Abstract
Background
Fatigue and sleep problems are prevalent in cancer patients and can be associated with disruption of circadian rhythmicity. In this prospective phase II trial, we sought to assess the effect of melatonin on circadian biomarkers, sleep, and quality of life in breast cancer patients.
Methods
Thirty-two patients with metastatic breast cancer, receiving hormonal or trastuzumab therapy, took 5 mg of melatonin at bedtime for 2 months. Before starting and after 2 months on melatonin therapy, sleep and circadian rhythmicity were assessed by actigraphy, diurnal patterns of serum cortisol, and the expression of the core clock genes PER2 and BMAL1 in peripheral blood mononuclear cells. The European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 questionnaire was completed for subjective parameters.
Results
Bedtime melatonin was associated with a significant improvement in a marker of objective sleep quality, sleep fragmentation and quantity, subjective sleep, fatigue severity, global quality of life, and social and cognitive functioning scales. Morning clock gene expression was increased following bedtime melatonin intake. Melatonin did not affect actigraphy measure of circadian rhythmicity, or the diurnal cortisol pattern.
Conclusion
These results invite further investigation of melatonin as a potentially useful therapeutic agent for improving sleep and quality of life in cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fatigue and sleep problems are among the most prevalent complaints of cancer patients. Their incidence has been reported to be as high as 90 and 80 %, respectively [1]. While these symptoms frequently co-occur, their etiology is multifactorial and poorly understood [2]. The available therapeutic options remain limited [3].
Circadian rhythms control a variety of behavioral (including sleep) and physiological processes in living systems ranging from bacteria to man [4]. The suprachiasmatic nuclei (SCN) of the anterior hypothalamus are the site of the circadian pacemaker in mammals. The SCN are synchronized to geophysical time by photic signals from the retina and drive rhythmic behavior and physiology in extraneural organs through rhythmic temperature and humoral and neural signals. The circadian expression of core clock genes in the SCN and their interactions in transcriptional networks are at the core of the SCN clock network and impact the synchronized rhythmic expression of clock genes in peripheral organs. These peripheral tissue clocks in turn control rhythms in cellular physiology and metabolism including xenobiotic detoxification, glucose homeostasis, and lipid metabolism [5].
A disruption of circadian rhythmicity has been associated with several human disease states including cancer [6, 7]. A meta-analysis of 13 studies that examined cancer risk among female shift workers and cabin crew found a 48 % increase in the relative risk of breast cancer [8]. The International Agency for Research on Cancer (IARC) has classified shift work, involving circadian disruption, as probably carcinogenic to humans. This designation was mainly based on the experimental and epidemiologic evidence for circadian disruption and breast cancer and prompted a panel of experts to suggest preventive measures [9].
Circadian disruption is associated with faster tumor progression and shorter survival in tumor-bearing rodents [10, 11]. In one study, this was reversed by melatonin therapy [12]. Circadian disruption is common in cancer patients and can contribute to both fatigue and sleep problems [2, 7, 13, 14]. The bidirectional connections of the circadian system with multiple biological and physiological functions make it sensitive to disturbances caused by the cancer itself and anticancer therapy [4, 7]. Circadian disruption has been associated with more severe systemic symptoms, poorer quality of life, and shorter overall survival in patients with breast, colon, lung, kidney, and ovary cancer [2, 15–21]. In healthy individuals, cortisol levels have a circadian rhythm—high in the morning and low at night. Abnormalities in the diurnal cortisol rhythm are common in cancer patients and have been associated with poorer survival in breast cancer patients [17].
These observations in rodents and cancer patients raise the possibility that a reversal of circadian disruption could lessen systemic symptoms, improve quality of life, and even improve patient outcomes. Melatonin is safe and commonly used to reset the circadian timing system in subjects with circadian disruption [22]. Melatonin is secreted by the pineal gland in a circadian pattern with high values during the night, peaking early in the morning, and low values during the day. When humans are exposed to light, neural input from the SCN inhibits pineal activity and thus melatonin synthesis. The normal diurnal rhythm of melatonin secretion is disrupted in cancer patients, usually with a dampened difference between daytime and nighttime values [23, 24].
The use of exogenous melatonin in the oncology setting is relatively unexplored. Lissoni has performed several small clinical trials in which melatonin therapy was associated with reduced toxicity from cancer therapy, improved quality of life, improved response rates, and longer survival [25]. However, these clinical studies included a small sample size and did not document the effect of melatonin on the circadian timing system at either the physiological or the molecular level.
We hypothesized that melatonin therapy could improve circadian disruption in breast cancer patients. To test this hypothesis, we conducted a prospective phase II trial to assess the impact of bedtime melatonin on sleep and circadian rhythmicity, assessed objectively by actigraphy, diurnal patterns of serum cortisol, and clock gene expression, and subjectively by a quality of life questionnaire.
Materials and methods
Study design
This was an open-label phase II trial assessing the efficacy of melatonin 5 mg (N-acetyl-5-methoxytryptamine, supplied by Circa Dia BV, Amsterdam, Netherlands) taken orally at each patient’s usual bedtime for 2 months. The trial was based on a repeated-measures design, with each patient being her own control. Eligible patients had histologically proven metastatic breast cancer with stable disease receiving either no systemic treatment, bisphosphonates, hormonal therapy (tamoxifen, aromatase inhibitors, or progestins), or trastuzumab. Patients doing shift work and taking steroids or beta blockers and those with ECOG performance status >2 were excluded from study. The Ethics Review Board at Sunnybrook Health Sciences Centre approved the study, and all patients signed informed consent. Staging radiological investigations were done at baseline and after 2 months on melatonin. For patients with bone metastases only, plain X-rays, carcino-embyonic antigen (CEA), and alkaline phosphatase were done to assess disease status. Toxicity was graded according to NCI Common Terminology Criteria for Adverse Events version 3. Patients were taken off the study if there was clinical or radiological evidence of progression of disease before the end of the 2-month study period or at the patient request. Patients completed the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 v3.0 questionnaire before wearing the actigraph at baseline and after 2 months of melatonin treatment. Scores were calculated using the recommended EORTC procedures. Higher values for domains indicate better functioning, while higher scores for symptoms reflect more severe complaints.
Assessment of sleep and circadian rhythmicity
A Basic-Motionlogger actigraph (Ambulatory Monitoring Inc., Ardsley, NY, USA) was used to assess individual rest-activity patterns before and after treatment with melatonin [26]. This watch-sized device, worn on the non-dominant wrist, contains a piezoelectric linear accelerometer to detect wrist movements and a memory chip for data storage. The actigraph was worn for at least 4 days before starting melatonin therapy, and again during the last week of the 2-month course of melatonin. The actigraphy time series were analyzed for several validated parameters using software provided by the manufacturer (Action 4 and AW2, Ambulatory Monitoring Inc.) and using previously described algorithms implemented in MATLAB (MathWorks, Natick, MA) [27]. The primary endpoints included a circadian parameter, autocorrelation coefficient at 24 h (r24), and a sleep parameter (pRA). The circadian parameter r24 is a measure of the regularity and reproducibility of the activity pattern over a 24-h period from one day to the next, and reaches 1 in subjects with a robust circadian pattern [16, 28, 29]. The sleep metric pRA is a probabilistic measure of sleep fragmentation with higher values representing sleep fragmentation and lower values representing more consolidated sleep. In brief, pRA estimates the probability of arousal (as indicated by movement) per 15-s period of sleep (as indicated by sustained rest).
Nine other parameters were calculated: three estimating the circadian rest-activity pattern (dichotomy index, I<O [29]; intraday variability, IV; and interday stability, IS [30]), one estimating sleep (sleep fragmentation index, SFI [31]), and five related to physical activity (average activity counts; average duration of rest; a probabilistic metric of activity fragmentation, pAR that is analogous to pRA [27]; average activity during 6 most active hours, M6; and during 6 least active hours, L6). Finally, the actigraph provided two estimates of the phase of the activity pattern using a cosine regression (acrophase) or a non-parametric analysis of the average clock time of the midpoint of the eight most active hours of each day (M8) [32]. Patients kept record of their sleeping and waking times in a diary during the actigraphy periods [26].
Blood was obtained at 08:00 and at 16:00, at baseline, and after 2 months of melatonin therapy, for serum cortisol measurements (performed at Hospital Biochemical laboratory) and to measure the relative expression of the core clock genes hPer2 and hBmal1 in peripheral blood mononuclear cells (PBMCc). The cortisol rhythm can be accurately described by sampling two times per day [33]. In healthy volunteers, hPer2 peaks at about 06:00 and hBmal1 peaks at around 14:00 [34].
PBMCs were separated from whole blood by centrifugation, and total RNA extracted using TRIzol (Life Technology, Inc.). Before a real-time PCR reaction, genomic DNA was eliminated using the Genomic DNA elimination reaction kit (Qiagen). Real-time polymerase chain reaction (PCR) was performed, using the Applied Biosystems ABI7000 sequence detection system (Applied Biosystems, Foster City, CA). First, total RNA was extracted (Quantiscript Reverse Transcriptase with RNase inhibitor) and incubated for 15 min at 42 °C to generate complementary DNA (cDNA). Then, the cDNA product was amplified with one cycle at 95 °C for 15 min, followed by 45 cycles of denaturation at 94 °C for 15 s, elongation at 55 °C for 30 s, and annealing at 72 °C for 30 s, followed by the routine dissociation protocol at 60 °C. Standard curves were run at cDNA twofold series dilution on each plate to check efficiency. All data was standardized to the reference gene GAPDH. Primers, designed using Primer Express software (Applied Biosystems) and purchased through ACGT Corp (Toronto, Ontario, Canada), were the following: GAPDH forward, TGGGCTACACTGAGCACCAG, and reverse, GGGTGTCGCTGTTGAAGTCA; hPER2 forward, ACTCAGCGAAGTGTCGGACAC, and reverse, TTCGATCCTGTGATTCAAGGG; and hBMAL1 forward, GCCGAATGATTGCTGAGGAA, and reverse, GGCGATGACCCTCTTATCCTG.
Statistical analyses
The primary endpoints were the within-patient changes in the circadian parameter r24 and in the sleep parameter pRA at baseline versus after 2 months on melatonin. The sample size required to detect a clinically meaningful difference in r24 (the interquartile range) with a two-sided alpha error of 0.05 and a power of 90 % was 31 analyzable patients. This was based on the distribution of this parameter in patients with metastatic breast [28] and colorectal cancer [29]. Secondary endpoints included changes in other actigraphy parameters, in quality of life scales, and in the ratio of morning/afternoon cortisol and clock gene expression. Descriptive statistics were calculated, and two-sided paired-samples t tests were used for comparisons between baseline and after treatment. The threshold for statistical significance was set at p < 0.025 for the primary endpoints, following a Bonferroni correction for multiple testing. Two-sided Spearman’s rank correlations were computed for cortisol and clock gene data. Given the exploratory nature of secondary analyses, the threshold for statistical significance was set at p < 0.05. All analyses were performed using SPSS 16 software (SPSS Inc., IL, USA).
Results
Study sample
Forty-one patients were enrolled. Of those, 32 (78 %) completed the study and provided valid actigraphy data. There was one male patient. Nine patients were not included in the analyses due to surgery unrelated to breast cancer (n = 1), actigraphy file unreadable (n = 3), melatonin stopped too early (n = 2), not eligibility for study (n = 1), progressed and started chemotherapy before the second assessment (n = 1), and withdrew from study (n = 1). Some parameters could be calculated only in a smaller number of recordings due to technical issues.
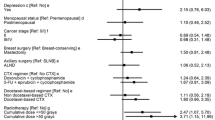
The clinical and demographic features of the study sample (n = 32) are summarized in Table 1. Patients experienced no melatonin-related toxicity during the 2 months on study.
Actigraphy recordings
Patients wore the actigraph for an average of 115 h (SD, 29 h) at baseline and 105 h (SD, 35 h) after melatonin treatment. The median interval between recordings was 59 days (range, 50 to 84).
There was no significant difference in the distribution of the circadian parameter r24 before and after treatment with melatonin (p = 0.11, Fig. 1a). The mean difference in r24 values was −0.06, ranging between −0.58 and 0.37. Twelve patients (37.5 %) improved their r24 after having taken melatonin. In contrast, overall sleep fragmentation measured by pRA was significantly reduced after treatment with melatonin (p = 0.0015; Fig. 1b). This represents a 40 % relative reduction in pRA (Fig. 1b).
Significant post-treatment differences were observed for L6 (Fig. 2c), pAR (Fig. 2i), SFI (Fig. 2h), and for the total duration of rest (Fig. 2g). The relative changes in these four parameters, decrease in the first three and increase in the fourth, indicate an improvement in rest quality and duration. Conversely, the circadian parameters (IS, IV, and I<O, see Fig. 2d–f) and overall-activity-related parameter (mean daily activity and M6, see Fig. 2a and 2b) did not show significant changes. Melatonin did not modify the phase of the activity pattern, as indicated by the timing of the activity acrophases calculated with the cosinor (Fig. 3a) or M8 (Fig. 3b) methods for all patients (p = 0.52 and p = 0.18, respectively). Nonetheless, phase shifts (both delays or advances) up to 5 h were observed in some patients (Fig. 3a, b).
Quality of life
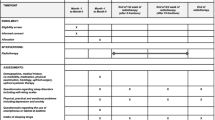
Melatonin treatment was associated with a significant improvement in global quality of life, social and cognitive functioning domains (Fig. 4), and self-rated sleep disturbance and fatigue (Fig. 4). A clinically relevant increase (i.e., ≥10 points [35]) of global quality of life was reported by 35.7 % of the patients, whereas 39.5 % of patients reported significant increase in social and cognitive functions. Clinically meaningful decreases (i.e., ≤10 points [35]) in sleep disturbance and fatigue occurred in 50.0 and 47.4 % of patients, respectively. The remaining domains and symptoms, including appetite, showed no significant change (Fig. 4).
Effect of melatonin on subjective health-related quality of life. Mean ± SEM of the domains (top: higher values indicate better functioning) or symptoms (bottom: higher values indicate more severe complaint) assessed using the EORTC QLQ-C30 v3.0 questionnaire before (white boxes) and after (gray boxes) melatonin treatment. N = 22. Only results with p ≤ 0.05 are tagged. NS, not significant
Cortisol and clock genes
Treatment with melatonin did not affect average morning/afternoon differences in cortisol patterns (p = 0.89), with normal significantly higher values in the morning compared to afternoon both at baseline and after melatonin (both p < 0.0001; Fig. 5). At baseline, the relative expression of hPer2 did not differ between morning and afternoon (p = 0.41), whereas, following melatonin treatment, hPer2 displayed significantly higher morning values (p < 0.0001; Fig. 5). Conversely, hBmal1 showed significantly higher afternoon values (p = 0.01) at baseline, and this difference was suppressed after melatonin (p = 0.91; Fig. 5). Thus, melatonin significantly increased morning expression of both hPer2 and hBmal1 (both p = 0.006), with no effect on afternoon expression (p = 0.96 for hPer2 and p = 0.94 for hBmal1; Fig. 5). hPer2 morning-to-afternoon changes following melatonin administration were significantly correlated to those of hBmal1 (r = 0.83; p < 0.0001).
Discussion
We report for the first time that daily bedtime melatonin therapy is associated with reduction in sleep fragmentation, increases in sleep duration, improvements in self-rated sleep quality (Figs. 1b, 2c, h, i, and 4), and improvement in global quality of life and pertinent social and cognitive domains, as well as reduction in fatigue severity (Fig. 4). These clinically important effects were obtained without any short-term toxicity.
The expression patterns of two core clock genes, hPer2 and hBmal1, in PBMC were modified [4, 34] (Fig. 5). The observed increase in morning expression of hPer2 after melatonin is consistent with an increase in the amplitude of circadian rhythmicity since hPer2 peaks early in the morning [34]. For hBmal1, an increase in the amplitude of circadian rhythmicity would have been expected to result in an increase in afternoon hBmal1 expression [34]. Our findings could reflect a melatonin-induced phase-shift in hBmal1 expression patterns. The effect of melatonin on hPer2 is intriguing since a germline polymorphism of this gene is associated with a higher risk of breast cancer [36], and its downregulation accelerates experimental breast cancer growth [37]. Altered expression of several other clock genes has been associated with breast cancer risk, recurrence rates, and prognosis [38].
We did not find any significant effects of melatonin on several objective circadian rest-activity parameters that have been extensively validated in various settings (r24, IS, IV, and I<O, see Figs. 1a and 2d–f respectively) [31]. This is consistent with the lack of any significant impact on the diurnal pattern of cortisol (Fig. 5). It is unknown whether a higher dose or longer treatment duration would have affected these circadian parameters. In agreement with our results, a double-blind placebo-controlled study reported no effect of a higher melatonin dose (20 mg for 4 weeks) on appetite in cancer patients with cachexia [39].
Our patients displayed a much more robust locomotor activity pattern at baseline than we have reported for patients with metastatic colorectal cancer [15, 16]. This may partly explain the lack of effect on objective circadian rest-activity parameters. In the current study, only 19.1 % of the patients had clinically important baseline circadian disruption, as estimated by the validated parameter I<O [15, 16] (Fig. 2f). This could lead to a ceiling effect, making it more difficult to demonstrate a beneficial effect of melatonin therapy. Similarly, two-point serum cortisol assessments indicated a normal diurnal pattern [33] at baseline (Fig. 5), confirming the relative robustness of the circadian system function of the patients enrolled. The values for baseline subjective sleep problems in our study were consistent with those observed in similar cancer populations [40]. We show for the first time that melatonin can lead to clinically relevant improvements in sleep parameters without significant changes in circadian actigraphy parameters, biochemical measures of circadian rhythmicity, or overall average physical activity.
The clinical correlates of sleep disturbances and circadian disruption in cancer patients include poor quality of life, altered physical, social, and cognitive functions, fatigue, and appetite loss [2, 13, 14, 16, 22]. Our findings, showing a concomitant improvement in sleep and several of these domains (Fig. 4), support the hypothesis of their shared mechanism [2].
The main limitation of our study is the lack of a blind allocation to a control arm, either a placebo or a different hypnotic or chronobiotic treatment. A placebo effect is unlikely in our study since we observed a significant improvement in objective sleep parameters, as well as a significant increase in the morning expression levels of two core clock genes.
Our findings support the use of melatonin as a safe and feasible intervention to improve sleep and quality of life in cancer patients. Randomized controlled trials are needed to compare melatonin therapy to placebo or to other interventions in order to establish its efficacy and to understand whether such interventions could improve survival. The possibility of a survival benefit from a therapy that improves circadian disruption is suggested by retrospective data showing that women with breast cancer who exercise have a 30 to 50 % lower risk of breast cancer recurrence and breast cancer death [41]. Both rodent and human data have shown that exercise can change the phase of the circadian rhythm [42, 43]. The benefit of routine exercise may therefore to some extent be related to its reversal of circadian disruption. The concept that re-synchronizing circadian rhythms might be associated with a survival benefit is further supported by studies in breast, colon, lung, kidney, and ovary cancer documenting shorter overall survival in patients with circadian disruption [2, 15–21].
Future studies might focus on breast cancer patients receiving chemotherapy given the high prevalence of circadian disruption, sleep problems, fatigue, and cognitive dysfunction in this group of patients [15, 44, 45]. Our results are encouraging for the continued development of therapeutic interventions to reverse circadian disruption in an effort to reduce systemic symptoms, improve quality of life, improve sleep, and possibly improve survival in patients with cancer.
References
Palesh OG, Roscoe JA, Mustian KM, Roth T, Savard J, Ancoli-Israel S, Heckler C, Purnell JQ, Janelsins MC, Morrow GR (2010) Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol 28(2):292–298
Innominato PF, Mormont MC, Rich TA, Waterhouse J, Levi FA, Bjarnason GA (2009) Circadian disruption, fatigue, and anorexia clustering in advanced cancer patients: implications for innovative therapeutic approaches. Integr Cancer Ther 8(4):361–370
Minton O, Richardson A, Sharpe M, Hotopf M, Stone P (2008) A systematic review and meta-analysis of the pharmacological treatment of cancer-related fatigue. J Natl Cancer Inst 100(16):1155–1166
Mohawk JA, Green CB, Takahashi JS (2012) Central and peripheral circadian clocks in mammals. Annu Rev Neurosci 35:445–462
Bass J (2012) Circadian topology of metabolism. Nature 491(7424):348–356
Scheer FA, Hilton MF, Mantzoros CS, Shea SA (2009) Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A 106(11):4453–4458
Innominato PF, Levi FA, Bjarnason GA (2010) Chronotherapy and the molecular clock: clinical implications in oncology. Adv Drug Deliv Rev 62(9–10):979–1001
Megdal SP, Kroenke CH, Laden F, Pukkala E, Schernhammer ES (2005) Night work and breast cancer risk: a systematic review and meta-analysis. Eur J Cancer 41(13):2023–2032
Bonde JP, Hansen J, Kolstad HA, Mikkelsen S, Olsen JH, Blask DE, Harma M, Kjuus H, de Koning HJ, Olsen J, Moller M, Schernhammer ES, Stevens RG, Akerstedt T (2012) Work at night and breast cancer—report on evidence-based options for preventive actions. Scand J Work Environ Health 38(4):380–390
Filipski E, King VM, Li X, Granda TG, Mormont MC, Liu X, Claustrat B, Hastings MH, Levi F (2002) Host circadian clock as a control point in tumor progression. J Natl Cancer Inst 94(9):690–697
Fu L, Pelicano H, Liu J, Huang P, Lee C (2002) The circadian gene Period2 plays an important role in tumor suppression and DNA damage response in vivo. Cell 111(1):41–50
Li JC, Xu F (1997) Influences of light–dark shifting on the immune system, tumor growth and life span of rats, mice and fruit flies as well as on the counteraction of melatonin. Biol Signals 6(2):77–89
Ancoli-Israel S, Liu L, Marler MR, Parker BA, Jones V, Sadler GR, Dimsdale J, Cohen-Zion M, Fiorentino L (2006) Fatigue, sleep, and circadian rhythms prior to chemotherapy for breast cancer. Support Care Cancer 14(3):201–209
Sephton S, Spiegel D (2003) Circadian disruption in cancer: a neuroendocrine-immune pathway from stress to disease? Brain Behav Immun 17(5):321–328
Innominato PF, Giacchetti S, Bjarnason GA, Focan C, Garufi C, Coudert B, Iacobelli S, Tampellini M, Durando X, Mormont MC, Waterhouse J, Levi FA (2012) Prediction of overall survival through circadian rest-activity monitoring during chemotherapy for metastatic colorectal cancer. Int J Cancer 131(11):2684–2692
Innominato PF, Focan C, Gorlia T, Moreau T, Garufi C, Waterhouse J, Giacchetti S, Coudert B, Iacobelli S, Genet D, Tampellini M, Chollet P, Lentz MA, Mormont MC, Levi F, Bjarnason GA (2009) Circadian rhythm in rest and activity: a biological correlate of quality of life and a predictor of survival in patients with metastatic colorectal cancer. Cancer Res 69(11):4700–4707
Sephton SE, Sapolsky RM, Kraemer HC, Spiegel D (2000) Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst 92(12):994–1000
Cohen L, Cole SW, Sood AK, Prinsloo S, Kirschbaum C, Arevalo JM, Jennings NB, Scott S, Vence L, Wei Q, Kentor D, Radvanyi L, Tannir N, Jonasch E, Tamboli P, Pisters L (2012) Depressive symptoms and cortisol rhythmicity predict survival in patients with renal cell carcinoma: role of inflammatory signaling. PLoS One 7(8), e42324
Sephton SE, Lush E, Dedert EA, Floyd AR, Rebholz WN, Dhabhar FS, Spiegel D, Salmon P (2013) Diurnal cortisol rhythm as a predictor of lung cancer survival. Brain Behav Immun 30:S163–170
Schrepf A, Thaker PH, Goodheart MJ, Bender D, Slavich GM, Dahmoush L, Penedo F, DeGeest K, Mendez L, Lubaroff DM, Cole SW, Sood AK, Lutgendorf SK (2015) Diurnal cortisol and survival in epithelial ovarian cancer. Psychoneuroendocrinology 53:256–267
Innominato PF, Roche VP, Palesh OG, Ulusakarya A, Spiegel D, Levi FA (2014) The circadian timing system in clinical oncology. Ann Med 46(4):191–207
Waterhouse J, Reilly T, Atkinson G, Edwards B (2007) Jet lag: trends and coping strategies. Lancet 369(9567):1117–1129
Mazzoccoli G, Carughi S, De Cata A, La Viola M, Vendemiale G (2005) Melatonin and cortisol serum levels in lung cancer patients at different stages of disease. Med Sci Monit 11(6):CR284–288
Parker KP, Bliwise DL, Ribeiro M, Jain SR, Vena CI, Kohles-Baker MK, Rogatko A, Xu Z, Harris WB (2008) Sleep/Wake patterns of individuals with advanced cancer measured by ambulatory polysomnography. J Clin Oncol 26(15):2464–2472
Lissoni P, Barni S, Mandala M, Ardizzoia A, Paolorossi F, Vaghi M, Longarini R, Malugani F, Tancini G (1999) Decreased toxicity and increased efficacy of cancer chemotherapy using the pineal hormone melatonin in metastatic solid tumour patients with poor clinical status. Eur J Cancer 35(12):1688–1692
Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP (2003) The role of actigraphy in the study of sleep and circadian rhythms. Sleep 26(3):342–392
Lim AS, Yu L, Costa MD, Buchman AS, Bennett DA, Leurgans SE, Saper CB (2011) Quantification of the fragmentation of rest-activity patterns in elderly individuals using a state transition analysis. Sleep 34(11):1569–1581
Roscoe JA, Morrow GR, Hickok JT, Bushunow P, Matteson S, Rakita D, Andrews PL (2002) Temporal interrelationships among fatigue, circadian rhythm and depression in breast cancer patients undergoing chemotherapy treatment. Support Care Cancer 10(4):329–336
Mormont MC, Waterhouse J, Bleuzen P, Giacchetti S, Jami A, Bogdan A, Lellouch J, Misset JL, Touitou Y, Levi F (2000) Marked 24-h rest/activity rhythms are associated with better quality of life, better response, and longer survival in patients with metastatic colorectal cancer and good performance status. Clin Cancer Res 6(8):3038–3045
Witting W, Kwa IH, Eikelenboom P, Mirmiran M, Swaab DF (1990) Alterations in the circadian rest-activity rhythm in aging and Alzheimer’s disease. Biol Psychiatry 27(6):563–572
Pati AK, Parganiha A, Kar A, Soni R, Roy S, Choudhary V (2007) Alterations of the characteristics of the circadian rest-activity rhythm of cancer in-patients. Chronobiol Int 24(6):1179–1197
Lim AS, Chang AM, Shulman JM, Raj T, Chibnik LB, Cain SW, Rothamel K, Benoist C, Myers AJ, Czeisler CA, Buchman AS, Bennett DA, Duffy JF, Saper CB, De Jager PL (2012) A common polymorphism near PER1 and the timing of human behavioral rhythms. Ann Neurol 72(3):324–334.
Mormont MC, Hecquet B, Bogdan A, Benavides M, Touitou Y, Levi F (1998) Non-invasive estimation of the circadian rhythm in serum cortisol in patients with ovarian or colorectal cancer. Int J Cancer 78(4):421–424
James FO, Boivin DB, Charbonneau S, Belanger V, Cermakian N (2007) Expression of clock genes in human peripheral blood mononuclear cells throughout the sleep/wake and circadian cycles. Chronobiol Int 24(6):1009–1034
Osoba D, Rodrigues G, Myles J, Zee B, Pater J (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16(1):139–144
Dai H, Zhang L, Cao M, Song F, Zheng H, Zhu X, Wei Q, Zhang W, Chen K (2011) The role of polymorphisms in circadian pathway genes in breast tumorigenesis. Breast Cancer Res Treat 127(2):531–540
Yang X, Wood PA, Oh EY, Du-Quiton J, Ansell CM, Hrushesky WJ (2009) Down regulation of circadian clock gene Period 2 accelerates breast cancer growth by altering its daily growth rhythm. Breast Cancer Res Treat 117(2):423–431
Climent J, Perez-Losada J, Quigley DA, Kim IJ, Delrosario R, Jen KY, Bosch A, Lluch A, Mao JH, Balmain A (2010) Deletion of the PER3 gene on chromosome 1p36 in recurrent ER-positive breast cancer. J Clin Oncol 28(23):3770–3778
Del Fabbro E, Dev R, Hui D, Palmer L, Bruera E (2013) Effects of melatonin on appetite and other symptoms in patients with advanced cancer and cachexia: a double-blind placebo-controlled trial. J Clin Oncol 31(10):1271–1276
Fayers PM (2001) Interpreting quality of life data: population-based reference data for the EORTC QLQ-C30. Eur J Cancer 37(11):1331–1334
Ligibel JA (2011) Role of adjuvant and posttreatment exercise programs in breast health. J Natl Compr Canc Netw 9(2):251–256
Van Reeth O, Sturis J, Byrne MM, Blackman JD, L’Hermite-Baleriaux M, Leproult R, Oliner C, Refetoff S, Turek FW, Van Cauter E (1994) Nocturnal exercise phase delays circadian rhythms of melatonin and thyrotropin secretion in normal men. Am J Physiol 266(6 Pt 1):E964–974
Buxton OM, Frank SA, L’Hermite-Baleriaux M, Leproult R, Turek FW, Van Cauter E (1997) Roles of intensity and duration of nocturnal exercise in causing phase delays of human circadian rhythms. Am J Physiol 273(3 Pt 1):E536–542
Liu L, Rissling M, Natarajan L, Fiorentino L, Mills PJ, Dimsdale JE, Sadler GR, Parker BA, Ancoli-Israel S (2012) The longitudinal relationship between fatigue and sleep in breast cancer patients undergoing chemotherapy. Sleep 35(2):237–245
Savard J, Liu L, Natarajan L, Rissling MB, Neikrug AB, He F, Dimsdale JE, Mills PJ, Parker BA, Sadler GR, Ancoli-Israel S (2009) Breast cancer patients have progressively impaired sleep-wake activity rhythms during chemotherapy. Sleep 32(9):1155–1160.
Acknowledgments
Supported by a grant from the Ontario Cancer Research Network 03-APR-0316OCRN to Dr. Bjarnason, the National Cancer Institute K07CA132916 to Dr. Palesh, and the Canadian Institutes of Health Research OOG MOP125934 to Dr. Lim.
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Innominato, P.F., Lim, A.S., Palesh, O. et al. The effect of melatonin on sleep and quality of life in patients with advanced breast cancer. Support Care Cancer 24, 1097–1105 (2016). https://doi.org/10.1007/s00520-015-2883-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2883-6