Abstract
Purpose
Esophageal cancer has a high mortality rate, and its multimodality treatment is often associated with significant rates of severe toxicity. Effort is needed to uncover ways to maximize effectiveness of therapy through identification of predictive markers of response and toxicity. As such, the aim of this study was to identify genes predictive of chemoradiotherapy-induced gastrointestinal toxicity using an immune pathway-targeted approach.
Methods
Adults with esophageal cancer treated with chemotherapy consisting of 5-fluorouracil and cisplatin and 45–50 Gy radiation were recruited to the study. Pre-therapy-collected whole blood was analyzed for relative expression of immune genes using real-time polymerase chain reaction (RT-PCR). Gene expression was compared between patients who experienced severe regimen-related gastrointestinal toxicity vs. those experiencing mild to moderate toxicity.
Results
Blood from 31 patients were analyzed by RT-PCR. Out of 84 immune genes investigated, TNF was significantly elevated (2.05-fold, p = 0.025) in the toxic group (n = 12) compared to the non-toxic group (n = 19). Nausea and vomiting was the most commonly documented severe toxicity. No associations between toxicity and response, age, sex, histology, or treatment were evident.
Conclusions
This study supports evidence of TNF as a predictive biomarker in regimen-related gastrointestinal toxicity. Confirming these findings in a larger cohort is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Across the past four decades, the incidence of esophageal adenocarcinoma (EAC) has increased 6-fold throughout the Western World, particularly in men, while rates of squamous cell carcinoma (SCC) of the esophagus remain unchanged [1]. Esophageal cancer has one of the poorest survival rates among patients with solid tumors, and its multimodality treatment with combined chemotherapy and radiotherapy is often associated with significant rates of severe toxicity [2, 3]. Effort is needed to uncover ways to maximize the effectiveness of therapy through identification of predictive markers of response and toxicity.
Acute toxicity affecting the gastrointestinal (GI) mucosa is a major impediment to optimal cancer treatment and is particularly problematic in cancers of the esophagus. Patients with locally advanced tumors are typically managed with neoadjuvant or definitive chemoradiotherapy (CRT) [4, 5], which results in up to 43 % of patients experiencing severe (grade ≥3) GI toxicity (including oral mucositis, esophagitis, nausea and vomiting, and diarrhea) depending on the protocol [6]. Of significant clinical importance, GI toxicity can lead to up to 45 % of patients not receiving full-dose chemotherapy and up to 30 % having interrupted radiotherapy [3, 7], and this can negatively impact on treatment success. Complete pathological response to CRT is associated with better long-term survival [8]. However, 25 % of patients do not respond to CRT and hence undergo this treatment and its toxicities unnecessarily [9].
Reliable predictive markers of severe GI toxicity risk are currently unavailable. One potential approach is the use of gene expression signatures [10–12]. Numerous lines of evidence support the role of basal gene expression in establishing a pre-treatment risk profile, and a number of studies have found associations between genetic factors and regimen-related toxicity [13–15]. Recently, attention has moved away from pharmacogenetic risk gene such as dihydropyrimidine dehydrogenase (DPYD) due to the rarity of informative variants and consequent failure to account for the majority of toxicity seen [16]. Instead, increased focus has been placed on the role of immune determinants of mucosal inflammation. This is borne out of the knowledge that GI toxicity (most notably mucositis) is fundamentally underpinned by mucosal inflammatory damage. Substantial pre-clinical and clinical research has shown that many of the key mediators of regimen-related mucosal injury are derived from the innate immune response pathway [17]. In particular, activation of the transcription factor NF-κB and upregulation of its pro-inflammatory cytokine target genes including TNF-α, IL-1β, and IL-6 are implicated in modulating injury [18, 19]. Furthermore, the severity of mucosal injury correlates with the intensity of pro-inflammatory cytokine production, and interference with cytokine production favorably modifies the course of experimental mucositis [20]. In clinical studies, increased levels of TNF-α and IL-6 measured in peripheral blood correlates with mucositis severity [21, 22]. These findings implicate pro-inflammatory cytokines as central medicators in the pathogenesis of cancer therapy-induced GI toxicity and promote their further investigation as risk modifiers. In support of observations from mRNA and animal models, genetic variants in mucosal injury mediators, such as TNF-α, NF-κB, IL-1β, and IL-6, have been linked to toxicity [13, 23, 24].
Based on these previous studies, we hypothesized that pre-therapy expression of innate immune genes would be measurably different in patients that go on to suffer from severe GI toxicity compared to those that do not. As such, this proof of concept pilot study used an immune pathway-targeted, multiarray approach to prospectively analyze pre-therapy gene expression profiles in patients with esophageal cancer treated with CRT.
Methods
Patient identification and sample collection
This study was approved by the Royal Adelaide Hospital Research Ethics Committee and complied with the Declaration of Helsinki. All study participants gave written informed consent. Eligible participants were identified at the South Australian Statewide Upper Gastrointestinal Cancer Multidisciplinary Team Meeting or by endoscopy surgical lists and approached for inclusion at the hospital or by mailed study information sheets. Patients with cancer of the esophagus (including adenocarcinoma, squamous cell carcinoma, and gastroesophageal junction) scheduled to receive concurrent CRT were eligible for inclusion. Chemotherapy entailed 2 cycles of 5-fluorouracil (4000 mg/m2 over 96–120 h by ambulatory pump) and cisplatin (75–80 mg/m2) spaced 4 weeks apart. Radiation consisted of 45 Gy, if given before surgical resection, and 50 Gy if given as definitive treatment, administered as 25 equal fractions across 5 weeks. Pre-treatment supportive medication was standard and consisted of 165 mg aprepitant, 12 mg dexamethasone, and 10 mg ondansetron/250 mcg palonosetron. Post infusion medication included 165 mg aprepitant, 10–20 mg metoclopramide (as required for nausea), 8 mg dexamethasone (two tablets daily × 3 days), and 2–4 mg loperamide (as required for diarrhea). Patients who had received prior chemotherapy or radiation, had a serious concomitant medical or psychiatric illness, or had active mucosal ulceration were excluded. Patients were prospectively recruited and gave 2.5 mL of blood, collected into PaxGene RNA tubes for stabilization of RNA (PreAnalytiX, Qiagen) prior to therapy.
Clinical records were reviewed for collection of clinical information, including patient demographics, chemotherapy and radiation protocol, tumor histology, and toxicity. Two specialist esophageal surgeons independently reviewed the clinical records to determine response to CRT, as summarized in Table 1. All toxicity data was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0. To maintain uniformity, a single investigator [IW] was responsible for data extraction and final toxicity scoring as directed by physician reporting in case notes. For the purpose of analysis, patients were categorized as either toxic or non-toxic. Patients with any reported GI toxicity grade ≥3 were assigned as toxic, whereas patients with grade ≤2 toxicity were assigned as “non-toxic”. Any patient that required a dose reduction, treatment break, or hospitalization due to GI toxicity was automatically assigned to the toxic group. The Fisher’s exact test was used to compare patient characteristics between groups.
RNA isolation
Total RNA was isolated from whole blood using the PreAnalytiX RNA extraction kit as per manufacturers’ instructions (Qiagen, CA, USA). Briefly, silica-membrane spin column technology is used, where RNA >18 nucleotides (including miRNA) binds to the membrane, and is subjected to DNase digestion to remove genomic DNA contamination and washed before final elution in proprietary buffer solution. Integrity of eluted RNA was tested with the Agilent Bioanalyzer at the Adelaide Microarray Centre (University of Adelaide).
PCR arrays and RT-PCR
The RT2 Profiler™ PCR Array Human Innate & Adaptive Immune Responses in 100 disk format (Qiagen, CA, USA) was used to compare relative transcript expression between groups. All arrays were conducted according to manufacturers’ instructions, including complementary DNA (cDNA) synthesis using the RT2 HT First Strand Kit and use of SYBR Green ROX FASTMastermix for the Rotor-Gene cycler. Cycle threshold values were analyzed by 2−∆∆CT to determine expression fold changes and unpaired t test used to detect significance between groups, respectively.
For real-time polymerase chain reaction (RT-PCR) validation of differentially expressed transcripts, RNA was converted to cDNA using the iScript cDNA synthesis kit (Biorad, CA, USA) as per manufacturers’ instructions. Primers were purchased from Qiagen (QuantiTect Primer Assays) with expression normalized to housekeeping gene, UBC, which has been extensively used in our laboratory [25], although not present on the PCR array. All RT-PCR reactions contained 1 μl (10 ng) cDNA, 5 μl Sybr Green, 3 μl RNase-free water, and 1 μl of primer mix. Using the Rotor-Gene Q (Qiagen, CA, USA), each run consisted of 40 cycles: 95 °C (15 s), 55 °C (30 s), and 72 °C (30 s). Cycle threshold cutoff was set while viewing fluorescent readings in log scale. A melt curve analysis was conducted to ensure amplification of specific products. Normalized expression values were assessed by Wilcoxon signed-rank test, with a p value of <0.05 considered significant.
Results
Patient toxicity
Between December 2009 and March 2013, a total of 31 blood samples were collected from eligible patients (Fig. 1). These were classified as toxic (n = 12) or non-toxic (n = 19) and included in the molecular analysis (full description in supplementary Table 1). Patients were well balanced across the two groups for age, tumor histology, clinical stage, and treatment (Table 2). Grade ≥3 nausea or vomiting occurred in 8/31 (26 %) patients, making it the most common severe GI toxicity documented. This was as expected given that the regimen is highly emetogenic. All GI toxicities that occurred with frequency of 10 % or greater are shown in Table 3.
PCR array
Initially, RNA from four toxic and four non-toxic patients was compared in the PCR array analysis which included 84 innate and adaptive immune response genes and five housekeeping genes. A filter was applied so that genes with less than 75 % detection rate (three out of four arrays in each group) were classified as absent. This limit resulted in 25 genes being excluded from analysis (Supplementary Table 2). Three housekeeping genes were stable and used for normalization: B2M (−1.11-fold), ACTB (−1.05-fold), and GAPDH (1.17-fold). Two housekeeping genes, RPL13A and HPRT1, were excluded due to a significant difference in expression (average CT value difference greater than 2) between the two groups. Three innate immunity genes were significantly upregulated in the toxic group compared to the non-toxic group: NFKB1 (1.67-fold, p = 0.01), IL1B (2.19-fold, p = 0.029), and TNF (2.14-fold, p = 0.042). No genes were significantly downregulated in the toxic group.
RT-PCR validation
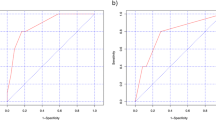
The three genes identified as significantly upregulated by PCR array were then investigated in all toxic and non-toxic samples by semi-quantitative RT-PCR. TNF expression was significantly increased in the toxic group (2.05-fold, p = 0.025), whereas IL1B and NFKB1expression was similar between groups (Fig. 2). The housekeeping gene, UBC, was stable (−1.27-fold).
Response to CRT
Response data was available for 29 patients. Complete or near complete response was 31 %, partial response (including minimal, moderate, good partial, and poor partial) was 62 %, and poor or no response was 7 %. Severe GI toxicity was not associated with the response of the tumor to CRT treatment (Table 4).
Discussion
GI toxicity is a collection of adverse effects of cancer treatment that seriously impact on patient quality of life and treatment compliance. This study included the most commonly experienced acute GI symptoms associated with 5-FU, cisplatin, and radiation therapy, namely nausea and vomiting, diarrhea, and mucositis/esophagitis [3, 6, 7], to uncover genes that would act as pre-therapy predictive markers of GI toxicity. We found that severe GI toxicity occurred frequently within our cohort, with 39 % of patients experiencing at least one of the symptoms at a severe level within the first cycle of treatment. Importantly, each of the GI toxicity symptoms occurred within the wide range of frequency expected for the regimen [3]. Most patients did not experience toxicities singularly, but rather two or more toxicities were reported within the first cycle of therapy. This is consistent with previous studies that have shown that toxicities do not occur in isolation and are likely to be biologically linked, perhaps through systemic cytokine production and release [26, 27]. In regards to potential underpinning mechanisms between TNF and nausea and vomiting, this has not been studied directly to date. However, in a phase I clinical trial of systemic TNF for solid tumors, nausea and vomiting were of the most common toxicities, indicating a possible relationship between TNF levels and this symptom [28]. In the present study, toxicity that developed only within the first 4 weeks of treatment was included in the analysis. As such, late onset radiation esophagitis may have been under reported. This is a serious and dose-limiting toxicity for patients receiving thoracic radiation and is associated with fibrotic changes that can present months to years following completion of radiotherapy [29]. Acute radiation esophagitis has also been reported to occur during or just after the completion of therapy and is highly dose-dependent [15], although the etiology is difficult to separate from mucosal injury in other areas including the oral cavity and pharynx. In response to this, previous clinical trials have classified mucositis and acute esophagitis as a single entity [30, 31] and shown incidence rates similar to that seen in our study.
In our cohort of patients, we found that pre-therapy elevated expression of pro-inflammatory genes was associated with toxicity. In particular, TNF was consistently elevated in patients that experienced severe CRT-induced GI toxicity. In contrast, IL1B and NFKB1 were only elevated in the PCR array. PCR arrays were not conducted on the full cohort of patients, and the PCR array cohort was more homogeneous than the full cohort by only including males and a maximum of grade 1 toxicity in the non-toxic group. This may have led to a much wider separation in gene expression signatures compared to the full cohort, which included females and grade 2 toxicity. The observation of elevated TNF supports findings by other investigators that have shown evidence of inflammatory markers as risk predictors of treatment toxicity. An association between the TNFA-1031T > C promoter polymorphism, which is known to alter protein levels, and toxicity has been shown in Japanese patients with esophageal cancer treated by CRT [13]. Investigators used a multivariate logistic regression model to show that TNFA-1031T > C was significantly associated with oral mucositis and this was the only significant independent risk factor identified. Furthermore, patients heterozygous for the TNFA-308G > A promoter polymorphism (known to increase expression of TNF-α) are at significantly increased risk of severe toxicity affecting the mucosa following myeloablative chemotherapy for HSCT [23]. In a study investigating genetic variation and risk of radiation esophagitis in patients with non-small cell lung cancer, investigators identified the TNFA-857C > T promoter polymorphism [24]. They found no significant differences between patients who developed severe esophagitis and those who did not with regard to age, sex, smoking status, histology, clinical stage, and performance status. In addition, previous research using samples collected from patients with esophageal cancer treated with neoadjuvant chemotherapy found monocytes with increased capacity to secrete IL-12 and reduced IL-10 in response to lipopolysaccharide and interferon that were predictive of severe mucositis [32]. Collectively, these studies strongly support a role for elevated TNF signaling as an important risk factor for CRT-induced GI toxicity. However, it is important to note the limitation of our current approach, which is the use of housekeeping genes for normalization of data. Future research will utilize a quantitative approach to improve accuracy and reproducibility of results.
With regard to toxicity severity, grade ≥3 GI toxicities are reported to occur at a rate of anywhere between 6 and 50 % [3, 33–37], showing high interstudy and interpatient variability. This may be partially explained by the different regimens in use as well as the difficulty of assessing GI toxicities, which rely on the subjective description given by the patients and lack of quantitative tests for the assessment of nausea, vomiting, and diarrhea. There is currently no effective tool to stratify patients for toxicity, and traditional treatment-based and patient-based factors are poor predictors [38]. Our study found no associations between toxicity and age, sex, tumor histology, stage, or treatment, which is in line with previous studies [39–41]. However, it should be noted that we did not look specifically for associations between gene expression, and these same variables separate to toxicity. Given that gene expression profiles have been used previously to generate predictive models of patient response to CRT [42–44], this approach may be equally able to generate predictive models of toxicity from CRT in patients. We chose the arbitrary cutoff of CTCAE grade 3 toxicity to categorize patients as toxic. As such, the non-toxic group contained a mixture of no (grade 0), mild (grade 1), and moderate (grade 2) GI toxicities, which may have caused reduced separation in marker expression. Comparison of our findings to other studies is also made difficult by the use of different toxicity scoring systems and variation in group allocation thresholds.
Finally, we found no association between severe GI toxicity and response to CRT, although our study size was underpowered to detect this. The roughly 30 % complete or near complete response rate seen in our study is in line with previous clinical studies for esophageal cancer [45]. Our findings are in contrast to a recent study that found that acute toxicity may be a significant prognostic factor for response and overall survival in patients with esophageal cancer [41]. Investigators showed that patients with worsening odynophagia (described as mucositis of the esophagus) during CRT were more likely to have tumor regression grade 1 and improved 5-year survival. Importantly, this was the only independent prognostic factor identified. As such, there is merit in investigating the relationship between acute tissue toxicity and tumor response in clinical trials to help delineate supportive care approaches for patients with esophageal cancer.
In conclusion, this study has provided supporting evidence for TNF as a gene associated with GI toxicity risk. Use of molecular, blood-based biomarkers such as gene expression is a quick and non-invasive method for obtaining toxicity risk information and could be easily translated to a diagnostic tool. Although these initial results are positive, the interpretation of our findings is limited given the small sample size of this pilot study which will require confirmation in a larger cohort.
References
El-Serag HB (2007) Time trends of gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol 5:17–26
Monjazeb AM, Blackstock AW (2013) The impact of multimodality therapy of distal esophageal and gastroesophageal junction adenocarcinomas on treatment-related toxicity and complications. Semin Radiat Oncol 23:60–73
Courrech Staal EF, Aleman BM, Boot H, van Velthuysen ML, van Tinteren H, van Sandick JW (2010) Systematic review of the benefits and risks of neoadjuvant chemoradiation for oesophageal cancer. Br J Surg 97:1482–1496
Fiorica F, Di Bona D, Schepis F, Licata A, Shahied L, Venturi A, Falchi AM, Craxi A, Camma C (2004) Preoperative chemoradiotherapy for oesophageal cancer: a systematic review and meta-analysis. Gut 53:925–930
van Soest EM, Dieleman JP, Siersema PD, Sturkenboom MC, Kuipers EJ (2005) Increasing incidence of barrett's oesophagus in the general population. Gut 54:1062–1066
Morgan MA, Lewis WG, Casbard A, Roberts SA, Adams R, Clark GW, Havard TJ, Crosby TD (2009) Stage-for-stage comparison of definitive chemoradiotherapy, surgery alone and neoadjuvant chemotherapy for oesophageal carcinoma. Br J Surg 96:1300–1307
Hiura Y, Takiguchi S, Yamamoto K, Kurokawa Y, Yamasaki M, Nakajima K, Miyata H, Fujiwara Y, Mori M, Doki Y (2012) Fall in plasma ghrelin concentrations after cisplatin-based chemotherapy in esophageal cancer patients. Int J Clin Oncol 17:316–323
Thompson SK, Ruszkiewicz AR, Jamieson GG, Esterman A, Watson DI, Wijnhoven BP, Lamb PJ, Devitt PG (2008) Improving the accuracy of tnm staging in esophageal cancer: a pathological review of resected specimens. Ann Surg Oncol 15:3447–3458
Gebski V, Burmeister B, Smithers BM, Foo K, Zalcberg J, Simes J (2007) Australasian Gastro-Intestinal Trials G: Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis. Lancet Oncol 8:226–234
Cortez MA, Scrideli CA, Yunes JA, Valera ET, Toledo SR, Pavoni-Ferreira PC, Lee ML, Petrilli AS, Brandalise SR, Tone LG (2009) Mrna expression profile of multidrug resistance genes in childhood acute lymphoblastic leukemia. Low expression levels associated with a higher risk of toxic death. Pediatr Blood Cancer 53:996–1004
Hummerich J, Werle-Schneider G, Popanda O, Celebi O, Chang-Claude J, Kropp S, Mayer C, Debus J, Bartsch H, Schmezer P (2006) Constitutive mrna expression of DNA repair-related genes as a biomarker for clinical radio-resistance: a pilot study in prostate cancer patients receiving radiotherapy. Int J Radiat Biol 82:593–604
Rieger KE, Hong WJ, Tusher VG, Tang J, Tibshirani R, Chu G (2004) Toxicity from radiation therapy associated with abnormal transcriptional responses to DNA damage. Proc Natl Acad Sci U S A 101:6635–6640
Sakamoto K, Oka M, Yoshino S, Hazama S, Abe T, Okayama N, Hinoda Y (2006) Relation between cytokine promoter gene polymorphism and toxicity of 5-fluorouracil plus cisplatin chemotherapy. Oncol Rep 16:381–387
Schwab M, Zanger UM, Marx C, Schaeffeler E, Klein K, Dippon J, Kerb R, Blievernicht J, Fischer J, Hofmann U, Bokemeyer C, Eichelbaum M (2008) German FUTSG: Role of genetic and nongenetic factors for fluorouracil treatment-related severe toxicity: a prospective clinical trial by the german 5-fu toxicity study group. J Clin Oncol 26:2131–2138
Zhang L, Yang M, Bi N, Ji W, Wu C, Tan W, Zhao L, Yu D, Lin D, Wang L (2010) Association of tgf-beta1 and xpd polymorphisms with severe acute radiation-induced esophageal toxicity in locally advanced lung cancer patients treated with radiotherapy. Radiother Oncol 97:19–25
Ezzeldin HH, Diasio RB (2008) Predicting fluorouracil toxicity: can we finally do it? J Clin Oncol 26:2080–2082
Sonis ST (2007) Pathobiology of oral mucositis: novel insights and opportunities. J Support Oncol 5:3–11
Logan RM, Stringer AM, Bowen JM, Yeoh AS, Gibson RJ, Sonis ST, Keefe DM (2007) The role of pro-inflammatory cytokines in cancer treatment-induced alimentary tract mucositis: pathobiology, animal models and cytotoxic drugs. Cancer Treat Rev 33:448–460
Sonis ST (2002) The biologic role for nuclear factor-kappab in disease and its potential involvement in mucosal injury associated with anti-neoplastic therapy. Crit Rev Oral Biol Med 13:380–389
Sonis ST (2004) The pathobiology of mucositis. Nat Rev Cancer 4:277–284
Meirovitz A, Kuten M, Billan S, Abdah-Bortnyak R, Sharon A, Peretz T, Sela M, Schaffer M, Barak V (2010) Cytokines levels, severity of acute mucositis and the need of peg tube installation during chemo-radiation for head and neck cancer—a prospective pilot study. Radiat Oncol 5:16
Morales-Rojas T, Viera N, Moron-Medina A, Alvarez CJ, Alvarez A (2012) Proinflammatory cytokines during the initial phase of oral mucositis in patients with acute lymphoblastic leukaemia. Int J Paediatr Dent Br Paedodontic Soc Int Assoc Dent Child 22:191–196
Bogunia-Kubik K, Polak M, Lange A (2003) Tnf polymorphisms are associated with toxic but not with agvhd complications in the recipients of allogeneic sibling haematopoietic stem cell transplantation. Bone Marrow Transplant 32:617–622
Hildebrandt MA, Komaki R, Liao Z, Gu J, Chang JY, Ye Y, Lu C, Stewart DJ, Minna JD, Roth JA, Lippman SM, Cox JD, Hong WK, Spitz MR, Wu X (2010) Genetic variants in inflammation-related genes are associated with radiation-induced toxicity following treatment for non-small cell lung cancer. PLoS One 5:e12402
Al-Dasooqi N, Bowen JM, Gibson RJ, Logan RM, Stringer AM, Keefe DM (2011) Selection of housekeeping genes for gene expression studies in a rat model of irinotecan-induced mucositis. Chemotherapy 57:43–53
Aprile G, Ramoni M, Keefe D, Sonis S (2008) Application of distance matrices to define associations between acute toxicities in colorectal cancer patients receiving chemotherapy. Cancer 112:284–292
Aprile G, Ramoni M, Keefe D, Sonis S (2009) Links between regimen-related toxicities in patients being treated for colorectal cancer. Curr Opin Support Palliat Care 3:50–54
Keefe DM, Elting LS, Nguyen HT, Grunberg SM, Aprile G, Bonaventura A, Selva-Nayagam S, Barsevick A, Koczwara B, Sonis ST (2014) Risk and outcomes of chemotherapy-induced diarrhea (CID) among patients with colorectal cancer receiving multi-cycle chemotherapy. Cancer Chemother Pharmacol 74:675–680
Bradley J, Movsas B (2004) Radiation esophagitis: predictive factors and preventive strategies. Semin Radiat Oncol 14:280–286
Meluch AA, Greco FA, Gray JR, Thomas M, Sutton VM, Davis JL, Kalman LA, Shaffer DW, Yost K, Rinaldi DA, Hainsworth JD (2003) Preoperative therapy with concurrent paclitaxel/carboplatin/infusional 5-fu and radiation therapy in locoregional esophageal cancer: final results of a minnie pearl cancer research network phase ii trial. Cancer J 9:251–260
Brucher BL, Stein HJ, Zimmermann F, Werner M, Sarbia M, Busch R, Dittler HJ, Molls M, Fink U, Siewert JR (2004) Responders benefit from neoadjuvant radiochemotherapy in esophageal squamous cell carcinoma: results of a prospective phase-ii trial. Eur J Surg Oncol 30:963–971
Schauer MC, Holzmann B, Peiper M, Friess H, Knoefel WT, Theisen J (2010) Interleukin-10 and -12 predict chemotherapy-associated toxicity in esophageal adenocarcinoma. J Thorac Oncol 5:1849–1854
Adelstein DJ, Rice TW, Rybicki LA, Saxton JP, Videtic GM, Murthy SC, Mason DP, Rodriguez CP, Ives DI (2009) Mature results from a phase ii trial of postoperative concurrent chemoradiotherapy for poor prognosis cancer of the esophagus and gastroesophageal junction. J Thorac Oncol 4:1264–1269
Crosby TD, Brewster AE, Borley A, Perschky L, Kehagioglou P, Court J, Maughan TS (2004) Definitive chemoradiation in patients with inoperable oesophageal carcinoma. Br J Cancer 90:70–75
Hurmuzlu M, Monge OR, Smaaland R, Viste A (2010) High-dose definitive concomitant chemoradiotherapy in non-metastatic locally advanced esophageal cancer: toxicity and outcome. Dis Esophagus 23:244–252
Ishida K, Ando N, Yamamoto S, Ide H, Shinoda M (2004) Phase ii study of cisplatin and 5-fluorouracil with concurrent radiotherapy in advanced squamous cell carcinoma of the esophagus: a japan esophageal oncology group (jeog)/japan clinical oncology group trial (jcog9516). Jpn J Clin Oncol 34:615–619
Kato H, Sato A, Fukuda H, Kagami Y, Udagawa H, Togo A, Ando N, Tanaka O, Shinoda M, Yamana H, Ishikura S (2009) A phase ii trial of chemoradiotherapy for stage i esophageal squamous cell carcinoma: Japan clinical oncology group study (jcog9708). Jpn J Clin Oncol 39:638–643
Sonis ST, Elting LS, Keefe D, Peterson DE, Schubert M, Hauer-Jensen M, Bekele BN, Raber-Durlacher J, Donnelly JP, Rubenstein EB (2004) Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer 100:1995–2025
Doyen J, Benezery K, Follana P, Ortholan C, Gerard JP, Hannoun-Levi JM, Gal J, Francois E (2013) Predictive factors for early and late local toxicities in anal cancer treated by radiotherapy in combination with or without chemotherapy. Dis Colon Rectum 56:1125–1133
Schwab M, Zanger UM, Marx C, Schaeffeler E, Klein K, Dippon J, Kerb R, Blievernicht J, Fischer J, Hofmann U, Bokemeyer C, Eichelbaum M (2008) Role of genetic and nongenetic factors for fluorouracil treatment-related severe toxicity: a prospective clinical trial by the german 5-fu toxicity study group. J Clin Oncol 26:2131–2138
Hennies S, Hermann RM, Gaedcke J, Grade M, Hess CF, Christiansen H, Wolff HA (2014) Increasing toxicity during neoadjuvant radiochemotherapy as positive prognostic factor for patients with esophageal carcinoma. Dis Esophagus 27:146–151
Duong C, Greenawalt DM, Kowalczyk A, Ciavarella ML, Raskutti G, Murray WK, Phillips WA, Thomas RJ (2007) Pretreatment gene expression profiles can be used to predict response to neoadjuvant chemoradiotherapy in esophageal cancer. Ann Surg Oncol 14:3602–3609
Maher SG, Gillham CM, Duggan SP, Smyth PC, Miller N, Muldoon C, O'Byrne KJ, Sheils OM, Hollywood D, Reynolds JV (2009) Gene expression analysis of diagnostic biopsies predicts pathological response to neoadjuvant chemoradiotherapy of esophageal cancer. Ann Surg 250:729–737
Motoori M, Takemasa I, Yamasaki M, Komori T, Takeno A, Miyata H, Takiguchi S, Fujiwara Y, Yasuda T, Yano M, Matsuura N, Matsubara K, Monden M, Mori M, Doki Y (2010) Prediction of the response to chemotherapy in advanced esophageal cancer by gene expression profiling of biopsy samples. Int J Oncol 37:1113–1120
van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, Richel DJ, Nieuwenhuijzen GA, Hosper GA, Bonenkamp JJ, Cuesta MA, Blaisse RJ et al (2012) Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366:2074–2084
Acknowledgments
We acknowledge the assistance provided by Bronwen Jones and Jeff Bull in patient identification, Associate Professor Peter Devitt and DrNimitSinghal for patient recruitment, Mr Tim Bright for tumor response classification, and Mark Van der Hoek for RNA bioanalysis.
Conflict of interest
The authors have no conflict of interest associated with publication of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(DOCX 22 kb)
Supplementary Table 2
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Bowen, J.M., White, I., Smith, L. et al. Pre-therapy mRNA expression of TNF is associated with regimen-related gastrointestinal toxicity in patients with esophageal cancer: a pilot study. Support Care Cancer 23, 3165–3172 (2015). https://doi.org/10.1007/s00520-015-2696-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2696-7