood flow. There is a possibility that liver infarction and/or biliary complication will result if the blood flow is sparse [4]. A communicating arcade is also present between the lateral and medial segments of the liver [5]. Despite the use of the severed MHA for RHA reconstruction in Case 1 in the present study, the postoperative course was found to be uneventful. Although, in most cases, reconstruction can be performed with end-to-end anastomosis for the CHA, the reconstruction techniques already described in this article were necessary in cases requiring reconstruction of the RLHA. Although diverse techniques with the use of a venous graft, an arterial graft, or prosthetic materials can be applied at the time of hepatic artery reconstruction [1, 6–9], it should be borne in mind that anastomosis should be conducted for two sites when a graft is used, thus making the operative procedure complicated. The risk of infection should also be taken into consideration when prosthetic materials have been made use of. In this series, we employed the LGA, the RGEA, the SA, MHA, and the CHA as the inflow arteries for RLHA reconstruction, but no complications, including hepatic artery thrombosis, liver failure, or biliary fistula occurred. Postoperative 3D-CT showed that the patency of the anastomosed arteries was maintained in all three patients. Further examinations are needed to establish the significance of these operative techniques, although the R0 operation can be carried out safely even for locally advanced pancreatic cancer with RLHA involvement, on condition that the operative procedures to be used are well planned.
References
Del Gaudio M, Grazi GL, Ercolani G, Ravaioli M, Varotti G, Cescon M, et al. Outcome of hepatic artery reconstruction in liver transplantation with an iliac arterial interposition graft. Clin Transplant. 2005;19:399–405.
Tohma T, Cho A, Okazumi S, Makino H, Shuto K, Mochiduki R, et al. Communicating arcade between the right and left hepatic arteries: evaluation with CT and angiography during temporary balloon occlusion of the right or left hepatic artery. Radiology. 2005;237:361–5.
Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Yoshidome H, et al. Unilateral hepatic artery reconstruction is unnecessary in biliary tract carcinomas involving lobar hepatic artery: implications of interlobar hepatic artery and its preservation. Hepatogastroenterology. 2000;47:1526–30.
Allendorf JD, Bellemare S. Reconstruction of the replaced right hepatic artery at the time of pancreaticoduodenectomy. J Gastrointest Surg. 2009;13:555–7.
Cho A, Gunji H, Koike N, Narumoto S, Asano T, Yamamoto H, et al. Intersegmental arterial communication between the medial and left lateral segments of the liver. Dig Surg. 2007;24:328–30.
Yekebas EF, Bogoevski D, Cataldegirmen G, Kunze C, Marx A, Vashist YK, et al. En bloc vascular resection for locally advanced pancreatic malignancies infiltrating major blood vessels: perioperative outcome and long-term survival in 136 patients. Ann Surg. 2008;247:300–9.
Sasson AR, Hoffman JP, Ross EA, Kagan SA, Pingpank JF, Eisenberg BL. En bloc resection for locally advanced cancer of the pancreas: is it worthwhile? J Gastrointest Surg. 2002;6:147–8.
Adham M, Mirza DF, Chapuis F, Mayer AD, Bramhall SR, Coldham C, et al. Results of vascular resections during pancreatectomy from two European centres: an analysis of survival and disease-free survival explicative factors. HPB (Oxford). 2006;8:465–73.
Stitzenberg KB, Watson JC, Roberts A, Kagan SA, Cohen SJ, Konski AA, et al. Survival after pancreatectomy with major arterial resection and reconstruction. Ann Surg Oncol. 2008;15:1399–406.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Amano, H., Miura, F., Toyota, N. et al. Pancreatectomy with reconstruction of the right and left hepatic arteries for locally advanced pancreatic cancer. J Hepatobiliary Pancreat Surg 16, 777–780 (2009). https://doi.org/10.1007/s00534-009-0202-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-009-0202-7