Abstract
Purpose
Patient navigation (PN) is a model of healthcare coordination designed to reduce barriers to achieving optimal health outcomes. Systematic reviews evaluating whether PN is associated with higher patient satisfaction with cancer care are lacking.
Methods
We conducted a systematic review to synthesize evidence of comparative studies evaluating the effectiveness of PN programs to improve satisfaction with cancer-related care. We included studies reported in English that: (1) evaluated a PN intervention designed to increase satisfaction with cancer care; and (2) involved a randomized controlled trial (RCT) or non-RCT approach. Standardized forms were used to abstract data from studies. These data were evaluated for methodological quality, summarized qualitatively, and synthesized under a random effects model.
Results
The initial search yielded 831 citations. Nine met inclusion criteria. Five had adequate data (1 RCT and 4 non-RCTs) to include in the meta-analysis. Methodological quality of included studies ranged from weak to strong, with half rated as weak. Findings of the RCTs showed a statistically significant increase in satisfaction with cancer care involving PN (standardized mean difference (SMD) = 2.30; 95% confidence interval 1.79, 2.80, p < 0.001). Pooled results from non-RCTs showed no significant association between PN and satisfaction with cancer-related care (standardized mean difference = 0.39; 95% confidence interval − 0.02, 0.80, p = 0.06).
Conclusions
Although PN has been widely implemented to improve cancer care, high-quality studies are needed to characterize the relationship between PN and satisfaction with cancer-related care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
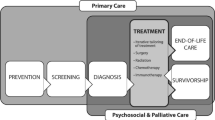
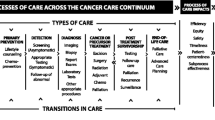
Patient navigation (PN) is a patient-centered healthcare delivery model that involves provision of support and guidance by trained lay or professional (e.g., nurse) navigators. Support and guidance are strategically delivered to help patients overcome barriers to obtaining optimal and timely cancer-related care and effectively utilize available cancer care resources. Three models of PN have been recommended based on navigator training and background [1, 2]. The first model emphasizes that navigators who provide screening, diagnostic, treatment, and survivorship PN should have specific professional training, such as nursing [3]. A second model indicates that the most important qualification of a patient navigator is being a “cultural broker and interpreter” who is from communities served by the PN program [4]. A third model indicates that a multidisciplinary team of lay and professional navigators should provide PN [5,6,7]. Some narrative and systematic reviews have found PN improves receipt and timeliness of cancer early detection care [8,9,10,11]. However, it is unknown whether PN improves receipt of cancer treatment [9, 10, 12, 13].
Patients’ satisfaction with cancer-related care is influenced by the degree to which healthcare experienced is perceived to match expectations. Patient satisfaction is frequently assessed when evaluating PN programs. Multiple working groups at the 2010 National Patient Navigation Leadership Summit recommended patient satisfaction with care as a key metric to evaluate PN interventions [14, 15]. As PN programs have been widely implemented in cancer care, the Academy of Oncology Nurse and Patient Navigators has recommended assessing patient satisfaction as an indicator of the “patient experience” [16]. Numerous studies have evaluated whether PN is associated with improved satisfaction with cancer-related care, but to date this research has not been critically evaluated or synthesized. In the present study, we critically assessed and synthesized currently available evidence on the effect of PN interventions (intervention) on satisfaction with cancer care (outcome) as compared to those not receiving PN (comparison). Participants included those being provided any type of cancer care. Study designs included randomized controlled trials (RCTs), case control trials, or quasi-experimental designs.
Materials and methods
Search strategy
A study protocol was developed a priori outlining the methodology for the present systematic review. In collaboration with a health librarian, an extensive literature search was conducted for relevant studies published between 1995 (year the first PN study was published) and May 25, 2016. The search strategy included MeSH terms and other identified key words (Fig. 1). Our research team searched multiple databases (PubMed/MEDLINE, CINAHL, Web of Science, PsycINFO) to locate studies that focused on evaluating effect of PN on satisfaction with cancer care.
Citations identified through four database searches were exported to the reference manager software Endnote® [17]. After completion of all searches, duplicate citations were removed, and titles and abstracts of remaining articles were reviewed by one study author to determine whether each study was eligible for inclusion in the systematic review. The final inclusion decision was based on a review of full text of the article describing that specific study. In addition, reference lists of all studies included in this systematic review were examined to identify additional published or unpublished studies that may not have been discovered during initial database searches. The same process was used to review articles identified from study references.
Inclusion criteria
Studies were included if they evaluated a PN program related to cancer care, measured patient satisfaction following a PN intervention, and compared it with a measurement of patient satisfaction among individuals who did not receive PN. Patient satisfaction was defined as the extent to which a person’s experience paralleled with his or her expectations [18]. For the purpose of this systematic review, we defined PN using a previously published definition of PN [10]. Thus, PN was defined as a barrier-focused intervention with the following common characteristics: (1) PN is provided to individual patients for a defined episode of cancer-related care (e.g., evaluating an abnormal screening test); (2) PN has a definite endpoint where services provided are complete (e.g., patient achieves diagnostic resolution following a screening abnormality); (3) PN targets a defined set of health services that are required to complete an episode of cancer-related care; (4) PN services focus on identification of individual patient-level barriers to accessing cancer care; and (5) PN aims to reduce delays in accessing the continuum of cancer care services [10]. Studies were included if they described interventions delivered by a patient navigator (paid or voluntary) in a community or medical setting that was intended to facilitate the following types of cancer-related care: screening, diagnostic resolution, initiation and completion of treatment, survivorship, genetic testing, and cancer clinical trials. Studies implementing any model of PN were included. Comparison groups in these studies included those that provided any health promotion intervention (i.e., health education, reminders) which did not involve the services of a patient navigator. Comparison groups also included participants who received no intervention or were placed in a wait-list control group. To be included, each study was required to have participants complete a measure of patient satisfaction with cancer-related care administered via self-report or interview.
Additionally, studies were eligible for inclusion in this systematic review if they used one of the following research approaches: RCT, case control trial, or a quasi-experimental design. Studies without comparison groups, review papers, and case studies were excluded. Furthermore, studies not published in English and those with fewer than five participants in each group were excluded. Both unpublished and published studies were eligible for inclusion. Unpublished studies included abstracts, conference presentations, unpublished theses and dissertations, or findings from studies that had been conducted but were not yet published in peer-reviewed or gray literature.
Data abstraction and management
Name of first author and publication year were used to identify each article in the present review. Two reviewers independently reviewed full text of all studies and abstracted data using a standardized data abstraction form that was modified from a previous systematic review [19]. A third researcher reviewed all data on the two sets of data abstraction forms for disagreements. Disagreements in data abstraction were resolved by consensus in collaboration with the third reviewer.
The primary study outcome was patient satisfaction with some aspect of cancer care. In addition, we abstracted data regarding whether the following variables influence the relationship between PN interventions and satisfaction with cancer-related care: sample characteristics (e.g., sample size, gender, age, race, ethnicity, education), PN intervention settings (e.g., urban, rural, medical or community centers), study design, measurement of patient satisfaction, model of PN intervention, type of cancer, and phase of cancer care targeted by the PN intervention.
Quality assessment
Quality of evidence for each study was examined using the Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies [20], which evaluates the following components of study quality: selection bias, bias due to study design, confounders, blinding of outcome assessment, data collection methods, and withdrawals and drop-outs. The strength of each component and global ratings range from weak to strong. Additional key assessment components included: type of comparison group, matching of control to intervention participants in quasi-experimental studies, length of time from baseline to follow-up, length of intervention, recruitment method, adherence to sampling period used for intervention, use of intention-to-treat analysis, and unit of randomization.
Statistical analysis
Data from RCTs and observational studies were pooled separately. Continuous data (i.e., overall patient satisfaction in both intervention and comparison groups at follow-up) were pooled under a random effects model and summarized as standardized mean difference along with 95% confidence intervals. Heterogeneity was assessed using I2 values where an I2 > 50% was considered significant. The meta-analysis was performed using Review Manager 5.3 [21].
Results
Study identification
Initial database searches yielded 816 articles (Fig. 2). Review of reference sections of these 816 articles revealed an additional 15 studies. Duplicate studies were removed along with 637 others based on reviews of their titles and abstracts. Thirty-two studies were retained, and full text of these studies was thoroughly reviewed to determine eligibility for inclusion in our analysis. Of these 32 studies, 23 did not meet inclusion criteria. Studies were excluded for the following reasons: did not include a PN intervention (n = 2), did not assess satisfaction with cancer care following a PN intervention (n = 11), no comparison group (n = 8), and reviews of literature (n = 2). Nine peer-reviewed published studies [22,23,24,25,26,27,28,29,30] were included in our systematic review (see Table 1), which made it impossible to adequately assess for publication bias.
Methodological quality
Based on criteria of the Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies [20], methodological quality of eight studies in this systematic review ranged from weak to strong. Two studies were rated as strong [25, 26], two were rated as moderate [24, 27], and four were rated as weak quality (Table 2) [22, 23, 28, 29]. One study [30] was not rated for methodological quality because it pooled data from eight other studies, making it impossible to provide specific data required to rate methodological quality. Additionally, the three studies that found PN was associated with higher satisfaction had quality ratings of “weak” [28], “moderate” [24], and “strong” [25]. The other five studies which found no relationship between patient satisfaction and PN were also rated as “weak” [22, 23, 29], “moderate” [27], and “strong” [26]. Multiple studies displayed weak ratings related to selection bias, handling of confounders, data collection methods, and tracking of withdrawals and dropouts.
Characteristics of studies
Measurement of study outcome: patient satisfaction
There were multiple self-report measures used to assess patient satisfaction. Five studies assessed patient satisfaction using measures with psychometric validation, ranging from calculation of internal consistency using Cronbach’s alpha to application of factor analysis and principal components analysis, as well as item response theory analysis. These measures included a modified version of the Satisfaction with Hospital Care Questionnaire [24, 31], the 18-item Patient Satisfaction with Cancer-Related Care (PSCC) scale [26, 30, 32], the European Organisation for Research and Treatment of Cancer quality of life group cancer inpatient satisfaction questionnaire (EORTC QLQ-SAT32) [25, 33], and the 18-item Patient Satisfaction Questionnaire (PSQ-18) [27, 34]. One study reported using a 29-item version of the PSCC (which included items discarded based on principal components analysis of the initial item pool) [29]. The remaining studies (n = 3) utilized non-psychometrically validated scales or surveys, including a single-item measure of satisfaction with care [22], an 8-item measure of satisfaction with care [28], and a 12-item measure of satisfaction with care comprised of items used in previous patient satisfaction tools [23].
There was limited information regarding assessment of reliability or validity of satisfaction measures among each study’s participants. Four studies reported information regarding internal consistency of the satisfaction measure that was calculated from participants’ responses, and all of these studies indicated that there was evidence of internal consistency for the measures used [24, 27, 28, 30]. Of three studies reporting that PN was associated with higher patient satisfaction, two used measures with evidence demonstrating their reliability or validity. Half of the studies that reported no statistically significant group difference in satisfaction between PN and control groups used patient satisfaction measures with evidence of reliability or validity [26, 27, 30].
Overall, we found satisfaction with cancer care to be moderate or high across most studies. In one study [22], mean patient satisfaction with cancer care scores were relatively high in both PN and control groups. Other studies dichotomized single items measuring satisfaction at “excellent” versus “not excellent” [23], or the entire patient satisfaction survey as “high satisfaction” versus “not high satisfaction” [26, 30]. The three studies that showed more variation in satisfaction had significantly lower patient satisfaction scores in the control groups [24, 25, 28]. Nonetheless, even the control groups had moderate to high levels of patient satisfaction [24, 25, 28].
Study sample characteristics
Baseline sample sizes for each individual study ranged from 44 to 1788 participants, with one study [30] including two samples—one sample assessing satisfaction with cancer diagnostic care and the other sample assessing satisfaction with cancer treatment. The combined samples of all the studies included in the present systematic review comprised 4210 individuals who completed satisfaction measures. Most of these studies provided PN to diverse populations (e.g., medically underserved racial-ethnic minority and lower income populations) [23, 26, 27, 30], non-English speakers [23], and people with a high school education or less [23, 24, 26,27,28, 30]. Two of these studies found that PN was associated with increased patient satisfaction in these populations [24, 28]. Additionally, two of the three studies that reported that PN was significantly associated with at least some increases in patient satisfaction were conducted outside of the USA (i.e., Korea and Canada), and provided minimal information about participants’ demographic characteristics [25, 28].
Model of patient navigation
Four PN studies utilized a nurse-delivered model of PN [22, 25, 27, 28], and three studies used a lay PN model [24, 26, 29]. One study that pooled data from multiple studies included multiple models of PN [30]. Another study did not specify the type of PN model [23]. Of the three studies that found some indication that PN was effective in improving some aspect of patient satisfaction, two implemented nurse navigation models [25, 28] and one used a lay PN model [24].
Type of cancer and point on cancer continuum
There was significant heterogeneity in studies included in this systematic review in terms of type of cancer care targeted by the PN intervention. Most studies had samples that combined patients with different types of cancer or different types of cancer-related abnormalities [22, 26, 28,29,30]. Two studies conducted with patients who received PN following abnormal test results found that PN was not related to higher patient satisfaction [29, 30]. Only one [28] of four studies conducted with patients diagnosed with cancer [22, 26, 28, 30] found that patients were more satisfied if they received PN compared to those who received usual care.
The remaining four studies narrowly focused on care related to one specific type of cancer. These studies included individuals who had an abnormal test finding for breast cancer [23, 24, 27] or individuals who were diagnosed with head and neck cancer [25]. Two of the breast cancer studies reported no significant differences in patient satisfaction between participants who received PN and those who did not [23, 27], and one study found those who received PN were more satisfied than those who received usual care [24]. The study of patients receiving treatment for head and neck cancer indicated that PN improved some aspects of patient satisfaction [25].
Setting of Patient Navigation Intervention
In four studies, PN was provided in hospitals [22, 24, 25, 28], including a comprehensive cancer center [22], university-affiliated hospitals [24, 28], and the oncology clinic of a university hospital [25]. Three hospital-based studies found PN was associated with better patient satisfaction with cancer-related care [24, 25, 28]. The other studies were conducted in a combination of settings [30] or in outpatient clinics [23, 26, 27, 29], including outpatient radiology clinics [27], oncology practices [26], and community health centers [23].
In addition, three studies [23, 24, 26] were conducted in urban areas, one was conducted in a rural area [22], and the geographic locations for four studies were not indicated [25, 27,28,29]. One study combined data from other studies conducted in both rural and urban locations [30]. Of three studies that reported that PN was associated with a higher level of patient satisfaction, one was conducted in an urban area [24] and the other two were conducted outside of the USA, in Korea and Canada [25, 28].
Outcomes of patient navigation intervention on patient satisfaction
Of the nine included studies, three [24, 26, 29] were RCTs, including two studies that randomized participants to navigation or control at the individual level [24, 26], and one study in which randomization was conducted at the clinic level [29]. Five studies were non-randomized studies [22, 23, 25, 27, 28], and one pooled data from both RCTs and non-randomized studies in its analysis [30]. All of these studies assessed overall satisfaction with cancer care. In addition, three studies [23, 25, 27] used single item or subscale measures of specific aspects of satisfaction with cancer care, including time spent with a physician, technical quality, communication and interpersonal skills, and satisfaction with financial aspects of care.
Overall satisfaction
Evaluation of the results of each specific study revealed that three studies reported higher overall satisfaction with cancer-related care among individuals who received PN compared to those who did not receive PN [24, 25, 28]. In contrast, five studies reported no statistically significant difference in overall satisfaction between PN and control groups [22, 23, 26, 27, 30]. Additionally, one study compared changes in patient satisfaction from the time of the identification of a potential cancer abnormality to within 180 days of diagnostic resolution between individuals who received PN and those who received written cancer information plus usual care [29]. This study found no significant differences between the two groups in satisfaction with cancer care (Table 3) [29].
Five studies [22, 24, 25, 27, 28] provided adequate data to be included in a meta-analysis to evaluate whether receipt of PN was associated with higher overall satisfaction with cancer-related care (Fig. 3). Of these five studies, one was a RCT [24] and the other four [22, 25, 27, 28] were non-randomized controlled trials (non-RCTs). The standardized mean difference for the RCT was 2.30 (95% confidence interval 1.79, 2.80, p < 0.001), indicating that participants in this study who received a PN intervention (n = 53) were significantly more satisfied than those participants who did not receive PN (n = 49) [24]. The pooled standardized mean difference for the four non-RCTs was 0.39 (95% confidence interval −0.02, 0.80, p = 0.06), indicating that patients who received PN (n = 241) were not more satisfied than those who did not receive PN (n = 176). Our analysis also revealed significant heterogeneity (I2 = 73%; p < 0.001) among the non-RCTs.
Satisfaction with specific types of cancer-related care
The three studies that evaluated satisfaction with specific types of cancer-related care varied considerably in outcome assessments [23, 25, 27] making it impossible to group their reported outcomes in any meaningful way. Therefore, each study is described separately with respect to whether there were differences in satisfaction with specific aspects of cancer-related care between participants who did and those who did not receive PN.
In a study of women undergoing cancer-related breast biopsies, those who received care in an outpatient radiology clinic with nurse-delivered PN had similar satisfaction scores as those who did not receive PN on all PSQ-18 subscales: Technical Quality, Interpersonal Manner, Communication, Financial Aspects, Time Spent with Doctor, and Accessibility and Convenience [27]. Overall, satisfaction with care was relatively high across most subscales of the PSQ-18 for both PN and usual care groups [27].
A second study assessed satisfaction among women referred to a hospital breast center for follow-up after an abnormal mammogram showed that patients who received PN had similar levels of satisfaction as those who did not receive PN [23]. This study used multiple single-item measures of patient satisfaction that were dichotomized to indicate whether patients rated each item as “excellent” or “not excellent.” More than half of participants in both groups rated care as excellent in the following areas: staff communication regarding what to expect during exam, being treated with dignity and respect, staff respect for privacy, staff assistance with pain and discomfort, instructions about home care, the way doctors and nurses answered questions, concern staff showed for patient’s concerns and worries, respect staff showed to family and friends, helpfulness of information, and communication between the breast center and patient’s primary care provider. Individuals who received PN were less likely to rate “staff concern for their cultural and religious beliefs and concerns” as excellent compared to individuals who did not receive PN [23].
The third study evaluating satisfaction with specific types of cancer-related care compared two cohorts of patients with head and neck cancer using the EORTC QLQ-SAT32 [33]. Patients who received PN reported significantly higher satisfaction with availability of doctors and nurses, interpersonal qualities of doctors, technical skills of doctors, doctors’ and nurses’ provision of information, and hospital waiting when compared to patients who did not receive PN [25]. Although there is not a nurse “psychosocial support” EORTC QLQ-SAT32 subscale [33], this study reported that individuals who received PN had more satisfaction with nurses’ “psychosocial support” than those who did not. There were no differences between patients who received PN and those who did not on satisfaction with the technical skills of nurses, hospital access, kindness, helpfulness, provision of information by hospital personnel, exchange of information with cancer care team, and comfort and cleanliness of hospital. Overall, this study found that patient satisfaction across specific aspects of care was relatively high across groups (cohorts that received PN and the cohort that did not) [25].
Discussion
In the present study, we critically assessed and synthesized available evidence regarding the effect of PN on satisfaction with cancer care. Our systematic review of nine studies that included a total of 4210 participants who completed patient satisfaction surveys found that most studies demonstrated that PN had either a neutral effect (neither increased nor decreased) or a positive effect (increased) patient satisfaction with cancer-related care. Across studies, ratings of satisfaction with cancer care were either moderate or high, indicating patients were generally satisfied with their care, whether or not they received PN. Data from five studies pooled for meta-analysis revealed mixed findings. One RCT indicated that PN was effective in increasing patient satisfaction with cancer care [24], whereas the remaining four non-RCTs showed that PN was not effective in increasing patient satisfaction with cancer care [22, 25, 27, 28]. There was significant heterogeneity among the non-RCTs, with varying types of cancer care targeted, settings where PN was implemented, PN models, and measures of patient satisfaction. All studies included in the systematic review applied PN to improve outcomes related to cancer diagnostic care (i.e., diagnostic resolution) or treatment (e.g., timely initiation and completion of cancer care). There were no studies evaluating whether PN improves satisfaction with cancer care related to screening, survivorship, genetic counseling, and recruitment and retention in clinical trials. There was significant variation in the methodological quality of the studies reviewed, with half of these studies rated as “weak,” due to limitations in the reporting of the studies. Many studies measured patient satisfaction with cancer-related care with patient satisfaction measures that were not psychometrically validated or reported administration or scoring of measuring using procedures that differed from standardized instructions. Additionally, our review only included one RCT in the meta-analysis [24] because the other single RCTs included in the present systematic review did not report adequate patient satisfaction data. Thus, poor reporting of patient satisfaction data in specific studies included in this review limited the ability to pool data from multiple RCTs and conduct any sensitivity analysis that may have been indicated.
To our knowledge, this study is the first comprehensive systematic review of cancer PN research focused on patient satisfaction. Findings should be considered in light of the fact that PN is viewed as a standard of cancer care. Starting in 2015, the American College of Surgeons Commission on Cancer required that a PN process be in place in order to accredit cancer centers [35]. While PN is associated with improvements in cancer screening rates, adherence to follow-up care after abnormal cancer results, and timeliness of diagnostic resolution of a cancer-related abnormality [9,10,11,12], the present study indicates that additional research needs to be conducted regarding whether PN is effective in increasing patient satisfaction across the cancer care continuum and across different types of cancers.
The present systematic review includes certain limitations to be considered in its interpretation. First, this study is comprised only of published peer-reviewed manuscripts that assessed effectiveness of PN on patient satisfaction with cancer care. While unpublished studies were eligible for inclusion, none met inclusion criteria for this systematic review. Another limitation involves the inclusion of PN studies published in English only. As such, we may have missed relevant data from studies published in different languages. Similar to all systematic reviews, our findings are limited by data reported in the original studies we reviewed, and some studies we reviewed did not report data in a format that could be incorporated in the meta-analysis.
In conclusion, this systematic review revealed mixed data regarding whether PN is effective in increasing patient satisfaction with cancer-related care. All studies included in this review evaluated PN interventions designed to improve cancer diagnostic and treatment care. There were significant limitations in quality and reporting of data in the original studies we reviewed, which also limited the data available for meta-analysis. Our findings suggest that given the limitations in quality and scope of research on PN, well-designed and systematically implemented RCTs are needed to draw conclusions about the effects of PN on patient satisfaction with cancer-related care across the cancer care continuum.
References
Wells KJ, Valverde P, Ustjanauskas AE, Calhoun EA, Risendal BC (2017) What are patient navigators doing, for whom, and where? A national survey evaluating the types of services provided by patient navigators. Patient Educ Couns 101:285–294. https://doi.org/10.1016/j.pec.2017.08.017
Wells KJ, Nuhaily S (2018) Models of patient navigation. In: Calhoun E, Esparza A (eds) Developing and implementing patient navigation programs. Springer, New York, NY
Hopkins J, Mumber MP (2009) Patient navigation through the cancer care continuum: an overview. J Oncol Pract 5:150–152
Braun KL, Kagawa-Singer M, Holden AE, Burhansstipanov L, Tran JH, Seals BF, Corbie-Smith G, Tsark JU, Harjo L, Foo MA, Ramirez AG (2012) Cancer patient navigator tasks across the cancer care continuum. J Health Care Poor Underserved 23:398–413
National Accreditation Program for Breast Centers (2014) NAPBC standards manual 2014 edition. American College of Suregons, Chicago, IL
Oncology Nursing Society, Association of Oncology Social Workers, National Association of Social Workers (2010) Oncology Nursing Society, the Association of Oncology Social Work, and the National Association of Social Workers joint position on the role of oncology nursing and oncology social work in patient navigation. Oncol Nurs Forum 37:251–252
Freeman HP (2012) The origin, evolution, and principles of patient navigation. Cancer Epidemiol Biomark Prev 21:1614–1617. https://doi.org/10.1158/1055-9965.EPI-12-0982
Genoff MC, Zaballa A, Gany F, Gonzalez J, Ramirez J, Jewell ST, Diamond LC (2016) Navigating language barriers: a systematic review of patient navigators' impact on cancer screening for limited English proficient patients. J Gen Intern Med 31:426–434. https://doi.org/10.1007/s11606-015-3572-3
Paskett ED, Harrop JP, Wells KJ (2011) Patient navigation: an update on the state of the science. CA Cancer J Clin 61(4):237–249. https://doi.org/10.3322/caac.20111
Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, Mandelblatt JS, Paskett ED, Raich PC, Program PNR (2008) Patient navigation: state of the art or is it science? Cancer 113:1999–2010. https://doi.org/10.1002/cncr.23815
Sunny A, Rustveld L (2016) The role of patient navigation on colorectal cancer screening completion and education: a review of the literature. J Cancer Educ. https://doi.org/10.1007/s13187-016-1140-0
Robinson-White S, Conroy B, Slavish KH, Rosenzweig M (2010) Patient navigation in breast cancer: a systematic review. Cancer Nurs 33:127–140. https://doi.org/10.1097/NCC.0b013e3181c40401
Baik SH, Gallo LC, Wells KJ (2016) Patient navigation in breast cancer treatment and survivorship: a systematic review. J Clin Oncol 34:3686–3696. https://doi.org/10.1200/JCO.2016.67.5454
Fiscella K, Ransom S, Jean-Pierre P, Cella D, Stein K, Bauer JE, Crane-Okada R, Gentry S, Canosa R, Smith T, Sellers J, Jankowski E, Walsh K (2011) Patient-reported outcome measures suitable to assessment of patient navigation. Cancer 117 (15, Suppl):3603-3617. doi:https://doi.org/10.1002/cncr.26260
Pratt-Chapman M, Simon MA, Patterson AK, Risendal BC, Patierno S (2011) Survivorship navigation outcome measures: a report from the ACS patient navigation working group on survivorship navigation. Cancer 117(15 Suppl):3575–3584. https://doi.org/10.1002/cncr.26261
Strusowski T, Sein E, Johnston D (2017) Academy of Oncology Nurse & Patient Navigators announces standardized navigation metrics. Journal of Oncology Navigation & Survivorship:8
Reuters T (2016) EndNote, New York
Pascoe GC (1983) Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann 6:185–210
Wells KJ, Lee JH, Calcano ER, Meade CD, Rivera M, Fulp WJ, Roetzheim RG (2012) A cluster randomized trial evaluating the efficacy of patient navigation in improving quality of diagnostic care for patients with breast or colorectal cancer abnormalities. Cancer Epidemiol Biomark Prev 21:1664–1672. https://doi.org/10.1158/1055-9965.Epi-12-0448
Effective Public Health Practice Project (1988) Quality assessment tool for quantitative studies. Effective Public Health Practice Project, Hamilton
Manager R (2014) The Cochrane collaboration. The Nordic Cochrane Centre, Copenhagen
Campbell C, Craig J, Eggert J, Bailey-Dorton C (2010) Implementing and measuring the impact of patient navigation at a comprehensive community cancer center [corrected] [published erratum appears in Oncol Nurs Forum 2010 May;37:260]. Oncol Nurs Forum 37:61–68. doi:https://doi.org/10.1188/10.ONF.61-68
Donelan K, Mailhot JR, Dutwin D, Barnicle K, Oo SA, Hobrecker K, Percac-Lima S, Chabner BA (2011) Patient perspectives of clinical care and patient navigation in follow-up of abnormal mammography. J Gen Internal Med 26:116–122. https://doi.org/10.1007/s11606-010-1436-4
Ferrante JM, Chen PH, Kim S (2008) The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health 85(1):114–124. https://doi.org/10.1007/s11524-007-9228-9
Fillion L, de Serres M, Cook S, Goupil RL, Bairati I, Doll R (2009) Professional patient navigation in head and neck cancer. Semin Oncol Nurs 25:212–221. https://doi.org/10.1016/j.soncn.2009.05.004
Fiscella K, Whitley E, Hendren S, Raich P, Humiston S, Winters P, Jean-Pierre P, Valverde P, Thorland W, Epstein R (2012) Patient navigation for breast and colorectal cancer treatment: a randomized trial. Cancer Epidemiol Biomark Prev 21:1673–1681. https://doi.org/10.1158/1055-9965.epi-12-0506
Harding M (2015) Effect of nurse navigation on patient care satisfaction and distress associated with breast biopsy. Clin J Oncol Nurs 19:E15–E20. https://doi.org/10.1188/15.CJON.E15-E20
Lee T, Ko I, Lee I, Kim E, Shin M, Roh S, Yoon D, Choi S, Chang H (2011) Effects of nurse navigators on health outcomes of cancer patients. Cancer Nurs 34:376–384. https://doi.org/10.1097/NCC.0b013e3182025007
Post DM, McAlearney AS, Young GS, Krok-Schoen JL, Plascak JJ, Paskett ED (2015) Effects of patient navigation on patient satisfaction outcomes. J Cancer Educ 30:728–735. https://doi.org/10.1007/s13187-014-0772-1
Wells KJ, Winters PC, Jean-Pierre P, Warren-Mears V, Post D, Van Duyn MA, Fiscella K, Darnell J, Freund KM (2016) Effect of patient navigation on satisfaction with cancer-related care. Support Care Cancer 24:1729–1753. https://doi.org/10.1007/s00520-015-2946-8
Hendriks AA, Oort FJ, Vrielink MR, Smets EM (2002) Reliability and validity of the Satisfaction with Hospital Care Questionnaire. Int J Qual Health Care 14:471–482
Jean-Pierre P, Fiscella K, Freund KM, Clark J, Darnell J, Holden A, Post D, Patierno SR, Winters PC (2011) Structural and reliability analysis of a patient satisfaction with cancer-related care measure: a multisite patient navigation research program study. Cancer 117:854–861. https://doi.org/10.1002/cncr.25501
Bredart A, Mignot V, Rousseau A, Dolbeault S, Beauloye N, Adam V, Elie C, Leonard I, Asselain B, Conroy T (2004) Validation of the EORTC QLQ-SAT32 cancer inpatient satisfaction questionnaire by self- versus interview-assessment comparison. Patient Educ Couns 54:207–212. https://doi.org/10.1016/S0738-3991(03)00210-6
Marshall GN, Hays RD (1994) The patient satisfaction questionnaire short-form (PSQ-18). Rand, Santa Monica, CA
Comission on Cancer (2012) Cancer program standards: ensuring patient-centered care. American College of Surgeons
Acknowledgements
The authors thank Kathryn Houk for her support in the development of the search strategy for this systematic review. We are also thankful to Charles Wells, Roxann Mouratidis, and Robyn Rosasco for their feedback on this manuscript.
Funding
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award numbers: 3U01CA116924-03S1, U54CA132384, U54CA132379, and R21CA161077. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wells, K.J., Campbell, K., Kumar, A. et al. Effects of patient navigation on satisfaction with cancer care: a systematic review and meta-analysis. Support Care Cancer 26, 1369–1382 (2018). https://doi.org/10.1007/s00520-018-4108-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4108-2