Abstract
Background
Expressive writing interventions are shown to confer physical and psychological benefits for Caucasian cancer survivors. This study evaluated the health benefits of an expressive writing intervention among breast cancer patients in mainland China.
Methods
Stage I-III Chinese breast cancer survivors undergoing chemotherapy were recruited in Shanghai, China. They (n = 90) were randomly assigned to one of three conditions: a positive thinking group (PTC) to write about the positive aspects of their cancer experience; a self-regulation condition (SRC) to write about their stress and coping efforts, deepest feelings, and positive aspects of their cancer experience; or a cancer-fact group (CFC) to write about facts relevant to their cancer experience. All groups wrote for 30 min every week for 4 weeks. Quality of life (QOL) was assessed using the FACT-B at baseline and 1- and 2-month follow-ups. Linear mixed effects models were used to test the hypotheses that the SRC and PTC would improve QOL compared to the CFC.
Results
QOL improved overtime in the whole sample. Contrary to hypotheses, the CFC had increased QOL compared with the SRC from baseline to both the 1- and 2-month follow-ups (ΔQOL = 9.31, p = 0.01, d = 0.44; ΔQOL = 9.45, p = 0.025, d = 0.49). The PTC did not differ from cancer-fact writing but had increased QOL compared with the SRC from baseline to both the 1- and 2-month follow-ups (ΔQOL = 7.44, p = 0.04, d = 0.35; ΔQOL = 11.72, p = 0.06, d = 0.61).
Conclusion
Interventions through expressive writing about positive experience and cancer facts are feasible and can benefit Chinese cancer patients undergoing chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cancer is the second leading cause of death worldwide [1]. Asia represents 60% of the world’s population [2], approximately 45% of all new cancer cases, and 50% of all cancer deaths in the world [3]. China, as one of the most populated countries, is currently observing a country-wide increase of cancer incidence [4]. A recent report estimated 4.3 million new cancer cases and 2.8 million cancer-related deaths in China in 2015, with breast cancer being the most common among women (estimated 268,000 new cases) [5]. As cancer treatments become more effective in China, the number of breast cancer survivors will rise bringing with it psychosocial and quality of life concerns (QOL) [6]. A recent study reported that Chinese breast cancer patients had lower quality of life compared with breast cancer patients in the USA [7]. However, with only a few exceptions [8], interventions focusing on improving QOL among survivors in China are largely lacking.
Expressive writing interventions have been shown to confer a variety of health benefits among non-Hispanic White cancer survivors in Western countries [9]. However, few studies examine how expressive writing benefits people from Eastern countries. The primary goal of the study was to examine the health benefits of expressive writing among Chinese breast cancer survivors in mainland China. Because quality of life is often jeopardized during chemotherapy [10, 11], the current study aims to examine the effects of expressive writing on quality of life among breast cancer survivors undergoing chemotherapy.
Expressive writing intervention
Over the past decade, there has been a growing interest in the health benefits of expressive writing interventions. Pennebaker and Beall conducted the first expressive writing study and randomly assigned participants to either an intervention group to write about their deepest thoughts and feelings related to traumatic experiences, or to a control group to write about a neutral topic unrelated to deep feelings. After four 20-min writing sessions, the intervention group experienced improved health outcomes [12]. Since then, a growing number of studies have found that expressive writing improves a variety of outcomes ranging from improved immunity and reduced stress [13]. A meta-analysis with 146 randomized controlled trials revealed that emotional disclosure confers a variety of benefits, including increased physical and psychological well-being [14].
Among cancer survivors in Western countries, expressive writing has been shown to improve multiple physical and mental health outcomes, including improvements in energy and sleep characteristics [15], depressive symptoms [16], emotional support [17], pain [18], and physical symptoms [19]. These findings suggest that expressive writing is an important brief intervention to investigate among cancer survivors. In a randomized controlled trial, 60 white breast cancer patients were randomly assigned to one of the three conditions: an emotional disclosure condition to write about their deepest feelings and thoughts, a benefit-finding condition to write about positive aspects of their cancer experience, and a control group to write about their cancer facts unrelated to emotions [19]. It was found that emotional disclosure reduced physical symptoms, and both emotional disclosure and benefit finding reduced medical appointments for cancer-related morbidities. If these findings can be directly applied to patients in Eastern countries, we expect that expressive writing can facilitate benefit finding and emotional disclosure would improve health outcomes compared to writing about cancer facts. Despite the success in some expressive writing studies discussed above, a recent meta-analysis on 16 RCTs did not find conclusive evidence for the benefits of writing on health or quality of life outcomes among cancer survivors [20]. The review, however, suggested that those who experience low levels of emotional support may benefit from expressive writing.
Expressive Writing and Culture
In Chinese culture, high levels of emotional restraint and control is encouraged to preserve group harmony [21]. Thus, Chinese individuals tend to suppress emotions and not disclose their emotional distress to others. Chinese breast cancer survivors are reluctant to disclose cancer-related distress with family members due to concerns of burdening others [22]. They are also reluctant to seek emotional support from friends or coworkers, as they may view seeking help from non-family members to be shameful [23]. Expressive writing interventions allow individuals to disclose emotional distress without burdening others or disrupting group harmony and may be a culturally sensitive and efficacious intervention for Chinese.
Most of the expressive writing studies have been conducted among non-Hispanic Whites and only a few among Asians. Lu and Stanton [24] developed a self-regulation moderator (SRM) model of expressive writing. The SRM model postulates cognitive reappraisal as a critical pathway in reducing the impact of stress and producing beneficial effects through expressive writing. The model was supported in a study showing that conditions prompting cognitive reappraisal benefited Asians more than Caucasians in improving physical symptoms, and combining emotional disclosure and cognitive reappraisal improved positive affect for both Asian and Caucasian healthy young adults [24]. A recent randomized controlled trial suggested that Chinese American breast cancer survivors may benefit from writing instructions that facilitate cognitive reappraisal and may not benefit from expressive writing that solely encourages emotional disclosure [25]. These studies suggest the effects of expressive writing vary depending on writing instructions and population characteristics. Although studies tested expressive writing among undergraduates in Mainland China [26, 27], no known studies to date have investigated the feasibility and efficacy of an expressive writing intervention among Chinese cancer survivors in Mainland China.
Current study
The current study aimed to investigate the effects of expressive writing on quality of life among Chinese breast cancer survivors undergoing chemotherapy in Mainland China. Quality of life (QOL) is a multi-dimensional concept that includes domains related to physical, functional, psychological/emotional, and social well-being in relation to health [28, 29]. QOL is an important outcome during cancer treatment as cancer patients often experience declined quality of life during chemotherapy [10, 11]. We hypothesized that the two experimental conditions (i.e., self-regulation and the positive thinking) would have better QOL compared to the control condition (i.e., cancer-fact writing). We additionally explore the differences in QOL between the two experimental conditions.
Methods
Participants
Eligible Chinese breast cancer survivors were asked to participate in a study that would address questions about their health and to write about their experiences relevant to cancer. Inclusion criteria were as follows: (1) being comfortable with writing in Chinese, (2) being between 18 and 65 years of age, (3) having been diagnosed with breast cancer stage I-III, and (4) finishing primary treatment (i.e., surgery) and undergoing chemotherapy. Exclusion criteria were diagnosis of (1) recurrent or metastatic disease, (2) brain dysfunction, or (3) psychosis. Eligibility was determined by two nurses who were part of the research team. Patients who were undergoing chemotherapy at the Clinical Center at the Fudan University Shanghai Cancer Center in Shanghai, China were evaluated for eligibility. The research team provided detailed information on the study, assessed participants for eligibility, and obtained informed consent. Approval for the study was obtained from the Fudan University Cancer Hospital Institutional Review Board.
Randomization
After eligibility was established, consent agreed, and baseline data collected, we randomly allocated participants using a computer-generated allocation (1:1:1) to one of the three writing conditions. Ninety participants were randomly assigned to three writing groups, and each group was assigned 30 participants. The investigator who conducted the randomization procedure placed group assignments in sealed opaque envelopes. After participants completed the baseline questionnaire, the investigator opened the envelope and gave participants corresponding writing instructions based on their condition assignment. Participants were told that the study aimed to understand their experiences through writing and were not aware of whether they were assigned to an active treatment or a control condition. Assessments of the outcomes were completed by participants’ self-report on the standardized questionnaire.
Procedures
Eligible survivors who consented to participate in this study completed a baseline questionnaire during their hospital visit in an office at the clinical center. After completing the questionnaires, participants were randomly assigned to one of three groups: a cancer-fact group, a positive thinking group, or a self-regulation group. The participants completed a 30-min expressive writing exercise at home every week for 4 weeks.
Participants in the cancer-fact condition (CFC) were asked to write about facts regarding their cancer diagnosis and cancer treatment for all four sessions. Participants in the positive thinking condition (PTC) were asked to write about positive experiences related to cancer for all four sessions. Participants in the self-regulation condition (SRC) engaged in four writing sessions which together were designed to prompt self-regulation by spurring stressors and goals into awareness and regulating thoughts and emotions through finding benefits and coping efforts. Participants in SRC wrote about a different topic each week: stress and impact of their cancer at week 1, their deepest thoughts and feelings regarding cancer at week 2, their coping efforts during week 3, and positive experiences related to their cancer at week 4. Participants were instructed to write for 30 min each week at a convenient time in a comfortable and private home setting. They were assured that their writing was confidential. To ensure participants felt their information would be kept private, participants were not asked to return their essays after completing the writing sessions. Following the four writing sessions, participants completed a questionnaire at 1- and 2-month follow-up.
Primary Outcome
Quality of Life
Participants completed a Chinese version [30] of the Functional Assessment of Cancer Therapy-Breast (FACT-B) [28]. The FACT-B includes a 27-item general scale (FACT-G) and an additional subscale assessing breast cancer concerns. The FACT-G has four subscales assessing physical (e.g., “I have pain”), social (e.g., “I get support from my friends”), emotional (e.g., “I am nervous”), and functional (e.g., “I am able to enjoy life”) aspects of QOL. The scale has been validated in a sample of Chinese breast cancer patients and demonstrated adequate psychometric properties [30]. Participants rated on a 5-point Likert scale ranging from 0 (not at all) to 4 (very much), and a composite total score was calculated by summing the 27 items. Higher scores indicated better overall QOL and specific health functioning. The Cronbach’s alpha were 0.86, 0.90, and 0.92 at baseline, 1-month, and 2-month follow-up, respectively.
Demographic (e.g., age, education, income, etc.) and medical information (e.g., stage at diagnosis) were self-reported through the baseline questionnaire.
Statistical Analysis
Power analysis revealed that 25 participants per group would yield 80% power to test the hypothesis with an estimated effect size of d = 0.8 [31] derived from a previous study [24] based on sample size calculation (http://www.sample-size.net/sample-size-means/). Data analyses were conducted using IBM statistics SPSS 24. Preliminary analyses were first conducted for descriptive statistics, baseline equivalence tests, attrition, and correlation among major variables. Baseline equivalence tests evaluating the success of randomization were also conducted with ANOVAs for continuous variables and chi-square tests for categorical variables to examine whether conditions differed in any variables at baseline. Attrition analysis was conducted to determine whether completers and non-completers differed in baseline variables.
Hypotheses were tested using a linear mixed model with the SPSS MIXED procedure to account for within-person correlation between time points and missing at randomness. The models included an AR1 covariance structure and a random intercept. The model regressed QOL on dummy-coded fixed effects of time (baseline as reference), treatment group (control as reference), and time by treatment group interactions. An additional model was repeated with SRC as the reference group. Significant time by treatment group interactions were followed up with contrasts examining differences in QOL changes across time (i.e., baseline to one-month and two-month follow-up) between groups. Additional planned post hoc tests also examined QOL change in time (i.e., baseline to 1-month and 2-month follow-up) within group to describe the trajectory.
Results
Preliminary Analysis
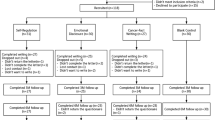
Participants were recruited between March and September, 2012. Figure 1 displays the trial profile. One-hundred twenty potential participants who met initial eligibility criteria were invited to participate in the study. Thirty declined due to lack of interest, being busy, or health concerns. The final sample included 90 patients who provided consented. Two participants from each of the conditions withdrew before completing any writing sessions. Eighty completed the 1-month follow-up, and 77 completed the 2-month follow-up. At the 1-month follow-up, two participants dropped out from PTC, and two participants dropped out from the CFC. At the 2-month follow-up, one more participant dropped out from each of the three groups.
All randomized participants were included in the data analyses. The final sample consisted of 90 survivors undergoing chemotherapy. Table 1 displays participant characteristics. ANOVA and chi-square tests were conducted to examine condition differences in the demographic and medical variables. Results showed no significant condition differences (ps > .163). There were also no significant condition differences at baseline QOL, F (2, 87) = 1.22, p = .300, ηp2 = .027.
The completers and non-completers were compared using independent-samples t tests and chi-square tests. The two groups did not differ in demographic variables (i.e., age, employment, and marital status), medical variables (i.e., stage and time since the first diagnosis of breast cancer) (ps > .182), or QOL at baseline (ps > .377). However, non-completers had lower education levels than completers (t = −3.33, p = .001). Household family income and education level were included as covariates based on bivariate correlations.
Main Analysis
We hypothesized that the intervention groups (i.e., SRC, PTC) would report higher QOL scores compared to the control group (i.e., CFC). We would also explore the differences between the SRC and the PTC. Tables 2 and 3 display estimated marginal means and results of the linear mixed effects model. Table 2 shows a significant time by group interaction and main effect of time, and no main effect of group. The time by group interaction was followed up by analyses examining QOL differences across time between groups. Table 3 shows that the CFC had more improvement in QOL compared to the SRC from baseline to both the 1-month and 2-month follow-ups. The PTC did not differ from the CFC; however, it had more improvement in QOL compared to the SRC from baseline to both the 1-month and 2-month follow-ups.
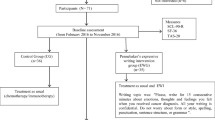
The significant main effect of time suggested that QOL in the sample improved over time. Figure 2 displays the time trend within each group. Contrasts examining QOL across times within group showed in Table 3 that the QOL improved in the PTC and had an upward but non-significant trend in the CFC from baseline to the 2-month follow-ups. The QOL declined in the SRC from the baseline to the 1-month follow-up but the change from baseline to the 2-month follow-up was not significant.
Discussion
The study examined the impact of expressive writing on quality of life. We hypothesized that the self-regulation condition (SRC) would report higher QOL compared to the cancer-fact condition (i.e., CFC). This hypothesis was not supported. On the contrary, the cancer-fact condition had increased quality of life compared with the self-regulation condition from baseline to both the 1-month and 2-month follow-ups. We also hypothesized that the positive thinking condition (PTC) would report higher QOL compared to the cancer-fact condition (i.e., CFC). This hypothesis was not supported. The positive thinking condition did not differ from the cancer-fact condition; however, it had increased quality of life compared with the self-regulation condition from baseline to both the 1-month and the 2-month follow-ups.
Cancer patients often experience declined quality of life during chemotherapy [10, 11]. In this intervention with patients undergoing chemotherapy, QOL improved in the whole sample. Specifically, the QOL improved in the positive thinking group and had an upward trend in the fact-writing condition from baseline to the 2-month follow-ups and only declined in the self-regulation condition from the baseline to the 1-month, but not 2-month follow-up. The self-regulation condition did not deliver benefits. It is plausible that the temporary decline of QOL in the self-regulation condition may be the natural course of chemotherapy. If that is the case, the improvement in QOL (7–11 points differences in FACT-B) among the PTC and CFC compared to the SRC could mark clinically significant changes, as 7–8-point differences in FACT-G are indicative of clinically significant QOL differences.
The findings that the cancer-fact condition had higher quality of life compared with the self-regulation condition did not support the previous literature among Caucasian cancer patients; however they were in line with a previous study among Chinese Americans, which found that cancer-fact-writing condition had better quality of life compared with the self-regulation and emotional disclosure conditions. In the previous study, the linguistic analysis of the written essays also revealed that the cancer-fact-writing group used more insight and causation words compared to the emotional disclosure group [25]. The current study also found that QOL significantly improved in PTC compared with SRC from baseline to 2-month follow-up. During chemotherapy, cancer patients often experience declined quality of life [10, 11]. The data suggest that writing about positive experiences and cancer-facts helped to cope better with the difficulties of chemotherapy than SRC did.
There are several plausible explanations. Both PTC and CFC focus on cognitive aspects rather than emotional disclosure. These findings suggest that Chinese may benefit from writing instructions facilitating cognitive processes [25]. Objective descriptions of stressful events could facilitate cognitive processing and increase acceptance of one’s breast cancer diagnosis, which in turn promotes adjustment [32]. The cancer-fact writing may also match well with thinking styles that Asians prefer. Cross-cultural research suggests that Asians are more likely to adopt avoidance goal [33] or avoidant coping strategies compared to non-Hispanic Whites [34]. Stanton et al. [19] found that those who were highly avoidant benefited more from writing about positive experiences, whereas those low in avoidance benefited more from emotional disclosure in improving psychological symptoms. Because Chinese are high in avoidance, they may benefit more from instructions facilitating cognitive tasks, such as fact writing or positive experiences, rather than tasks involving emotional disclosure. Future research should examine avoidance as a moderator of expressive writing in this population. Furthermore, perception of stigma surrounding cancer is prevalent in Chinese communities [35]. Perhaps due to the stigma, many women in the study had not disclosed to others about the events they wrote. Disclosing the suppressed emotions or thoughts, even intrapersonally, may require cancer patients to have more mental preparation than simply reading and following writing instructions. In contrast, women may be more comfortable with writing about cancer facts, which helps them to face the cancer experience, to process relevant information, and to find benefits without re-experiencing painful emotions. Finally, because women were in the middle of dealing with treatment, switching writing topics swiftly from stress, coping, emotions, to benefit finding as did in the self-regulation condition, might have not helped women from a coherent story naturally, even though the condition benefited survivors who have completed treatment [36].
Several limitations remain. First, written essays were not collected in the study and therefore no content or linguistic analysis could be made. However, this was a result of a conscious decision to ensure complete confidentiality, as many people have concerns about privacy due to the stigma of cancer in China. Second, the study was conducted with breast cancer survivors in China undergoing chemotherapy. Whether this could be generalized to other stages of cancer survivorship and to other countries needs to be tested in future research. Third, we did not have an assessment only control condition. However, previous expressive writing studies with cancer survivors suggest that the studies with a non-writing assessment only control group were more likely to find benefits of writing [16, 17] and thus the potential benefits of expressive writing may actually be larger compared to inactive controls. Finally, it is possible that longer-term follow-ups may reveal greater benefits of writing. Previous studies have showed that more robust effects emerged at the 6-month follow-up [25, 37], suggesting the importance of a long-term follow-up among patient populations for future studies.
Despite the limitations, the study has several strengths including a randomized controlled trial and two monthly follow-ups. Furthermore, it sheds light onto the expressive writing literature by extending a validated paradigm to an understudied patient population. Expressive writing is a brief intervention with minimal personnel requirement. As the first RCT expressive writing study conducted among cancer survivors in China, the study suggests that expressive writing is feasible and can be implemented among patients in hospital settings or at home. Thus, expressive writing has potential in China where mental health resources or well-trained mental health professionals are scarce.
Our findings suggest that Chinese breast cancer survivors undergoing chemotherapy treatment tend to benefit from writing instructions that facilitate cognitive processing. Future expressive interventions should test writing instructions focusing on cognitive tasks such as cognitive reappraisal and self-affirmation. The study challenges the implicit assumption that psychosocial interventions validated among Western countries can directly generalize to Eastern countries. Cultural adaptation and evaluation are critical for applying validated psychosocial interventions to new populations.
References
Global Burden of Disease Cancer C (2016) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 3:524. https://doi.org/10.1001/jamaoncol.2016.5688
Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat (2012) World Population Prospects: The 2012 Revision. Total Population - Both Sexes
Centers of Disease Control and Prevention (2011) Cancer survivors—United States, 2007. MMWR 60:269–272
Shin HR, Joubert C, Boniol M, Hery C, Ahn SH, Won YJ, Nishino Y, Sobue T, Chen CJ, You SL, Mirasol-Lumague MR, Law SC, Mang O, Xiang YB, Chia KS, Rattanamongkolgul S, Chen JG, Curado MP, Autier P (2010) Recent trends and patterns in breast cancer incidence among Eastern and Southeastern Asian women. Cancer Causes Control 21:1777–1785. https://doi.org/10.1007/s10552-010-9604-8
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66(2):115–132. https://doi.org/10.3322/caac.21338
WHOQOL group (1993) Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual Life Res 2:153–159
Lu Q, You J, Kavanagh A, Warmoth K, Meng Z, Chen Z, Chandwani KD, Perkins GH, McQuade JL, Raghuram NV (2016) Differences in quality of life between American and Chinese breast cancer survivors. Support Care Cancer 24(9):3775–3782. https://doi.org/10.1007/s00520-016-3195-1
Ye ZJ, Liang MZ, Qiu HZ, Liu ML, Hu GY, Zhu YF, Zeng Z, Zhao JJ, Quan XM (2016) Effect of a multidiscipline mentor-based program, Be Resilient to Breast Cancer (BRBC), on female breast cancer survivors in mainland China—a randomized, controlled, theoretically-derived intervention trial. Breast Cancer Res Treat 158(3):509–522
Merz EL, Fox RS, Malcarne VL (2014) Expressive writing interventions in cancer patients: a systematic review. Health Psychol Rev 8(3):339–361
van der Kloot WA, Uchida Y, Inoue K, Kobayashi K, Yamaoka K, Nortier HWR, Kaptein AA (2016) The effects of illness beliefs and chemotherapy impact on quality of life in Japanese and Dutch patients with breast or lung cancer. Chin Clin Oncol 5(1):3. https://doi.org/10.3978/j.issn.2304-3865.2016.01.01
Fairclough DL, Fetting JH, Cella D, Wonson W, Moinpour CM (1999) Quality of life and quality adjusted survival for breast cancer patients receiving adjuvant therapy. Qual Life Res 8(8):723–731. https://doi.org/10.1023/a:1008806828316
Pennebaker JW, Beall SK (1986) Confronting a traumatic event; toward an understanding of inhibition and disease. J Abnorm Psychol 95:274–281. https://doi.org/10.1037/0021-843X.95.3.274
Smyth J (1998) Written emotional expression: effect sizes, outcome types, and moderating variables. J Consult Clin Psychol 66(1):174–184. https://doi.org/10.1037/0022-006X.66.1.174
Frattaroli J (2006) Experimental disclosure and its moderators: a meta-analysis. Psychol Bull 132(6):823–865. https://doi.org/10.1037/0033-2909.132.6.823
De Moor C, Sterner J, Hall M, Warneke C, Gilani Z, amato R, Cohen L (2002) A pilot study of the effects of expressive writing in a phase II trial of vaccine therapy for metastatic renal cell carcinoma. Health Psychol 21:615–619. doi:https://doi.org/10.1037/0278-6133.21.6.615
Henry EA, Schlegel RJ, Talley AE, Molix LA, Bettencourt BA (2010) The feasibility and effectiveness of expressive writing for rural and urban breast cancer survivors. Oncol Nurs Forum 37:749–757. https://doi.org/10.1188/10.ONF.749-757
Gellaitry G, Peters K, Bloomfield D, Horne R (2010) Narrowing the gap: the effects of an expressive writing intervention on perceptions of actual and ideal emotional support in women who have completed treatment for early stage breast cancer. Psychooncology 19(1):77–84. https://doi.org/10.1002/pon.1532
Rosenberg HJ, Rosenberg SD, Ernstoff MS, Wolford GL, Amdur RJ, Elshamy MR, Bauer-Wu SM, Ahles TA, Pennebaker JW (2002) Expressive disclosure and health outcomes in a prostate cancer population. Int J Psychiatry Med 32(1):37–53. https://doi.org/10.2190/AGPF-VB1G-U82E-AE8C
Stanton AL, Danoff-Burg S, Sworowski LA, Collins CA, Branstetter AD, Rodriguez-Hanley A, Kirk SB, Austenfeld JL (2002) Randomized, controlled trial of written emotional expression and benefit finding in breast cancer patients. J Clin Oncol 20:4160–4168. https://doi.org/10.1200/JCO.2002.08.521
Zachariae R, O'Toole MS (2015) The effect of expressive writing intervention on psychological and physical health outcomes in cancer patients—a systematic review and meta-analysis. Psychooncology 24(11):1349–1359. https://doi.org/10.1002/pon.3802
Markus HR, Kitayama S (1991) Culture and the self: implications for cognition, emotion, and motivation. Psychol Rev 98(2):224–253. https://doi.org/10.1037/0033-295x.98.2.224
Warmoth K, Cheung B, You J, Yeung NCY, Lu Q (2017) Exploring the social needs and challenges of Chinese American immigrant breast cancer survivors: a qualitative study using an expressive writing approach. Int J Behav Med 24:827–835. https://doi.org/10.1007/s12529-017-9661-4
Wellisch D, Kagawa-Singer M, Reid SLR, Lin Y-J, Nishikawa-Lee S, Wellisch M (1999) An exploratory study of social support: a cross-cultural comparison of Chinese-, Japanese-, and Anglo-American breast cancer patients. Psychooncology 8(3):207–219. https://doi.org/10.1002/(sici)1099-1611(199905/06)8:3<207::aid-pon357>3.0.co;2-b
Lu Q, Stanton AL (2010) How benefits of expressive writing vary as a function of writing instructions, ethnicity and ambivalence over emotional expression. Psychol Health 25(6):669–684. https://doi.org/10.1080/08870440902883196
Lu Q, Wong C, Gallagher M, Tou R, Young L, Loh A (2016) Expressive writing among Chinese American breast cancer survivors: a randomized controlled trial. Health Psychol 36:370–379. https://doi.org/10.1037/hea0000449
Yang Z, Tang X, Duan W, Zhang Y (2015) Expressive writing promotes self-reported physical, social and psychological health among Chinese undergraduates. Int J Psychol 50(2):128–134. https://doi.org/10.1002/ijop.12081
Zhang Y, Duan W, Tang X, Yang Z (2014) Can virtues enhance the benefits of expressive writing among healthy Chinese? A pilot study. J Ment Health 23(5):231–235. https://doi.org/10.3109/09638237.2014.924050
Cella DF, Tulsky DS (1993) Quality of life in cancer: definition, purpose, and method of measurement. Cancer Investig 11(3):327–336. https://doi.org/10.3109/07357909309024860
Ware JE Jr, Manning WG Jr, Wells KB, Duan N, Newhouse JP (1984) Health status and the use of outpatient mental health services. Am Psychol 39(10):1090–1100. https://doi.org/10.1037/0003-066X.39.10.1090
Wan C, Zhang D, Yang Z, Tu X, Tang W, Feng C, Wang H, Tang X (2007) Validation of the simplified Chinese version of the FACT-B for measuring quality of life for patients with breast cancer. Breast Cancer Res Treat 106(3):413–418. https://doi.org/10.1007/s10549-007-9511-1
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Erlbaum, Hillsdale
Stanton AL, Danoff-Burg S, Cameron CL, Bishop M, Collins CA, Kirk SB, Sworowski LA, Twillman R (2000) Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. J Consult Clin Psychol 68:875–882. https://doi.org/10.1037/0022-006X.68.5.875
Elliot AJ, Chirkov VI, Kim Y, Sheldon KM (2001) A cross-cultural analysis of avoidance (relative to approach) personal goals. Psychol Sci 12(6):505–510
Chang EC (1996) Cultural differences in optimism, pessimism, and coping: predictors of subsequent adjustment in Asian American and Caucasian American college students. J Couns Psychol 43(1):113–123
Lu Q, Yeung NC, You J, Dai J (2016) Using expressive writing to explore thoughts and beliefs about cancer and treatment among Chinese American immigrant breast cancer survivors. Psychooncology 25(11):1371–1374. https://doi.org/10.1002/pon.3991
Lu Q, Gallagher MW, Loh A, Young L (2018) Expressive writing intervention improves quality of life among Chinese-American breast cancer survivors: a randomized controlled trial. Ann Behav Med kax067-kax067. https://doi.org/10.1093/abm/kax067
Lu Q, Zheng D, Young L, Kagawa-Singer M, Loh A (2012) A pilot study of expressive writing intervention among Chinese-speaking breast cancer survivors. Health Psychol 31(5):548–551. https://doi.org/10.1037/a0026834
Acknowledgments
We would like to thank all participants and nurses at the Fudan University Shanghai Cancer Center involved in the study and acknowledge the vital contributions of study researchers in the University of Houston and Fudan University.
Contributors
Author contributions include conception and design (Q.L., Y.H.), acquisition of data (L.D, J.L.H, Y.H.), data analysis and interpretation (Q.L., I.W., J.Y.), drafting (Q.L., J.Y.), or revising article (Q.L., I.W.) for intellectual content, and approval of the final draft (Q.L., L.D., I.W., J.Y., J.L.H., Y.H.).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Informed Consent statement
The human investigations were performed after approval by an institutional review board. The investigators obtained informed consent from each participant.
Rights and permissions
About this article
Cite this article
Lu, Q., Dong, L., Wu, I.H.C. et al. The impact of an expressive writing intervention on quality of life among Chinese breast cancer patients undergoing chemotherapy. Support Care Cancer 27, 165–173 (2019). https://doi.org/10.1007/s00520-018-4308-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4308-9