Abstract
Purpose
The aim of this study was to assess the difference in explained variance of Health-Related Quality of Life (HRQoL) between comorbidity, sociodemographic characteristics and cancer characteristics. This association was assessed among thyroid cancer, colorectal cancer, and (non-)Hodgkin's lymphoma patients.
Methods
Data from three large population-based surveys on survivors of thyroid cancer, colorectal cancer, and (non-)Hodgkin's lymphoma were used. Cancer-specific HRQoL was assessed with the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30) of which physical function, emotional function, fatigue, and pain were included in the analyses. Comorbidity was assessed using the Self-reported Comorbidity Questionnaire. The association between comorbidity and HRQoL was assessed with multivariate linear regression models. Semi-partial R 2 was reported to assess the amount of variance in HRQoL explained by comorbidity in comparison with sociodemographic and cancer characteristics.
Results
In total, 3,792 cancer survivors were included in this analysis. The variance in HRQoL subscales explained by comorbidity was higher compared with sociodemographic and cancer characteristics for physical function (11–17 vs. 2–4 and 1–2 %, respectively) and emotional function (7–17 vs. 1–3 and 1–3 %, respectively), regardless of cancer type. In addition, comorbidity explained 7–20 and 11–13 % of the variance in pain and fatigue, respectively, compared to 0–4 % for both sociodemographic and cancer characteristics. Osteoarthritis and back pain were strongly associated with physical function and pain, while depression was strongly associated with emotional function. Depression and back pain were strongly associated with fatigue.
Conclusions
This study showed that comorbidity explained more variance in physical and emotional function, pain, and fatigue in comparison with sociodemographic and cancer characteristics in cancer survivors, regardless of cancer type. Our findings emphasize the importance of adjusting for the presence of comorbid diseases when assessing HRQoL in cancer survivors.
Implication for cancer survivors
Cancer survivors suffering from comorbid diseases experience lower levels of health-related quality of life. Clinicians should become more aware of the impact of comorbidity on HRQoL and provide necessary psychological support to assist self-management of comorbid diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Comorbidity is a complex issue in cancer research. Worldwide, there is a trend of aging of the population [1]. At the same time, the number of cancer survivors is rapidly increasing due to earlier diagnosis and more effective treatments [2]. Together, these two trends increase the number of patients who survive cancer and have coexisting disease(s), comorbidity. In The Netherlands, around 60 % of elderly cancer patients aged 65 years or older suffer from at least one other serious condition with the highest prevalence being previous cancer, heart disease, hypertension, chronic obstructive pulmonary disease (COPD), and diabetes mellitus [3].
Recently, in cancer research, more attention is being paid to health-related quality of life (HRQoL) of cancer survivors [4], where previously the focus was more on objective outcome measures such as treatment effects and mortality. Comorbid diseases generally affect patients' HRQoL negatively, with somatic comorbid conditions affecting mainly physical HRQoL and psychiatric disorders affecting mainly psychosocial aspects of HRQoL [5, 6]. A study among head and neck cancer patients showed that having two or more comorbid conditions was strongly associated with decreased HRQoL subscales [7, 8]. Another previous study among 158 prostate cancer survivors showed that the Charlson combined comorbidity index impacted on global health and physical function domains of HRQoL [9]. Furthermore, severe comorbidity among lung cancer patients resulted in poorer HRQoL compared to lung cancer patients with no severe comorbidity [10]. Our previous research showed that comorbidity is a strong independent predictor of HRQoL in colon and rectal cancer survivors [11, 12]. Furthermore, disease characteristics were less important in predicting HRQoL in cancer survivors, compared with social and demographic characteristics [13, 14]. Previous studies mainly focused on head and neck cancer, lung cancer, and prostate cancer patients, and all studies found an association between comorbidity and a lower HRQoL. This implies that comorbidity might impact on HRQoL generalizable to a wider range of cancer types.
Furthermore, not much attention has been paid to the relative impact of comorbidity on HRQoL. Most studies do not investigate the variance in HRQoL explained by comorbidity, while this effect size can address the relative importance of comorbidity in comparison with sociodemographic characteristics and cancer characteristics. One study conducted among inpatients showed that comorbidity explained 20–60 % of the total variance of the model predicting HRQoL subscales [15]. One previous study among breast cancer patients found that comorbidities explained most variance on nearly all subscales of HRQoL in comparison with demographics and clinical variables [16]. Furthermore, comorbidity was found to be an independent prognostic indicator among cancer survivors [3]. While the number of comorbidities increases with age [17], the elderly are often less aggressively treated compared to younger cancer patients [3]. Therefore, we will also conduct a subanalysis among elderly cancer survivors.
The aim of this study was to assess the difference in explained variance of HRQoL between comorbidity, sociodemographic characteristics and cancer characteristics. This association was assessed among thyroid cancer, colorectal cancer, and (non-)Hodgkin's lymphoma patients. We hypothesized that (1) comorbidity explains a similar or higher amount of variance in HRQoL measures compared with sociodemographic and cancer characteristics, (2) comorbidity has an impact on HRQoL regardless of cancer type, and (3) there is a higher prevalence of comorbidity and a higher impact of comorbidity on HRQoL among the elderly cancer patients. The results of this study could highlight the importance of including and correcting for a measure of comorbidity in studies addressing HRQoL among cancer survivors.
Methods
Subjects
For this study, data from three large population-based surveys on survivors of thyroid cancer, colorectal cancer, and non-Hodgkin's and Hodgkin's lymphoma conducted between 2008 and 2010 were used. The aim of these surveys was to assess late treatment effects, physical, and mental HRQoL along with other patient-reported outcomes among cancer survivors. Data from these studies will become available online for noncommercial scientific research, subject to study question, privacy and confidentiality restrictions, and registration from our patient-reported outcomes registry, PROFILES (www.profilesregistry.nl) [18].
The Eindhoven Cancer Registry (ECR), maintained by the Comprehensive Cancer Center South, records data on all newly diagnosed cancer patients in the southern region of The Netherlands covering an area with 2.3 million inhabitants and ten hospitals [19]. All thyroid cancer patients diagnosed between 1990 and 2008, all colorectal cancer patients diagnosed between 2000 and 2009, and all lymphoma patients diagnosed between 1999 and 2008 were eligible for participation in the surveys. All cancer patients were surveyed at least 6 months after their cancer diagnosis, in order to ensure that cancer treatment was completed at the time of the survey, and at most 10 years (colorectal cancer and (non-)Hodgkin's lymphoma) to 20 years (thyroid cancer) after cancer diagnosis. Detailed flow charts of the patient samplings have been reported elsewhere [20–22]. Patients who died prior to the study start were identified through the Central Bureau of Genealogy, which collects information on all deceased Dutch citizens via the civil municipal registries and hospital records. After excluding the deceased patients, the treating physicians verified the status of each eligible patient before the patient was approached for study participation (e.g., patients with serious cognitive impairment or who were in transition to terminal care were excluded). All eligible patients received an invitation letter with a login account and password to complete the survey online. If patients did not have access to internet or preferred to take the survey on paper, they could return a postcard, and they received the paper questionnaire within 1 week. After 2 months, reminders were sent to patients who did not respond to the survey. More detailed information on the method of data collection is described elsewhere [18]. After completion of the data collection, data from each patient were linked to their clinical characteristics registered in the ECR. All surveys were approved by a medical ethics committee.
Clinical and sociodemographic characteristics
Information on clinical characteristics was available from the ECR, where date of cancer diagnosis, primary treatment, and cancer stage are routinely collected from medical records by trained registrars. Since the ECR only collects data on the primary tumor and treatment, it cannot be ascertained that patients were disease-free at the time of the survey. Sociodemographic characteristics, including age, gender, and educational level, were assessed in the questionnaire. In this study, education level was categorized as high (pre-university education, high vocational training or university) compared with medium or low.
Health-Related Quality of Life
All cancer survivors completed the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30) (version 3.0) to assess cancer-specific quality of life. The QLQ-C30 is a 30-item self-report questionnaire which covers five function scales, a measure of global health or quality of life, and nine scales on symptoms and side effects. [23]. Since the EORTC QLQ-C30 does not include an overall score of all scales, and in order to prevent multiple testing and avoid an associated type 1 error, the four most important or distinctive scales were selected. Physical function was included; this scale is hypothesized to be most distinctive for the somatic health of different subgroups of cancer survivors [11, 21]. Furthermore, the emotional function scale was included to investigate the impact of comorbidity on mental health as well. Finally, the symptoms pain and fatigue were included since these symptoms are highly prevalent among different groups of cancer survivors [24–26]. All items were scored on a scale from 1 (not at all) to 4 (very much) and then linearly transformed to a 1 to 100 scale; a higher score on function domains represents better function and quality of life, while a higher score on symptom scales represents more symptoms [27].
Comorbidity
Comorbidity was assessed using a modified version of the Self-Administered Comorbidity Questionnaire [15]. The questionnaire addressed the prevalence, hindrance in daily activity, and treatment of 14 comorbidities including heart disease, stroke, high blood pressure, COPD/asthma, diabetes, stomach disease, kidney disease, liver disease, anemia, depression, thyroid disease, osteoarthritis, back pain, and rheumatoid arthritis. Since measuring hindrance in daily activities could be intertwined with measures of HRQoL, this could pose a confounding effect in our planned analyses. Therefore, we only addressed the number of prevalent comorbidities, and not treatment, and hindrance in daily activities, resulting in a score ranging between 0 and 14.
In addition, the effect of individual comorbidities on HRQoL was studied among the two largest cancer patient samples including colorectal cancer and non-Hodgkin's lymphoma patients. Among thyroid cancer and Hodgkin's lymphoma patients, the prevalence of specific comorbidities was not high enough, with 10 out of 14 and 14 out of 14 comorbidities being prevalent in less than 50 patients, respectively. Stroke, stomach, kidney, and liver diseases were prevalent in less than 5 % of the colorectal cancer and non-Hodgkin's lymphoma patients and were therefore excluded from further analysis as well.
Statistical analyses
Differences in baseline characteristics of the study population were analyzed using analysis of variance or chi-square, where appropriate. Unadjusted associations between the number of prevalent comorbidities (0, 1 or ≥2) and HRQoL subscales were studied and presented graphically.
Multivariate linear regression models were constructed to assess the variance in HRQoL subscales explained by the number of comorbidities, which was entered as a continuous variable into the model. Explained variance was reported as the semi-partial correlation coefficient in percentages in order to assess the unique contribution of each independent variable. The semi-partial correlation coefficients (R 2) of age, gender, and education were summed and further referred to as sociodemographic characteristics. Similarly, the coefficients of years after cancer diagnosis, primary cancer treatment, and, where appropriate, cancer stage, are further referred to as cancer characteristics. Thereafter, all comorbidities, with an arbitrarily chosen prevalence of 5 % or higher, were included separately into the model to study the effect of each individual comorbid disease on HRQoL domains. Since anemia (3–8 %) has previously been reported as being an important long-term effect of cancer treatment in non-Hodgkin's and Hodgkin's lymphoma patients, this disease was included in further analyses [28].
A subanalysis among the elderly aged 70 years or older was conducted to investigate whether the association between comorbidity and HRQoL domains was different from the total study population by using a comparable method as for the main analyses. We defined elderly oncology patients as those ≥70 years old, according to the European Society for Medical Oncology [29]. Hodgkin's patients were excluded from this analysis since only 13 Hodgkin's patients were 70 years or older. Due to the large number of statistical tests conducted in this study and to avoid type 1 errors, all differences with a P value <0.01 were indicated as statistically significant. All statistical analyses were performed using SAS statistics (version 9.2 for Windows, SAS institute Inc., Cary, NC).
Results
Characteristics of the study population
Seventy-one percent of the 5,317 invited cancer survivors returned a completed questionnaire; 892 invited patients actively refused or did not complete the survey for other reasons; and the address of 633 patients could not be verified (Fig. 1). Response rates were 69, 73, and 67 % among thyroid cancer, colorectal cancer, and (non-)Hodgkin's lymphoma patients, respectively. Respondents were on average 2 years younger and 6 % more often male and surveyed closer to their cancer diagnosis compared with nonrespondents. In addition, respondents were 4 % more often treated with surgery and 6 % more often treated with chemotherapy or surgery and radiotherapy. Detailed information of the study populations is described elsewhere [20, 21, 30]. In total, 3,792 patients were included in the present study (Table 1). Hodgkin's lymphoma patients were the youngest and most highly educated compared to the other cancer patients included. Thyroid cancer patients were surveyed furthest from their diagnosis (10 ± 5 years) compared with other cancer patients included (5 ± 3 years). Primary cancer treatment and cancer stage differed significantly between the four different cancer types. Hodgkin's lymphoma patients scored highest on physical function compared to the other cancer patients. Emotional function was highest, while fatigue symptoms were lowest among colorectal cancer survivors.
Comorbidity
Colorectal and thyroid cancer patients suffered from most comorbid diseases with 46 and 44 % suffering from two or more comorbid conditions, respectively (Table 2). Heart disease was most prevalent among colorectal cancer and non-Hodgkin's lymphoma patients with an approximate prevalence of 20 %. High blood pressure (35 %) and diabetes (15 %) were most prevalent among colorectal cancer survivors. Anemia was highest among non-Hodgkin's lymphoma patients (8 %), while thyroid disease was most prevalent among thyroid cancer patients (30 %) and Hodgkin's lymphoma patients (12 %).
Number of comorbidities and HRQoL
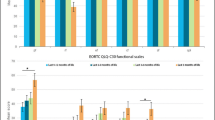
Among all cancer survivors, except for thyroid cancer patients, having one and/or two or more comorbidities was significantly associated with lower physical and emotional function and higher levels of pain and fatigue (Fig. 2a–d). Among thyroid cancer patients, no significant difference in emotional function between no, one, or two or more comorbidities was observed. Similarly, physical function was lower, while levels of pain and fatigue were higher among thyroid cancer patients having one and/or two comorbidities compared with those who had no comorbidity.
a–d Means of four domains of the QLQ-C30 questionnaire according to the number of comorbidities among thyroid (a), colorectal cancer (b), Hodgkin's lymphoma, (c) and non-Hodgkin's lymphoma patients (d). †P < 0.01, significantly different from participants with no comorbidity. ‡P < 0.01, significantly different from participants with no comorbidity and those with one comorbidity. Pain and fatigue are scored in opposite direction with higher scores indicating more symptoms
Multivariate linear regression models showed that the number of comorbidities was strongly related to the studied subscales of the QLQ-C30, with a P value <0.01 among all cancer survivors. All standardized betas were in the expected direction with more comorbidities resulting in lower physical and emotional function (standardized betas; −0.3 to −0.5). Similarly, having more comorbidities was associated with higher levels of pain and fatigue, with all standardized betas ranging between 0.3 and 0.5.
These models also showed that the variance explained by the number of comorbidities was higher compared with sociodemographic and cancer characteristics for all cancer survivors (Fig. 3a–d). The number of comorbidities explained 11–17 % of the variance in physical function compared with 2–4 and 1–2 % for sociodemographic and cancer characteristics, respectively. A 7–17 % of the variance in emotional function was explained by the number of comorbidities compared with 1–3 % for both sociodemographic and cancer characteristics. Finally, the number of comorbidities explained 7–20 and 11–13 % of the variance in pain and fatigue, respectively, compared with 0–4 % for both sociodemographic and cancer characteristics. When including the overlap between the studied predictors of HRQoL as well, the total explained variance (R 2) of the models ranged between 9 and 27 % (Fig. 3a–d).
a–d Variance (semi-partial R 2 (in percentage)) explained by sociodemographic characteristics (age, gender, and educational level), cancer characteristics (primary treatment, stage, and years after diagnosis), and the number of comorbidities among thyroid cancer (a), colorectal cancer (b), Hodgkin's lymphoma, (c) and non-Hodgkin's lymphoma patients (d)
Individual comorbidities and HRQoL
Including the selected comorbidities separately in the model resulted in higher proportions of explained variance (2–11 %) for all studied subscales compared to including the number of comorbidities (Table 3 and Fig. 3). Variance in physical function was explained most by heart disease and back pain with 2–4 % among colorectal and non-Hodgkin's lymphoma patients (Table 3). Depression explained most variance in emotional function with 12 and 8 % among colorectal and non-Hodgkin's lymphoma patients, respectively. Variance in pain was explained most by back pain with around 7 %, and variance in fatigue was mainly explained by depression and back pain with 2–3 %. Again, all significant standardized betas were in the expected direction ranging between −0.1 and −0.2 for physical function, between −0.1 and −0.4 for emotional function, between 0.1 and 0.3 for pain, and between 0.1 and 0.2 for fatigue. The total explained variance (R 2) in HRQoL ranged between 20 and 30 % across the different models.
Elderly
Comorbidity among thyroid cancer, colorectal cancer, and non-Hodgkin's lymphoma patients was significantly higher among the elderly. Fifty-two percent of those aged ≥70 years suffered from two or more comorbid conditions compared with 38 % of survivors younger than 70 years old. Compared to patients aged <70 years old, the prevalence of heart disease (28 vs 11 %), stroke (4 vs 1 %), hypertension (38 vs 27 %), diabetes (16 vs 10 %), anemia (7 vs 4 %), and osteoarthritis (31 vs 21 %) was significantly (P value < 0.01) higher among elderly aged ≥70 years. Thyroid disease and depression were less prevalent among the elderly aged ≥70 years compared to the younger patients with 5 vs 8 % and 6 vs 8 %, respectively. When studying the association between the number of comorbidities and HRQoL outcomes in multivariate regression models, similar results as for the total study population were found for elderly colorectal cancer patients (Fig. 4b). Among elderly thyroid cancer patients, the number of comorbidity explains more of the variance in emotional function, pain, and fatigue compared to the total sample (Fig. 4a). Among elderly non-Hodgkin's patients, the number of comorbidities explained less while cancer characteristics explained more variance in all studied subscales compared with the total population (Fig. 4c). When including the overlap between the studied predictors of HRQoL, the total explained variance (R 2) of the models ranged between 9 and 46 %.
a–c Variance (semi-partial R 2 (in percentage)) explained by sociodemographic characteristics (age, gender and educational level), cancer characteristics (primary treatment, stage, and years after diagnosis), and the number of comorbidities among the elderly (≥70 years) thyroid cancer (a), colorectal cancer (b), and non-Hodgkin's lymphoma patients (c)
Discussion
In this study, we showed that in comparison with sociodemographic and cancer characteristics, comorbidity explained more variance in physical function, emotional function, pain, and fatigue. This was found regardless of cancer type. Similar patterns were seen for thyroid cancer, colorectal cancer, and (non-)Hodgkin's lymphoma patients. Among the elderly (≥70 years) thyroid cancer patients, comorbidity seemed to become more important, while in elderly (≥70 years) non-Hodgkin's lymphoma patients, cancer characteristics seemed to have greater impact on HRQoL compared to the results for the total population. As hypothesized, the prevalence of comorbidity was higher among the elderly, but did not have a higher impact compared to sociodemographic and cancer characteristics among all cancer survivors.
The total explained variance found in the models predicting physical function, emotional function, pain, and fatigue ranged between 9 and 27 %. This amount of explained variance is comparable to that of a previous study conducted among hospitalized patients who reported a total explained variance of 25, 19, and 20 % for physical functioning, bodily pain, and vitality, respectively [15]. Comorbidity explained about 7–19 % of the variance in HRQoL in our study. A previous study among breast cancer patients found that comorbidity explained less variance ranging between 0 and 10 %, which might be the result of this different study population [16]. In general, the total explained variance in our study is still somewhat low, with a maximum of 27 % of the variance explained. Other factors, which we did not take into account, could have contributed to the unexplained variance. Previous studies showed that personality traits such as neuroticism and coping strategies are also associated with HRQoL [31] and might have played a role. Another possible predictor is social support [32, 33], which might contribute to the studied association. In addition, symptoms of pain and fatigue are found to be associated with physical function [16], and omitting these symptoms could account for the low amount of explained variance in physical function that we found.
Among thyroid cancer patients, comorbidity seemed to increase in importance among the elderly compared with the total thyroid cancer sample. This might be a result of the increased prevalence of heart disease, high blood pressure, diabetes, and rheumatoid arthritis among the elderly. Similar results were found in a study among breast cancer patients, in which the impact of cancer and its treatment attenuated over time, while multimorbidity had greater impact on functional decline [34]. However, the prevalence of comorbidity was also higher among elderly colorectal cancer and non-Hodgkin's lymphoma patients where this higher importance of comorbidity was not observed. Among non-Hodgkin's lymphoma patients, the opposite was found, with comorbidity explaining less of the variance in HRQoL among the elderly compared to the total sample. Instead, cancer characteristics were more important among the elderly non-Hodgkin's lymphoma patients. This difference between the young and elderly non-Hodgkin's lymphoma patients could not be explained by differences in cancer stage, primary treatment, and time since diagnosis or type of non-Hodgkin's lymphoma (indolent or aggressive). Non-Hodgkin's lymphoma patients often receive intensive medical treatment which can interfere with HRQoL long after their treatment [35, 36]. But why elderly experience lower HRQoL as a result of cancer characteristics is unclear. Future studies should further assess the complex association between comorbidity and HRQoL among elderly cancer survivors.
This study contributes to the paucity of knowledge on the association between comorbidity and HRQoL in cancer survivors. It showed that comorbidity explained more of the variance in HRQoL compared with sociodemographic and cancer characteristics. Therefore, these results can contribute to further research addressing the challenging issue of the effect of comorbidity on HRQoL in cancer patients. In addition, clinicians should become more aware of the impact of comorbidity on HRQoL and provide necessary psychological support to assist self-management of comorbid diseases. The self-reported nature of our comorbidity assessment could be advantageous, since self-report shows high agreement with physician diagnoses [37], while comorbidity in administrative data is often underreported [38]. In addition, this is a large population-based study with a high response rate which enabled the identification of the comorbidities that were strongly associated with separate HRQoL subscales.
The inclusion of long-term survivors could have resulted in survivorship bias. This might especially be an issue among colorectal cancer and non-Hodgkin's lymphoma patients, since these patients have generally a worse prognosis compared to the other cancer types. As such, the possible inclusion of a healthier sample could have underestimated the prevalence of comorbidity. Furthermore, patients who are unable to complete questionnaires, due to severe illness or cognitive impairments, were excluded, while these patients are more likely to have a high burden of comorbidities as well. This could have resulted in an underestimation of the found association. In addition, our inclusion of the cancer types in this analysis is somewhat arbitrary, which was based on the availability of QLQ-C30 scores for comparison. However, we expect similar results in different cancer types as our results are in line with other studies focusing on other cancers.
Furthermore, the cross-sectional study design makes the direction of the association between comorbidity and HRQoL debatable. We cannot ascertain whether the self-reported comorbid conditions were present before the cancer diagnosis or developed thereafter. In addition, it is questionable whether the comorbidities measured in this study are independent predictors of HRQoL, since comorbid conditions can interact with treatments or could be caused by cancer treatment and synergistically lower HRQoL [39]. For example, anemia is common in cancer patients, and the risk of anemia increases when patients receive chemotherapy for a longer time [28], while thyroid disease is common among thyroid cancer patients and among Hodgkin's lymphoma survivors treated with external radiotherapy [40]. Furthermore, the prevalence of thyroid disease might have been overestimated among thyroid cancer patients as these patients might have reported having thyroid disease as a result of their cancer diagnosis. However, sensitivity analyses among thyroid cancer patients excluding thyroid disease as a comorbidity revealed similar findings (data not shown). In addition, some comorbid conditions might increase the risk of complications from cancer therapy, with, for example, diabetes increasing the risk of neuropathy in patients treated with paclitaxel [41], and hypertension and obesity increasing the risk of heart failure in patients treated with trastuzumab [42, 43]. Furthermore, lifestyle factors, such as eating patterns and physical activity, were out of the scope of this study but could have influenced the association between comorbidity and HRQoL. Therefore, future research should address the complex association between comorbidity and lifestyle factors and its association with HRQoL.
In conclusion, this study showed that comorbidity explains more variance in physical and emotional function, and pain and fatigue compared with sociodemographic and cancer characteristics in cancer survivors, regardless of cancer type. These results emphasize the importance of adjusting for the presence of comorbid diseases when assessing HRQoL in cancer survivors. Future research should focus on the prevention and treatment of comorbidity to improve HRQoL in cancer patients.
References
WHO. Active ageing: a policy framework. Geneva: World Health Organization; 2002.
Coleman MP, Gatta G, Verdecchia A, et al. EUROCARE-3 summary: cancer survival in Europe at the end of the 20th century. Ann Oncol. 2003;14:v128–49.
Janssen-Heijnen MLG, Houterman S, Lemmens VEPP, et al. Prognostic impact of increasing age and co-morbidity in cancer patients: a population-based approach. Crit Rev Oncol Hematol. 2005;55:231–40.
Kaplan RM. Quality of life: an outcomes perspective. Arch Phys Med Rehabil. 2002;83:s44–50.
Gijsen R, Hoeymans N, Schellevis FG, et al. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54:661–74.
Baumeister H, Balke K, Härter M. Psychiatric and somatic comorbidities are negatively associated with quality of life in physically ill patients. J Clin Epidemiol. 2005;58:1090–100.
El-Deiry MW, Futran ND, McDowell JA, et al. Influences and predictors of long-term quality of life in head and neck cancer survivors. Arch Otolaryngol Head Neck Surg. 2009;135:380–4.
Terrell JE, Ronis DL, Fowler KE, et al. Clinical predictors of quality of life in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 2004;130:401–8.
Wahlgren T, Levitt S, Kowalski J, et al. Use of the Charlson combined comorbidity index to predict postradiotherapy quality of life for prostate cancer patients. Int J Radiat Oncol Biol Phys. 2011;81:997–1004.
Grønberg BH, Sundstrøm S, Kaasa S, et al. Influence of comorbidity on survival, toxicity and health-related quality of life in patients with advanced non-small-cell lung cancer receiving platinum-doublet chemotherapy. Eur J Cancer. 2010;46:2225–34.
Thong MSY, Mols F, Lemmens VEPP, et al. Impact of chemotherapy on health status and symptom burden of colon cancer survivors: a population-based study. Eur J Cancer. 2011;47:1798–807.
Thong MSY, Mols F, Lemmens VEPP, et al. Impact of preoperative radiotherapy on general and disease-specific health status of rectal cancer survivors: a population-based study. Int J Radiat Oncol Biol Phys. 2011;81:e49–58.
Parker PA, Baile WF, Moor C, Cohen L. Psychosocial and demographic predictors of quality of life in a large sample of cancer patients. Psychooncology. 2003;12:183–93.
Lehto U-S, Ojanen M, Kellokumpu-Lehtinen P. Predictors of quality of life in newly diagnosed melanoma and breast cancer patients. Ann Oncol. 2005;16:805–16.
Sangha O, Stucki G, Liang MH, et al. The self-administered comorbidity questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Care Res. 2003;49:156–63.
Arndt V, Stegmaier C, Ziegler H, Brenner H. A population-based study of the impact of specific symptoms on quality of life in women with breast cancer 1 year after diagnosis. Cancer. 2006;107:2496–503.
Carreca I, Balducci L, Extermann M. Cancer in the older person. Cancer Treat Rev. 2005;31:380–402.
van de Poll-Franse LV, Horevoorts N, Eenbergen MV et al. The Patient Reported Outcomes Following Initial treatment and Long term Evaluation of Survivorship registry: scope, rationale and design of an infrastructure for the study of physical and psychosocial outcomes in cancer survivorship cohorts. Eur J Cancer. 2011;47:2188–94.
Coebergh JWW, Janssen-Heijnen MLG, Louwman WJ, Voogd AC. Cancer incidence and survival in the south of the Netherlands, 1955–1999 & incidence in the north of Belgium, 1996–1998 [CD-ROM]. Eindhoven: Comprehensive Cancer Centre South (IKZ); 2001.
Mols F, Denollet J, Kaptein AA, et al. The association between type D personality and illness perceptions in colorectal cancer survivors: a study from the population-based PROFILES registry. J Psychosom Res. 2012;73:232–9.
Mols F, Thong MSY, van de Poll-Franse LV, et al. Type D (distressed) personality is associated with poor quality of life and mental health among 3080 cancer survivors. J Affect Disord. 2012;136:26–34.
Husson O, Haak HR, Buffart LM, et al. Health-related quality of life and disease specific symptoms in long-term thyroid cancer survivors: a study from the population-based PROFILES registry. Acta Oncol. 2013;52:249–58.
Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Hofman M, Ryan JL, Figueroa-Moseley CD, et al. Cancer-related fatigue: the scale of the problem. Oncologist. 2007;12:4–10.
Green CR, Hart-Johnson T, Loeffler DR. Cancer-related chronic pain. Cancer. 2011;117:1994–2003.
Oerlemans S, Mols F, Issa DE, et al. A high level of fatigue among (long-term) non-Hodgkin lymphoma survivors: results from the longitudinal population-based PROFILES registry in the south of the Netherlands. Haematologica. 2013;98(3):479–86. doi:10.3324/haematol.2012.064907.
Fayers PM, Aaronson NK, Bjordal K, Sullivan M. EORTC QLQ-C30 scoring manual. Brussels, Belgium. 1995;1:1–49.
Ludwig H, van Belle S, Barrett-Lee P, et al. The European Cancer Anaemia Survey (ECAS): a large, multinational, prospective survey defining the prevalence, incidence, and treatment of anaemia in cancer patients. Eur J Cancer. 2004;40:2293–306.
Kristjansson S, Wyller T. Introduction. In: Schrijvers D, Aapro M, Zakotnik B et al. (eds): ESMO handbook of cancer in the senior patient, 1st Edition. Switzerland: Informa; 2010.
Husson O, Haak HR, Mols F, et al. Development of a disease-specific health-related quality of life questionnaire (THYCA-QoL) for thyroid cancer survivors. Acta Oncol. 2013;52(2):447–54. doi:10.3109/0284186X.2012.718445.
Østhus A, Aarstad AH, Olofsson J, Aarstad H. Comorbidity is an independent predictor of health-related quality of life in a longitudinal cohort of head and neck cancer patients. Eur Arch Otorhinolaryngol. 2013;270:1721–8.
Kroenke C, Kwan M, Neugut A et al. Social networks, social support mechanisms, and quality of life after breast cancer diagnosis. Breast Cancer Res. Treat. 2013;1–13.
Sammarco A. Perceived social support, uncertainty, and quality of life of younger breast cancer survivors. Cancer Nurs. 2001;24:212–9.
Cohen HJ, Lan L, Archer L, Kornblith AB. Impact of age, comorbidity and symptoms on physical function in long-term breast cancer survivors (CALGB 70803). J Geriatr Onco. 2012;3:82–9.
Jensen RE, Arora NK, Bellizzi KM, et al. Health-related quality of life among survivors of aggressive non-Hodgkin lymphoma. Cancer. 2013;119(3):672–80. doi:10.1002/cncr.27781.
Oerlemans S, Mols F, Nijziel M, et al. The impact of treatment, socio-demographic and clinical characteristics on health-related quality of life among Hodgkin's and non-Hodgkin's lymphoma survivors: a systematic review. Ann Hematol. 2011;90:993–1004.
Baumeister H, Kriston L, Bengel J, Härter M. High agreement of self-report and physician-diagnosed somatic conditions yields limited bias in examining mental–physical comorbidity. J Clin Epidemiol. 2010;63:558–65.
Powell H, Lim LLY, Heller RF. Accuracy of administrative data to assess comorbidity in patients with heart disease: an Australian perspective. J Clin Epidemiol. 2001;54:687–93.
Chen RC, Royce TJ, Extermann M, Reeve BB. Impact of age and comorbidity on treatment and outcomes in elderly cancer patients. Semin Radiat Oncol. 2012;22:265–71.
Hancock SL, Cox RS, McDougall IR. Thyroid diseases after treatment of Hodgkin's disease. N Engl J Med. 1991;325:599–605.
Lee JJ, Swain SM. Peripheral neuropathy induced by microtubule-stabilizing agents. J Clin Oncol. 2006;24:1633–42.
Perez EA, Suman VJ, Davidson NE, et al. Cardiac safety analysis of doxorubicin and cyclophosphamide followed by paclitaxel with or without trastuzumab in the North Central Cancer Treatment Group N9831 adjuvant breast cancer trial. J Clin Oncol. 2008;26:1231–8.
Tan-Chiu E, Yothers G, Romond E, et al. Assessment of cardiac dysfunction in a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel, with or without trastuzumab as adjuvant therapy in node-positive, human epidermal growth factor receptor 2-overexpressing breast cancer: NSABP B-31. J Clin Oncol. 2005;23:7811–9.
Acknowledgments
We thank all the patients and their doctors for their participation in the study. Special thanks to Dr. M van Bommel for her availability as an independent advisor and willingness to answer patients' queries. In addition, we thank the following hospitals for their cooperation: Amphia Hospital (Breda), Bernhoven Hospital (Veghel and Oss), Catharina Hospital (Eindhoven), Elkerliek Hospital (Helmond), Jeroen Bosch Hospital ('s-Hertogenbosch), Maxima Medical Center (Eindhoven and Veldhoven), St Anna Hospital (Geldrop), St Elisabeth Hospital (Tilburg), Twee Steden Hospital (Tilburg and Waalwijk), and VieCuri Hospital (Venlo and Venray).
The present research is supported in part by a Social Psychology Fellowship from the Dutch Cancer Society to Melissa Thong (no. UVT2011-4960) and a Cancer Research Award from the Dutch Cancer Society (no. UVT-2009-4349) to Lonneke van de Poll-Franse. Data collection for this study was funded by the Comprehensive Cancer Center South, Eindhoven, The Netherlands; the Center of Research on Psychology in Somatic diseases (CoRPS), Tilburg University, The Netherlands; and an investment subsidy (no. 480-08-009) of The Netherlands Organization for Scientific Research (The Hague, The Netherlands). The funding sources were neither involved in the collection, interpretation, and analysis of the data, nor in the decision for the writing and submission of this report for publication.
Conflict of interest
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vissers, P.A.J., Thong, M.S.Y., Pouwer, F. et al. The impact of comorbidity on Health-Related Quality of Life among cancer survivors: analyses of data from the PROFILES registry. J Cancer Surviv 7, 602–613 (2013). https://doi.org/10.1007/s11764-013-0299-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-013-0299-1