Abstract
Purpose
Higher symptom burden in oncology patients is associated with poorer quality of life (QOL). However, the long-term predictive relationship between pre-treatment symptom profiles and QOL is unknown. The aim of this study was to identify subgroups of breast cancer patients based on their presurgical symptom profiles and to examine the predictive effect of group membership on QOL 2 years after surgery.
Methods
Data were analyzed from a longitudinal study of women’s (N = 198) symptoms after breast cancer surgery. Patient subgroups were identified by latent class analysis based on presurgical severity of five symptoms (i.e., attentional and physical fatigue, sleep disturbance, depression, and anxiety). Among these 198 women, quality of life 2 years after surgery was available for 97. Group differences in QOL were examined by general linear models.
Results
We identified four distinct patient groups. Group A (All Low) had low levels of all symptoms. Group B (Low Fatigue and Moderate Mood) was characterized by low attentional and physical fatigue but moderate sleep disturbance, depression, and anxiety. Group C (All Moderate) was characterized by moderate levels of all five symptoms. Group D was characterized by moderate attentional and physical fatigue and severe sleep disturbance, depression, and anxiety (Moderate Fatigue and High Mood). Group D had significantly lower overall QOL scores 2 years after surgery than Group A (p = 0.002).
Conclusions
Breast cancer patients’ presurgical symptom profile had a long-term predictive effect on QOL. Routine assessment of patients’ pre-treatment symptom is suggested to identify high risk group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of female breast cancer in Taiwan increased over 5-fold from 1979 (11.86 per 100,000 persons) to 2011 (64.28 per 100,000 persons) [1]. However, early detection and advances in treatment have led to higher survival rates for patients with invasive breast cancer. The 5-year relative survival rate in 2011 was 86.5 % [1]. Given this increase in breast cancer survivors, quality of life has become an important issue. The association between cancer-related symptoms and quality of life is well recognized. For example, fatigue was found to be the strongest predictor of quality of life in breast cancer survivors [2]. Other symptoms, such as pain, insomnia, mood disturbances, and arm problems are known to have a negative impact on quality of life in breast cancer survivors [3, 4].
Cancer patients often experience multiple concurrent symptoms and some of these symptoms are correlated. Research on the management of cancer symptoms has gradually shifted from a focus on individual symptoms to multiple co-occurring symptoms. When such concurrent symptoms are correlated, they are called symptom clusters [5]. Since the concept of symptom clusters was first proposed by Dodd and colleagues [6], symptom clusters have emerged as an important area for cancer symptom research. Correlated symptoms (symptom clusters) have been identified in patients with various cancer diagnoses [4, 7, 8] or with specific conditions, such as breast cancer [9] or metastatic disease [10, 11]. Symptom clusters have been associated with clinical characteristics (e.g., pain and treatment mode) and demographic characteristics (e.g., age and gender) [7, 8]. Instead of grouping symptoms, others have focused on grouping patients based on similar responses to selected multiple symptoms (i.e., symptom profiles) and investigating the link between these patient subgroups and important outcome variables such as quality of life or functional performance status [12–16].
The link between patient subgroups, each with a distinct symptom profile, and quality of life was first reported by Miaskowski and colleagues [12]. In their study of 191 outpatients under active cancer treatment, four patient subgroups were identified based on patients’ responses to fatigue, sleep disturbance, depression, and pain. The subgroups with low levels of all four symptoms reported the best functional status and quality of life [12]. Similar associations between symptom profiles and quality of life were reported in cancer outpatients [13, 15] and specifically in women with breast cancer [14, 16]. In these studies, the association between patient subgroups and outcome variables was based on data collected at the same time, regardless of whether the study had a cross-sectional or a longitudinal design. This lack of temporal relationship makes it difficult to confirm a causal relationship between symptom profiles and quality of life. One only study reported a temporal association between pre-treatment levels of symptom clusters (sleep disturbance, fatigue, and depression) in breast cancer patients and levels of these symptoms during chemotherapy [17]. However, this association was studied for only four 3-week cycles of chemotherapy and did not examine other patient outcomes. Thus, the long-term effect of pre-treatment symptom profiles on patient outcomes is still unknown.
The purposes of this study were to (1) identify distinct patient subgroups based on their symptom profiles before breast cancer surgery, and to (2) examine the predictive relationship between these symptom profiles and quality of life 2 years after breast cancer surgery. Symptoms included were the four most common behavioral symptoms in breast cancer patients, i.e., fatigue, cognitive disturbance (attentional fatigue in this study), sleep disturbance, and depression [18]. The last symptom included was anxiety, a common psychological problem before breast cancer treatment [19, 20].
Patients and methods
Participants and settings
This study is part of a larger longitudinal study that assessed postsurgical symptoms in Taiwanese women with breast cancer treated at one medical center located in Northern Taiwan. Women were invited to participate in the parent study if they met these criteria: (1) at least 18 years old, (2) underwent breast cancer surgery on one breast, and (3) could understand and speak Chinese. Women were excluded if they had breast cancer surgery on both sides, distant metastasis at diagnosis, and/or a defibrillator implanted. Data were collected at enrollment (before surgery), 1, 2, 3, 4, 5, 6, 8, 10, 12, 18, and 24 months after surgery. Written informed consent was obtained from all participants of the study. The current study used only enrollment data (demographics and disease/treatment characteristics, symptoms) and data collected 24 months after surgery (quality of life, performance status, weight gain, and lymphedema). Results using data from all the time points were published elsewhere [21–23]. This study was approved by the Institutional Review Board of the study hospital.
Measures
Patient groups were identified by their distinct profiles of five symptoms: attentional fatigue, physical fatigue, sleep disturbance, depression and anxiety.
Attentional fatigue, or decreased ability to concentrate, was used as a proxy for cognitive impairment and was measured with the 16-item Attentional Function Index (AFI) [24]. The AFI was designed to measure perceived effectiveness in everyday activities requiring use of directed or controlled attention [25]. Each item is rated on a numeric rating scale from 0 (“not at all”) to 10 (“extremely well” or “a great deal”). The overall AFI score, representing the mean of 16 item scores, can range from 0 to 10, with lower scores indicating poorer levels of attentional function. In the current study, overall AFI scores were reversed to better represent the concept of attentional problems (i.e., higher scores indicate higher levels of attentional fatigue). In the current study, the AFI had internal consistency reliability (Cronbach’s alpha) of 0.95.
Physical fatigue was measured with the 13-item fatigue subscale of the 18-item Lee Fatigue Scale (LFS) [26]. Each item is rated on a 0–10 scale and a fatigue severity score is calculated as the mean of 13 items. Higher LFS scores indicate higher levels of physical fatigue. The reliability and validity on the LFS was shown in patients with cancer [27] and caregivers of cancer patients [28]. In the current study, Cronbach’s alpha for the LFS was 0.95.
Sleep disturbance was measured with the 20-item General Sleep Disturbance Scale (GSDS) [29]. The GSDS assesses the frequency of sleep problems during the past week. Each item is rated on an 8-point scale from 0 (not at all) to 7 (every day). The total score ranges from 0 to 140, with higher scores indicating greater frequency and severity of sleep disturbance. The GSDS has been used in breast cancer patients with satisfactory reliability [30]. In this study, the GSDS had a Cronbach’s alpha of 0.82.
Depression was assessed by the 20-item Center for Epidemiological Study-Depression (CES-D) scale [31] that measures depressive symptoms for the past week. Each symptom is rated for its frequency on a 4-point scale from 0 (rarely or none of the time) to 3 (most or all of the time). The total score ranges from 0 to 60. Scores >16 indicate the need for a diagnostic evaluation for major depression. The CES-D has demonstrated good reliability and validity in cancer patients [32]. In this study, the CES-D had a Cronbach’s alpha of 0.93.
Anxiety was measured using the State Anxiety Scale of 20-item Spielberger State-Trait Anxiety Inventory (STAI-S) [33]. Patients are asked to rate emotional response intensity at this moment on a 4-point scale (1 = “not at all,” 2 = “somewhat,” 3 = “moderately so,” and 4 = “very much so”). Total scores range from 20 to 80, with higher scores indicating greater anxiety. The STAI is the most widely used measure of anxiety, with high internal consistency ranging from 0.83 to 0.92 and documented evidence of validity [33, 34]. Cronbach’s alpha in this study was 0.94.
Quality of life was measured using the 41-item Quality of Life-Cancer Survivor (QOL-CS) [35], which was specifically designed for patients with cancer. The QOL-CS measures quality of life in four domains: physical well-being (8 items), psychological well-being (18 items), social well-being (8 items), and spiritual well-being (7 items). Each item is rated on a 0–10 scale along with anchors. The scoring should be based on a scale of 0 = worst outcome to 10 = best outcome. Both domain scores and overall quality of life score range from 0 to 10, with higher scores indicating better quality of life. The 2-week test-retest and internal consistency reliability for overall QOL-CS were 0.89 and 0.93, respectively [36]. Overall QOL-CS scores were highly correlated with scores on the Functional Assessment of Cancer Therapy-General scale [36]. Internal consistency reliability of the Chinese version QOL-CS was reported as 0.85 and 0.86 [37]. Cronbach’s alpha of the QOL-CS in the current study was 0.91.
Information regarding the psychometric properties of Chinese-version of all measures for symptoms can be found in the previous publication [21].
Analysis
Subgroups of breast cancer patients were identified by latent class analysis based on their severity ratings for five presurgical symptoms. We tested the fit of different models from one to four classes by the Bayesian information criterion (BIC); the smaller the BIC the better the fit. Identified subgroups had different combinations of severity scores for the five symptoms. Each person was then assigned to a subgroup based on the estimated modal probability. The distinctness of each identified subgroup was confirmed by one-way analysis of variance (ANOVA) to test for differences among subgroups in symptom severity scores for each of the five symptoms. Demographic and clinical factors associated with group membership were explored using chi-square tests.
Demographic and disease/treatment variables associated with quality of life 2 years after surgery were first explored by t-tests or ANOVAs. Subgroup differences in quality of life at 2 years after breast cancer surgery were then tested by general linear modeling, controlling for covariates identified in the first step. Pairwise comparisons was adjusted with the Bonferroni method [38].
Results
Sample characteristics
Of 200 women enrolled in the original study, 198 had complete presurgical data on symptoms. Among these 198 women, 97 were able to be contacted to complete quality of life measurements 2 years after surgery. At enrollment, the 198 patients had a mean age of 47.7 years (SD = 10.18, range = 23 to 85) and 36.4 % were postmenopausal. The majority (57 %) had at least a senior high school education, and most were married (81 %) and lived with someone (82 %). At enrollment, 51 % of the patients were working for pay and 49 % had a monthly household income of at least NT$ 50,000 (around US$ 1667). Most women did not exercise regularly and 84 % had an early disease stage (stage II or earlier). The majority (59 %) received mastectomy, while the remaining 41 % received breast conservation surgery. The largest proportion (74 %) received adjuvant chemotherapy, 50 % received radiotherapy, and 62 % hormonal therapy. At enrollment, most women (97 %) had very good functional status (Karnofsky Performance Status score > 90 %) (Table 1). Except for receipt of adjuvant chemotherapy, no differences were found in any demographic and clinical characteristics between the 198 patients who enrolled and 97 patients who were available for the 2 year follow up. More patients who received chemotherapy (53.7 %) were available 2 years after surgery than those who did not receive chemotherapy (35.3 %).
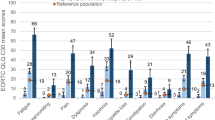
Distinct patient subgroups
Considering both model fit index and clinical interpretability, the latent class analysis identified four subgroups (Groups A, B, C, and D). Groups A, B, C, and D comprised 22, 37, 24, and 17 %, respectively of the total sample. The presurgical mean levels of five symptoms for each subgroup and the total sample are presented in Table 2. On average, women with breast cancer experienced low attentional fatigue, low physical fatigue, moderate sleep disturbance, depressive symptoms, and anxiety before surgery. To facilitate comparisons among groups, the mean score for each symptom was re-scaled to 0–1, and these re-scaled means were used to construct a radar chart of symptom profiles for the four identified subgroups (Fig. 1).
Group A (22 %) was characterized by low mean scores (re-scaled means ranged from 0.01 to 0.24) on all five symptoms, especially for attentional and physical fatigue. Therefore, Group A was labeled “All Low.” Group B (37 %) was characterized by low scores on attentional and physical fatigue (both <0.1), but moderate scores on sleep disturbance (0.36), depression (0.31), and anxiety (0.51). This group was labeled “Low Fatigue and Moderate Mood.” Group C (24 %) was characterized by moderate levels (range = 0.30 to 0.52) on all five symptoms. Therefore, this group was labeled “All Moderate.” Of all four groups, Group D (17 %) had the highest mean symptom severity scores for all five symptoms (0.36 to 0.89) and could have been labeled “All High.” However, based on the magnitude of re-scaled means, this group had moderate levels of attentional fatigue (0.43) and physical fatigue (0.36), but high levels of sleep disturbance (0.67), depression (0.78), and anxiety (0.89). Therefore, we labeled group D “Moderate Fatigue and High Mood.”
The success of this solution in identifying distinct patient groups was tested by comparing group differences in mean scores for the five symptoms. The overall group differences on each of the five symptoms were all significant (p < 0.001) (Table 2). For attentional and physical fatigue, Group C (All Moderate) and D (Moderate Fatigue and High Mood) had significantly higher levels than Group A (All Low) and B (Low Fatigue and Moderate Mood). For sleep disturbance, all paired group comparisons were significant, with the mean sequence D > C > B > A. For depressive symptoms and anxiety, Group A had significantly lower levels than all other groups and Group D had significantly higher levels than all other groups (Table 2).
Characteristics associated with group membership
Characteristics associated with group membership were marital status (p = 0.044), education level (p = 0.004), and functional performance (p < 0.001). Group A (All Low) had a lower percentage (66.7 %) of married women than the other three groups (82.7−88.4 %). Women with more education (> senior high school) were more likely to be in Group C (All Moderate) (79.1 %) and less likely to be in Group B (Low Fatigue and Moderate Mood) (45.3 %). Group D (Moderate Fatigue and High Mood) had a higher percentage of patients with KPS score ≤ 90 (77.1 %) than Groups A (20 %), B (29.3 %), and C (32.6 %) (Table 1).
Long-term predictive effect of symptom profile (patient subgroups) on quality of life
After screening for potential covariates of quality of life 2 years after surgery, only functional status and the occurrence of lymphedema 2 years after surgery were associated with quality of life. After controlling for these two covariates, women in the four subgroups were significantly different in their overall quality of life scores (p = 0.002). Women in Group A had the highest mean quality of life score (M = 6.96), followed by Groups B (M = 6.37), C (M = 6.17), and D (M = 5.54). Pairwise comparisons with Bonferroni adjustment showed that women in Group A had significantly better overall quality of life than those in Group D (p = 0.002) (Table 3). In addition, group membership was significantly associated with the quality of life subscale scores of Psychological well-being (p = 0.001), and marginally associated with Physical well-being (p = 0.07) and Social well-being (p = 0.08), but not Spiritual well-being (Table 3).
Discussion
This study successfully identified four distinct groups of breast cancer patients based on their response patterns to five presurgical symptoms (i.e., attentional fatigue, physical fatigue, sleep disturbance, depression, and anxiety). Distinct symptom profiles were found for each patient group. Most importantly, group membership prior to surgery predicted quality of life 2 years after breast cancer surgery. Our study is the first to demonstrate the long-term predictive effect of pre-treatment symptom profiles on quality of life.
Despite using different symptom combinations, our findings on patient groups are similar to those of other studies on cancer patients [12–14, 16] in that “All High” and “All Low” patient groups were identified, even though our putative “All High” group was more accurately labeled “Moderate Fatigue and High Mood.” The cumulative evidence suggests that some cancer patients, around 40 % in our sample, either have severe symptom burden (“All High”) or very mild symptoms that may be ignored (“All Low”). Clinicians can easily identify these two groups of patients using validated tools that assess multiple symptoms.
Groups A and B were similar in that they both had relatively low scores for attentional and physical fatigue while groups C and D had higher mean scores for these two symptoms. Unlike physical fatigue, attentional fatigue refers to a decreased capacity to concentrate, usually following intense mental effort [24]. For some women, being diagnosed with breast cancer and facing multiple treatment options can be stimuli that require intense mental effort to focus on, resulting in directed attentional fatigue. This mental fatigue has been correlated with physical fatigue not only in our study, but also in previous research on breast cancer patients [39]. Mental fatigue has also been shown to impair physical performance [40]. Since Groups A and B (low fatigue groups) had relatively better quality of life, clinicians may briefly screen patients for both physical and attentional fatigue before cancer treatment as an initial step before assessing for multiple symptoms.
Married women were less likely to be classified in Group A (All Low). This finding may be explained by married Asian women with breast cancer having multiple responsibilities, such as work, child care, and parent care, during their illness process [22]. These multiple responsibilities may lead to more behavioral symptoms. Women with higher education were more likely to be in Group C and less likely to be in Group B. Groups B and C had similar levels of anxiety and depressive symptoms, but Group C had higher levels of attentional and physical fatigue, suggesting that more educated people have more chances in daily life to consciously recognize any changes in their cognitive function (attentional fatigue in this study). More studies are needed to elucidate this association. In addition, consistent with previous studies [12–16], we also found that functional status was associated with group membership.
Our study showed that breast cancer patients’ pre-treatment symptom experience predicted their overall quality of life 2 years after treatment, strengthening previous reports of a concurrent association between symptom profile and quality of life [12–16]. Our finding highlights the importance of pre-treatment symptom assessment, which not only serves as a baseline for evaluating treatment impact, but also has long-term predictive power. Routine pre-treatment screening is warranted to identify groups at high risk for poor quality of life. Women who are married, well educated, and have less than optimal pre-treatment functional status may need special attention from healthcare providers.
It is interesting to note that pre-treatment symptom profile did not predict the spiritual dimension of quality of life. However, women who received hormonal therapy tended to have lower scores on spiritual well-being. These women were still receiving hormonal therapy 2 years after surgery, which may have contributed to their uncertainty about the future or lack of hope. Other factors that predict the spiritual dimension of quality of life should be explored in future studies.
One of the study limitations was that only half of the original sample was assessed 2 years after surgery. While patients who were and were not available for the 2 year follow up did not differ significantly on demographic characteristics and initial symptom levels, patients who were not followed may have had poorer or better 2-year quality of life than those who were followed. Although patients had no difficulty to complete all the scales, repeatedly asking patients to respond to a large amount of questions might have contributed to the high attrition in this study. In addition, the study sample selected from the single medical center may limit the generlaizability of the study findings.
In conclusion, this study successfully identified four distinct patient groups based on their pre-treatment response profiles for five symptoms and demonstrated the long-term predictive power of these profiles on quality of life after treatment. This finding strengthens the importance of early screening of symptoms. To make symptom screening as a routine practice, development of a brief and reliable measurement system cannot be overemphasized. Future studies could explore the predictive power of pre-treatment symptom profiles on disease prognosis.
References
Liao M-N, Chen M-F, Chen S-C, Chen P-L (2008) Uncertainty and Anxiety During the Diagnostic Period for Women With Suspected Breast Cancer. Cancer Nurs 31: 274-283
Arndt V, Stegmaier C, Ziegler H, Brenner H (2006) A population-based study of the impact of specific symptoms on quality of life in women with breast cancer 1 year after diagnosis. Cancer 107:2496–2503
Engel J, Kerr J, Schlesinger-Raab A, Eckel R, Sauer H, Hölzel D (2003) Predictors of quality of life of breast cancer patients. Acta Oncol 42:710–718
Cheng KK, Lee DT (2011) Effects of pain, fatigue, insomnia, and mood disturbance on functional status and quality of life of elderly patients with cancer. Crit Rev Oncol Hematol 78:127–137
Dodd M, Janson S, Facione N, Faucett J, Froelicher ES, Humphreys J, Lee K, Miaskowski C, Puntillo K, Rankin S, Taylor D (2001) Advancing the science of symptom management. J Adv Nurs 33:668–676
Dodd MJ, Miaskowski C, Paul SM (2001) Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum 28:465–470
Chen ML, Tseng HC (2006) Symptom clusters in cancer patients. Support Care Cancer 14:825–830
Thomas BC, Waller A, Malhi RL, Fung T, Carlson LE, Groff SL, Bultz BD (2014) A longitudinal analysis of symptom clusters in cancer patients and their sociodemographic predictors. J Pain Symptom Manag 47:566–578
Bender CM, Ergyn FS, Rosenzweig MQ, Cohen SM, Sereika SM (2005) Symptom clusters in breast cancer across 3 phases of the disease. Cancer Nurs 28:219–225
Cheung WY, Le LW, Zimmermann C (2009) Symptom clusters in patients with advanced cancers. Support Care Cancer 17:1223–1230
Hird A, Wong J, Zhang L, Tsao M, Barnes E, Danjoux C, Chow E (2010) Exploration of symptoms clusters within cancer patients with brain metastases using the spitzer quality of life index. Support Care Cancer 18:335–342
Miaskowski C, Cooper BA, Paul SM, Dodd M, Lee K, Aouizerat BE, West C, Cho M, Bank A (2006) subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: a cluster analysis. Oncol Nurs Forum 33:E79–E89
Pud D, Ben Ami S, Cooper BA, Aouizerat BE, Cohen D, Radiano R, Naveh P, Nikkhou-Abeles R, Hagbi V, Kachta O, Yaffe A, Miaskowski C (2008) The symptom experience of oncology outpatients has a different impact on quality-of-life outcomes. J Pain Symptom Manag 35:162–170
Dodd MJ, Cho MH, Cooper BA, Miaskowski C (2010) The effect of symptom clusters on functional status and quality of life in women with breast cancer. Eur J Oncol Nurs 14:101–110
Ferreira KA, Kimura M, Teixeira MJ, Mendoza TR, da Nobrega JC, Graziani SR, Takagaki TY (2008) Impact of cancer-related symptom synergisms on health-related quality of life and performance status. J Pain Symptom Manag 35:604–616
Kim HJ, Barsevick AM, Beck SL, Dudley W (2012) Clinical subgroups of a psychoneurologic symptom cluster in women receiving treatment for breast cancer: a secondary analysis. Oncol Nurs Forum 39:E20–E30
Liu L, Fiorentino L, Natarajan L, Parker BA, Mills PJ, Sadler GR, Dimsdale JE, Rissling M, He F, Ancoli-Israel S (2009) Pre-treatment symptom cluster in breast cancer patients is associated with worse sleep, fatigue and depression during Chemotherapy. Psychooncology 18:187–194
Bower JE (2008) Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol 26:768–777
Lehto RH, Cimprich B (1999) Anxiety and directed attention in women awaiting breast cancer surgery. Oncol Nurs Forum 26:767–772
Liao MN, Chen MF, Chen SC, Chen PL (2008) Uncertainty and anxiety during the diagnostic period for women with suspected breast cancer. Cancer Nurs 31:274–283
Chen ML, Miaskowski C, Liu LN, Chen SC (2012) Changes in perceived attentional function in women following breast cancer surgery Breast Cancer Res Treat 131:599–606
Huang HP, Chen ML, Liang J, Miaskowski C (2014) Changes in and predictors of severity of fatigue in women with breast cancer: a longitudinal study. Int J Nurs Stud 51:582–592
Liu LN, Wen FH, Miaskowski C, Lin YC, Wang JS, Jeng C, Chen ML (2014) Weight change trajectory in women with breast cancer receiving chemotherapy and the effect of different regimens. J Clin Nurs 23:2757–2768
Cimprich B (1992) Attentional fatigue following breast cancer surgery. Res Nurs Health 15:199–207
Cimprich B, Visovatti M, Ronis DL (2011) The attentional function index–a self-report cognitive Measure. Psychooncology 20:194–202
Lee KA, Hicks G, Nino-Murcia G (1991) Validity and reliability of a scale to assess fatigue. Psychiatry Res 36:291–298
Miaskowski C, Lee KA (1999) Pain, fatigue, and sleep disturbances in oncology outpatients receiving radiation therapy for bone metastasis: a pilot study. J Pain Symptom Manag 17:320–332
Fletcher BS, Paul SM, Dodd MJ, Schumacher K, West C, Cooper B, Lee K, Aouizerat B, Swift P, Wara W, Miaskowski CA (2008) Prevalence, severity, and impact of symptoms on female family caregivers of patients at the initiation of radiation therapy for prostate cancer. J Clin Oncol 26:599–605
Lee KA (1992) Self-reported sleep disturbances in employed women Sleep 15: 493–498
Van Onselen C, Cooper BA, Lee K, Dunn L, Aouizerat BE, West C, Dodd M, Paul S, Miaskowski C (2012) Identification of distinct subgroups of breast cancer patients based on self-reported changes in sleep disturbance. Support Care Cancer 20:2611–2619
Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Hann D, Winter K, Jacobsen P (1999) Measurement of depressive symptoms in cancer patients: evaluation of the center for epidemiological studies depression scale (CES-D). J Psychosom Res 46:437–443
Spielberger CG, Gorsuch RL, Suchene R, Vagg PR, Jacobs GA (1983) Manual for the state-trait anxiety inventory (form Y). Consulting Psychologists Press, Palo Alto
Novy DM, Nelson DV, Goodwin J, Rowzee RD (1993) Psychometric comparability of the state-trait anxiety inventory for different ethnic subpopulations. Psychol Assess 5:343–349
Ferrell BR, Dow KH, Grant M (1995) Measurement of the quality of life in cancer survivors. Qual Life Res 4:523–531
Ferrell BR, Grant M Quality of Life Patient/Cancer Survivor Version. Retrieved from http://prc.coh.org/QOL-CS.pdf
Chen L-M (2007) The influence of pain beliefs/attitudes on pain experience among advanced cancer patients in Taiwan. Doctoral dissertation. University of California, San Francisco
Bland JM, Altman DG (1995) Multiple significance tests: the bonferroni method. BMJ 310:170
Merriman JD, Dodd M, Lee K, Paul SM, Cooper BA, Aouizerat BE, Swift PS, Wara W, Dunn L, Miaskowski C (2011) Differences in self-reported attentional fatigue between patients with breast and prostate cancer at the initiation of radiation therapy. Cancer Nurs 34:345–353
Marcora SM, Staiano W, Manning V (2009) Mental fatigue impairs physical performance in humans J Appl Physiol (1985) 106: 857-864
Acknowledgments
This study was supported by a research grant to Dr. Mei-Ling Chen from the National Science Council of Taiwan (grant number: NSC 94–2314-B-182–025, NSC 95–2314-B-182–005, NSC 96–2628-B-182–032).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, ML., Liu, LN., Miaskowski, C. et al. Presurgical symptom profiles predict quality of life 2 years after surgery in women with breast cancer. Support Care Cancer 24, 243–251 (2016). https://doi.org/10.1007/s00520-015-2784-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2784-8