Abstract
Purpose
Studies of fatigue in childhood cancer survivors (CCS) are inconclusive, with some reporting increased fatigue prevalence in this population while others do not. Given the potentially significant consequences of unmanaged fatigue, we sought to estimate the prevalence of fatigue and to identify factors associated with fatigue in a population of non-CNS CCS ranging from adolescence to middle adulthood using a single fatigue measurement tool.
Methods
Two hundred sixty-eight CCS ages 12–49 years followed in a survivorship clinic at a single cancer center completed validated self-report measures of fatigue, depression, and quality of life. Demographic and current health data were collected by study questionnaire and chart review
Results
Based on age-adjusted population norms, the prevalence of fatigue was 13.8 %, which is not significantly different compared to results in healthy populations. Fatigue was independently associated with having ≥3 chronic health conditions (OR 4.27, 95 % CI 1.52–11.99). Fatigued participants reported lower overall quality of life scores (OR 0.86, 95 % CI 0.82–0.89) and were more likely to be depressed compared to non-fatigued patients (20.4 vs. 1.4 %, respectively, p < 0.0001). There were 41(78.8 %) survivors with fatigue in our population who did not report significant depression.
Conclusions
CCS did not demonstrate increased fatigue compared to age-matched normative data. Fatigued survivors were more likely to have multiple chronic conditions, depression, and decreased quality of life. Longitudinal study will promote better understanding of the relationship between fatigue and specific chronic conditions, thereby facilitating early identification of those individuals most at risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Significant advances in the care of children and adolescents diagnosed with cancer now ensure that more than 80 % will survive their disease [1]. Unfortunately many of these life-saving treatments lead to future health problems, and most of all CCS (95 %) will face at least one chronic health condition by middle age [2, 3]. Fatigue is a common and distressing symptom experienced by survivors of adult cancer, with research indicating a higher prevalence of fatigue in this group compared to the general population [4–7]. While a well-established side effect of active cancer treatment in children, less is known about the prevalence of fatigue in CCS after completion of therapy. Current research demonstrates inconsistent findings, with some studies reporting the prevalence of fatigue as greater in the CCS population [7–9], and others suggesting it is similar to fatigue prevalence in the general population [10, 11]. Characteristics of patient populations differ between studies, as do fatigue measurement tools, which may contribute to the variety of result outcomes.
Most studies of fatigue in CCS to date have been limited to reports of adult survivors (ages ≥18 years), with fewer studies including or specifically examining fatigue in adolescent survivors. The potential debilitating nature of severe fatigue necessitates a solid understanding of the role fatigue plays in survivorship. For adolescents and young adults, fatigue may interfere with acquisition of critical developmental milestones, including autonomy from parents, individual identity and personal values, strong peer relationships, including intimate and sexual relationships, as well as starting families, gaining financial independence, and preparing for advanced education or employment [12]. Disruption of any one of these developmental milestones by fatigue may significantly limit social and vocational opportunities and impair quality of life. Fatigue in middle adulthood can interfere with ability to work, maintain financial independence, and engage in care of family and relationships with partners and peers. However, before we can understand the impact of fatigue on key developmental milestones and quality of life indicators, we must first determine whether or not fatigue is a problem for this survivor population. To better understand the impact of fatigue on CCS across these age groups, our study aimed to determine the prevalence of self-reported fatigue in a CCS population including adolescents and adults using a single fatigue measurement tool. In addition, we sought to identify disease, treatment, and demographic correlates of fatigue and examine the relationship between fatigue and quality of life, including depression, in this CCS population.
Methods
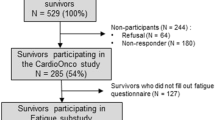
Participants
Participants were recruited from Project REACH (Research Evaluating After-Cancer Health), a longitudinal cohort study designed to evaluate psychosocial and medical outcomes in pediatric and adult cancer survivors followed in one of several long-term follow-up clinics within a single cancer center [13]. To be eligible for Project REACH, participants must be survivors of a malignancy other than nonmelanomatous skin cancer; ≥2 years from cancer diagnosis; ≥1 year from completion of cancer therapy (excluding chemopreventative agents); willing to complete a yearly self-report survey of health outcomes; and be able to complete forms independently in English. The cancer center’s Institutional Review Board approved the study. Informed consent was obtained from each participant or participant’s guardian with accompanying assent prior to study enrollment.
For this analysis, participants were drawn from a REACH cohort followed in a survivorship clinic providing long-term care to CCS diagnosed with hematological malignancies and solid tumors (survivors of CNS tumors who are followed in a neuro-oncology outcomes clinic are being evaluated in a separate study). Study participants were ages 12–49 years.
Measures
Demographic and medical information
Participants provided information regarding their age, gender, ethnicity, and current health problems directly on study forms. Additional medical information regarding cancer diagnosis, treatment modality, age at diagnosis, and time since diagnosis, was obtained from medical records.
Pediatric quality of life multidimensional fatigue scale
The multidimensional fatigue scale (MFS) measures self-reported fatigue symptoms with 18 items which are scored to produce an overall MDF [14–16]. Subscale scores are available, however, were not used in this evaluation. Each item is rated on a five-point Likert scale ranging from “not at all” to “always”. Higher scores indicate better functioning (i.e., less fatigue). While initially developed for use within a child and adolescent population, the MFS has been shown to be a reliable and valid measure in the young adult (ages 18–25) and middle adult (ages 26–53) pediatric cancer survivor populations [15, 16]. Though no established MFS cutoff score exists to identify clinically significant fatigue, prior studies have reported mean and standard deviation of MFS scores in healthy community samples that allow for comparison of our survivor sample with these normative groups [14–16].
Pediatric quality of life measurement model generic core scale
The 23-item pediatric quality of life measurement model (PedsQL) generic core scale comprises four multidimensional scales: physical, emotional, social, and school/work functioning (work was added to the school items for the PedsQL used in participants >18 years) [14–16]. Each item is rated on a five-point Likert scale ranging from “not at all” to “always.” Higher scores indicate better functioning. The PedsQL has been shown to be a reliable and valid measure in the adult population, including adult pediatric cancer survivors [15, 16].
Brief symptom inventory-18 depression scale
The brief symptom inventory-18 (BSI-18) is an 18-item self-report checklist designed to evaluate psychological distress in adults and was used to measure symptoms of depression in study participants ≥18 years [17]. This scale has been used to measure psychological symptoms in a variety of psychiatric and medical populations including young adult and adult cancer populations [18, 19]. The six BSI-18 depression items were scored following the published manual to yield gender-specific t scores based on a community sample. Participants with a t score ≥63 on the depression subscale were characterized as severely depressed. [17].
The Beck youth inventories depression subscale (BYI-D)
A 20-item self-report checklist used to assess symptoms of depression in study participants < age 18 years [20]. Each Beck youth inventories depression subscale (BYI-D) item asks participants to rank how frequently a statement has been true for them on a 4-point scale over the prior two weeks. The BYI is modular in nature and each 20-item subscale can be administered separately or together with other subscales. For this study, only the depression subscale was utilized. The BYI-D Cronbach’s alpha coefficients range from 0.86–0.96 demonstrating strong internal consistency, and the instrument has been validated in comparison with previously developed symptom report scales [20]. The BYI-D was used to assess depression in study participants aged 12–17 years. Participants were classified as depressed if they had a t score ≥63.
Statistical analysis
We calculated descriptive statistics to characterize the sample’s demographic, medical, and mental health characteristics. As noted, there is no established MFS cutoff score used to define clinically significant fatigue. However, studies using the MFS in community-based samples of adolescents and adults [14–16] reported means and standard deviations which we used as the basis of comparison with our survivor sample. Specifically, each survivor’s MFS score was compared to the mean and standard deviation available for a community sample of similar age (<18 years, 18 to <26 years, and 26+ years). The proportion of survivors observed to have scores ≥1 standard deviation below the mean for their age group was compared to the proportion expected based on the community data (16 %) using a z test.
Though using age-specific means and standard deviations are useful for comparing our sample with prior reports from non-cancer groups, they are not appropriate for comparing fatigued and non-fatigued survivors within our sample. This is because fatigue has been shown to be associated with age [8] so that young survivors who are one SD below their age-appropriate mean MFS scores may have little clinically significant fatigue, whereas older survivors may have very significant fatigue even though they are not in the most fatigued 16 % of their age group. For analyses of fatigued vs. non-fatigued survivors in our cohort, we required a classification that would be consistent across age groups; therefore, we classified survivors in the lowest quintile (most fatigued 20 %) of our sample as fatigued and compared them to all other survivors. To confirm that survivors classified as fatigued in this way differed from the other survivors, we compared the two groups on three MFS items we posited to reflect clinically significant aspects of fatigue using a z test. Subsequently, we compared the fatigued and non-fatigued survivors using univariate logistic regression models and odds ratios (OR) to identify significant correlates of fatigue.
We then constructed a multivariable model to identify demographic, cancer-related and health outcome variables independently associated with fatigue. Significant variables in the univariate models (p < .05) as well as gender (shown to be a significant fatigue correlate in prior studies [8] were initially placed in the model. Using a backward selection procedure nonsignificant variables (p > 0.05) were removed unless they increased or decreased a beta coefficient of another model variable by more than 10 %, in which case they were retained as likely confounders. Quality of life and mental health variables were not included in the multivariable modeling due to the complex relationships between these variables. Instead, we performed independent analyses to describe potential differences in quality of life (PedsQL) and depression (BSI-18 and BYI-D) in fatigued and non-fatigued survivors using t tests and univariate logistic regression. Data analyses were conducted using Statistical Package for Social Sciences (SPSS) statistical software (Windows Version 17.0), and all statistical tests were two-sided.
Results
Study population
During the study period, 301 potentially eligible childhood cancer survivors were asked to complete the measures reported in here; 268 completed these measures and are included in this analysis (89 % response rate). The 268 participants (129 male; 139 female) had a median age of 21.4 years and median age at diagnosis of 6.4 years (Table 1). Over 90 % were <40 years at time of study and 44 % were between the ages of 12 and 20 years. Mean time since diagnosis was 13.1 years (range 2–46 years). The primary cancer diagnoses included leukemia (35.1 %), lymphoma (24.3 %), bone tumor (9.3 %), and other solid tumors (31.3 %).
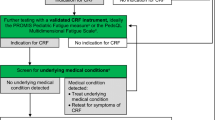
Description of fatigue in the sample
Based on comparison with published data for the MSF in community samples, 37 survivors (13.8 %) were considered fatigued (MDF score ≥1 standard deviation below means for non-cancer patients of similar age) which is not statistically different from the 16 % (43 cases) that would have been expected based on community sample data [15, 16, 14] for the MFS (z = −0.727, p = 0.467). As described, study participants in the lowest quintile on the MFS were classified as fatigued and compared to all other “non-fatigued” survivors for all further analyses. A significantly larger proportion of participants classified as fatigued reported that they often/almost always “felt tired” (52 vs. 2 %, p < 0.001), sometimes/often/almost always, “felt too tired to do things that they like to do,” (65 vs. 4 %, p < 0.001), and sometimes/often/almost always “felt too tired to spend time with friends,” (44 vs. 1 %, p < 0.001) (Table 2). These results support the selection of the 20 % of participants with the lowest scores on the MSF as a clinically fatigued sample for further analysis.
Comparison of fatigued and non-fatigued survivors
Univariate logistic regression analyses
The results of the univariate analysis show demographic factors positively associated with fatigue include age at participation (p = 0.001) and household income (p = 0.03) (Table 1). Fatigue was associated with increased age, with fatigued survivors being more commonly found in the 30–39 years (OR 2.86, 95 % CI 1.19–6.89) and 40–49 years (OR 4.58, 95 % CI 1.48–14.17) age groups. While fatigue was significantly associated with an annual family income of $50,000–99,000 (OR 2.65, 95 % CI 1.29–5.46), there was no apparent directionality to this relationship, as fatigue did not appear to be associated with increasing or decreasing income. Fatigue was not associated with gender or ethnicity. Time since diagnosis was associated with fatigue status (p = 0.02) with being 30 or more years out from treatment completion significantly associated with fatigue (OR 4.69, 95 % CI 1.65–13.29). No significant associations were found between fatigue and any other treatment-related variables (i.e., cancer diagnosis, age at diagnosis, disease recurrence or any of the treatment exposure variables). However, fatigue was significantly associated with chronic health conditions with fatigued survivors being six times more likely to report having three or more chronic health conditions compared to non-fatigued survivors (OR 6.13, 95 % CI 2.62–14.37).
Multivariate logistic regression analyses for fatigue
The multivariable logistic regression model with the variables’ current age, time since diagnosis, income, number of chronic conditions, and gender (Table 3) found the only variable significant in the final model was the presence of three or more chronic conditions (OR 4.27, 95 % CI 1.52–11.99). To explore this association further, we used univariate logistic regression to examine how chronic medical conditions were associated with age and fatigue status. The number of chronic conditions reported increased with participant age. The mean age of participants with no chronic conditions was 20.3 years (sd = 6.4), with 1–2 chronic conditions 23.7 years (sd = 9.6), and with ≥3 chronic conditions 32.3 years (sd = 10.0). Specific participant-reported conditions significantly associated with fatigue status included cardiac conditions, hepatitis, gallstones, liver condition, migraines, and thyroid problems (Table 4).
Fatigue, Mental health and Quality of Life
To examine how quality of life and depression differ between fatigued and non-fatigued participants we compared the PedsQL psychosocial health summary and global core scores. (Table 5). There was a significant difference between fatigued and non-fatigued participants with fatigued patients reporting lower psychosocial health summary (OR 0.87, 95 % CI 0.84–0.90) and global core scores (OR 0.86, 95 % CI 0.82–0.89). Fatigued participants also reported significantly lower scores across each of the subscales (physical function, emotional function, social function, school/work function, and psychosocial health summary (p < 0.001). These findings suggest that fatigued survivors are more likely to experience decreased quality of life compared to non-fatigued survivors. While fatigued survivors demonstrate significantly more depression compared to non-fatigued patients (20.4 vs. 1.4 %, respectively, with p < 0.0001); it is notable that 76 % of survivors with fatigue were not elevated on the BSI-18 depression scale, suggesting that other factors not measured in this study likely contribute to fatigue status.
Discussion
Our study found that the prevalence of fatigue in our CCS sample is not significantly different from age-matched community sample data. While these results stand in contrast to studies that have reported increased fatigue in CCS [9], they fall in line with those showing fatigue prevalence concordant with control populations [10, 11]. For example, the Childhood Cancer Survivor Study (CCSS) looked at 1897 adult survivors (over 18 years) and found they have increased fatigue compared to sibling-matched controls [9]. However, a Dutch study of 416 CCS ages 16–49 years with variable primary cancer diagnoses and an American study looking at 161survivors of acute lymphoblastic leukemia ages 18–41 years each showed no significant difference in fatigue prevalence in CCS vs. control populations. [10, 11].
Where most prior studies of fatigue after childhood cancer have focused on survivors well into adulthood [9–11, 21], our study sample included many adolescents. In fact, 44 % of our sample participants fell between the ages of 12 and 19 years, adding a unique perspective to this work and the opportunity to characterize fatigue in the adolescent age group. Only one prior study has examined the role of fatigue in adolescent CCS (≤17 years) and, like our study, did not find increased fatigue compared to population-matched controls [22]. It is possible that our study did not find significant fatigue in CCS given the younger age of the study population. This seems particularly plausible since fatigue is associated with increased age in our sample on univariate statistics suggesting that fatigue in our CCS cohort may emerge in later adulthood.
Consistent with previous reports [9, 23], fatigue was not associated with disease-related factors. In addition, we found no association between fatigue and treatment factors. Over the past few decades, there has been a significant evolution in pediatric cancer treatment so that today many therapeutic regimens aim to both treat disease and mitigate late effects by reducing chemotherapy and radiation exposure. For example, recognition of significant cardiac morbidity secondary to anthracyclines led to changes in therapeutic regimens that reduce the likelihood of congestive heart failure which can result in debilitating fatigue. [25] Patients treated more recently, such as the younger participants in our study population, with more than 90 % treated since 1990, could have a different late-effect profile compared to earlier studies (i.e., CCSS sample treated between 1970 and 1986), as suggested in survivorship research. [24].
We found the presence of three or more chronic conditions to be significantly associated with fatigue. These results are consistent with similar findings in an older CCS population where fatigue status was associated with the presence of chronic conditions/late effects [10]. The number of chronic conditions per participant trended towards increasing with age, suggesting that the full impact of treatment late effects, including fatigue, may not be fully realized in our young population. While our results show a significant relationship between increased number of chronic conditions and age, age itself was not significantly associated with fatigue on multivariable analysis as seen in earlier studies. [10, 11] This suggests that adjusting for chronic conditions in the final model likely attenuates the age effect. While prior research has established that CCS carry an increased risk for the development of chronic conditions compared to the general population, these older data reflect CCS more intensely treated compared to many current regimens [26]. It is quite possible that our cohort of more recently treated patients will develop fewer chronic conditions and less fatigue compared to the CCSS group even as they age. The question of increased risk for chronic conditions will be assessed through ongoing analysis of our CCS cohort.
Consistent with previous reports, we found a strong association between fatigue and depression [9, 11, 27, 28]. The cross-sectional analysis performed creates a challenge in examining the relationship between depression and fatigue given its bi-directional nature and variable manifestations in individual people. Recognition of this relationship should prompt providers caring for CCS to incorporate appropriate psychosocial evaluation and care in patients reporting fatigue. Important to recognize is that a notable number of participants identified as fatigued were not depressed. This is critical to our understanding of fatigue in this population as it highlights both the relationship between fatigue and depression as well as the important distinction between the two conditions. Our findings also support an association between fatigue and decreased quality of life. The fatigued survivors’ physical and mental health scores were significantly lower compared to non-fatigued survivors across all sub-domains of the PedsQL. This is consistent with findings in similar studies [11, 29], and indicates that fatigued survivors are experiencing impairment across a full range of quality of life domains. Therefore, while we found that fatigue is not more prevalent in CCS compared to same-age peers, the fact that survivors with fatigue have increased risk for poor QOL and mental health problems suggests we should focus on identifying fatigued CCS and providing appropriate intervention when possible.
The study has several limitations including a study population drawn from a single clinical site with a specialized childhood cancer survivorship program and the lack of a control group. For myriad reasons, not all CCS engage in survivorship care, and a study population comprised of only CCS that do may not accurately reflect the role of fatigue in the general CCS population. While we used a validated self-report measure of fatigue, there is no generally accepted cutoff for the measure to indicate clinically significant fatigue, which would have facilitated the categorization of fatigue experienced by survivors into clinical context. Nonetheless, our approach enabled us to make a general comparison of fatigue prevalence between our study population and normative data, as well as identify a group of participants most likely to demonstrate clinically significant fatigue and compare them against non-fatigued survivors to better understand potential predictors of fatigue in the survivorship population. Future studies should explore clinical performance to more accurately assess fatigue and impact on daily function. The small numbers in our study and the limitations of self-reported data restricted our ability to identify significant relationships between fatigue and specific chronic conditions; however, exploratory analyses suggest fatigue is associated with cardiac conditions, liver conditions, migraines, and thyroid problems, which have been previously described [11]. These relationships are speculatory in nature, and highlight the need for future research to better understand the connections between fatigue and specific chronic conditions in CCS.
Despite these limitations, our findings that a cohort of adolescent and predominantly young adult CCS does not demonstrate increased fatigue compared to healthy peers of similar age are reassuring. The most optimistic interpretation of the results would suggest that with improvement in cancer therapy, CCS will be spared many late effects; including fatigue and the potential impact clinically significant fatigue may have on adolescent and adult physical and psychological health. Unlike prior research, our study includes a substantial adolescent and young adult population. Given the unique developmental stages of adolescence and young adulthood, a time period in which young people begin to set the course for their personal and professional lives and make life decisions with enduring ramifications, fatigue may potentiate particularly serious consequences. [12] However, it remains too early to make definitive conclusions as these data may also represent an early snapshot of a high-risk group with potential to develop fatigue over time. Longitudinal studies currently underway will help us better understand the relationship between fatigue and specific chronic conditions, thereby facilitating early identification of those individuals most at risk.
References
Mariotto AB, Rowland JH, Yabroff KR, Scoppa S, Hachey M, Ries L, Feuer EJ (2009) Long-term survivors of childhood cancers in the United States. Cancer Epidemiol Biomark Prev 18:1033–1040
Hudson MM, Ness KK, Gurney JG, Mulrooney DA, Chemaitilly W, Krull KR, Green DM, Armstrong GT, Nottage KA, Jones KE, Sklar CA, Srivvastave DK, Robison LL (2013) Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 309:2371–2381
Armstrong GT, Kawashima T, Leisenring W, Stratton K, Stovall M, Hudson MM, Sklar CA, Robison LL, Oeffinger KC (2014) Aging and risk of severe, disabling, life-threatening, and fatal events in the childhood cancer survivor study. J Clin Oncol 32:1218–1227
Vogelzang NJ, Breitbart W, Cella D, Curt GA, Groopman JE, Horning SJ, Itri LM, Johnson DH, Scherr SL, Portenoy RK (1997) Patient, caregiver, and oncologist perceptions of cancer-related fatigue: results of a tripart assessment survey. Semin Hematol 34:4–12
Andrykowski MA, Curran SL, Lightner R (1998) Off-treatment fatigue in breast cancer survivors: a controlled comparison. J Behav Med 21:1–18
Loge JH, Abrahamsen AF, Ekeberg Ø, Kaasa S (1999) Hodgkin’s disease survivors more fatigued than the general population. J Clin Oncol 17:253–261
Calaminus G, Dörffel W, Baust K, Teske C, Riepenhausen M, Brämswig J, Flechtner H-H, Singer S, Hinz A, Schellong G (2014) Quality of life in long-term survivors following treatment for Hodgkin’s disease during childhood and adolescence in the German multicentre studies between 1978 and 2002. Support Care Cancer 22:1519–1529
Jóhannsdóttir IMR, Hjermstad MJ, Moum T, Wesenberg F, Hjorth L, Schroder H, Mort S, Jonmundsson G, Loge JH (2012) Increased prevalence of chronic fatigue among survivors of childhood cancers : a population-based study. Pediatr Blood Cancer 58:415–420
Mulrooney DA, Ness KK, Neglia JP, Whitton JA, Green DM, Zeltzer LK, Robison LL, Mertens AC (2008) Fatigue and sleep disturbance in adult survivors of childhood cancer: a report from the childhood cancer survivor study (CCSS). Sleep 31:271–281
Langeveld NE, Grootenhuis M a, Voûte P a, de Haan RJ, van den Bos C (2003) No excess fatigue in young adult survivors of childhood cancer. Eur J Cancer 39:204–214.
Meeske KA, Siegel SE, Globe DR, Mack WJ, Bernstein L (2005) Prevalence and correlates of fatigue in long-term survivors of childhood leukemia. J Clin Oncol 23:5501–5510
Arnett JJ (2000) Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol 55:469–480
Bober SL, Zhou ES, Chen B, Manley PE, Kenney LB, Recklitis CJ (2013) Sexual function in childhood cancer survivors: a report from project REACH. J Sex Med 10:2084–2093
Varni JW, Ph D, Burwinkle TM, Katz ER, Meeske K, Dickinson P, Pedsql T (2002) The PedsQL ™ in pediatric cancer reliability and validity of the pediatric quality of life inventory ™ generic Core. Cancer 94:2090–2106
Varni JW, Limbers CA (2008) The PedsQL multidimensional fatigue scale in young adults: feasibility, reliability and validity in a university student population. Qual Life Res 17:105–114
Robert RS, Paxton RJ, Palla SL, Yang G, Askins M, Joy SE, Ater JL (2012) Feasibility, reliability, and validity of the pediatric quality of life inventory generic Core Scales, cancer module, and multidimensional fatigue scale in long-term adult survivors of pediatric cancer. Pediatr Blood Cancer 59:703–707
Derogatis L (2000) BSI 18: brief symptom inventory 18. National Computer Systems, Inc., Minneapolis
Zabora J, Brintzenhofseszoc K, Jacobsen P, Curbow B, Piantadosi S, Hooker C, Owens A, Derogatis L (2001) A new psychosocial screening instrument for use with cancer patients. Psychosomatics 42:241–246
Recklitis CJ, Parsons SK, Shih M-C, Mertens A, Robison LL, Zeltzer L (2006) Factor structure of the brief symptom inventory-18 in adult survivors of childhood cancer: results from the childhood cancer survivor study. Psychol Assess 18:22–32
Beck JS, Beck AT, Jolly JB, Steer RA (2005) Manual for Beck youth inventories, second edi. Harcourt Assessment, Oxford
Kenney LB, Nancarrow CM, Najita J, Vrooman LM, Rothwell M, Recklitis C, Li FP, Diller L (2010) Health status of the oldest adult survivors of cancer during childhood. Cancer 116:497–505
Gordijn MS, van Litsenburg RR, Gemke RJ, Huisman J, Bierings MB, Hoogerbrugge PM, Kaspers GJL (2013) Sleep, fatigue, depression, and quality of life in survivors of childhood acute lymphoblastic leukemia. Pediatr Blood Cancer 60:479–485
Langeveld NE, Stam H, Grootenhuis M, Last BF (2002) Quality of life in young adult survivors of childhood cancer. Support Care Cancer 10:579–600
Armstrong GT, Pan Z, Ness KK, Srivastava D, Robison LL (2010) Temporal trends in cause-specific late mortality among 5-year survivors of childhood cancer. J Clin Oncol 28:1224–1231
Krischer JP, Epstein S, Cuthbertson DD, Goorin AM, Epstein ML, Lipshultz SE (1997) Clinical cardiotoxicity following anthracycline treatment for childhood cancer: the pediatric oncology group experience. J Clin Oncol 15:1544–1552
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, Friedman DL, Marina N, Hobbie W, Kaden-Lottick NS, Schwartz CL, Leisenring W, Robison LL (2006) Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355:1572–1582
Visser MR, Smets EM (1998) Fatigue, depression and quality of life in cancer patients: how are they related? Support Care Cancer 6:101–108
Kanellopoulos A, Hamre HM, Dahl AA, Ruud E, Fossa SD (2013) Factors associated with poor quality of life in survivors of childhood acute lymphoblastic leukemia and lymphoma. Pediatr Blood Cancer 60(5):849–855
Clanton NR, Klosky JL, Li C, Jain N, Srivastava DK, Mulrooney D, Zeltzer L, Stovall M, Robison LL, Krull KR (2011) Fatigue, vitality, sleep, and neurocognitive functioning in adult survivors of childhood cancer: a report from the childhood cancer survivor study. Cancer 117:2559–2568
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Frederick, N.N., Kenney, L., Vrooman, L. et al. Fatigue in adolescent and adult survivors of non-CNS childhood cancer: a report from project REACH. Support Care Cancer 24, 3951–3959 (2016). https://doi.org/10.1007/s00520-016-3230-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3230-2