Abstract
Purpose
Studies examining longitudinal associations between socioeconomic factors and quality of life (QoL) in cancer patients are rare. This study investigates changes in QoL over a 6-month period.
Methods
Four hundred forty-two cancer patients (mean age 64, SD = 11, 70% male) completed standardized questionnaires at the beginning (t1) and end (t2) of their hospital stay and 3 (t3) and 6 months (t4) thereafter. QoL was assessed with the EORTC QLQ-C30 core questionnaire. Mixed effect models were employed to analyze individual changes in QoL in relation to socioeconomic status (education, income, job status) over the four timepoints. Age, sex, cohabitation, disease and treatment factors, and comorbidity were included as covariates in the models.
Results
Income was a predictive factor for QoL. Patients with a low income had 8.8 percentage points (PP) lower physical, 4.9 PP lower emotional, and 11.4 PP lower role functioning. They also had 6.6 PP lower global QoL. Lower social functioning (6.2 PP) was found in patients with higher education or university degrees compared with those who were less educated or had not undergone an apprenticeship. Income also influenced trajectories of role functioning. There was no evidence that primary or secondary education and job type were related to QoL.
Conclusions
The fact that income is negatively associated with many aspects of quality of life should be considered during and after treatment with a focus on patients with special needs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Social inequalities in health and disease risk have been found in several countries and for various indicators such as income, education, and occupational status [1]. In recent years, social inequalities have received increased attention in the field of cancer research. There is evidence that socioeconomic status (SES) is associated with morbidity or mortality, cancer survival, and disease stage at diagnosis to the disadvantage of patients with low SES across all tumor sites [2,3,4,5,6]. Results for cancer incidence are inconclusive so far. In most of the studies, low SES was associated with an increased risk for lung, colorectal, and cervical cancer [7, 8]. Incidence of breast and prostate cancer was increased in people with high SES [9]. However, total cancer incidence is higher in people with low SES [10].
Despite these social inequalities in cancer incidence and mortality, the number of people who are living with the disease for five or more years is constantly rising [11]. This is due to new treatment methods, early detection through cancer screening programs, and better access to clinical care. Consequently, one of the main goals in providing treatment is to improve patients’ quality of life (QoL). Whereas much is known about the association of socioeconomic disadvantages and their impact on well-being and QoL for other chronic diseases [12, 13], the relationship in cancer patients remains unclear.
In contrast, the association between SES and cancer survival has been well investigated so far. Stage at diagnosis and differences in treatment are two variables in particular that have received more in-depth attention [3]. Differences were observed in most countries and all genders, and results were consistent regardless of which SES indicator was used [14, 15]. Because QoL is an independent predictive factor for overall survival [16, 17], the association between SES and QoL should be addressed while interpreting social inequalities in cancer survival, even in patients with advanced stages of the disease [18]. Whereas a lot of evidence exists concerning QoL in cancer patients in general, very few studies have examined associations with socioeconomic factors. There is some evidence indicating that lower SES is associated with decreased QoL in cancer survivors [19]. Reduced QoL was also found in low-income prostate cancer patients over a 1-year period [20]. In another study, low SES was negatively related to QoL immediately after diagnosis but not at follow-up [21]. Penson et al. also reported worse QoL for cancer patients with lower household incomes in the first 6 months following diagnosis but not in subsequent follow-ups [22]. However, SES differences are smaller in studies which focus on area-based measures as indicators for inequalities [3]. In cases where individual SES information was available, most studies focused on one factor (e.g., income), and different indicators were seldom considered at the same time. Because of this lack of longitudinal research on different indicators of socioeconomic status and cancer outcomes [23], the present study investigates the effect of income, education, and job hierarchy on QoL in patients with different types of cancer over the course of the first 6 months after hospital release.
Methods
Design and data collection
The present study surveyed patients who were admitted to the Leipzig University Hospital between October 2012 and June 2014 for the treatment of cancer. Exclusion criteria were no histologically confirmed malignancy, no written informed consent, aged < 18 years, poor understanding of German, dementia, or cognitive restrictions. Shortly after admission, eligible patients were contacted by study nurses who informed them about the procedure and aim of the study. After they had provided written informed consent, patients were interviewed upon hospitalization (t1), at hospital discharge (t2), 3 months after baseline (t3), and 6 months after baseline (t4). Data collection was performed with the help of tablet computers at t1 and t2. At t3 and t4, participants were contacted and interviewed via telephone. The study received ethical approval by the Institutional Review Board of Leipzig University (#210-12-02072012).
Instruments
Education was categorized by (a) the highest level of primary or secondary education completed (compulsory education, post-compulsory education, higher secondary school) and (b) higher education completed (none, apprenticeship, higher, university). Both variables were further dichotomized into compulsory and post-compulsory for lower school education versus higher secondary school (high school education). Participants who had no degrees or professional training (i.e., completed apprenticeship) were classified as having a low level of education, and those who did were classified as having a higher level of education.
To ascertain the income of the individual patients, the net household income (total income minus taxes) was weighted with the number of persons living in the household and their age according to OECD (Organization for Economic Co-operation and Development) standards to obtain the equivalence income. Patients who earned 1000 euros per person per month or above were classified as having a high income. Those who earned less than that were classified as having a low income.
Job hierarchy pertains to patient’s position within certain job categories. Participants were asked to report their job category (e.g., worker) and their job grade (e.g., skilled or unskilled) and were accordingly assigned to the corresponding category. Middle and low positions were classified as low and others as high job status.
Quality of life was measured at baseline and all follow-ups using the European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire (EORTC QLQ-C30). This is a validated self-report questionnaire for use in cancer clinical studies [24]. In total, the EORTC captures five subscales, global quality of life, and various symptoms. For the present study, we used all of the functional scales of the EORTC QLQ-C30: physical functioning (five items, Cronbach’s alpha at t1 = 0.85, t2 = 0.85, t3 = 0.85, t4 = 0.86), emotional functioning (four items, 0.73, 0.73, 0.75, 0.81), role functioning (two items, 0.90, 0.85, 0.88, 0.93), social functioning (two items, 0.71, 0.72, 0.80, 0.71), cognitive functioning (two items, 0.72, 0.69, 0.73, 0.65), and global quality of life (two items, 0.89, 0.84, 0.90, 0.94). Participants responded using a four-point Likert scale ranging from 0 (“not at all”) to 3 (“very much”), with the exception of global quality of life for which the range was 1 (“very poor”) to 7 (“excellent”). The measures are scaled from 0 to 100, whereby higher scores in the selected scales indicate better QoL [25].
Clinical data including method of therapy (chemotherapy, radiotherapy, surgery), tumor stage, and type of cancer (advanced, not advanced) was assessed from the medical reports. If cancer was recurrent, metastatic, or secondary, patients were classified as having advanced cancer. Tumor stage was classified according to the Union for International Cancer Control [UICC] classification system. Tumor stage was dichotomized with I + II = “low” and III + IV = “high.”
Comorbidities were self-reported by the patients at baseline (“Do you have other physical illnesses?”). If they reported at least one comorbid disease, they were classified as having a comorbid condition.
Statistical analysis
Trends in the development of the QoL domains over four measurement points were graphically investigated with age-adjusted marginal means. ANOVAS were calculated to test if there were significant changes in means between all four time points. To analyze longitudinal associations between SES and QoL, mixed effect models for repeated measures were calculated using maximum likelihood (ML) estimation. Covariance type for within-participant correlation was selected using − 2 log likelihood and fit indices (AIC, BIC) to account for correlations among repeated measures in participants (PF, SF, RF: diagonal; GQoL, EF: scaled identity). To capture longitudinal associations between the variables of interest, seven models for each scale were calculated. First, unconditional mean models (model 1) with random intercepts were examined to assess individual variation in QoL domains at baseline without regard to time. The proportion of outcome variation (intraindividual and interindividual) is calculated to evaluate the necessity of individual growth curve modeling [26]. If the ICC (intraclass correlation coefficient) is 0.25 or above, growth curve modeling is required. Next, unconditional linear growth models (model 2) were performed to evaluate individual changes over time. Therefore, time × time (time quadratic, model 3) and time × time × time (time cubic, model 4) were added to test non-linear changes in QoL. If the χ2 difference test indicated significant improvements in the fitness of the non-linear growth model compared to the linear growth model, quadratic and cubic time terms were retained for further analyses. Afterwards, three conditional growth models were conducted for all scales. The first model (model 5) included all SES indicators (income, school education, vocational training, job type) and the relevant covariates (age, sex, cohabitation). If there were significant associations in model 5 between SES indicators and QoL, disease and treatment factors (tumor stage, type of cancer, therapy) were added to the next model (model 6). In a following step, comorbidity was included (model 7) because prior studies have shown its impact on QoL [27]. Finally, interactions containing significant SES indicators with the respective growth parameters were added to model 7. Analyses were done using the IBM SPSS® Statistics Version 22.
Results
Sample characteristics
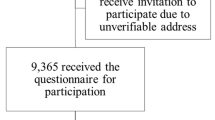
A total of 591 patients were admitted to the hospital during the study period. Twenty-six patients (4%) had to be excluded because cancer was not histologically confirmed, leaving 565 patients eligible for the study. Of those, 123 (22%) declined study participation (reasons were lack of interest n = 81, too distressed because of the disease n = 13, mentally distressed n = 18; 11 did not provide any reason). There was no evidence for differences in age (p = .44), sex (p = .21), and tumor stage at presentation (p = .06) between participants and non-participants. Baseline data was available from 411 patients, and 31 entered the study after t1 (reasons were declined participation at t1 n = 2, could not be reached at t1 n = 6, interviewer was notified too late n = 23), resulting in 442 sets of data to be analyzed.
The mean age of participants was 64 years (SD = 11), and 70% of them were male. The most frequent tumor sites were head and neck (19%), prostate (18%), urinary organs (11%), brain (9%), lung (8%), and colorectal (7%). The majority of the patients (64%) had tumor stage III or IV at the time of diagnosis, and 105 (24%) suffered from advanced cancer (Table 1).
In total, 63 (14%) study participants died over the course of the 6-month follow-up period (until t2 n = 4, until t3 n = 43). Those patients reported lower levels of physical functioning (p < .01), role functioning (p < .01), social functioning (p = .03), cognitive functioning (p = .02), and global quality of life (p = .04) at baseline. Participation per time point was n = 411 at t1, n = 355 at t2, n = 265 at t3, and n = 235 at t4 (192 subjects were assessed all four times, 78 three times, 92 twice, and 80 were assessed at a single timepoint).
Trends in quality of life
There was a significant (p < .05) decrease in physical, social, and role functioning and global QoL and an increase in emotional functioning in the time between hospital admission and hospital discharge (Fig. 1). Physical and role functioning, as well as global QoL, increased significantly between hospitalization and the 3-month follow-up measurement point. There were no significant changes on any of the scales between 3 and 6 months after baseline. There were no significant changes in cognitive functioning between baseline and any of the follow-up measurement points.
Trends in cancer patients’ quality of life over 6 months starting with hospital admission (estimated marginal means, age-adjusted). PF physical functioning, EF emotional functioning, RF role functioning, SF social functioning, QL global quality of life, CF cognitive functioning: t1 = beginning of hospitalization, t2 = hospital discharge, t3 = 3 months after baseline, t4 = 6 months after baseline
Unconditional mean models (model 1)
For physical functioning, the ICC was 0.55, suggesting that 55% of the variation is due to interindividual differences. The ICC for emotional functioning, role functioning, social functioning, cognitive functioning, and global QoL was 0.50, 0.43, 0.41, 0.57, and 0.50, respectively.
Unconditional linear growth models (model 2)
There were significant intercepts and slopes in all QoL domains, except for cognitive and role function, indicating that patients varied in their baseline levels and linear growth with a linear decrease in physical functioning and social functioning, and linear increase in emotional functioning and global QoL. Because cognitive functioning showed no changes over the course of the study and no interindividual difference in trajectory change (β = − 0.52, SE = 0.53, p = .33); this scale was omitted from further analyses [26]. Because of the obvious non-linear growth and the significant changes from baseline to t2 and t2 to t3 and t4, role functioning was also tested for non-linear growth in further analyses. The estimated intercept and linear slope parameters for the unconditional linear growth models are presented in Table 2 (model 2).
Unconditional non-linear growth models (models 3 and 4)
There was a significant positive quadratic effect in physical functioning, role functioning, and global QoL and a negative quadratic effect in emotional functioning (Table 2). Comparing the unconditional linear models to the non-linear growth models, there was a significant improvement for physical functioning (χ2 = 11,515.24–11,498.19 = 17.05, p < .01) [28], emotional functioning (Δχ2 = 5.11, p = .02), role functioning (Δχ2 = 29.30, p < .01), and global QoL (Δχ2 = 5.16, p = .02). Because there was no significant quadratic effect for social functioning and no improvement in model fit (Δχ2 = .68, p = .41), we only retained the linear time term in the subsequent models.
Physical functioning, role functioning, and global QoL showed a significant negative cubic change. Given that the cubic models improved model fit over the quadratic growth models for the three scales (PF Δχ2 = 5.58, p = .02, RF: Δχ2 = 25.61, p < .01, GQoL: Δχ2 = 11.46, p < .01), cubic growth parameters were retained in the subsequent models. Because no cubic effect was found for emotional functioning (Δχ2 = 0.03, p = .86), the following models contained only the quadratic time term.
Conditional growth models (models 5–7)
Because of some missing data in SES indicators and the necessity of having equal numbers of participants to be able to compare models, conditional models were analyzed with n = 318. Fixed effects of the conditional growth models are presented in Table 2 (models 5–7). Income was a predictive factor for QoL for all functional scales except social functioning. After adjustment for age, sex, and cohabitation, lower income was still associated with worse QoL. We additionally controlled for tumor stage, type of cancer, therapy, and comorbidity in the final models (model 7), and the effects remained significant. Patients with lower income showed 8.8 percentage points (PP) lower physical functioning, 4.9 PP lower emotional functioning, 11.4 PP lower role functioning, and 6.6 PP lower global QoL. Social functioning was associated with participants’ vocational training. After controlling for all covariates, having no vocational education or apprenticeship was associated with 6.2 PP better social functioning compared to higher or university education. School education and job type showed no relation to any of the QoL domains. To examine whether income and vocational training not only predict the level of QoL but also the rate of change, an interaction was added to model 7 (time × vocational training to social functioning and time × income, time2 × income, time3 × income to the other scales). Interactions were only significant for role functioning (time × income: β = 37.38, SE = 14.88, p = .01, time2 × income: β = − 33.63, SE = 13.31, p = .01, time3 × income: β = 6.86, SE = 2.90, p = .02) indicating that the decline in role functioning from t1 to t2 was greater for high-income participants (− 45.50) than the decline by lower income participants was (− 45.50 + 37.38 = − 8.12). However, in terms of quadratic growth, there was a faster rate of change for high-income patients (33.61) compared to low-income people (33.61 + (− 33.63) = − 0.20). High income was also associated with a slower rate of cubic change (Fig. 2). Comparing residual variances of the unconditional linear growth model with the model with interaction shows that income accounted for 23% (t1), 8% (t2), 7% (t3), and 22% (t4) of the within-individual variations in role functioning [26].
Discussion
The current study investigates the impact of SES on QoL among cancer patients using a longitudinal design with four measurement points. Results show that income is a predictive factor of QoL. Patients living in households that have a monthly income of less than 1000 euros per person had lower physical, emotional, and role functioning as well as reduced global QoL compared to patients with incomes above that threshold. Our findings are in line with previous studies which also found associations between income and functional scales and global QoL among breast and prostate cancer patients [20, 29]. However, Hofreuter-Gätgens [23] identified income disparities among prostate cancer patients but not among breast cancer patients.
The association between income and QoL could have been created by confounding factors. One possible explanation is that the difference in tumor stage at presentation leads to worse QoL. There is indeed evidence that low-income patients are more likely to be diagnosed with more advanced disease stages compared to high-income patients [2]. This may be due to delayed presentation in people with lower SES [30]. Additionally, longer waiting times until first treatment for free of charge access could also influence QoL at time of diagnosis [31]. At the same time, impairments in QoL due to income were also found in long-term cancer survivors [19]. Because income remained a significant predictor after controlling for tumor stage, type of cancer, and therapy, there must be further factors, which influence the association between income and QoL. The mediating role of health behavior is a second possible explanation. In a cancer mortality study, physical activity, diet, and BMI were all found to be possible risk factors that contribute to the association between mortality and SES [32]. Psychosocial factors may also explain the differences in QoL. Low SES people report lower levels of social support and weaker social networks [33]. This is of great importance, because poorly functioning social relationships have been found to negatively influence health [34, 35]. In addition, lower income was associated with higher rates of labor force departure [36] which in turn leads to more fractured social networks and decreased social support. Furthermore, people with low SES report more depressive symptoms and anxiety, both conditions which can negatively impact QoL [37]. In particular, fearful and fatalistic beliefs concerning cancer diagnoses and greater worries about money were more commonly found in patients with lower SES [38, 39]. At the very least, high income serves as resource for accessing additional forms of support in coping with the disease (e.g., supplements, alternative medicine, recreation).
To date, no study has tested the influence of income on the trajectories of the QoL scales. In our study, changes in role functioning were influenced by patients’ income. Whereas there was a faster decline for patients with high income between diagnosis and the end of hospitalization, they also had a substantial increase in the 3 months afterward. One explanation could be that patients with higher incomes have a greater feeling of being restricted by their hospitalization because it forces them to miss work. Because of their financial resources, it may be easier for these patients to cope with the disease after their hospital stay, resulting in a faster increase in their role functioning.
In the present study, vocational training was associated with better social functioning in that way that patients with no higher education or apprenticeship showed better functioning. Because higher education was found to positively influence social network size [33], less educated patients may represent a case of quality trumping quantity since they appear to have better social functioning and fewer social relations.
Primary or secondary education and job type were not related to QoL in our study. Maybe this is due to the short length of the follow-up period (6 months following hospitalization). In another study, social inequalities became apparent 12 months after acute treatment and were much less pronounced 6 months after diagnosis [23].
The present study has a number of strengths. To our knowledge, this is one of the first longitudinal studies to examine different SES indicators and their impact on a range of QoL outcomes among cancer patients in Germany. This is of great importance considering the fact that QoL is a powerful predictor for survival [16, 17]. Moreover, the findings underline the fact that social inequalities not only exist at the time of diagnosis but remain unchanged after treatment.
Besides these strengths, the current study is subject to some limitations. Changes in QoL may be biased by response shift which means that changes in QoL are not due to the studied variables but rather to shifts in internal standards, values, or conceptualizations [40]. Because income was assessed at the time of admission to the hospital, the current cancer diagnosis may already have negatively influenced the actual amounts. It also has to be noted that there was a large number of missing data for income.
In conclusion, the present analysis shows that income plays an important role in cancer patients’ QoL. Not having received vocational training or undergone an apprenticeship was associated with better social functioning. Primary or secondary education and job type seem to be less important for cancer patients’ QoL. Tailored interventions should be developed to improve low-income patients’ QoL considering the special needs they have in coping with this disease.
References
Mackenbach JP, Stirbu I, Roskam A-JR et al (2008) Socioeconomic inequalities in health in 22 European countries. N Engl J Med 358(23):2468–2481
Singer S, Roick J, Briest S, Stark S, Gockel I, Boehm A, Papsdorf K, Meixensberger J, Müller T, Prietzel T, Schiefke F, Dietel A, Bräunlich J, Danker H (2016) Impact of socio-economic position on cancer stage at presentation. Int J Cancer 139(8):1696–1702
Woods LM, Rachet B, Coleman MP (2006) Origins of socio-economic inequalities in cancer survival. Ann Oncol 17(1):5–19
Kogevinas M, Porta M (1997) Socioeconomic differences in cancer survival: a review of the evidence. IARC Sci Publ 138:177–206
Klein J, Knesebeck O (2016) Soziale Ungleichheit und Krebs. In: Mehnert A, Koch U (eds) Handbuch Psychoonkologie, 1. Auflage edn. Hogrefe, Göttingen, pp 121–244
Kuznetsov L, Mielck A (2012) Regional concentration of social disadvantage and of risks for lung cancer and colon cancer: systematic review and recommendations for research. Gesundheitswesen 74(6):42–51
Doubeni CA, Laiyemo AO, Major JM, Schootman M, Lian M, Park Y, Graubard BI, Hollenbeck AR, Sinha R (2012) Socioeconomic status and the risk of colorectal cancer. Cancer 118(14):3636–3644
Shack L, Jordan C, Thomson CS et al (2008) Variation in incidence of breast, lung and cervical cancer and malignant melanoma of skin by socioeconomic group in England. BMC Cancer 8:271
Meijer M, Bloomfield K, Engholm G (2013) Neighbourhoods matter too. J Epidemiol Community Health 67(1):6–13
Hoebel J, Kroll LE, Fiebig J, Lampert T, Katalinic A, Barnes B, Kraywinkel K (2018) Socioeconomic inequalities in total and site-specific cancer incidence in Germany. Front Oncol 8:402
Gondos A, Bray F, Brewster DH, Coebergh JW, Hakulinen T, Janssen-Heijnen ML, Kurtinaitis J, Brenner H, EUNICE Survival Working Group (2008) Recent trends in cancer survival across Europe between 2000 and 2004. Eur J Cancer 44(10):1463–1475
Mielck A, Vogelmann M, Leidl R (2014) Health-related quality of life and socioeconomic status. Health Qual Life Outcomes 12:58
Miravitlles M, Naberan K, Cantoni J, Azpeitia A (2011) Socioeconomic status and health-related quality of life of patients with chronic obstructive pulmonary disease. Respiration 82(5):402–408
Kogevinas M, Pearce N, Susser M et al (2006) Social inequalities and cancer. IARC scientific publication no. 138. World Health Organization, Geneva
Dalton SO, Schüz J, Engholm G, Johansen C, Kjær SK, Steding-Jessen M, Storm HH, Olsen JH (2008) Social inequality in incidence of and survival from cancer in a population-based study in Denmark, 1994-2003. Eur J Cancer 44(14):2074–2085
Montazeri A (2009) Quality of life data as prognostic indicators of survival in cancer patients. Health Qual Life Outcomes 7:102
Quinten C, Martinelli F, Coens C, Sprangers MAG, Ringash J, Gotay C, Bjordal K, Greimel E, Reeve BB, Maringwa J, Ediebah DE, Zikos E, King MT, Osoba D, Taphoorn MJ, Flechtner H, Schmucker-von Koch J, Weis J, Bottomley A, on behalf of Patient Reported Outcomes and Behavioral Evidence (PROBE) and the European Organization for Research and Treatment of Cancer (EORTC) Clinical Groups (2014) A global analysis of multitrial data investigating quality of life and symptoms as prognostic factors for survival in different tumor sites. Cancer 120(2):302–311
Lee YJ, Suh S-Y, Choi YS, Shim JY, Seo AR, Choi SE, Ahn HY, Yim E (2014) EORTC QLQ-C15-PAL quality of life score as a prognostic indicator of survival in patients with far advanced cancer. Support Care Cancer 22(7):1941–1948
Ferrell BR, Dow KH, Leigh S, Ly J, Gulasekaram P (1995) Quality of life in long-term cancer survivors. Oncol Nurs Forum 22(6):915–922
Klein J, Lüdecke D, Hofreuter-Gätgens K, Fisch M, Graefen M, von dem Knesebeck O (2017) Income and health-related quality of life among prostate cancer patients over a one-year period after radical prostatectomy. Qual Life Res 26(9):2363–2373
Simon AE, Wardle J (2008) Socioeconomic disparities in psychosocial wellbeing in cancer patients. Eur J Cancer 44(4):572–578
Penson DF, Stoddard ML, Pasta DJ, Lubeck DP, Flanders SC, Litwin MS (2001) The association between socioeconomic status, health insurance coverage, and quality of life in men with prostate cancer. J Clin Epidemiol 54(4):350–358
Hofreuter-Gätgens K, Klein J, Knesebeck Ovd (2017) Soziale Ungleichheit bei Brust- und Prostatakrebs. Inanspruchnahme von Versorgungsleistungen, gesundheitsbezogene Lebensqualität und Rückkehr zur Arbeit. Medizinsoziologie
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, Haes JCJM, Kaasa S, Klee M, Osoba D, Razavi D, Rofe PB, Schraub S, Sneeuw K, Sullivan M, Takeda F (1993) The European Organization for Research and Treatment of Cancer QLQ-C30. JNCI J Natl Cancer Inst 85(5):365–376
Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A (2001) ORTC QLQ-C30 Scoring Manual, 3rd edn. EORTC Publications, Brussels
Shek DTL, Ma CMS (2011) Longitudinal data analyses using linear mixed models in SPSS. Sci World J 11:42–76
Vissers PAJ, Thong MSY, Pouwer F, Zanders MMJ, Coebergh JWW, van de Poll-Franse LV (2013) The impact of comorbidity on health-related quality of life among cancer survivors. J Cancer Surviv 7(4):602–613
Singer JD, Willett JB (2003) Applied longitudinal data analysis. Modeling change and event occurrence. Oxford Univ. Press, Oxford
Ristevska G, Rajchanovska D, Jovanovska T, Dejanova B (2017) Low income deteriorates quality of life in early breast cancer survivors. Eur Psychiatry 41:S670–S671
Macleod U, Mitchell ED, Burgess C, Macdonald S, Ramirez AJ (2009) Risk factors for delayed presentation and referral of symptomatic cancer. Br J Cancer 101(Suppl 2):S92–S101
Domenighetti G, Vineis P, de Pietro C et al (2010) Ability to pay and equity in access to Italian and British National Health Services. Eur J Pub Health 20(5):500–503
Hastert TA, Ruterbusch JJ, Beresford SAA, Sheppard L, White E (2016) Contribution of health behaviors to the association between area-level socioeconomic status and cancer mortality. Soc Sci Med (1982) 148:52–58
Weyers S, Dragano N, Möbus S, Beck EM, Stang A, Möhlenkamp S, Jöckel KH, Erbel R, Siegrist J (2008) Low socio-economic position is associated with poor social networks and social support. Int J Equity Health 7:13
Vonneilich N, Jöckel K-H, Erbel R, Klein J, Dragano N, Weyers S, Moebus S, Siegrist J, von dem Knesebeck O (2011) Does socioeconomic status affect the association of social relationships and health? A moderator analysis. Int J Equity Health 10:43
Mehnert A, Lehmann C, Graefen M et al (2010) Depression, anxiety, post-traumatic stress disorder and health-related quality of life and its association with social support in ambulatory prostate cancer patients. Eur J Cancer Care 19(6):736–745
Earle CC, Chretien Y, Morris C, Ayanian JZ, Keating NL, Polgreen LA, Wallace R, Ganz PA, Weeks JC (2010) Employment among survivors of lung cancer and colorectal cancer. J Clin Oncol 28(10):1700–1705
Alfonsson S, Olsson E, Hursti T, Lundh MH, Johansson B (2016) Socio-demographic and clinical variables associated with psychological distress 1 and 3 years after breast cancer diagnosis. Support Care Cancer 24(9):4017–4023
Loehrer PJ, Greger HA, Weinberger M et al (1991) Knowledge and beliefs about cancer in a socioeconomically disadvantaged population. Cancer 68(7):1665–1671
Macleod U, Ross S, Fallowfield L, Watt GCM (2004) Anxiety and support in breast cancer. Br J Cancer 91(5):879–883
Hamidou Z, Dabakuyo TS, Bonnetain F (2011) Impact of response shift on longitudinal quality-of-life assessment in cancer clinical trials. Expert Rev Pharmacoecon Outcomes Res 11(5):549–559
Funding
This study was funded by the German Federal Ministry of Health (grant number NKP-332-026).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed within this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roick, J., Danker, H., Kersting, A. et al. The association of socioeconomic status with quality of life in cancer patients over a 6-month period using individual growth models. Support Care Cancer 27, 3347–3355 (2019). https://doi.org/10.1007/s00520-018-4634-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4634-y