Abstract
Purpose
This randomized controlled trial tested the effects of a specially designed strength and endurance training on the independence and quality of life in lung cancer patients in stages IIIA/IIIB/IV during palliative chemotherapy.
Methods
Between August 2010 and December 2011, 46 patients were randomized into two groups receiving either conventional physiotherapy or special physiotherapeutic training. The Barthel Index served as primary endpoint. The secondary endpoints were the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core-30 (EORTC QLQ C-30/LC-13) questionnaire, the 6-Minute Walk Test (6MWT), stair walking, the Modified Borg Scale, and muscle strength. Nonparametrical data were analyzed with the Wilcoxon and Mann–Whitney U test. For parametric, data student t tests were used. A p value of ≤.05 was accepted.
Results
Twenty-nine patients completed the trial (Intervention group (IG), n = 18; control group (CG), n = 11). Significant differences were detectable in the Barthel Index (IGmean = 92.08; CGmean = 81.67; p = .041), in single scores of the EORTC QLQ C-30/LC-13 questionnaire (physical functioning, p = .025; hemoptysis, p = .019; pain in arms or shoulder, p = .048; peripheral neuropathy, p = .050; cognitive functioning, p = .050), in the 6MWT, stair walking, strength capacity, and in the patient’s dyspnoea perception during submaximal walking activities (IG > CG).
Conclusion
According to these findings, lung cancer patients should receive enhanced physical activity intervention during palliative chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
Chemotherapy in patients with unresectable lung cancer stages III and IV may improve survival and palliates symptoms [1–3]. Nevertheless, two problems, which are directly related to the disease itself and side effects of chemotherapy, are not yet faced within most treatment approaches: the patient’s activity level is tremendously limited while receiving chemotherapy [4] and the reduced ability to perform activities of daily living leads to a diminished quality of life [5]. Both problems can be addressed within one treatment approach.
Formerly, lung cancer patients were advised to take physical rest to reduce symptoms such as dyspnoea and exhaustion. Thus, negative consequences were often not taken into consideration: a lack of exercise leads to a fast progressing muscular atrophy [6]. Activities of daily life are therefore harder or even impossible to perform [7]. A vicious circle is created which might be used to explain the connection of physical inactivity and the worsening of symptoms and side effects.
By developing a specially designed strength and endurance training for advanced lung cancer patients, the patients’ physical capacity should be maintained.
The strength exercises should have a positive impact on the patients’ muscle strength, while the endurance training should keep the patients’ submaximal exercise tolerance.
Since lung cancer is frequently diagnosed in the advanced stage, patients often do not meet the criteria for surgery. The need for high quality palliative and supportive care to minimize symptom distress, to maintain the patients’ physical capacity, and especially to promote quality of life becomes apparent. Nowadays, this need is widely accepted during rehabilitation following curative therapy but not yet in palliative cancer care.
Objectives
Although current evidence suggests that exercise training is a safe and feasible therapy for patients with operable lung cancer both before and after pulmonary resection, feasibility studies of well-described exercise training among patients with inoperable disease are still warranted. Although preliminary evidence in this area suggests that exercise therapy may be an important consideration in multidisciplinary management of patients, specific explanations concerning the designed training program are still needed in order to guarantee tolerability, safety, or efficacy [8].
This study tried to fill this gap by examining the feasibility and effects of a specially designed treatment protocol for advanced lung cancer patients on the patient’s quality of life and their ability to be independent in activities of daily living during the time patients received palliative chemotherapy.
Methods
Study design
This clinical trial was a prospective randomized controlled trial which started in August 2010 after receiving approval from the ethic committee. The monocentric research study was conducted at Vivantes Hospital in Neukoelln/Berlin/Germany.
Setting and participants
Between August 2010 and December 2011, 46 lung cancer patients were randomized into either an intervention (IG) or control group (CG). Patients, who were older than 18 years, diagnosed with non-small cell lung cancer (NSCLC) or small cell lung cancer (SCLC) in stage IIIA/IIIB/IV, who received an inpatient palliative platinum-based chemotherapy treatment at the Vivantes Klinikum Neukoelln/Berlin, were eligible. Their diagnoses had to be confirmed histologically, and they had to be in a stable clinical condition (Karnofsky performance index > 50).
We excluded patients who participated in similar clinical studies, suffered from epilepsy, or symptomatic cardiovascular diseases and who were diagnosed with rheumatic disorders. Patients who were confined to bed were also excluded.
A computer-generated randomization took place after the patient had signed the informed consent.
The IG received an additional strength and endurance training program under the supervision of a licensed physiotherapist, whereas the CG received only conventional physiotherapy.
Baseline and end-of-study measures
The Barthel Index served as primary outcome measure to evaluate the effects on the patient’s independence in carrying out activities of daily living (Table 1). The secondary outcome measure of this study was the German version of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core-30 (EORTC QLQ-C30/LC13) questionnaire, which was used to record the patient’s quality of life.
The 6-Minute Walk Test (6MWT) and staircase walking in combination with the Modified Borg Scale (MBS) have been used to test the patient’s endurance capacity and dyspnoea perception. Furthermore, the maximal amount of repetitions possible was recorded for four different exercises. (Table 2)
These outcome measures were taken at baseline and after three cycles of chemotherapy.
Intervention
The additional strength and endurance training took place while the patient received three cycles of chemotherapy. The intervention started with the first day of chemotherapy and ended after completing the third cycle of chemotherapy.
The endurance training and breathing techniques were performed 5 days a week, while the strength training was performed every other day of the week.
In case of fever, infection, a haemoglobin level <8, psychological instability, or clinical complications, the training program was interrupted. Results of patients that participated in less than 75 % of the training sessions were not considered for statistical analysis.
Endurance training
The functional endurance training consisted of two separate exercises, a walking exercise in the hallway and a stair walking exercise.
Each patient had to walk 6 min in the hallway 5 days a week. To train at a moderate intensity, the patient’s maximum heart rate (HRmax) was determined before calculating the right intensity. A formula for estimating HRmax that has high accuracy for nonfit males and females is as follows [9]:
Finally, the Karvonen formula was used to determine the patient’s individual training intensity. The aim was to maintain the patient’s heart rate between 55 and 70 % of his or her heart rate reserve (HRR). The intensity was set depending on the patient’s score on the MBS, a 0 to 10 rated scale to grade the patient’s dyspnoea perception prior, in the middle, and after the walking test. Thus, the lower the patient scored on the MBS, the higher the training’s intensity was set.
With an MBS score of 0, 0.5, or 1, the patient trained at 60 % of his or her HRR. With an MBS score of 2 or 3, the patient trained at 55 % of the individual HRR, and with an MBS score of 4, the patient trained at 50 % of the individual HRR. As soon as the patient scored 5 or higher on the MBS (severe breathlessness), the patient trained at own intensity.
If the patient did not reach the determined training’s heart rate, the treating physiotherapist was in charge to either encourage the patient to increase his or her walking speed, or to slow down in case of increasing dyspnoea.
This way of determining the patient’s individual training’s intensity made it possible to guarantee for a safe and, for the patient, stress-reduced conduction.
The heart rate was measured with a heart rate monitor (model: FT7 by Polar).
Since walking is an activity performed on a daily basis by every participating patient, any effect with regards to the endurance capacity can be measured with the help of the 6MWT. The test was performed according to the Guidelines for the 6-Minute Walk Test [10], and the walked distance was carefully reported after each training session.
Additionally, staircase walking exercises were added to the training to improve both the patient’s strength and endurance.
Each patient had to walk the stairs for 2 min. We made use of a ten-step staircase, which the patient had to walk up and down within these 2 min. The amount of stairs each patient was able to walk within this time period was reported. Again, the MBS was used to determine the individual training’s intensity. The heart rate was also measured with a heart rate monitor (model: FT7 by Polar), which was regularly checked by the treating physiotherapist in order to reach the right training intensity.
Strength training
Moreover, four different endurance strength exercises were combined training trunk stability, leg, arm, and abdominal musculature. Accordingly, a bridging exercise, an abdominal exercise, a biceps curl exercise, and a triceps extension exercise were included. The arm exercises were performed with the help of an elastic band of medium resistance (model, Thera-band; color, green; 4.6 Ibs resistance at 100 % elongation). Emphasis was put on many repetitions, not on an increased weight load. At baseline, patients repeated each exercise as many times as possible in order to find out the maximal amount of repetitions possible for each specific exercise. The maximal amount of repetitions possible was equalized with 100 %. The patient trained at 50 % of his or her maximal capacity. The physiotherapist was in charge of the correct execution of the movements with the aid of a specific algorithm for each exercise. For instance, if the patient was able to perform the bridging exercise 20 times perfectly without compensating, this amount was equalized with 100 %. During the training sessions, the patient trained at 50 % and in this case repeated the exercise 10 times.
Each training session consisted of three sets. After each set, a break of 1 min was held.
After two cycles of chemotherapy, the maximal amount of repetitions possible for each exercise was tested again in order to have a better control of the individual training intensity. In case of any change in the maximal amount of repetitions possible, the training intensity was adjusted for the third cycle of chemotherapy.
Breathing techniques
Physiotherapeutic breathing techniques were added to the treatment. The breathing techniques included the active cycle of breathing (ACBT), which is designed to reduce airway obstruction and improve the clearance of secretions from the lung [11].
Conventional physiotherapy
Conventional physiotherapy was prescribed to patients of both groups in case a patient suffered from severe dyspnoea, which already occurred with a minimal amount of physical activity or even in resting state, or in case of a reduced range of motion in one or more joints. In these situations, patients received breathing techniques or manual therapy. Manual therapy was started if the patient complained about soft tissue or joint problems using special physiotherapeutic techniques. Manual techniques include massage and muscle stretching of soft tissues, distraction, and traction techniques, specific or general high-velocity manipulation and joint mobilization [12].
Statistical analysis and sample size calculation
The statistical data analysis was performed with the commercial software SPSS Statistics 19.0.
Nonparametrical data were statistically analyzed with the Wilcoxon and Mann–Whitney U test. For parametric data, student t tests were used. A significance level of p ≤ .05 was accepted. The delta value was calculated (post-pre/pre), in order to compare differences between the groups.
A power analysis was conducted prior to the research study and was used to determine an appropriate sample size to achieve adequate power. The needed sample size with a high effect size, alpha 0.05, and power of 0.81 is 21 participants in the experimental group and 21 participants in the CG.
Results
Study feasibility
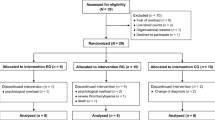
Out of 46 patients, 29 patients completed the trial and were tested again after the intervention (IG, n = 18; CG, n = 11).
Seventeen patients ended the trial early due to death (n = 6), noncompliance (n = 10), or because they continued treatment at a different hospital (n = 1).
Patients that dropped out due to noncompliance refused to repeat the physical assessment for a second time and/or did not attend scheduled appointments with the treating physiotherapist.
The patient flow is illustrated in Fig. 1.
Outcomes
After the intervention, significant differences between the groups were detectable in the Barthel Index (IGmean (SD) = 97.78 (6.24), CGmean (SD) = 81.67 (14.98); p = .003), measuring the patient’s independency in activities of daily living. The CG scored significantly worse on the Barthel Index after the intervention (CGmean pre (SD) = 92.08 (15.15), CGmean post (SD) = 81.67 (14.98); p = .041). Table 1 presents the mean pre–post scores for the Barthel Index. Additionally, significant statistical differences were found in single scores of the EORTC QLQ C-30/LC-13 questionnaire (Physical functioning, p = .025; hemoptysis, p = .019; pain in arms or shoulder, p = .048; peripheral neuropathy, p = .050; cognitive functioning, p = .050). Results can be found in Tables 3 and 4. Table 2 shows the mean pre–post scores for the functional capacity and strength tests. It can be seen that the patients’ endurance capacity and strength results (biceps, triceps) show baseline differences between the groups before and after the intervention started. Differences within the groups show that the IG improved significantly and the CG scored significantly lower after receiving palliative chemotherapy without additional intervention.
Concerning the functional capacity measurements, significant differences were found between the groups concerning the 6MWT, the staircase walking exercise, and strength capacity (IG > CG). Moreover, the level of dyspnoea decreased significantly in the IG while performing submaximal walking activities.
Discussion
Temel et al. reported the only study which tested a specific exercise program for advanced NSCLC patients [13]. Due to the low recruitment rate, the study was closed early and remained uncompleted.
Accordingly, this research study filled the gap by testing the feasibility and effects of a specific strength and endurance training during the time patients received chemotherapy.
The results of this study are consistent with current findings of other studies dealing with different kinds of cancer patients [14].
Although palliative lung cancer treatment aims at improving survival and reducing symptoms, it appears that the treatment frequently focuses on medical and physiological aspects and little attention is given to psychosocial components as well as the patient’s coping mechanisms in daily life activities. The complementary therapy was supposed to contribute to a multidisciplinary treatment approach and tried to integrate the clinical aspect of physiotherapy into the treatment of lung cancer patients.
Overall, the statistical analysis showed significant differences between both groups concerning the primary outcome measure and most of the other outcome measures. Since patients receiving palliative chemotherapy treatment do not have much opportunity or self-motivation to exercise during chemotherapy periods spent at the hospital or even at home, they often complain about a reduction of their endurance capacity, an increase in their level of dyspnoea, and loss of muscle strength [15]. Patients that followed the specially designed treatment protocol were used to these specific exercises, such as walking and climbing stairs. By preventing further muscle atrophy and by building up affected muscle groups, the decrease in muscle strength has been reduced. Patients of the CG reported that they had tremendous difficulties to complete tasks of daily living after completing three cycles of chemotherapy. The immobilization at the hospital, which is promoted by the everyday hospital routines, is a mentionable reason for the progressing atrophy, which is hard to be stopped without specific training. The fact that many patients still believe that physical rest is desirable during cancer treatment is another mechanism that contributes to the complaints and side effects.
Activities of daily living, which have to be performed on a daily basis, such as walking and climbing stairs, were chosen on purpose, since patients should be prepared for their normal lives at home. The results regarding the primary endpoint demonstrate that the vicious circle, which is created through the connection of physical inactivity and the worsening of symptoms and side effects, had been successfully broken.
As mentioned before, the main problem in oncological patients is a general decrease in muscle tissue due to an increase in immobilization during therapy aggravated with each stationary stay at the hospital [9]. Since different types of exercise produce quite different changes in the strength and endurance capacity of a muscle, an individual must choose a type of exercise compatible with the type of activity he or she would like to perform [16]. Accordingly, it is not surprising that the patients, who completed the intervention, improved in the outcome measures or maintained their physical capacity. The maintenance of the patient’s physical capacity is already a valuable achievement.
When looking at the dropout rate in both groups, it is noticeable that more people in the CG dropped out due to noncompliance. It can be assumed that patients of the CG refused to repeat the second assessment due to a drastic worsening of signs and symptoms. The small sample sizes and the higher amount of drop outs in the CG led to the differences in group sizes.
The lower dropout rate in the IG might be due to the fact that personal achievements, such as reaching the first staircase or increasing the distance walked in 6 min resulted in a constantly increasing motivation. Some of the patients were visibly surprised about their physical performance and became more and more enthusiastic about their regained independence.
However, the patient’s individual sporting background, the strength of disease-related symptoms, the treatment’s side effects, the distance between the patient’s home and the hospital, and especially the patient’s mobility level had tremendous influence on the patient’s compliance to the additional training program.
A mentionable limitation to this study was the great variability in the physical capacity and strength results (biceps curl, triceps extension) between groups at baseline. It can be assumed that this variability is due to the small sample size, and outcomes have to be taken with caution. However, the demonstration of significant improvements in the IG and the fact that the CG scored significantly worse after the intervention suggests that further research with larger numbers of subjects is justified.
Montazeri et al. already stated that baseline quality of life was the best predictor of both response to the treatment and survival [15]. Thus, it would be of our interest to start with a well-designed physiotherapy treatment before baseline. In order to improve the patients’ functional capacity and motivation, patients will start to train as early as possible before receiving three cycles of chemotherapy. This research study has already shown the positive effects of such an additional training, which should be the foundation of this more time-consuming program. Due to the small amount of patients, it was not possible to test whether or not the additional training has a different effect in NSCLC or SCLC patients. Future studies are needed to test the effects in each separate patient population. Studies including larger sample sizes could improve the external validity and show an even bigger statistical significant difference between the groups.
Conclusion
The training program has a positive impact on the patient’s independence in carrying out activities of daily living.
Single factors influencing the patient’s quality of life can be significantly improved. In addition, the training has a positive effect on the patient’s endurance and strength capacity. The dyspnoea perception is improved during submaximal walking activities. This study demonstrated that even lung cancer patients receiving a palliative chemotherapy treatment should have enhanced physical activity intervention.
References
Silvestri GA, Tanoue LT, Margolis ML et al (2003) The noninvasive staging of non-small cell lung cancer. The guidelines. Chest 123:147–156
Socinski MA, Morris DE, Masters GA et al (2003) Chemotherapeutic management of stage IV non-small cell lung cancer. Chest 123:226–243
Lung cancer (CG121) (2011) the diagnosis and treatment of lung cancer (update of NICE clinical guideline 24) http://guidance.nice.org.uk/CG121 Accessed 02. November 2012
Rajarejeswaran P, Vishnupriva R (2009) Exercise in cancer. Indian J of Med Paediatr Oncol 30(2):61–70
Kosmidis P (1996) Quality of life as a new end point. Chest 109:110–112
Peterson MD, Rhea MR, Sen A et al (2010) Resistance exercise for muscular strength in older adults: a meta-analysis. Ageing Res Rev 9(3):226–37
Seamark DA, Seamark CJ, Halpin DM (2007) Palliative care in chronic obstructive pulmonary disease: a review for clinicians. J Royal Soc of Med 100(5):225–33
Jones LW, Eves ND, Waner E et al (2009) Exercise therapy across the lung cancer continuum. Curr Oncol Rep 11(4):255–62
Mc Ardle WD, Katch FI, Katch VL (2007) Exercise physiology: energy, nutrition, and human performance, 6th edn. Lippincott Williams & Wilkins, Philadelphia
ATS Statement: Guidelines for the Six-Minute Walk Test 2002 update. www.atsjournals.org. Accessed 25. October 2012
Watson A, Polland K (2001) Physiotherapy (online). Seacroft University Hospitals, Leeds UK
Farrell JP, Jensen GM (1992) Manual therapy: a critical assessment of role in the profession of physical therapy. Phys Ther 72:843–852
Temel JS, Greer JS, Goldberg B et al (2009) A structured exercise program for patients with advanced non-small cell lung cancer. J Thorac Oncol 4(5):595–601
Granger CL, McDonald CF, Bernev S et al (2011) Exercise intervention to improve exercise capacity and health related quality of life for patients with non-small cell lung cancer: a systematic review. Lung Cancer 72:139–153
Montazeri A, Gillis CR, Mc Ewen J (1998) Quality of life in patients with lung cancer: a review of literature from 1970 to 1995. Chest 113:467–481
Widmaier EP, Raff H, Strang KT (2006) Vander’s human physiology: the mechanisms of body function, Tenthth edn. McGraw-Hill, New York
Acknowledgments
The authors would like to thank the patients who gave their precious time to participate in the study.
This study was presented at the 2012 ASCO Annual Meeting in Chicago, USA (poster discussion session) and at the 2012 DGHO Congress in Stuttgart, Germany (poster session).
Conflict of interest
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Henke, C.C., Cabri, J., Fricke, L. et al. Strength and endurance training in the treatment of lung cancer patients in stages IIIA/IIIB/IV. Support Care Cancer 22, 95–101 (2014). https://doi.org/10.1007/s00520-013-1925-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1925-1