Abstract
Purpose
To examine a predictive theoretical model of psychological distress based on the following variables reflected on family caregivers of patients with cancer: the unmet supportive care needs, subjective caregiving burden, social support, and the positive aspects of caregiving.
Methods
A cross-sectional descriptive study was conducted on a sample of 484 dyads of patients and their family caregivers. The caregivers completed structured questionnaires designed to measure psychological distress, unmet supportive care needs, subjective caregiving burden, positive aspects of caregiving, and social support. Patients’ demographic variables and medical data were collected from a medical record review. We used a structural equation modeling to test the predictive theoretical model.
Results
Path analysis results partially supported the proposed model with satisfactory fit indices. Specifically, family caregivers with an increasing number of unmet needs or a heavier caregiving burden were more likely to have more severe psychological distress. Bootstrapping results supported that the caregiving burden and social support were significant mediators. Greater unmet supportive care needs predicted higher psychological distress through increasing caregiving burden. Stronger social support predicted lower psychological distress through decreasing caregiving burden. Positive aspects of caregiving predicted lower caregiving burden through the increasing perceived social support, which in turn eliminated psychological distress.
Conclusions
Unmet supportive care needs could cause psychological distress through increasing caregiving burden. The positive aspects of caregiving reduced caregiving burden through increasing social support, which subsequently alleviated psychological distress. Interventions that aim to satisfy supportive care needs, to reduce caregiving burden, and to strengthen social support ties may boost the mental health of family caregivers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer causes distress to not only patients but also the family caregivers (FCs) who assist with the daily activities, medication, lifestyle management of patients, and provide informational, emotional, or financial support [1]. The demands of caregiving is seemingly casting negative impact on the physical and mental health of FCs [2,3,4,5], and indeed, FCs experienced more distress symptoms and compromise in quality of life as compared to patients [6, 7]. Studies showed that FCs revealed greater distress than population norms with 38% FCs exceeding the threshold for clinical depression [8]. Another study reported that the prevalence of clinical depression among FCs reached 63.5% [9]. FCs’ psychological distress may negatively influence their own health [10] and undermine the quality of care provided [11]. Importantly, high level of psychological distress may also result in increased distress in the care recipients [12], which eventually leads to decreased quality of life of patients.
Given the high prevalence and negative impacts of psychological distress among FCs, it is important to investigate the predictive factors which can potentially facilitate the development of effective interventions to prevent or alleviate distress among FCs of patients with cancer.
Theoretical framework and empirical background
Pearlin’s stress process model has been verified in FCs to understand the process of emotional adjustment [13]. Although it was developed for dementia care, the sociological concepts of stress and stress-coping factors that the model is based on are applicable to other disease contexts like cancer [13,14,15,16,17]. Caregiver stress is deemed a consequence of a process involving several dimensions in the model, including the sociodemographic background and resources of caregivers, the primary and secondary stressors to which they are exposed [13]. Primary stressors are demands and hardships anchored directly in caregiving, which include objective (daily dependency of patients) and subjective (hardships subjectively experienced by caregivers) aspects. Secondary stressors derived from primary stressors, comprise of two categories: role strains (e.g., job-caregiving conflict, financial strains), and intrapsychic strains, involving the global (e.g., diminishment of self-concepts) and situational (e.g., personal gain or enrichment) aspects. The mechanism of the stress process model which explains the links between primary stressors, secondary stressors, and outcomes is proliferation. As the primary stressors rise, the related stress proliferates to other aspects of caregiver’s life (secondary stressor). Consequently, the overwhelming nature of caregiving is expected to negatively affect FCs’ psychological or physical well-being. The stress process model also presents psychosocial resources that mediate the effects of the primary and secondary stressors on negative outcomes. These psychosocial resources include social support and coping.
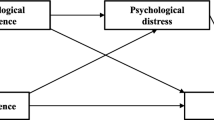
Caregiving activities can cause significant unmet supportive care needs across various domains including comprehensive cancer care, information, daily activities, healthcare service, and so on [18]. According to the stress process model [13], the stressors that directly stem from the illness and caregiving are primary stressors, and thus, the fact that FCs’ unmet needs (primary stressors) increase may give rise to negative reaction to caregiving (secondary stressors) and diminished positive aspects of caregiving (secondary stressors). The negative effects of the stressors are supported by various studies. To illustrate this, higher levels of unmet needs and subjective caregiving burden were found to act as predictors of poorer psychological well-being in FCs of patients with cancer [19,20,21,22,23]. A critical review also summarized and appraised the positive aspects of spousal caregiving for patients with cancer, and concluded that the positive aspects of caregiving was found to have an impact on the overall well-being of caregivers [24], whereas the association between the positive aspects of caregiving and outcomes was not identified in the stress process model [13]. Based on the model and literature review, it was hypothesized that the unmet needs might first predict caregiving burden and diminished positive aspects of caregiving, which might in turn lead to increased psychological distress (see Fig. 1).
Grounded in the mediating effect of social support in the model, social support may serve to prevent stressors from causing psychological distress and to inhibit the development of secondary stressors [13]. Social support has been documented to have significant effects on caregiving burden, anxiety, and depressive distress for FCs of patients with cancer [25,26,27,28]. Similarly, FCs with more unmet needs and sensing fewer positive aspects of caregiving were more likely to experience lower social support [22, 29, 30]. These results indicate that social support may be enhanced by positive feelings, and caregivers with stronger social support are more likely to weather care demands. As a result of caregivers being more capable of taking the care demands, negative reactions to caregiving can be inhibited, and thus, FCs experience less psychological impairment (see Fig. 1).
Despite of the large number of studies that testified the associations among the unmet supportive care needs, subjective caregiving burden, social support, positive aspects of caregiving, and psychological distress, only a few studies explored the underlying theoretical model that may explain the factors that predicts or mediates the degree of psychological distress among FCs of patients with cancer. The aim of the study was to test the predictive theoretical model of psychological distress based on unmet supportive care needs, subjective caregiving burden, social support, and positive aspects of caregiving in FCs of patients with cancer (Fig. 1).
Methods
Design and participants
This was a cross-sectional, descriptive study. Participants were recruited from five departments of three tertiary hospitals affiliated with a medical university in Anhui Province, China, by convenience sampling. Inclusion criteria for patients were (1) diagnosed with cancer by an oncologist and (2) cared for in a home setting instead of institutionalized. Inclusion criteria for FCs were (1) primarily responsible for providing direct care, (2) 18 years old and above, and (3) able to read, speak, and understand mandarin.
Data collection
Data were collected using structured self-report questionnaires. Trained researchers worked as interns in relevant departments. All eligible participants were identified and referred by oncologists or primary nurses. Whether the patients are aware of their diagnosis of cancer is figured out under ethical consideration. The FCs were interviewed face to face by researchers using standardized instructions, and the items in the questionnaire were explained to them when necessary. The interviews were conducted in a quiet ward or the head nurse’s office for the convenience of caregivers. A total of 515 potential participants were approached. Five hundred seven eligible FCs enrolled in the study. Twenty-three questionnaires with missing items greater than 50% due to the interruption of the interview were excluded. The remaining 484 FCs were included in the final analysis.
Measures
The 10-item Kessler Psychological Distress Scale
FCs’ psychological distress was evaluated using the Kessler 10, a screening instrument developed to identify clinically significant distress in population surveys [31]. FCs were asked how often they felt anxiety and depression during the past 4 weeks, answering on a five-point scale (1 = none of the time to 5 = all of the time). The total score ranges from 10 to 50, with higher scores indicating greater distress. The designated cutoff scores for a low level of distress range from 10 to 15, 16 to 21 for moderate, 22 to 29 for high, and 30 to 50 for very high. The Cronbach’s alpha of the scale in the study was 0.92.
The Chinese version of Supportive Care Needs Survey-Partners and Caregivers
The unmet supportive care needs of FCs were estimated by the Chinese version of SCNS-P&C [32]. The 45-item Chinese version of SCNS-P&C evaluates the content and level of caregivers’ supportive care needs during caregiving last month [32], including four domains: communication/interpersonal; healthcare service/information; social security/work; and psychological and emotional aspect. Participants were asked to indicate how much help they needed with each item (e.g., “support from family”) on a 5-point Likert scale (1 = no need, not applicable; 2 = need satisfied; 3 = low need; 4 = moderate need; 5 = high need). The scores of total scale and each domain were calculated, with higher scores suggesting higher level of unmet supportive care needs. The Cronbach’s alphas of the total scale and sub-dimensions range from 0.79 to 0.94 in the study.
Caregiver Reaction Assessment
The 24-item CRA is a valid and reliable tool to measure multidimensional experience of FCs [33]. This scale includes five domains considering both positive and negative aspects of caregiving reactions: self-esteem, lack of family support, impact on finances, impact on schedule, and impact on health. Participants rated their score from 1 (strongly disagree) to 5 (strongly agree) and the total score for each domain is calculated, with higher score reflecting higher caregiving burden except for the self-esteem domain. The four negative domains were used to assess the subjective caregiving burden in the study. The Cronbach’s alphas of the total scale and sub-dimensions in this study ranged from 0.64 to 0.72.
Positive Aspects of Caregiving
We used the PAC [34] to estimate FCs’ perception of benefits within the caregiving context. The PAC consists of 9 items covering 2 dimensions: self-affirmation and outlook on life. Each item is ranked on a 5-point scale from 1 (strongly disagree) to 5 (strongly agree). The total score ranges from 9 to 45, with a higher score suggesting more positive caregiving appraisals. The Cronbach’s alphas of the total scale and each sub-dimension in this study ranged from 0.81 to 0.87.
Perceived Social Support Scale
The PSSS [35] was used for evaluating FCs’ perception of social support from family, friends, and significant others. It includes 12 items with each item answered on a 7-point Likert-type scale from 1 (strongly disagree) to 7 (strongly agree), with higher scores representing the higher degree of support perceived by the individual. The Cronbach’s alphas for the total scale and sub-dimensions ranged from 0.83 to 0.90 in this study.
Demographic and care characteristics of FCs
The self-reported demographic data for FCs included gender, age, marital status, occupation, and religion, etc. Caregiving variables included relationship to the patient.
Demographic and clinical characteristics of patients
After explaining the study to patients who met the inclusion criteria and obtaining their approval, they were queried to nominate a primary family caregiver. Their demographic variables and medical data were collected using retrospective medical record. The former included age, gender, medical insurance, and the later included the type of cancer, time since diagnosis, complications, etc.
Data analysis
SPSS, version 23.0, was used for descriptive analysis. Independent sample t tests or one-way ANOVA examined the differences in psychological distress among different demographic and clinical characteristics. Pearson correlations were performed for major continuous variables.
The hypothesized theoretical paths among unmet supportive care needs, caregiving burden, social support, positive aspects of caregiving, and psychological distress were tested using structured equation modeling (SEM) using Mplus, version 8.3. The overall goodness of fit of the model with the data was examined using the following fit indices: Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), root-mean-square error of approximation (RMSEA), the standardized root-mean-square residual (SRMR), and the ratio of χ2 to the degree of freedom (df) of the model [36].
The significance of statistical estimates for indirect effects in predicting psychological distress was identified using bootstrap procedure [37]. From the primary data set (N = 484), a total of 5000 bootstrap samples were selected through random sampling with replacement. The parametric estimate of the total and the specific indirect effects of 95% bias-corrected bootstrap confidence intervals (CI) was generated using the bootstrap samples to test the mediation effect [38]. If the 95% bias-corrected bootstrap CI of the parameter estimate does not include zero, the indirect effect is considered statistically significant at the 0.05 level [38].
Results
FCs’ and patients’ characteristics
The mean age of FCs was 42.73 (SD = 13.78, range = 18–81) years old. The majority of FCs were male (50.83%), married (86.78%), and unemployed (67.36%) and obtained a junior or senior high school degree (53.72%); 86.36% of FCs held no religious beliefs; 49.59% were adult child and 42.56% lived in countryside; 44.42% had an average monthly income of 1000–2999 RMB (152–456 USD); the majority reported a good health status (64.46%).
The mean age of the patients was 57.07 (SD =13.36, range = 20–91) years old. Approximately 48.55% of the patients were men; 94.63% had health insurance or free medical care. The average time since diagnosis was 3.97 (IQR, 9.71) months. The majority of the patients had mainly self-care ability (70.45%), with no cancer metastasis (50.83%) and were receiving chemotherapy (64.67%). Nearly one-third were diagnosed with digestive system cancer.
Tables 1 and 2 summarize the sample characteristics and psychological distress of FCs. The longer the time from diagnosis, the more psychological distress the FCs would have (P < 0.05). The following groups of FCs had more psychological distress: caregivers who had a religion (P < 0.05) reported poor overall health status (P < 0.001) and lower monthly average income (P < 0.01); FCs of patients who had cancer metastasis (P < 0.01) and were unable to self-care (P < 0.05) had more psychological distress.
Description of variables
The mean score of Kessler-10 scale was 20.18 (SD = 7.41, range = 10–48). Most FCs revealed low (N = 152, 31.4%) and medium (N = 150, 31.0%) psychological distress, 26.65% and 10.95% of FCs revealed high and very high psychological distress respectively. In the domains of unmet needs, the highest score was observed in the healthcare service/information needs domain (mean = 40.72, SD = 12.42), followed by social security/work needs (mean = 21.17, SD = 7.37). The details of the scores of variables are presented in the online supplementary information (Supplementary Table 1).
The correlations among the five variables included in the model are presented in Table 3.
Measurement model
The measurement model exhibited reasonable fit to the data (χ2 [220] = 717.204; CFI = 0.898; TLI = 0.882; RMSEA = 0.068; 90% CI = 0.063, 0.074). All individual factor loadings were significant (P < 0.001). The factor loadings of Kessler 10’s measured variables ranged from 0.575 to 0.803 for each item. Specifically, factor loadings for social support ranged from 0.723 to 0.811, 0.772 to 0.791 for positive aspects of caregiving, 0.461 to 0.706 for caregiving burden, and 0.701 to 0.841 for unmet needs. All variances and residual variances were positive and significant, indicated that the model was correct, structurally specified, and can be further analyzed [39].
Structural model fits
The fit indices generated for the hypothesized model indicated a reasonable fit of the model to the data (χ2/df = 3.23; CFI = 0.898; TLI = 0.883; RMSEA = 0.068; SRMR = 0.055). The hypotheses were tested by examining the significance of the path coefficients, as shown in Fig. 2. The significant paths were partially consistent with the hypothesized model. An increase in the amount of unmet needs (β = 0.274, P < 0.001) and caregiving burden (β = 0.461, P < 0.001) predicted a higher level of psychological distress; higher levels of unmet needs (β = 0.267, P < 0.001) and a decrease in perceived social support (β = − 0.323, P < 0.001) predicted higher caregiving burden. However, there was no significant relationship between perceived social support and psychological distress. Positive aspects of caregiving predicted perceived social support (β = 0.537, P < 0.001) but not psychological distress. There was no significant direct effect of unmet needs on positive aspects of caregiving and perceived social support.
Final model for the path relationship between unmet supportive care needs, subjective caregiving burden, perceived social support, positive aspects of caregiving, and psychological distress. Note. The arrow indicates significant direct effects; the dashed arrow indicates non-significant direct effects; values are standardized coefficients for paths with statistical significance. ***P < 0.001
Indirect effects
Table 4 shows the statistical significance of the indirect effects of unmet needs and positive aspects of caregiving on psychological distress. Caregiving burden and social support were significant mediators. A higher level of unmet needs predicted more psychological distress, and it was mediated by caregiving burden (B = 0.105; 95%CI = 0.053, 0.183). Stronger social support predicted less psychological distress through decreasing caregiving burden (B = − 0.105; 95%CI = −0.180, −0.052). Positive aspects of caregiving predicted lower subjective caregiving burden through social support (B = −0.136; 95%CI = −0.218, −0.066). Although social support and caregiving burden each alone was not a significant mediator to the relationship between positive aspects of caregiving and psychological distress, the indirect effects of positive aspects of caregiving on psychological distress through the chain of social support and caregiving burden were significant (B = −0.067; 95%CI = −0.124, −0.032) (Table 4).
Discussion
While most FCs exhibited a low or medium level of psychological distress, almost half of them suffered from mental health problems. Studies have indicated that FCs of patients with cancer experienced greater psychological distress than general population [8, 40]. Chinese FCs assume the primary, more and more responsibilities in caring for the patients with cancer either in hospital or at home throughout the whole journey of the illness [14, 41]. The results of univariate analysis also indicated that the patients’ cancer metastasis, poor self-care ability, caregivers’ poor overall health status, and lower income are some factors contributing to FCs’ psychological distress. According to Pearlin’s stress process model, these factors are primary or secondary stressors to which FCs are exposed [13]. These all stressors make FCs more vulnerable to psychological distress. This result supports Pearlin’s theory, highlights the importance to recognize the early psychological distress, and implements target interventions to improve FCs’ mental health.
This study attempts to examine the relationships among unmet supportive care needs, caregiving burden, social support, positive aspects of caregiving, and psychological distress experienced by FCs of patients with cancer using SEM technique. The results supported the hypothesized indirect effects of the subjective caregiving burden on the relationships between the unmet needs and the extent of psychological distress (Fig. 2). The findings also supported that FCs with stronger social support would inhibit caregiving burden and thus experience lower psychological distress. Besides, social support functions as a mediator of the relationship between positive aspects of caregiving and caregiving burden. Though the results did not support the hypothesized mediation effects of social support alone on the relationship between positive aspects of caregiving and psychological distress, social support and caregiving burden together mediated the relationship between positive aspects of caregiving and psychological distress.
Differences in responses to caregiving have been proposed within a stress process paradigm [13, 15, 16]. Our results have added the body of knowledge in the cancer caregiving literature that subjective caregiving burden aggravates the deleterious effects of unmet needs, positive aspects of caregiving and social support ameliorates the deleterious effects of subjective caregiving burden on caregiver psychological distress.
Specifically, the unmet needs significantly predicted the level of psychological distress both directly and indirectly. Among all the reported unmet needs, healthcare service/information needs were most commonly nominated. This finding is consistent with previous studies [3]. Additionally, the extent to which unmet needs affect psychological distress is mediated by the subjective caregiving burden. Consistent with stress process model [13], once FCs’ unmet needs were not satisfied or increased, they may generate a negative reaction to caregiving, and, consequently, cause subjective caregiving burden, which in turn was associated with increased psychological distress. Empirically, unmet needs were found to predict increased subjective caregiving burden and psychological distress [20,21,22,23]. This means nursing practitioners have a new potential target to minimize psychological distress by mobilizing interventions that reduce both unmet needs and its consequent subjective caregiving burden.
Additionally, we found that social support can have significant and negative indirect effect on psychological distress through decreasing subjective caregiving burden. This corroborates the theory of the stress process model predicting that social support may inhibit the development of subjective caregiving burden, despite of the results that there is not a direct statistically significant relationship between psychological distress and social support. The effect of social support on the health outcomes of FCs has been documented in the literature as social support serves as an important resource in times of distress [25,26,27,28]. This finding added the empirical evidence that the perceived social support has an indirect benefit to psychological well-being through reducing caregiving burden. Therefore, it is important to enhance the perceived social support of FCs to decrease their negative caregiving reaction which will improve their mental health. The path between social support and unmet needs was not significant. This is inconsistent with the results of Lambert et al. suggesting that higher social support is associated with lower unmet needs [22]. This may imply that the perceived social support has limited effects in satisfying FCs’ supportive care needs, and therefore, developing a specific, targeted supportive care project to satisfy FCs’ unmet needs is more significant [42]. Healthcare personnel could also provide the information and guide them to use available social and public health services, such as “China Cancer Care Conference,” “hospice,” and “serious disease pension.”
Furthermore, we tested a mediation model explaining the relation between positive aspects of caregiving and subjective caregiving burden. Although positive aspects of caregiving did not exhibit significant direct association with subjective caregiving burden, positive aspects of caregiving could reduce caregiving burden through increasing social support, and this indirect effect contributes to the extant literature that relies on regression models to examine the direct association between positive aspects of caregiving and subjective caregiving burden [43]. Positive aspects of caregiving and perceived social support may be important factors to intervene upon to reduce caregiving burden.
Besides, in the pathway between positive aspects of caregiving toward psychological distress, although perceived social support alone was not a significant mediator, the distal mediation effect through perceived social support and subjective caregiving burden was statistically significant. FCs with high positive aspects of caregiving tend to have lower psychological distress because they perceived more social support and less subjective caregiving burden. These results emphasize the important roles of social support and caregiving burden. Studies indicated that FCs with more caregiving self-efficacy, skill mastery, and problem-focused coping had lower caregiving distress [44]. Therefore, it is essential for nurse practitioners to work out supportive care programs that emphasize meanings and deliver practical behavioral skills such as time management and scheduling, balancing work with caregiving activities, coping with financial challenges, obtaining support from one’s family members or other support systems that may be effective in reducing FCs’ psychological distress.
Finally, the other noteworthy result is that FCs who have a religious belief were more distressed than the counterpart. A focus on patient care may result in significant disturbance on FCs’ time [1]. FCs often prioritize patients’ needs and give up their own activities [1,2,3]. Therefore, FCs with a religious belief may experience an imbalance between the pursuit of religious belief and family function [1,2,3]. For example, they do not have time to pray or attend some religious activities, thereby impose psychological distress on them. Also, in mainland China, most hospitals do not attach importance to one’s religious need, let alone provide the spiritual care or the place for them to take religious activities [45]. Consequently, they may perceive some kind of debt to their religious belief and aggravate their psychological distress.
Limitations
Several limitations are presented in this study. Although analyses were based on theoretical models of stress-coping among FCs, cross-sectional analyses preclude causal inferences. Convenience sampling was used in this study, which may compromise the generalizability of findings. The sample was made up of FCs who agreed to participate, their willingness to participate may indicate important distinctions from other FCs. Our study sample was heterogeneous in terms of cancer diagnosis, duration of disease, treatment, and comorbidity. Further research should investigate the association among the variables in more homogeneous study samples.
Conclusion
Chinese FCs experienced high levels of psychological distress aggravated by considerable unmet supportive care needs and subjective caregiving burden directly. Furthermore, unmet needs predicted psychological distress through subjective caregiving burden, positive aspects of caregiving reduced caregiving burden through increasing social support, which subsequently alleviated psychological distress. Indeed, the structural equation model partially supported and developed the theoretical framework. Interventions aiming to satisfy FCs’ needs, reduce caregiving burden, emphasize on meaning finding, and strengthen social support ties may facilitate improvement in mental health.
Data availability
Data may be made available on reasonable request to the corresponding author.
References
Williams AL, Bakitas M (2012) Cancer: a new direction for interventions. J Palliat Med 15:775–783. https://doi.org/10.1089/jpm.2012.0046
Sherman DW, McGuire DB, Free D, Cheon JY (2014) A pilot study of the experience of family caregivers of patients with advanced pancreatic cancer using a mixed methods approach. J Pain Symptom Manag 48:385–399. https://doi.org/10.1016/j.jpainsymman
Shaw J, Harrison J, Young J, Butow P, Sandroussi C, Martin D, Solomon M (2013) Coping with newly diagnosed upper gastrointestinal cancer: a longitudinal qualitative study of family caregivers’ role perception and supportive care needs. Support Care Cancer 21:749–756. https://doi.org/10.1007/s00520-012-1575-8
Ji J, Zoller B, Sundquist K, Sundquist J (2012) Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. Circulation 125:1742–1747. https://doi.org/10.1161/CIRCULATIONAHA.111.057018
Oberoi DV, White V, Jefford M, Giles GG, Bolton D, Davis I, Winship I, Prince HM, Millar J, Harrison S, Kay A, Hill D (2016) Caregivers’ information needs and their ‘experiences of care’ during treatment are associated with elevated anxiety and depression: a cross-sectional study of the caregivers of renal cancer survivors. Support Care Cancer 24:4177–4186. https://doi.org/10.1007/s00520-016-3245-8
Sklenarova H, Krumpelmann A, Haun MW, Friederich HC, Huber J, Thomas M, Winkler EC, Herzog W, Hartmann M (2015) When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer 121:1513–1519. https://doi.org/10.1002/cncr.29223
Renovanz M, Maurer D, Lahr H, Weimann E, Deininger M, Wirtz CR, Ringel F, Singer S, Coburger J (2018) Supportive care needs in glioma patients and their caregivers in clinical practice: results of a multicenter cross-sectional study. Front Neurol 9:763. https://doi.org/10.3389/fneur.2018.00763
Kessler ER, Moss A, Eckhardt SG, Laudenslager ML, Kilbourn K, Mauss IB, Bowles DW, Hecker S, Fairclough DL, Kutner JS (2014) Distress among caregivers of phase I trial participants: a cross-sectional study. Support Care Cancer 22:3331–3340. https://doi.org/10.1007/s00520-014-2380-3
Yang X, Wang L, He J, Ge C, Chang Y, Fu J, Wei J, Pattaramongkolar E, Zhou Y (2012) Factors related to depressive symptoms among Chinese caregivers of cancer patients. Psychooncology 21:1063–1070. https://doi.org/10.1002/pon.1999
Yeh PM, Wierenga ME, Yuan SC (2009) Influences of psychological well-being, quality of caregiver-patient relationship, and family support on the health of family caregivers for cancer patients in Taiwan. Asian Nurs Res (Korean Soc Nurs Sci) 3:154–166. https://doi.org/10.1016/S1976-1317(09)60027-X
Chang YJ, Kwon YC, Lee WJ, Do YR, Seok LK, Kim HT, Park SR, Hong YS, Chung IJ, Yun YH (2013) Burdens, needs and satisfaction of terminal cancer patients and their caregivers. Asian Pac J Cancer Prev 14:209–216. https://doi.org/10.7314/apjcp.2013.14.1.209
Jacobs JM, Shaffer KM, Nipp RD, Fishbein JN, MacDonald J, El-Jawahri A, Pirl WF, Jackson VA, Park ER, Temel JS, Greer JA (2017) Distress is interdependent in patients and caregivers with newly diagnosed incurable cancers. Ann Behav Med 51:519–531. https://doi.org/10.1007/s12160-017-9875-3
Pearlin LI, Mullan JT, Semple SJ, Skaff MM (1990) Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 30:583–594. https://doi.org/10.1093/geront/30.5.583
Lazarus RS, Folkman S (1984) Stress, appraisal, and coping. Springer Publishing Company, New York
Nijboer C, Tempelaar R, Triemstra M, van den Bos GA, Sanderman R (2001) The role of social and psychologic resources in caregiving of cancer patients. Cancer 91:1029–1039. https://doi.org/10.1177/1524839918764667
Pitceathly C, Maguire P (2003) The psychological impact of cancer on patients’ partners and other key relatives: a review. Eur J Cancer 39:1517–1524. https://doi.org/10.1016/s0959-8049(03)00309-5
Tang ST, Cheng CC, Lee KC, Chen CH, Liu LN (2013) Mediating effects of sense of coherence on family caregivers’ depressive distress while caring for terminally ill cancer patients. Cancer Nurs 36:E25–E33. https://doi.org/10.1097/NCC.0b013e31826fc90d
Wang T, Molassiotis A, Chung BPM, Tan JY (2018) Unmet care needs of advanced cancer patients and their informal caregivers: a systematic review. BMC Palliat Care 17:96. https://doi.org/10.1186/s12904-018-0346-9
Tang ST, Chang WC, Chen JS, Wang HM, Shen WC, Li CY, Liao YC (2013) Course and predictors of depressive symptoms among family caregivers of terminally ill cancer patients until their death. Psychooncology 22:1312–1318. https://doi.org/10.1002/pon.3141
Armoogum J, Richardson A, Armes J (2012) A survey of the supportive care needs of informal caregivers of adult bone marrow transplant patients. Support Care Cancer 21:977–986. https://doi.org/10.1007/s00520-012-1615-4
Janda M, Steginga S, Dunn J et al (2008) Unmet supportive care needs and interest in services among patients with a brain tumour and their carers. Patient Educ Couns 71:251–258. https://doi.org/10.1016/j.pec.2008.01.020
Lambert SD, Harrison JD, Smith E, Bonevski B, Carey M, Lawsin C, Paul C, Girgis A (2012) The unmet needs of partners and caregivers of adults diagnosed with cancer: a systematic review. BMJ Support Palliat Care 2:224–230. https://doi.org/10.1136/bmjspcare-2012-000226
Zavagli V, Raccichini M, Ercolani G, Franchini L, Varani S, Pannuti R (2019) Care for carers: an investigation on family caregivers’ needs, tasks, and experiences. Transl Med UniSa 19:54–59
Li Q, Loke AY (2013) The positive aspects of caregiving for cancer patients: a critical review of the literature and directions for future research. Psychooncology 22:2399–2407. https://doi.org/10.1002/pon.3311
Arab M, Bernstein C, Haghshenas A, Ranjbar H (2019) Factors associated with caregiving burden for mothers of children undergoing Acute Lymphocytic Leukemia (ALL) treatment. Palliat Support Care 15:1–8. https://doi.org/10.1017/S1478951519000853
Chen X, Lou F (2020) The relationships among insecure attachment, social support and psychological experiences in family caregivers of cancer inpatients. Eur J Oncol Nurs 44:101691. https://doi.org/10.1016/j.ejon.2019.101691
Garcia-Torres F, Jacek Jabłoński M, Gómez Solís Á, Moriana JA, Jaén-Moreno MJ, Moreno-Díaz MJ, Aranda E (2020) Social support as predictor of anxiety and depression in cancer caregivers six months after cancer diagnosis: A longitudinal study. J Clin Nurs 29:996–1002. https://doi.org/10.1111/jocn.15123
Hu X, Peng X, Su Y, Huang W (2018) Caregiving burden among Chinese family caregivers of patients with lung cancer: a cross-sectional survey. Eur J Oncol Nurs 37:74–80. https://doi.org/10.1016/j.ejon.2018.11.003
Lichtenthal WG, Breitbart W (2015) The central role of meaning in adjustment to the loss of a child to cancer: implications for the development of meaning-centered grief therapy. Curr Opin Support Palliat Care 9:46–51. https://doi.org/10.1097/SPC.0000000000000117
Newberry A, Kuo J, Donovan H, Given B, Given CW, Schulz R, Sherwood P (2012) Identifying family members who are likely to perceive benefits from providing care to a person with a primary malignant brain tumor. Oncol Nurs Forum 39:E226–E232. https://doi.org/10.1188/12.ONF.E226-E232
Kessler R, Mroczek D (1994) Final versions of our non-specific psychological distress scale [written communication-memo dated 10/3/94]. Ann Arbor: Ann Arbor Mi. Survey Research Center of the Institute for Social Research, University of Michigan, Michigan. [Google Scholar]
Liu JJ, Liu QH, He HY, Zhang T, Song YX, Wang W, Hong JF (2020) Psychometric testing of the Chinese version of supportive care needs survey for partners and caregivers of cancer patients. J Cancer Educ 35:76–85. https://doi.org/10.1007/s13187-018-1442-5
Given CW, Given B, Stommel M, Collins C, King S, Franklin S (1992) The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health 15:271–283. https://doi.org/10.1002/nur.4770150406
Tarlow BJ (2004) Positive aspects of caregiving: contributions of the reach project to the development of new measures for Alzheimer’s caregiving. Res Aging 26:429–453. https://doi.org/10.1186/1471-2202-13-14
Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA (1990) Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess 55:610–617. https://doi.org/10.1080/00223891.1990.9674095
Iacobucci D (2010) Structural equations modeling: fit indices, sample size, and advanced topics. J Consum Psychol 20:90–98. https://doi.org/10.1016/j.jcps.2009.09.003
MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V (2002) A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 7:83–104. https://doi.org/10.1037/1082-989x.7.1.83
Mallinckrodt B, Abraham W, Wei M, Russell D (2006) Advances in testing the statistical significance of mediation effects. J Couns Psychol 53:372–378
Kolenikov S, Bollen KA (2008) Testing negative error variances: is a Heywood case a symptom of misspecification? Sociol Methods Res 41:124–167. https://doi.org/10.1177/0049124112442138
Goren A, Gilloteau I, Lees M, DaCosta Dibonaventura M (2014) Quantifying the burden of informal caregiving for patients with cancer in Europe. Support Care Cancer 22:1637–1646. https://doi.org/10.1007/s00520-014-2122-6
Ang WH, Lang SP, Ang E, Lopez V (2016) Transition journey from hospital to home in patients with cancer and their caregivers: a qualitative study. Support Care Cancer 24:4319–4326. https://doi.org/10.1007/s00520-016-3269-0
Primeau C, Paterson C, Nabi G (2017) A qualitative study exploring models of supportive care in men and their partners/caregivers affected by metastatic prostate cancer. Oncol Nurs Forum 44:E241–E249. https://doi.org/10.1188/17.ONF.E241-E249
Palacio C, Krikorian A, Limonero JT (2018) The influence of psychological factors on the burden of caregivers of patients with advanced cancer: resiliency and caregiver burden. Palliat Support Care 16:269–277. https://doi.org/10.1017/S1478951517000268
Harmell AL, Chattillion EA, Roepke SK, Mausbach BT (2011) A review of the psychobiology of dementia caregiving: a focus on resilience factors. Curr Psychiatry Rep 13:219–224. https://doi.org/10.1007/s11920-011-0187-1
Cheng Q, Xu X, Liu X, Mao T, Chen Y (2018) Spiritual needs and their associated factors among cancer patients in China: a cross-sectional study. Support Care Cancer 26:3405–3412. https://doi.org/10.1007/s00520-018-4119-z
Code availability
N/A.
Funding
The authors received financial grants from the National Natural Science Foundation of China (81573017; 81101750).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection and analysis were performed by Xiao-qing Lv, Jing-jing Liu, Yuan Feng, Shu-wen Li, and Huan Qiu. The first draft of the manuscript was written by Xiao-qing Lv, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate and publish
Informed consent to participate and publish was obtained for all participants in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Table 1
(DOCX 16 kb).
Rights and permissions
About this article
Cite this article
Lv, Xq., Liu, Jj., Feng, Y. et al. Predictive model of psychological distress in family caregivers of patients with cancer: a cross-sectional study. Support Care Cancer 29, 5091–5101 (2021). https://doi.org/10.1007/s00520-021-06022-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06022-1