Abstract
Background
The arterial anatomy supplying the liver is highly variable. One of the most common variants is a completely replaced right hepatic artery which is seen in about 11% of the population. Interruption of arterial flow to the right hepatic artery at the time of pancreaticoduodenectomy has been associated with biliary fistula and the consequent complications, as well as stenosis of the biliary enteric anastomosis. Malignancies of the posterior aspect of the head of the pancreas can encase a replaced right hepatic artery without involvement of other vascular structures. In this situation, it is possible to resect and reconstruct the replaced right hepatic artery to maintain oxygen delivery to the biliary enteric anastomosis.
Summary
Herein we describe a technique to reconstruct a replaced right hepatic artery following resection of the vessel en bloc with the tumor during a pancreaticoduodenectomy, using inflow from the gastroduodenal artery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
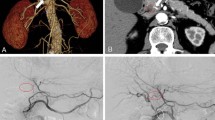
The arterial anatomy supplying the liver is highly variable. No less than ten anatomic variants have been described.1 In the configuration typically described as ‘normal’ in anatomy textbooks, the celiac truck gives rise to the common hepatic artery which then branches into the gastroduodenal and proper hepatic arteries. The right and left hepatic arteries are then branches of the proper hepatic artery. This anatomy is seen in about 55% of patients,1 while the remainder will exhibit an anatomic variant. One of the most common variants is a completely replaced right hepatic artery which is seen in about 11% of the population.1 A replaced right hepatic artery originates from the superior mesenteric artery, courses either within the pancreatic head or posterior to it, and then superiorly along the right posteriolateral border of the common bile duct before entering the right lobe of the liver (Figs. 1 and 2).
Operative photograph of the hepatoduodenal ligament demonstrating the aberrant anatomy of the replaced right hepatic artery. The bile duct has been transected and the distal portion has been reflected inferiorly. pCBD proximal common bile duct, dCBD distal common bile duct, RHA replaced right hepatic artery, CHA common hepatic artery, GDA gastroduodenal artery, PV portal vein.
Ligation of the right hepatic artery can have grave consequences for the patients undergoing pancreaticoduodenectomy because most of the blood supply to the common bile duct remnant is derived from the right hepatic artery following ligation of the gastroduodenal artery at the time of resection. Interruption of arterial flow to the right hepatic artery at the time of pancreaticoduodenectomy has been associated with biliary fistula and the consequent complications, as well as stenosis of the biliary enteric anastomosis. These complications are presumed to be a function of ischemia of the distal end of the common bile duct remnant.2,3
Malignancies of the posterior aspect of the head of the pancreas can encase a replaced right hepatic artery without involvement of other vascular structures. In this situation, it is possible to resect and reconstruct the replaced right hepatic artery to maintain oxygen delivery to the biliary enteric anastomosis. Sarmiento et al. previously described using inflow from the gastroduodenal artery to reconstruct an injured proper hepatic artery.4 Herein we describe a similar technique to reconstruct a replaced right hepatic artery following resection of the vessel en bloc with the tumor during a pancreaticoduodenectomy.
Technique
Once it has been determined that the tumor involves the replaced right hepatic artery, but is otherwise resectable, the hepatoduodenal ligament is dissected. The neck of the pancreas is divided. The patient is heparinized after obtaining vascular control of the common hepatic, proper hepatic artery, and replaced right hepatic arteries. The gastroduodenal artery is divided preserving as much length as possible. The uncinate dissection is completed, excising the segment of replaced right hepatic artery that is encased in tumor. The replaced right hepatic artery is ligated at its origin with the superior mesenteric artery. The remaining cut ends of the replaced right hepatic artery and gastroduodenal artery are then anastomosed to each other in an end-to-end fashion with interrupted sutures of 8-0 prolene. Vascular control is released and pulsitile flow is confirmed in the right hepatic artery (Figs. 3 and 4).
Operative photograph of the hepatoduodenal ligament following segmental resection and reconstruction of the replaced right hepatic artery demonstrating the end-to-end anastomosis between the right hepatic artery and the gastroduodenal artery. RHA replaced right hepatic artery, GDA gastroduodenal artery, CHA common hepatic artery, PV portal vein, CBD common bile duct.
Comment
Several options are available for reconstruction of the replaced right hepatic artery after it has been resected with the specimen. Techniques involving venous or prosthetic interposition have been described.5,6 Prosthetic material has the disadvantage of being placed in a field that is not sterile. Vein grafts require harvesting the vessel, often through a second incision. Any interposition graft will require two anastomoses. The gastroduodenal artery transposition technique described above eliminates the need for prosthetic material, provides arterial inflow with a size matched vessel, and requires a single anastomosis, enabling the surgeon to extend the safe limits of pancreatic resection to this unique patient population.
References
Michels NA. Blood supply and anatomy of the upper abdominal organs with a descriptive atlas. Philadelphia: Lippincott, 1955, pp 139–182.
Northover JMA, Terblanche J. A new look at the arterial supply of the bile duct in man and its surgical implications. Br J Surg 1979;66:379–384. doi:10.1002/bjs.1800660603.
Traverso LW, Freeny PC. Pancreaticoduodenectomy: the importance of preserving hepatic blood flow to prevent biliary fistula. Am Surg 1989;55:421–426.
Sarmiento JM, Panneton JM, Nagorney DM. Reconstruction of the hepatic artery using the gastroduodenal artery. Am J Surg 2003;185:386–387. doi:10.1016/S0002-9610(02)01416-2.
Hamazaki K, Mimua H, Kobayashi T. Hepatic artery reconstruction after resection of the hepatoduodenal ligament. Br J Surg 1991;78:1366–1367. doi:10.1002/bjs.1800781131.
Danielson GK, Davis NP, Giffen WO. Successful resection of distal hepatic artery aneurysm with graft reconstruction of the hepatic arteries. Surgery 1968;63:722–726.
Acknowledgements
The illustrations were kindly provided by Hyunch Sung and Kuta Brown. Further support was provided by the I.W. Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Allendorf, J.D., Bellemare, S. Reconstruction of the Replaced Right Hepatic Artery at the Time of Pancreaticoduodenectomy. J Gastrointest Surg 13, 555–557 (2009). https://doi.org/10.1007/s11605-008-0578-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0578-8