Abstract
Objective
It is a current hypothesis that chemotherapy-induced nausea and vomiting (CINV) may ultimately impede the clinical success of cancer treatments by hindering patients’ adherence to the optimal treatment schedule. The aim of this study is to examine clinical trial data retrospectively for possible evidence of such a detrimental impact of CINV.
Patients and methods
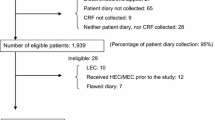
Data from three recent European Organization for Research and Treatment of Cancer (EORTC) trials of highly emetogenic cisplatin-based chemotherapy in diverse patient populations were analyzed retrospectively for incidence and possible impact of CINV. Data on the incidence of emesis are presented as simple descriptive analyses, while the hypothetical impact of CINV on clinical outcomes and on the patients’ length of hospital stays is analyzed by means of multivariate regression analysis techniques to control for confounding variables.
Main results
Between 42 and 59% of the patients in the trials experienced at least one episode of nausea of NCIC grade 2 or worse, while the incidence of vomiting of similar grade was between 31 and 58%. Only in one of the trials could the determinants of the adherence to protocol therapy be assessed, statistically significant variables were the severity of emesis (p<0.0001) and other toxicities combined (p<0.019). In turn, a Cox regression showed adherence to protocol therapy and other toxicities as the only statistically significant determinants of overall survival.
Conclusions
This study has shown a discernible detrimental impact of CINV on patients’ adherence to protocol therapy and, indirectly, on survival in one of the three trials examined. Further studies are required to substantiate this finding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced nausea and vomiting (CINV) is often reported to be one of the most important concerns of those cancer patients, for whom chemotherapy is currently the treatment of choice [6]. The symptoms of nausea and vomiting may be very distressing for the patients themselves as well as for their caregivers and have a serious negative impact on the patients’ quality of life. Despite the improvements in the control of emesis obtained by the advent of the setrons, there is still some way to go until achieving the goal of optimal emesis control, i.e. complete absence of episodes of nausea and vomiting.
Inadequately controlled emesis engenders a burden, whether the patient is hospitalized or not; however, in some cases, it may also precipitate medical complications such as dehydration and electrolyte imbalances that may even become life threatening. Such complications may lead to extended hospitalizations and increased use of medical resources in terms of nursing time and pharmacy services; however, even without suffering actual medical complications, patients with acute or delayed emesis will presumably often be retained in the hospital until their conditions have improved rather than be discharged to their homes.
It seems plausible that the distress caused by the symptoms of CINV may escalate over time during a course of chemotherapy because of the development of a kind of conditioned response in some patients, and many emesis researchers stress the importance of effective emesis prophylaxis from the very first treatment cycle (cf. [4, 6]). The idea of patients’ distress escalating over time has led some researchers to hypothesize that emesis may lead to important disturbances of the intended treatment schedule (dose delays and/or dose reductions), and some patients may even refuse to continue the initiated treatment. It may thus be hypothesized that emesis may ultimately have a detrimental impact on such clinical outcomes as survival time and not “only” diminish the patients’ health-related quality of life (QoL) during the period of treatment (cf. [2, 6, 8]).
The principal aim of the present study is to examine whether it is possible to discern such a negative impact of CINV on clinical outcomes such as progression-free and overall survival or on economic outcomes such as the patients’ length of stay in hospital. The data for the analysis come from three recent European Organization for Research and Treatment of Cancer (EORTC) randomized control clinical trials of new chemotherapy regimens in diverse populations of cancer patients.
Data and methods
This study is a retrospective analysis of data from three recent phase III clinical trials of highly emetogenic cisplatin-based chemotherapy regimens in cancer patients with advanced disease. The trials targeted three distinct patient populations, and in none of them was there paid any specific attention to the emesis issue (e.g. in terms of giving protocol directions for the use of antiemetics), besides recording the occurrence of symptoms and the possible use of antiemetics. It may therefore be contended that these trials can be assumed to represent ordinary clinical practice insofar as the incidence of emesis, the use of antiemetics, and the handling of emetic episodes by the hospitals are concerned.
The three trials were selected for this analysis because each of them had an economic evaluation integrated from its inception, which means that certain data not usually collected in RCTs have been recorded. This is notably the case for the number and duration of hospital stays, allowing an assessment of the possible impact of emesis on the total number of days patients spent in hospital. In addition, the primary analyses of these trials in terms of economic evaluations have recently been finalized; thus, the data are now available for secondary analyses.
The three trials are the following: (1) EORTC 30941, testing the equivalence of three vs four cycles of BEP (bleomycin, etoposide, cisplatin), each administered over 3 vs 5 days in good prognosis advanced testis cancer patients [3]; (2) EORTC 55931, testing cisplatin–paclitaxel vs cisplatin–cyclophosphamide in patients with advanced ovarian cancer [5]; and (3) EORTC 08975, testing cisplatin–gemcitabine and gemcitabine–paclitaxel vs cisplatin–paclitaxel in patients with advanced nonsmall cell lung cancer [7]. The patient populations included in the present study are thus very heterogenous; however, all received highly emetogenic chemotherapy with cisplatin doses ranging from 75 to 100 mg/m2.
In all three trials, the incidence and severity of nausea and vomiting (and all other toxicities) were assessed by the clinicians using the NCIC-2 toxicity grading scale. This assessment was always done just before the administration of each new cycle of chemotherapy and covered the period since the last cycle was received. Only the grade of the worst episode of toxicity experienced during this period was recorded, but not its duration or time of onset, so it’s not possible to distinguish between acute and delayed emesis. For most of the analyses of this study, emesis is treated as a binary variable, with nausea or vomiting of severity grade 2 or higher counted as emetic episodes, while recorded episodes of grade 1 are disregarded. For some other analyses, indices of the severity of nausea and vomiting, respectively, were constructed by summing the severity grades observed and dividing this by the sum that would have resulted, if the patient had suffered the worst possible grade of emesis in each cycle.
As a summary measure of the individual patient’s adherence to the protocol-stipulated therapy, a composite relative dose intensity (CRDI) measure has been constructed. This combines the relative dose intensity per unit of time (the standard measure of relative dose intensity) with the relative cumulated dose, i.e. the total dose received as a proportion of the cumulated dose stipulated by the protocol. This measure thus accounts for both the total dose given and the intensity over time with which it was administered.
The first part of the analyses performed was purely descriptive, describing the incidence of emesis, other toxicities, or the number of days in hospital per cycle of chemotherapy (the basic observational unit). Other descriptive analyses have been performed with the patient as observational unit, e.g. the relative dose intensity per patient according to incidence of emesis. For the descriptive analyses, statistical testing takes the form of χ2-tests for the categorical variables and (bootstrapped) t-tests of differences of means for continuous variables.
Further analyses performed were more analytical or exploratory aiming at elucidating the causal mechanisms behind the patterns observed in the descriptive analyses. These analyses were performed using multivariate regression techniques in order to discern the conceivable impact of emesis while controlling for possible confounding factors, for instance, the incidence of other toxicities and their role in explaining variations in the number of days spent in hospital. A large number of multivariate explanatory analyses have been performed in order to determine whether emesis has a discernible impact on the various outcomes of interest. The multivariate regression techniques applied were basically ordinary least squares (OLS) and logistic regressions; however, a number of analyses were rerun and elaborated upon by using mixed-model techniques.
Results
Descriptive analyses
Table 1 shows the incidence of emesis per cycle of chemotherapy in each of the trials. The large majority of the emesis events were of grade 2 severity. Nausea of grade 3 occurred only in about 3% of the cycles, while the incidence of grade 3 or 4 vomiting was about 2%. In the testis trial, the schedule of administration was important, with a statistically significantly higher incidence in the 3-day than in the 5-day schedule. The incidence of both nausea and vomiting was much higher in the ovarian trial than in the two other trials; this is probably a reflection of the gender differences between the patients in the trials, as women are frequently found to be more susceptible to emesis than men.
Analysis of the development of the incidence of emesis over the course of chemotherapy showed statistically nonsignificant trends of either an increase in incidence (testis) or a fall over time (lung). Contrary to this, there was a statistically significant increase in the incidence over the course of therapy in the ovarian cancer trial, especially with regard to nausea, as seen in Table 2.
In the lung cancer study, antiemetics were given in almost all cycles, while this information was not recorded in the ovarian cancer trial. In the testis cancer trial, there was about 20% of the cycles, where no antiemetics were given. It was not recorded whether antiemetics were given as prophylaxis or to alleviate symptoms after their occurrence; however, the incidence of emesis, especially vomiting, was much lower in cycles, where no antiemetics were given. This could indicate that antiemetics most often were given to treat symptoms in this trial.
It is rare that emesis is the only toxicity occurring during a cycle, and usually it appears simultaneously with several other types of toxicities. Table 3 shows the statistical associations between the incidence of emesis and other toxicitiesFootnote 1 per cycle. Across the trials, statistically significant associations are particularly found between emesis and other gastrointestinal toxicities (anorexia, diarrhea, pain/cramping, stomatitis, and constipation) plus certain other, nonspecific toxicities such as fatigue and lethargy.
Table 4 shows that there apparently was a clear association between the incidence of emesis (here, vomiting) and the length of stay in hospital per cycle of chemotherapy. The differences are highly statistically significant, except in the case of the testis cancer trial with chemotherapy administered over 5 days. The difference is particularly great in the lung cancer study with an average length of stay in cycles with emesis more than 2 days longer than in cycles without emesis.
Table 5 shows that the goal of absolute emesis control over the entire course of chemotherapy was obtained for about half of the patients in two of the trials, while only one third of the women in the ovarian trial escaped any emesis-related problems during the treatment period. On the other hand, a smaller, but not ignorable, group of patients (5–8% of all patients in the trials) suffered from emesis after each cycle of chemotherapy received.
Exceptionally, patients in the lung cancer trial were assessed for their experience of toxicities during the time period just before starting the first cycle of chemotherapy, and this allows an assessment of the incidence of anticipatory emesis. In the group of patients for whom the occurrence of toxicities was assessed before the first cycle of chemotherapy, the incidence of anticipatory emesis was 7.2%, and these patients also had a much higher than average incidence and severity of emesis over the course of therapy. In addition, they had much more frequent and severe grades than the rest of the patients of most of the other toxicities.
The lung cancer trial also comprised a systematic and detailed recording of each occurrence of a serious adverse event (SAE), its assumed relation to the study treatment and all the actions taken to resolve it.Footnote 2 The altogether 262 SAEs recorded in the trial involved 137 (28.5%) of all the patients randomized, and 14.9% of the SAEs, involving 5.2% of the patients, were related, partly or entirely, to emesis. Two and a half percent of all patients stopped the treatment before the end of protocol therapy for reasons partly (n=10) or entirely (n=2) related to emesis, while altogether, only 45% of the patients randomized received all the six cycles stipulated by the protocol; the principal reason for premature termination of treatment was disease progression. Similarly detailed data were not available for the other trials, but emesis has not been recorded as (part of) the reason for going off trial treatment in any of them.
The extent to which the patients, on average, actually received the cumulative dose of the cytotoxics stipulated by the protocol was estimated by a so-called composite relative dose intensity measure (described in the “Data and methods” section). In none of the trials did this relative dose intensity measure depend on the incidence or not of emesis, so according to this bivariate analysis, the patient’s adherence to the protocol-specified treatment was not related to emesis.
The relation between emesis and the length of hospital stays observed at the cycle level reappears when analyzed, cumulated over the course of therapy at the patient level. Patients having experienced one or more events of emesis over the course of therapy have, on average, spent 2 to 4 days more in hospital than those without emesis, and these differences are statistically significant (with p values<0.01).
Multivariate explanatory analyses
In general, it has not been possible to discern any direct emesis-related difference in the principal clinical outcome measures of the three trials, overall survival time, and progression-free survival time. As an example, Fig. 1 shows the estimated Kaplan–Meier survival curves for the lung cancer patients, stratified according to whether they had experienced emesis or not. The curves are indistinguishable (log–rank p value=0.71), and similar results are obtained for the two other trials.
Looking specifically at the 2.5% of the lung cancer patients that went off treatment for reasons partly or entirely related to emesis, it appears that their survival is quite similar to that of all the other patients of this trial.Footnote 3
However, the hypothesis of actual interest is that the occurrence of emesis might impede the patients’ adherence to the protocol-stipulated treatment and that this would be expected to have a negative impact on survival (assuming that the protocol stipulates optimal doses and administration schedules). Taking the composite relative dose intensity as the measure of adherence to the protocol, the average estimated value of this turns out to be very close to 1 in the testis cancer trial and with so little variation between patients that an analysis of the possible impact is hardly feasible. In the ovarian cancer trial, the assessment of the degree of adherence to the protocol therapy is much less obvious because patients that had not progressed after six cycles of chemotherapy could, but were not obliged to, continue with chemotherapy up to another three cycles. For these additional cycles, several other polydrug regimens than those used during the first six cycles were permitted as options, with the consequence that adherence to protocol therapy becomes a rather blurred notion in this case. Although the following type of analysis might have been attempted for all three trials, only the results of the analysis of the lung cancer trial will be reported here because of the ambiguities inherent in the ovarian cancer trial and the insufficient variability of the explanatory variable in the testis cancer trial.
The importance of adherence to the protocol therapy was analyzed by means of a Cox proportional hazards model, using a so-called landmark method (cf. [1]). The idea of this method is to take into consideration the fact that a patient who dies early for whatever reason, e.g. progression of disease or for reasons unrelated to the disease, will not have the chance to complete treatment as intended. This eventuality may accordingly jeopardize the possibility of drawing inference about the importance of completing treatment as intended. The landmark approach controls for early deaths by adjusting the outcome measure as considered appropriate in the case at hand. Here, this has been done by measuring survival only from the stipulated time of end of treatment (i.e. date of randomization+18 weeks). The results of the analysis of the Cox proportional hazards model with this adjusted survival time outcome measure was that only the index for all other toxicities and the composite relative dose intensity measure were retained as statistically significant explanatory factors among the many possible determinants included in the model analyzed (such as performance status, disease stage, etc.). The importance of completing the intended course of treatment appears from Fig. 2, which shows the estimated Kaplan–Meier survival curves for the lung cancer patients stratified according to whether their composite relative dose intensity measure was above or below 0.90. The log–rank test for the equality of these two KM survival curves has a p value of 0.0004.
Estimated Kaplan–Meier survival curves for the lung cancer trial separating patients that completed the full protocol treatment (bold line) with those who stopped treatment before having received six cycles, for whatever reasons (thin line). Survival is measured here from the stipulated end of treatment time (18 weeks after the date of randomization) to take account of early deaths (landmark method). Log–rank test, p=0.0004
The next step was then to examine the possible determinants of the composite relative dose intensity. This was done by using both multivariate OLS regression and mixed-model regression analysis techniques on models including variables such as emesis, other toxicities, patients’ performance status, age, sex, stage of disease, and treatment group as determinants. The results were that an emesis index and an index for other toxicities each had a statistically significant negative effect on the adherence to protocol therapy, while no other variables had a significant impact. While the coefficient for the effect of emesis was quite small compared to that of the index for other toxicities, emesis does seem in this case to have had an independent effect on the adherence to protocol therapy after the control for confounding variables.
Another possible impact of emesis of considerable interest is the increase in the number of days spent in hospital, which appeared from the descriptive, bivariate analyses of all the three trials. When this effect is appropriately analyzed by applying multivariate regression techniques, the results are somewhat mixed, however. In the lung cancer trial, the apparent impact of emesis on hospital days disappears completely when other explanatory variables are controlled for. The important statistically significant determinants of the number of days admitted to hospital are here the patients’ initial performance status, occurrence of any SAE, and the treatment group.Footnote 4
Similar analyses performed on the data from the testis cancer trial conclude that the positive effect of emesis on the number of hospital days remains statistically significant when other potentially important determinants are controlled for. Other statistically significant factors are ‘other toxicities’ (with a coefficient six times larger than that of emesis) and, obviously, the administration schedule (i.e. 3 vs 5 days) followed.
In the ovarian cancer trial, the multivariate analysis at the cycle level showed a borderline significant probability of “prolongation of hospitalization”Footnote 5 in cycles with an emetic episode. However, at the patient level, no association between emesis and length of hospital stays over the course of therapy was found in the multivariate mixed-model analyses. The principal statistically significant determinants of the number of hospital days in this trial were treatment group, SAEs, and hematological toxicities.
Discussion
The idea that chemotherapy-induced emesis may ultimately impede the treatment outcomes of cancer patients treated with highly emetogenic chemotherapy seems an interesting and plausible hypothesis. Previous evocations of this hypothesis (e.g. [4, 6, 8]) fail, however, to provide any actual, empirical evidence of such a detrimental impact of emesis and refer at best only to anecdotal evidence as support. The principal aim of the present study was therefore to examine whether it was possible to provide empirical evidence to corroborate or refute the hypothesis of a detrimental effect of emesis on the survival outcomes of cancer patients given chemotherapy. To the best of our knowledge, this study is the first to present an analysis focused on determining exactly the extent of such a possible effect.
However, the evidence gleaned from this retrospective analysis is less than clear-cut. Emesis has been recorded as (one of) the reason(s) for going off protocol therapy for a few of the patients in the lung cancer trial, while in the other two trials, apparently no patients went off study treatment because of emesis. The patients going off treatment because of emesis had survival similar to the rest of the patients, and the comparison of the survival times of the patients that have suffered at least one episode of emesis with that of patients free of emesis did not show any differences in any of the trials. However, such evidence is hardly sufficient to refute the hypothesis, which is more circumspect.
The multivariate analysis of the data from the lung cancer trial showed that overall survival time, when adjusted for early deaths by measuring survival from the time treatment would have ended, had the protocol been followed, was statistically significantly determined by an index for other toxicities, and a measure of patient adherence to the protocol therapy. This composite relative dose intensity measure was in turn determined by emesis and an index for other toxicities, while no other factors examined had any statistically significant impact.
This could be seen as evidence corroborating the hypothesis, but something similar is not found when analyzing the other trials. In the testis cancer trial, this type of analysis is hardly feasible because of too little variation in the extent of adherence to the protocol therapy schedule and because very few outcome events have occurred after a median follow-up period of more than 7 years. Neither was this kind of relation found in the ovarian cancer trial; however, in this case, the assessment of patients’ adherence to protocol therapy was much more uncertain because of ambiguities in the determination of what the protocol actually stipulated.
With respect to the impact of emesis on the amount of time spent in hospital by the patients, the evidence provided by this study is equally mixed. The obvious expected effect found in the bivariate analyses with the patient or the cycle of chemotherapy as analytical unit almost invariably disappears, when possible confounding factors are appropriately controlled for in multivariate analyses, which point to other severe toxicities as the most important determinant of the length of hospital stays. Only in the testis cancer trial does emesis remain a statistically significant determinant in addition to other, more important, factors.
An important caveat regarding this relative lack of evidence for an expected impact of emesis, however, is that the data recorded do not allow a distinction to be made between acute and delayed emesis. Acute emesis is usually defined as nausea and vomiting that occur within 24 h after the end of infusion of chemotherapy, while emesis is considered delayed if it starts later than this. Delayed emesis that starts after the patient has left the hospital will probably only lead to rehospitalization in the most severe cases; thus, delayed emesis will only have very little impact on the average time spent in hospital by a large group of patients. Where the antiemetics used have been recorded, setron-based regimens dominate completely; however, the setrons do not provide much protection against delayed emesis [4], and it cannot be excluded that the problems experienced by the patients in these trials have predominantly been delayed emesis.
Clearly, the ultimate goal of full control of emesis is still far from being attained, with about half of the patients suffering from emesis during part of the course of chemotherapy and a smaller group of patients having received barely any control at all.
In conclusion, the hypothesis of a detrimental impact of emesis on the clinical outcomes for cancer patients undergoing emetogenic chemotherapy is only partially corroborated by this study. Further studies on the empirical evidence for or against the hypothesis are warranted, before a final assessment of its validity can be made. It is clear from the analyses reported here that it is imperative that such studies be carried out with careful control of confounding variables by applying appropriate multivariate techniques of analysis.
Notes
The p values presented for the statistical tests are without correction for multiple testing, which makes it likely that some of the statistically significant associations found occur simply by chance.
This procedure had not yet been introduced at the time of initiation of the other trials, in the course of which only the occurrence or not of a SAE was recorded.
But statistical tests of this become meaningless because only 12 patients went off protocol for these reasons.
Patients were always hospitalized for a minimum of one night, when given the cisplatin-based regimens of chemotherapy, while the regimen without cisplatin was mostly given on an outpatient basis.
According to the subjective assessment of the clinician recording the patient’s data.
References
Anderson JR, Cain KC, Gelber RD (1983) Analysis of survival by tumor response. J Clin Oncol 1:710–719
Ballatori E, Roila F (2003) Impact of nausea and vomiting on quality of life in cancer patients during chemotherapy. Health Qual Life Outcomes 1:46
De Wit R, Roberts T, Wilkinson P et al (2001) Equivalence of three or four cycles of bleomycine, etoposide and cisplatin chemotherapy and of a 3- or 5-day schedule in good-prognosis germ cell cancer: a randomized study of the European Organization for Research and Treatment of Cancer Genitourinary Tract Cancer Cooperative Group and The Medical Research Council. J Clin Oncol 19:1629–1640
Kris MK (2003) Why do we need another antiemetic? Just ask. (editorial) J Clin Oncol 21(22):4077–4080
Piccart MJ, Bertelsen K, James K, Cassidy J, Mangioni C, Simonsen E et al (2000) Randomized intergroup trial of cisplatin–paclitaxel versus cisplatin–cyclophosphamide in women with advanced epithelial ovarian cancer: three year results. J Natl Cancer Inst 92:699–708
Schnell FM (2003) Chemotherapy-induced nausea and vomiting: the importance of acute antiemetic control. The Oncologist 8:187–198
Smit EF, van Meerbeeck PAM, Lianes P, Debruyne C, Legrand C, Schramel F, Smit H, Gaafaar R, Biesma B, Manegold C, Neymark N, Giaccone G (2003) Three-arm randomized study of two cisplatin-based regimens and paclitaxel plus gemcitabine in advanced non-small cell lung cancer: a phase III trial of the European Organization for Research and Treatment of Cancer Lung Cancer Group—EORTC 08975. J Clin Oncol 21:3909–3917
Uyl-de-Groot CA, Wait S, Buijt I (2000) Economics and health-related quality of life in antiemetic therapy: recommendations for trial design. Eur J Cancer 36:1522–1535
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neymark, N., Crott, R. Impact of emesis on clinical and economic outcomes of cancer therapy with highly emetogenic chemotherapy regimens: a retrospective analysis of three clinical trials. Support Care Cancer 13, 812–818 (2005). https://doi.org/10.1007/s00520-005-0803-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-005-0803-x