Abstract
Purpose
This study aims to describe the depressive symptoms in a sample of African-Caribbean and Latino cancer patients and examine differences in specific symptoms between the two groups.
Methods
The sample included immigrant Afro-Caribbean (n = 44) and Latino (n = 145) underserved cancer patients recruited from five hospitals in New York City. Participants completed a questionnaire comprised of measures of depression (Patient Health Questionnaire-9), health-related quality of life (EuroQol 5D), sociodemographic, and health-related questions.
Results
Results of the comparison of mean scores and percentage of patients meeting the cutoff scores showed that Afro-Caribbean patients reported comparable depressive symptoms to the Latino patients. But, upon closer inspection of specific symptoms and other self-report variables, Latino patients reported more frequently depressed mood, having a history of a depressive disorder, and overall higher psychological distress than Afro-Caribbean patients.
Conclusions
Different presentation of symptoms associated with depression is expressed by Afro-Caribbean and Latino cancer patients. Studies analyzing in detail the presentation of psychological responses of different cultural groups with chronic medical conditions are greatly needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Depression substantially impacts the health of patients with chronic medical conditions, including cancer. Depression not only worsens quality of life [1], but it may lead to poor adherence with anticancer treatment [2, 3]. Although some studies report depression rates up to 58 % among cancer patients [4], Ng [5], with a more conservative approach, estimated a prevalence rate of major depressive disorder in cancer patients at 10.8 %. Literature examining depression rates by ethnic group reveals different symptom presentation prevalence by group [6–9] and more severe, disabling, and underdetected symptoms among racial and ethnic groups [7, 9]. However, there are few studies on depressive symptoms among Latinos and Afro-Caribbean or African-American cancer patients [10–15].
Some researchers recognize that certain symptoms that are consistent with depression are also very similar to those of cancer. Diagnostic criteria for major depression include somatic symptoms (sleep change, energy decrease, appetite change, psychomotor change) that parallel physical responses to the cancer itself and to its treatment. Cancer patients commonly report fatigue, pain, poor appetite, and sleep problems [16–19]. As a result, identifying a depressive disorder among cancer patients can be more difficult than among the general population and is a subject of study [16, 19, 20].
An important shortcoming in research focusing on depression among cancer patients is that the majority of studies are conducted in middle- to upper middle-class non-Latino White cancer patients [13, 21]. With this limited focus, it is unknown if these findings generalize to the large numbers of immigrant cancer patients. However, the few studies conducted with different racial and ethnic groups have found differences. Studies focusing on depression with noncancer community samples indicate that non-Latino Blacks have a lower prevalence of depressive disorders than non-Latino Whites [22]. Williams [9] found that although Black and Caribbean Blacks have a lower lifetime prevalence, they have a higher risk of the persistence of depression and their symptoms are more severe and disabling compared with non-Latino Whites. Studies with Latinos have shown that they experience high rates of depression [23, 24] and are at particular risk for depression due to immigration stressors, job disruptions, and financial hardships [7, 25–27]. Furthermore, research suggests that in the Latin culture, depression is often expressed in terms of somatic and physiological symptomatology [28].
Within the cancer literature, few studies have explored the rates and prevalence of depression among minority or immigrant cancer patients. Eversly et al. [10], using the Center for Epidemiologic Studies Depression Scale, found that Latina breast cancer patients report almost twice the rate of depressive symptoms as Black and Caucasians and that being Latina was a significant predictor of reporting more posttreatment symptoms (depression, fatigue, and pain). Ell [14] found, using the Patient Health Questionnaire-9 in a sample of predominantly Latino cancer patients, high rates of clinically significant depression (29 % moderate to severe depression) and significant rates of depression recurrence after 24 months. Bowen [29] found that Black breast cancer survivors reported better mental health than non-Latino White women, whereas Latina women reported poorer mental health than non-Latino White and Black women. However, Christie [13] found similar depression levels among Latinas and non-Latino White breast cancer patients.
Although there are a substantial number of studies exploring the incidence, prevalence, and manifestation of depression in cancer patients [4], these studies have rarely been ethnicity specific, with the focus of this literature almost entirely on non-Latino Whites. As a result, there is a lack of understanding of how ethnicity plays a role in the prevalence and symptomatology of depression in cancer patients across ethnicities. It is vital to address the information gap on depression in minority cancer patients. On the other hand, most of the previous research regarding racial/ethnic minority patients’ depressive symptomatology has focused on comparing different groups without controlling for migration status. This study includes a sample of immigrant Latino, predominantly from the Caribbean, and immigrant Afro-Caribbean patients.
Objectives
This study explores the prevalence and symptomatology of depression using the Patient Health Questionnaire-9 (PHQ-9) in a sample of Afro-Caribbean and Latino cancer patients. Also, because cancer patients frequently report physical symptoms such as fatigue, sleep disturbance, poor appetite, and pain, we expect a higher endorsement of these symptoms than the emotional symptoms. This study will contribute to identifying specific symptoms that are most salient for each ethnic group. The aims of this study were to determine the rate of a positive screen of depression on both samples and to compare the overall somatic and nonsomatic depression symptoms and specific depressive symptoms between the two groups.
Methods
Design and participants
The current study uses data from the Cancer Portal Project, which provides services to immigrant and ethnic minority cancer patients to improve their quality of life and cancer treatment adherence. The Cancer Portal Project enrolls patients with cancer at hospital-based cancer clinics in New York City with large numbers of low-income patients. Eligible patients included all adults with a cancer diagnosis undergoing treatment at the hospitals. Portal Service Access Facilitators approached all patients in the waiting room before provider visits and administered an intake needs assessment survey in the patient’s preferred language (Spanish or English). The study was approved by the Institutional Review Board of Memorial Sloan-Kettering Cancer Center. A detailed description of the study methodology and recruitment procedures has been published previously [30].
This is a nested cohort study of immigrant Latino and Afro-Caribbean Portal patients. The sample included a total of 189 Afro-Caribbean (n = 44) and Latino (n = 145) cancer patients recruited from five safety net hospitals in New York City over the time period of March 2011 to December 2011. All the Latino patients reported being Latino or Hispanic and being born in a Latin American country, most predominantly in the Caribbean. All the Afro-Caribbean patients reported being Black, African-American, or Afro-Caribbean and were born in a non-Hispanic country in the Caribbean. Only patients born in Latin America or the Caribbean were included because immigrants have a different incidence of major depression than those born in the USA [31], and there is a dearth of research focusing on the impact of cancer on immigrant populations.
Measures
The survey, which was available in English and in Spanish, included sociodemographic data, health-related questions, quality of life and depression scales, and a socioeconomic needs assessment questionnaire. Depressive symptoms were measured through the PHQ-9, a clinical scale comprised of nine items to screen for depression and one item from the European Quality of Life 5-D (EQ-5D) measuring the severity of the patient’s anxiety and/or depression. The EQ-5D has demonstrated good construct validity and responsiveness for depression in several studies [32]. Patients also reported their current known comorbidities, including depression.
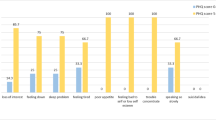
The PHQ-9 is based directly on the diagnostic criteria for major depressive disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. The PHQ-9 has been translated into Spanish and validated with English- and Spanish-speaking Latinos [33]. It assesses symptoms and functional impairment to screen for depression and derives a severity score. The PHQ-9 score can range from 0 to 27, since each of the nine items can be scored from 0 (not at all) to 3 (nearly every day). For major depressive disorder (MDD), the threshold score for PHQ-9 is 10 or greater. However, Thekkumpurath [34], measuring the diagnostic accuracy of the PHQ-9 as a screening tool for MDD in a cancer population, observed that a cutoff score of 8 offered a high sensitivity of 93 % while maintaining an adequate specificity of 81 %, for identifying clinically significant symptoms of depression among cancer patients when compared to the Structured Clinical Interview conducted by mental health professionals. In this study, we were interested in examining the somatic and cognitive/emotional dimensions of depression. In prior work by De Jonge and colleagues with chronically ill patients [35], four PHQ-9 items, problems with sleep, fatigability, appetite, and psychomotor agitation/retardation, were classified as somatic depressive symptoms, whereas five items, lack of interest, depressed mood, negative feelings about self, concentration problems, and suicidal ideation, were classified as nonsomatic depressive symptoms. Figure 2 presents the frequency of participants who endorse the symptoms by reporting they have experience the symptoms several days or more. The alpha coefficient for the PHQ-9 was .81, .68 for the somatic symptoms, and .67 for the nonsomatic symptoms.
Analysis
Statistical analyses were executed using the SPSS 19 software package. Less than 3 % of patients skipped a single PHQ item; the omitted value was imputed using mean substitution [36]. The final sample available for analysis was 189 cancer patients. Descriptive analyses were performed on the Latino and Afro-Caribbean cohort to examine sociodemographic characteristics. To test for potential sociodemographic differences, we compared gender, age, marital status, educational level, and income level. They were also compared on four health-related variables: cancer type (two most prevalent diagnoses: breast and gastrointestinal), type of treatment currently receiving, and stage at diagnosis. To explore for differences in depression scores related to immigration-related variables, we compared the groups on preferred language and length of time in the USA. Differences between groups were analyzed using t tests, and chi squares were used for comparisons of categorical data. All tests were two-sided, and a p value less than .05 was considered statistically significant.
To explore the prevalence of the depressive symptoms, we examined the frequency, percentage, and confidence interval for each symptom. Multiple chi squares were conducted to compare both groups on the depressive symptoms. Due to the pattern of response and the skewness of the distributions for each symptom, we report only the endorsement of the symptom. A probability value of less than 0.05 was considered to indicate statistical significance.
Results
Table 1 summarizes the demographic characteristics of the patient samples divided by ethnic group and the total sample, illustrating some significant group differences. The sample was evenly distributed across the five cancer clinics (30.3, 8.5, 21.8, 20.7, and 18.7 %). However, in one clinic, there were more Afro-Caribbean than Latino patients (54.5 % Afro-Caribbean vs. 11.8 % of Latinos, χ2 = 36.44, df = 1, p < .001). Latino patients were younger (Latinos: M = 54.19, SD = 13.19; Afro-Caribbean: M = 59.15, SD = 13.50; t = −2.15, df = 183, p = .03) as well as less educated (31 % of Latinos have graduated from high school or have higher education vs. 61.4 % of Afro-Caribbeans, χ2 = 10.77, df = 1, p < .001). In terms of country of origin, 56.6 % of the Latinos were born in the Caribbean, 22 % in Central America, and 21.4 % in South America. Most of the Afro-Caribbean sample was born in countries of the Lesser Antilles, and 22.7 % of the Afro-Caribbean patients were born in Jamaica, followed by 17.8 % in Trinidad-Tobago. In the Latino group, 77.2 % were monolingual Spanish speaking. No statistically significant differences were found among the most prevalent cancers (breast: 38.6 % of Latinas vs. 38.6 % of Afro-Caribbeans, χ2 = .0, df = 1, p = .99; GI: 18.6 % of Latinas vs. 11.4 % of Afro-Caribbeans, χ2 = 1.26, df = 1, p = .26), stage (40.8 % of Latinos with stage III or IV vs. 58.8 % of Afro-Caribbeans with stage III or IV, χ2 = 1.65, df = 1, p = .19), and the treatment they ever received (IV chemotherapy: 84 % of Latinos vs. 91.4 % of Afro-Caribbeans, χ2 = 2.81, df = 1, p = .25; radiation: 82.9 % of Latinos vs. 80 % of Afro-Caribbeans, χ2 = 2.34, df = 1, p = .31) between both ethnic groups. However, more Afro-Caribbean patients reported “currently receiving radiation” (50 %) than Latino patients (31 %, χ2 = 5.31, df = 1, p = .02).
Positive screen for depression
Figure 1 shows the mean depression screening scores by group. The mean PHQ-9 score for the total sample was 3.4 (SD = 3.67). Just over 10 % scored 8 or more on the PHQ-9 (n = 189, 10.6 %), which is the cutoff recommended by Thekkumpurath and colleagues [34] for the possible identification of major depressive disorder among cancer patients. Slightly, more Latino patients (n = 145, 11.6 %) exceeded this threshold for depression than Afro-Caribbean patients (n = 44, 7.1 %), but this small difference was nonsignificant (χ 2 = .68, df = 1, p = .41). Likewise, both groups exhibited similar depression screening scores (t = 1.37, df = 187, p = .17), somatic depressive symptoms (t = 1.04, df = 187, p = .30), and nonsomatic symptoms (t = 1.54, df = 187, p = .13).
However, when the groups were compared on the EQ5-D assessing severity of depression and anxiety, Latinos reported higher moderate to severe depression/anxiety (50 %) than Afro-Caribbean patients (25.6 %, χ 2 = 8.07, df = 2, p = .02). Furthermore, more Latinos (24.5 %) reported ever having a depressive disorder than the Afro-Caribbean counterparts (4.8 %, χ 2 = 7.92, df = 1, p < .01).
Comparison of symptoms
Table 2 and Fig. 2 show the prevalence of specific symptoms and comparisons by groups. Latino cancer patients reported depressive symptoms more frequently than their Afro-Caribbean counterparts. Fatigue (68.3 %) was the most frequent symptom reported by Latinos, followed by depressed mood (52.4 %) and sleep disturbance (46.6 %). The most common symptom reported by Afro-Caribbean patients was fatigue (57.1 %) as well, followed by appetite changes (34.1 %) and sleep disturbances (33.3 %), all are somatic complaints. Patients from both ethnic groups were comparable in all symptoms except depressed mood, with more Latinos reporting that symptom (52.4 %) than Afro-Caribbeans (21.4 %).
Discussion
This study contributes to reducing the gap in the literature of the expression of depression symptoms among immigrant cancer patients; most of what was known about depression in Afro-Caribbeans and Latinos comes from studies examining mental health issues among community-dwelling populations and populations with other chronic illnesses.
The goal of this study was to explore the prevalence of a positive screen for depression among two large immigrant groups presenting for cancer treatment and to compare their symptoms. The prevalence of a positive screen for clinical depression among this immigrant minority sample is approximately 10 %, slightly higher for Latinos patients (11.6 %) than for Afro-Caribbean patients (7.1 %). This finding is consistent with previous studies which estimate a prevalence rate of major depressive disorder of 10.8 % in samples with mainly non-Latino White cancer patients [5].
Results of the comparison of mean scores and percentage of patients meeting the cutoff scores showed that Afro-Caribbean patients reported comparable depressive symptoms as the Latino patients. Although we found similar levels of symptoms, previous studies have reported that, in general, Latino cancer patients report higher symptoms of depression and poorer mental health than other groups (African-Americans and non-Latino Whites) [10, 29].
However, upon closer inspection of specific symptoms and other self-report variables, Latino patients more frequently reported depressed mood, having a history of a depressive disorder, and overall higher psychological distress than Afro-Caribbean patients. In other words, mean scores of depressive symptoms and self-report of psychological distress are not consistent in these ethnic groups. Immigrant Latino cancer patients reported more frequently having depressed mood and a history of depression, whereas immigrant Afro-Caribbean patients reported less frequently experiencing depression and/or anxiety (EQ5D scale). These findings are consistent with a recent meta-analysis that found that depression is significantly worse in patients from ethnic minority groups, and this disparity is driven by comparisons of Latinos with non-Latino White cancer patients [37].
As expected, somatic symptoms, specifically fatigue, appetite, and sleep changes, were more frequently reported than emotional/cognitive symptoms. In line with these findings, several studies have highlighted the challenge of distinguishing between cancer-related and depression-related somatic symptoms [16, 17, 19]. It still remains unclear if the somatic symptoms are truly related to depression or to the cancer itself. Earlier studies with nonmedical samples have found that African-Americans are more likely to exhibit somatic and neurovegetative symptoms of depression than mood or cognitive symptoms [38] and African-American women report more somatic complaints associated to psychological symptoms than Latina women [8]. However, we did not find differences in the prevalence of somatic symptoms across groups.
Recommendations
It is increasingly recognized that screening for depression in cancer is crucial. With the growing diversity in the US population, we need efficient depression screenings which are valid and reliable for cancer patients from different ethnic groups. Although the psychometric properties of the PHQ-9 have been tested for different ethnic groups [15] and for primary care patients [39], there is a lack of information of its psychometric properties with cancer patients from different ethnic backgrounds and immigrant populations.
Studies analyzing in detail the presentation of specific symptoms and psychological responses of different cultural groups presenting chronic medical conditions are greatly needed to avoid the over-pathologization or underdetection of possible psychiatric diagnoses. Studies focusing on the presentation, prevalence, and symptom clusters of minority cancer patients are necessary.
Finally, depression screening inventories include somatic symptoms that often overlap with cancer symptoms. With cancer populations with positive screens for depression, it is crucial to go beyond the initial screening and conduct more comprehensive evaluations using structured interviews for diagnosis. Practitioners should give special attention to the cognitive/emotional and the somatic dimension of depression and assess the onset, intensity, and persistence of such symptoms to clarify if symptoms are due to the medical condition, to the mental health condition, or a combination of both.
Limitations
This study has several limitations. First, this is cross-sectional study performed in a convenience sample which limits the generalizability of results observed in this study. Second, the cross-sectional design limits the analysis to only one measure of depression in time. Because depression is known to be variable over time, to assess the variations and changes associated with depression and different disease stages, longitudinal studies are greatly recommended.
Depression was measured by a self-report inventory and not by a structured clinical interview. Such a strategy only reveals probable cases of depression; thus, a structured interview is necessary to detect psychiatric diagnoses. However, due to the scarcity of research in this area, the inventory was the best option available to get a preliminary assessment of depressive symptoms in the sample.
The sample size of immigrant patients limited the comparability of patients across cancer stages. We would expect different levels of symptomatology across different stages. A broader limitation is the imbalance of cancer types. Breast cancer patients comprised a disproportionately percentage of the sample; consequently, cases were too few for focused analyses with different types of cancer, which is the reason why we include all self-reported cancer types.
Finally, this sample was collected in New York City, from patients who were enrolled in ongoing health care and may not be representative of a national sample of Latino or Afro-Caribbean cancer patients.
Conclusions
This study is the first to explore and compare the presentation of depression in an immigrant group of Afro-Caribbean and Latino cancer patients, hence contributing to the scarce body of knowledge of these understudied populations. There is a need for further research examining depression in Afro-Caribbean and Latino cancer patients. Contrary to what was expected, the current study shows a similar level of a positive screen of depression for Latino and Afro-Caribbean cancer patients. Upon closer inspection of the symptoms, more Latinos reported experiencing depressed mood, being diagnosed with depression, and experiencing more intense depression/anxiety. Close attention should be devoted when screening for and diagnosing depression in cancer patients from different ethnicities. More research is necessary to establish the validity and psychometric properties of this measure (PHQ-9) with various cultural groups with chronic illnesses. Routine screening of emotional distress with valid and reliable instruments, followed by a comprehensive assessment of onset and intensity of symptoms for minority cancer patients, is necessary because it will identify patients for whom pharmaceutical or psychological interventions may be most warranted.
References
Brown LF, Kroenke K, Theobald DE et al (2010) The association of depression and anxiety with health-related quality of life in cancer patients with depression and/or pain. Pscyho-Oncology 19:734–741
Somerset W, Stout SC, Miller AH et al (2004) Breast cancer and depression. Oncology 18:1021–1034
Manning M, Bettencourt BA (2011) Depression and medication adherence among breast cancer survivors: bridging the gap with the theory of planned behaviour. Psychol Health 26:1173–1187
Massie MJ (2004) Prevalence of depression in patients with cancer. J Natl Cancer Inst 57–71
Ng CG, Boks MPM, Zainal NZ et al (2011) The prevalence and pharmacotherapy of depression in cancer patients. J Affect Disord 131:1–7
Alegria M, Mcguire T (2003) Rethinking a universal framework in the psychiatric symptom-disorder relationship. J Health Soc Behav 44:257–274
Alegria M, Shrout PE, Woo M et al (2007) Understanding differences in past year psychiatric disorders for Latinos living in the US. Soc Sci Med 65:214–230
Myers HF, Lesser I, Rodriguez N et al (2002) Ethnic differences in clinical presentation of depression in adult women. Cultur Divers Ethnic Minor Psychol 8:138–156
Williams DR, Gonzalez HM, Neighbors H et al (2007) Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry 64:305–315
Eversley R, Estrin D, Dibble S et al (2005) Post-treatment symptoms among ethnic minority breast cancer survivors. Oncol Nurs Forum 32:250–256
Nelson CJ, Balk EM, Roth AJ (2010) Distress, anxiety, depression, and emotional well-being in African-American men with prostate cancer. Psycho-Oncology 19:1052–1060
Meyerowitz BE, Formenti SC, Ell KO et al (2000) Depression among Latina cervical cancer patients. J Soc Clin Psychol 19:352–371
Christie KM, Meyerowitz BE, Maly RC (2010) Depression and sexual adjustment following breast cancer in low-income Hispanic and non-Hispanic White women. Psychooncology 19:1069–1077
Ell K, Xie B, Kapetanovic S et al (2011) One-year follow-up of collaborative depression care for low-income, predominantly Hispanic patients with cancer. Psychiatr Serv 62:162–170
Huang FY, Chung H, Kroenke K et al (2006) Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med 21:547–552
Jacobsen PB, Donovan KA, Weitzner MA (2003) Distinguishing fatigue and depression in patients with cancer. Semin Clin Neuropsychiatry 8:229–240
Donovan KA, Jacobsen PB (2007) Fatigue, depression, and insomnia: evidence for a symptom cluster in cancer. Semin Oncol Nurs 23:127–135
Nguyen J, Cramarossa G, Bruner D et al (2011) A literature review of symptom clusters in patients with breast cancer. Expert Rev Pharmacoeconomics Outcomes Res 11:533–539
Reuter K, Harter M (2004) The concepts of fatigue and depression in cancer. Eur J Cancer Care 13:127–134
Akechi T, Nakano T, Akizuki N et al (2003) Somatic symptoms for diagnosing major depression in cancer patients. Psychosomatics 44:244–248
Meyerowitz BE, Richardson J, Hudson S et al (1998) Ethnicity and cancer outcomes: behavioral and psychosocial considerations. Psychol Bull 123:47–70
Kessler RC, Berglund P, Demler O et al (2003) The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication. JAMA 289:3095–3105
Menselson T, Rehkopf DH, Kubzansky LD (2008) Depression among Latinos in the United States: a meta-analytic review. J Consult Clin Psychol 76:355–366
Riolo SA, Nguyen TA, Greden JF et al (2005) Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. Am J Public Health 95:998–1000
Ashing-Giwa KT, Kagawa-Singer M, Padilla GV et al (2004) The impact of cervical cancer and dysplasia: a qualitative, multiethnic study. Psycho-Oncology 13:709–728
Sue S, Chu JY (2003) The mental health of ethnic minority groups: challenges posed by the Supplement to the Surgeon General’s Report on Mental Health. Cult Med Psychiatry 27:447–465
Torres L (2010) Predicting levels of Latino depression: acculturation, acculturative stress, and coping. Cultur Divers Ethnic Minor Psychol 16:256–263
Comer R (1995) Abnormal psychology. Freeman, New York
Bowen DJ, Alfano CM, Mcgregor BA et al (2007) Possible socioeconomic and ethnic disparities in quality of life in a cohort of breast cancer survivors. Breast Cancer Res Treat 106:85–95
Gany F, Ramirez J, Nierodzick ML et al (2011) Cancer portal project: a multidisciplinary approach to cancer care among Hispanic patients. J Oncol Pract 7:31–38
Alegria M, Canino G, Shrout PE et al (2008) Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry 165:359–369
Peasgood T, Brazier J, Papaioannou D. (2012). A systematic review of the validity and responsiveness of EQ-5D and SF-6D for depression and anxiety. Health Economics and Decision Science, School of Health and Related Research, University of Sheffield
Somoza E (2002) The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Primary Care Companion. J Clin Psychiatry 4:191–195
Thekkumpurath PMBBS, Walker JM, Butcher IP et al (2011) Screening for major depression in cancer outpatients: the diagnostic accuracy of the 9-item patient health questionnaire. Cancer 117:218–227
De Jonge PP, Mangano DPMD, MaMD W (2007) Differential association of cognitive and somatic depressive symptoms with heart rate variability in patients with stable coronary heart disease: findings from the heart and soul study. Psychosom Med 69:735–739
Roth PL (1994) Missing data: a conceptual review for applied psychologists. Pers Psychol 47:537–560
Luckett T, Goldstein D, Butow PN et al (2011) Psychological morbidity and quality of life of ethnic minority patients with cancer: a systematic review and meta-analysis. Lancet Oncol 12:1240–1248
Fabrega H Jr, Mezzich J, Ulrich RF (1988) Black-white differences in psychopathology in an urban psychiatric population. Compr Psychiatry 29:285–297
Cameron IM, Crawford JR, Lawton K et al (2008) Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br J Gen Pract 58:32–36
Acknowledgments
This study was supported by the New York Community Trust. The contents of this article are solely the responsibility of the authors and do not necessarily represent the views of the awarding agency.
Conflict of interest
The authors indicated no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costas, R., Gany, F. Depressive symptoms in a sample of Afro-Caribbean and Latino immigrant cancer patients: a comparative analysis. Support Care Cancer 21, 2461–2468 (2013). https://doi.org/10.1007/s00520-013-1813-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1813-8