Abstract
Purpose
Physical activity is associated with a reduced risk of breast cancer development and recurrence. There are several hypothesised mechanisms for this including positive effects on metabolic and inflammatory biomarkers and favourable changes in anthropometric variables. This pilot study examined the effect of an 8-week aerobic exercise intervention on several of these outcomes, including body composition, the metabolic syndrome, C-reactive protein (CRP) and physical activity, in breast cancer survivors 2–6 months post-chemotherapy.
Methods
Assessments were completed at baseline, at 8-weeks and 3-months post-intervention. Measures taken following a 12-h fast included body composition (bioimpedance analysis), metabolic syndrome (waist circumference, blood pressure, high-density lipoprotein cholesterol, triglycerides and fasting glucose), insulin resistance (homeostatic model assessment), CRP and physical activity (accelerometry and questionnaire). Participants were randomized to either an 8-week moderate-intensity aerobic exercise group or a usual-care control group. Analysis was completed using repeated-measures analysis of variance (ANOVA) (p = 0.05).
Results
Twenty-six breast cancer survivors participated (mean (standard deviation) age 48.1 (8.8) years, exercise group; n = 16, control group; n = 10). At baseline, 13 participants were overweight, 6 were obese and 19 centrally obese. Intention-to-treat analysis revealed no significant differences between the exercise and control groups in any of the outcomes measures; however, analysis of those who adhered to >90 % of the supervised exercise class showed a significant decrease in waist circumference (p = 0.05) and a significant increase in subjectively reported “total weekly” (p = 0.005) activity.
Conclusion
While this 8-week aerobic exercise pilot intervention did not elicit significant improvements in biomarkers of breast cancer risk, there was some suggestion of improvements in waist circumference and subjectively measured physical activity in participants with >90 % adherence to the programme. A trial of longer duration and greater subject numbers is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most commonly diagnosed female cancer worldwide and is the leading cause of female cancer-related death [1]. In recent years, the numbers of women surviving breast cancer has increased greatly, generating interest in the role of modifiable risk factors for breast cancer, such as obesity and physical activity, in improving breast cancer outcomes.
Physical activity can reduce breast cancer occurrence by up to 25 % in postmenopausal women engaging in the highest quartile of habitual exercise [2]. Breast cancer survivors who engage in aerobic exercise equivalent to 9 metabolic equivalent-hours (MET-h) for 2–3 h per week have a significantly lower risk of breast cancer recurrence and improved breast cancer and all-cause mortality when compared with less active women (<3 MET-h /week) [3–5]. Obesity is a well-established risk factor for postmenopausal breast cancer development [6] and recurrence [7]. Weight gain, a common side-effect of adjuvant chemotherapy and hormonal therapy [8], observed most commonly in premenopausal women [9], has also been associated with poorer breast cancer outcomes [10].
The mechanisms through which physical activity exerts its protective effect are hypothesised to be through alterations in a number of biomarkers of breast cancer risk including the insulin-glucose pathways and inflammatory markers and improvements in anthropometrics [11, 12]. The current study is the first to examine the effect of aerobic exercise on the clustering of these variables in breast cancer survivors. The metabolic syndrome [13] represents a pro-inflammatory state and encompasses many of the biomarkers associated with breast cancer risk including abdominal obesity and insulin resistance [14]. While individually, high insulin resistance and chronic low-grade inflammation characterised by high circulating C-reactive protein (CRP) are associated with poor breast cancer prognosis and increased mortality [15, 16], the co-existence of inflammatory and metabolic biomarkers may be a more crucial target for improving breast cancer outcomes.
The aim of the current study was to evaluate the effect of aerobic exercise on a clustering of anthropometric and blood biomarkers for breast cancer risk, including the metabolic syndrome and CRP in breast cancer survivors. A secondary aim was to investigate if such a programme resulted in improvements in physical activity levels as measured by accelerometry.
Materials and methods
Setting and participants
This study was designed as an ancillary study to a randomized controlled trial (RCT) (Prescribed Exercise after Chemotherapy (PEACH)) [17]. The PEACH examined the effect of an 8-week aerobic exercise intervention on physical activity, aerobic fitness and quality of life in a heterogeneous group of cancer survivors, 2–6 months post-chemotherapy. Breast cancer survivors who had consented to the PEACH trial were eligible to participate in the current study. All other inclusion and exclusion criteria were as per the PEACH trial [17]. Ethical approval was granted by the hospital Research Ethics Committee.
Protocol
Participants attended the laboratory for testing on three occasions; baseline (pre-randomisation), immediately post-intervention (8-week visit) and 3 months post-intervention (3-month visit). Participants were randomized to either an exercise group (EG) or control group (CG) following the baseline visit, as per the PEACH trial using a computer-generated random numbers list (GraphPad Software, San Diego, CA). Assessments were completed by the same researcher at every visit who was blinded to the participants’ group assignment. Demographic details, medical and cancer treatment history were obtained from medical charts and through participant interview.
Exercise intervention
The intervention has been described in full previously [17]. The EG completed an 8-week, twice weekly supervised aerobic intervention and a home-exercise programme. Fitness levels were classified as “Poor”, “Fair” or “Average” from pre-determined cut-off values, as per baseline fitness tests. Participants with “Poor” fitness started the intervention at an intensity range of 35–55 % heart rate reserve (HRR), participants with “Fair” fitness started at 40–60 % HRR, while those classified as “Average” commenced at 45–65 % HRR. Aerobic intensity zones were progressed by 5 % HRR every 2 weeks. Class duration increased by 3 min every 2 weeks, alternate to the increase in exercise intensity, from 21 min in week 1 to 42 min in week 8. Heart rate (HR) was monitored using polar HR monitors (Polar FT4F Heart Rate Monitor). Participants rotated between three aerobic exercise stations during the class (stationary bike, treadmill, rowing ergometer).
The intensity of the home-exercise programme progressed in the same manner as the supervised class. Participants wore HR monitors to monitor compliance. Initially, participants exercised at home on one day of the week, increasing to 5 days per week at study completion. The CG did not engage in a structured exercise programme but were offered an exercise advice session following the final assessment.
Assessments
Body composition analysis and blood pressure
Anthropometric data were collected following a 12-h fast. Standing height was measured, barefoot, to the nearest millimetre using a SECA stadiometer. Body composition, including body weight, was estimated using a bioimpedance analyser, the Tanita MC 180 MA Multi-Frequency Body Composition Analyzer (Tanita Corp, Tokyo, Japan). Waist circumference was measured using a flexible measuring tape, in duplicate, to the nearest millimetre, at the mid-point between the top of the iliac crest and the last rib. Resting blood pressure was measured using the auscultatory method following a 5-min rest period. Blood pressure measurements were taken on the non-surgical side, in duplicate and averaged for data entry.
Venous blood sampling
Venous blood samples were collected in the morning following a 12-h fast. Participants were asked to refrain from moderate-vigorous intensity exercise for 24-h prior to collection. Samples were taken to measure glucose, insulin, lipid profile (total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) and triglycerides), glycosylated haemoglobin levels (HBA1c) and CRP. Insulin resistance was calculated using the Homeostatic Model Assessment (HOMA): [(fasting glucose (mmol/ L) × fasting insulin (mU /L))/22.5] [18].
Metabolic syndrome classification
The metabolic syndrome was diagnosed in the presence of any three of the following: elevated waist circumference (≥80 cm); elevated triglycerides (≥1.7 mmol/ L) or drug therapy for lipid abnormalities; reduced HDL-C (<1.3 mmol /L) or drug therapy for lipid abnormalities; elevated blood pressure (systolic ≥130 mmHg and/or diastolic ≥85 mmHg) or antihypertensive medication; elevated fasting glucose (≥100 mg /dL) or glucose-lowering medication [13].
Physical activity
Physical activity was measured objectively using the triaxial RT3 activity monitor (Stayhealthy Inc. Montrovia, California, USA). Participants wore the monitor for 7 days, during waking hours, following each assessment. The validity [19] and reliability [20] of the accelerometer have been established. The RT3 is a reliable tool for assessing moderate-to-vigorous activity in overweight and obese adults [21] and has been used previously in our laboratory to monitor activity levels in cancer patients prior to surgery [22].
Physical activity was measured subjectively using the Godin Leisure Time Exercise Questionnaire, which records the frequency of strenuous, moderate and mild exercise bouts of at least 15 min duration. The validity and reliability of the questionnaire has been established [23] and it has been used in cancer survivors [24].
Dietary intake
Participants were asked to complete an estimated dietary record (Medical Research Council, UK) on three consecutive days comprising of 2 weekdays and 1 weekend day, within 1 week of providing the blood samples at each assessment. No specific diet was prescribed. Diaries were analysed using WISP (Tinuveil Software, Llanfechell, Anglesey, UK) nutrition analysis programme.
Statistical analysis
Data was analysed using an intention-to-treat analysis with SPSS version 18.0 software (SPSS, Inc., Evanston, IL). The last-observation-carried forward procedure was used for missing variables. Secondary analysis examined if outcomes were influenced by adherence to the programme. Participants were grouped into two categories; adherence to >90 % of the exercise class or attended all three CG assessments (per-protocol analysis) or those who either dropped out or adhered to <90 % of the exercise class. Distributions were checked for normality using the K-S normality test.
Baseline characteristics were compared using independent sample t tests for continuous variables and Pearson chi-squared and Fisher’s exact tests for categorical variables. Log transformations were applied to non-parametric variables. Changes in endpoints were examined using general linear model repeated-measures ANOVA. Mean changes in variables from baseline to 8 weeks and from baseline to 3 months are described with 95 % confidence intervals (95 % CI). The lowest detectable value for CRP was 1 mg/L and therefore results <1 mg/L were assigned a value of 1 mg/L.
One participant was prescribed Metformin following baseline assessment and was excluded from analysis of metabolic variables. Another participant with a baseline CRP value over tenfold higher than subsequent results was excluded from CRP analysis as this result most likely represented an acute inflammatory event. Non-normally distributed data was examined using the Wilcoxon test. Statistical significance was set at p < 0.05.
Results
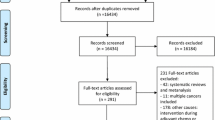
Participants were recruited from St. James’s Hospital, Dublin, between March 2010 and January 2011. Forty-three participants were enrolled onto the PEACH trial, 32 of whom with breast cancer and 26 consented to the current study. Baseline characteristics are described in Table 1. The two groups were similar for all demographics (p < 0.05). All participants received anthracycline and/or taxane containing adjuvant chemotherapy. Six participants, three per group, continued to receive anti-HER2 directed therapy during the intervention period.
Two participants dropped out of the EG due to time constraints. A further six adhered to <90 % of the exercise class but completed follow-up assessments. There were no differences between those who adhered to the exercise class and those who didn’t in terms of cancer stage (p = 0.74), time since completion of chemotherapy (p = 0.69), baseline body mass index (BMI) (p = 0.98) or baseline physical activity (p > 0.05 for all activity domains). Two members of the CG didn’t complete the final assessment due to illness unrelated to their breast cancer.
Metabolic and inflammatory biomarkers
At baseline, the metabolic syndrome was present in nine participants (EG: n = 6, CG: n = 3). Nineteen participants were centrally obese (waist circumference >80 cm), and there was no difference between the two groups (p = 0.60). Groups were similar for systolic and diastolic blood pressure (p = 0.96 and p = 0.38 respectively), with three members of each group taking antihypertensive medications. Lipid profiles were significantly worse in the exercise group for both TC (p = 0.002) and LDL-C (p = 0.001). Dyslipidaemia (TC >5.2 mmol/ L) was present in half the overall group (EG; n = 11, CG; n = 2) and two participants in the EG took lipid-lowering medication. Baseline glucose levels were <100 mg/dL (88.6 (7.6) mg/dL). Five participants in the EG were hyperinsulinemic (insulin >12 mU/ L) versus one in the CG (p = 0.06). Consequently, insulin resistance was significantly higher among exercisers (p = 0.05). There were no baseline differences in CRP (p > 0.05).
Results of the intention-to-treat analysis for metabolic parameters are presented in Table 2. Examination of the accompanying confidence intervals suggest significant within-group changes in a number of parameters; however, changes were not significant when groups were compared. Per-protocol analysis showed a significant (p = 0.05) decrease in waist circumference in the EG versus control subjects (EG; mean change baseline to 3 months −4.63 cm (95 % CI, −5.7 to −3.6), CG; mean change baseline to 3 months −0.30 (95 % CI, −2.3 to 1.7)).
CRP decreased by 1.53 mg/ L (95 % CI, −2.39 to −0.66 ) at 8 weeks and by 0.65 mg/L (95 % CI, −1.66 to 0.35) ) at 3 months post-intervention in the EG, while it increased by 0.38 mg/L (95 % CI, 0.03 to 0.74) at 8 weeks and decreased by 0.01 mg/L (95 % CI, −0.41 to 0.39) at 3 months in the CG; however, changes were not different between groups (p = 0.07 and p = 0.69, respectively).
Body composition and dietary intake
Groups were similar at baseline for all body composition measures (p > 0.05). The majority of participants were overweight (n = 13) or obese (n = 6). No changes occurred in body weight (p = 0.53), BMI (p = 0.43), percentage body fat (p = 0.25) or muscle mass (p = 0.46). There were no further changes with per-protocol analysis. Similarly, energy intake at baseline was 7.62 (1.69) MJ and did not change during the study (p = 0.37).
Physical activity
Groups were similar at baseline for subjectively and objectively measured physical activity. Neither the Godin questionnaire nor the RT3 accelerometer showed changes across any activity domain (Table 3). Per-protocol analysis showed significant improvements in subjectively reported “total weekly” (p = 0.005) activity but not in objectively measured data.
Analysis of objectively measured activity indicated that throughout the study, over 50 % of time was spent sedentary (baseline 52 %, 8 weeks 51 % and 3 months 50 %). Light intensity activity was high (baseline 42 %, 8 weeks 43 % and 3 months 42 %), while moderate-vigorous intensity time remained low (baseline 6 %, 8 weeks 6 % and 3 months 8 %) (Figs. 1 and 2). Data were further examined for adherence to physical activity guidelines (30 min moderate intensity activity (accumulated in ≥10 min bouts), 5 days per week [25]). At baseline, five participants were exercising to recommended activity guidelines (EG: n = 3, CG: n = 2), with no change post-intervention.
Discussion
This pilot study demonstrated that an 8-week aerobic exercise intervention did not improve features of the metabolic syndrome, CRP or anthropometric variables in breast cancer survivors. Sub-analysis of those with >90 % adherence to the exercise class demonstrated significant improvements in waist circumference and subjectively measured “total weekly” physical activity.
This is the first study to measure metabolic syndrome in breast cancer survivors in the acute stage post adjuvant chemotherapy. The majority of participants were overweight or obese (n = 19) and/or centrally obese (n = 19) at baseline and nine presented with the metabolic syndrome. The metabolic syndrome, characterised by abdominal obesity and insulin resistance [13], is identified as one of the potential links between obesity and cancer [26]. The metabolic syndrome as a collective unit and its individual components have been associated with increased breast cancer risk [6, 27, 28] as well as poorer breast cancer outcomes [15, 29].
In the current study, despite marked levels of central obesity, insulin resistance and CRP values were low, characterising an obese but metabolically healthy state [30]. Visceral adipose tissue is a multi-functional endocrine organ, secreting of a number of proteins including tumor necrosis factor-α, interleukin-6, leptin, insulin-like growth factor-I (IGF-I), resulting in a pro-inflammatory, insulin-resistant environment [14]. Prior to chemotherapy, the majority of participants in this trial were premenopausal, a group at high risk of chemotherapy-related weight gain [9]. The level of obesity observed may reflect recent weight gain among this group which has yet to have an adverse impact on metabolic and inflammatory pathways. In long-term breast cancer survivors, increasing concentrations of C-peptide, leptin, IGFs and CRP have been associated with increasing BMI (p < 0.05) [31, 32]. Thompson and colleagues [33] reported that the metabolic syndrome was present in 54.8 % of overweight/obese breast cancer survivors, 96 % of whom were centrally obese, with mean CRP levels of 5.1 mg/dL, suggestive of chronic low-grade inflammation.
Physical activity can improve breast cancer related outcomes [3–5], most likely through alterations in insulin and inflammatory pathways and improved anthropometrics [12]. While a number of interventions have examined the effect of exercise on individual components of the metabolic syndrome among breast cancer survivors [24, 34–37], this was the first study to consider the syndrome as a unit. While no changes in metabolic or inflammatory markers were observed, per-protocol analysis revealed a significant decrease in waist circumference. Previous studies have also reported reductions in waist circumference [38, 39]; however, unlike the current study, these have been limited due to non-randomized designs [38] and reporting of waist-to-hip ratio, not waist circumference [39]. Other studies in this population have reported decreases in triglycerides [24], systolic blood pressure [40, 41] and IGFs [34, 37, 42] with both aerobic and resistance training. Four RCTs have examined the effect of both aerobic and resistance exercise on markers of insulin resistance and have observed no changes in fasting glucose, fasting insulin or insulin resistance [34–37]. Only one other intervention measured CRP and reported no change [24]. In non-breast cancer populations, a number of RCTs have reported significant decreases in intra-abdominal and subcutaneous fat, insulin, insulin resistance and CRP [43–45], following year-long moderate-to-vigorous intensity aerobic interventions in overweight/obese postmenopausal women.
Whether improvements in metabolic parameters are stimulated by physical activity, without concurrent fat loss, is unclear. In the present study, no change in BMI or percentage body fat was observed. Generally, it appears that some fat loss is necessary for changes to occur; however, the extent to which visceral fat can be reduced is greatly influenced by incorporating high-intensity exercise into diet interventions [11]. Weight loss stimulated by diet alone reduces both fat-free mass and fat mass, having little effect on visceral fat [11]. Higher-intensity aerobic exercise specifically targets visceral fat deposits [11, 45]. The current study monitored dietary intake using food diaries and found no changes during the study period, suggesting that exercise stimulated the decrease in waist circumference observed in the per-protocol analysis.
A major strength of the current study is the use of accelerometry to objectively measure physical activity, allowing for accurate quantification of activity intensity and duration. A high percentage of objectively measured sedentary time was observed in both groups at all assessment stages (Figs. 1 and 2). This is consistent with other studies which show that breast cancer survivors spend the majority of time inactive [46]. Breast cancer patients significantly reduce activity levels upon diagnosis and rarely return to pre-morbid levels [47]. Objectively measured sedentary time is significantly associated with BMI, waist circumference, CRP, insulin and insulin resistance in postmenopausal women while moderate-to-vigorous intensity activity is inversely related to these variables [48]. These relationships were not observed in the current study. Subjectively, participants in the per-protocol analysis study reported significant increases in “total weekly” physical activity that was not reflected by increases in objectively measured physical activity. As the group remained predominantly sedentary throughout the study period, even light intensity activity may have been perceived at a higher intensity, leading to inaccurate and exaggerated reporting.
Reasons for the lack of change in the primary outcomes require consideration. The short duration of this intervention may have been insufficient to promote meaningful changes in lifestyle activity habits. The current study did not significantly reduce time spent sedentary nor did it improve adherence to physical activity guidelines, suggesting that participants compensated for exercise with prolonged rest periods. The high percentage of inactivity may reflect some side-effects of chemotherapy treatments such as cancer-related fatigue or reduced cardiorespiratory fitness, which may have a strong influence over a group in the acute stage post chemotherapy. However, all these subjects were able to participate in the exercise intervention, suggesting that they were not unduly fatigued.
The timing of the intervention may also have been unsuitable due to treatment related issues such as adjusting to hormonal therapy medication, anti-Her directed therapies during the intervention period and continuing medical appointments. Previous interventions have exercised participants during chemotherapy [41] to several years post-diagnosis [35, 38]. Courneya and Friedenreich [49] describe the 3–6-month period post-cessation of cancer treatment as the “rehabilitation period”. Although the current study included participants within this period, adherence to the protocol was poor (per-protocol analysis excluded 10/26 participants), suggesting that not all breast cancer survivors appear ready for such a demanding intervention so early in their recovery.
There are a number of limitations to this intervention that warrant discussion. Firstly, this study was designed as an exploratory pilot study. An inherent limitation of a pilot study is a small sample size, such as observed in the current study, which results in issues such as reduced statistical power to detect significant change. In addition, the study was set as an ancillary study to a larger RCT, resulting in uneven group assignments and statistically significant different between groups. Finally, the short duration of the intervention may have been insufficient to elicit change in the variables measured. While these issues limit the interpretation of results and the conclusions that are drawn, the study provides rationale for developing a larger RCT to explore the questions raised by this study.
Conclusions
The results from this eight-week aerobic exercise pilot intervention did not elicit significant improvements in metabolic or inflammatory biomarkers suggested to play a role in breast cancer risk, in breast cancer survivors, 2–6 months post-chemotherapy. While results may have been limited by the small sample size, higher adherence to the exercise class did stimulate significant decreases in waist circumference and increased subjectively measured “total weekly” activity. The lack of change may be due to the short duration of the intervention resulting in a failure to change in lifestyle activity habits. The results from this pilot study would suggest that future trials with breast cancer survivors in the early stages post-treatment should include a gradual build-up in aerobic intensity to accommodate on-going treatment related issues and be of longer duration to promote long-term changes in lifestyle activity habits. A larger RCT examining this issue is warranted.
References
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics 2002. CA Cancer J Clin 55(2):74–108
Lynch BM, Neilson HK, Friedenreich CM (2011) Physical activity and breast cancer prevention. Recent Results Cancer Res 186:13–42
Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA (2005) Physical activity and survival after breast cancer diagnosis. JAMA 293(20):2479–2486
Pierce JP, Stefanick ML, Flatt SW, Natarajan L, Sternfeld B, Madlensky L, Al-Delaimy WK, Thomson CA, Kealey S, Hajek R et al (2007) Greater survival after breast cancer in physically active women with high vegetable-fruit intake regardless of obesity. J Clin Oncol 25(17):2345–2351
Irwin ML, McTiernan A, Manson JE, Thomson CA, Sternfeld B, Stefanick ML, Wactawski-Wende J, Craft L, Lane D, Martin LW et al (2011) Physical activity and survival in postmenopausal women with breast cancer: results from the women’s health initiative. Cancer Prev Res (Phila) 4(4):522–529
World Cancer Research Fund / American Institute for Cancer Research (2007) Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. AICR, Washington, DC
Caan BJ, Kwan ML, Hartzell G, Castillo A, Slattery ML, Sternfeld B, Weltzien E (2008) Pre-diagnosis body mass index, post-diagnosis weight change, and prognosis among women with early stage breast cancer. Cancer Causes Control 19(10):1319–1328
Rock CL, Flatt SW, Newman V, Caan BJ, Haan MN, Stefanick ML, Faerber S, Pierce JP (1999) Factors associated with weight gain in women after diagnosis of breast cancer. J Am Diet Assoc 99(10):1212–1218
Goodwin PJ, Ennis M, Pritchard KI, McCready D, Koo J, Sidlofsky S, Trudeau M, Hood N, Redwood S (1999) Adjuvant treatment and onset of menopause predict weight gain after breast cancer diagnosis. J Clin Oncol 17(1):120–129
Thivat E, Therondel S, Lapirot O, Abrial C, Gimbergues P, Gadea E, Planchat E, Kwiatkowski F, Mouret-Reynier MA, Chollet P et al (2010) Weight change during chemotherapy changes the prognosis in non metastatic breast cancer for the worse. BMC Cancer 10:648
McTiernan A, Ulrich C, Slate S, Potter J (1998) Physical activity and cancer etiology: associations and mechanisms. Cancer Causes Control 9(5):487–509
Neilson HK, Friedenreich CM, Brockton NT, Millikan RC (2009) Physical activity and postmenopausal breast cancer: proposed biologic mechanisms and areas for future research. Cancer Epidemiol Biomarkers Prev 18(1):11–27
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645
Doyle SL, Donohoe CL, Lysaght J, Reynolds JV (2012) Visceral obesity, metabolic syndrome, insulin resistance and cancer. Proc Nutr Soc 71(1):181–189
Duggan C, Irwin ML, Xiao L, Henderson KD, Smith AW, Baumgartner RN, Baumgartner KB, Bernstein L, Ballard-Barbash R, McTiernan A (2011) Associations of insulin resistance and adiponectin with mortality in women with breast cancer. J Clin Oncol 29(1):32–39
Goodwin PJ, Ennis M, Pritchard KI, Trudeau ME, Koo J, Madarnas Y, Hartwick W, Hoffman B, Hood N (2002) Fasting insulin and outcome in early-stage breast cancer: results of a prospective cohort study. J Clin Oncol 20(1):42–51
Walsh JM, Hussey J, Guinan E, O’Donnell D (2010) Pragmatic randomized controlled trial of individually prescribed exercise versus usual care in a heterogeneous cancer survivor population’: a feasibility study PEACH trial: prescribed exercise after chemotherapy. BMC Cancer 10:42
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
Rowlands AV, Thomas PW, Eston RG, Topping R (2004) Validation of the RT3 triaxial accelerometer for the assessment of physical activity. Med Sci Sports Exerc 36(3):518–524
Powell SM, Jones DI, Rowlands AV (2003) Technical variability of the RT3 accelerometer. Med Sci Sports Exerc 35(10):1773–1778
Jerome GJ, Young DR, Laferriere D, Chen C, Vollmer WM (2009) Reliability of RT3 accelerometers among overweight and obese adults. Med Sci Sports Exerc 41(1):110–114
Feeney C, Reynolds JV, Hussey J (2011) Preoperative physical activity levels and postoperative pulmonary complications post-esophagectomy. Dis Esophagus 24(7):489–494
Godin G, Shephard RJ (1985) A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 10(3):141–146
Fairey AS, Courneya KS, Field CJ, Bell GJ, Jones LW, Martin BS, Mackey JR (2005) Effect of exercise training on C-reactive protein in postmenopausal breast cancer survivors: a randomized controlled trial. Brain Behav Immun 19(5):381–388
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP (2011) American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 43(7):1334–1359
Cowey S, Hardy RW (2006) The metabolic syndrome: a high-risk state for cancer? Am J Pathol 169(5):1505–1522
Del Giudice ME, Fantus IG, Ezzat S, McKeown-Eyssen G, Page D, Goodwin PJ (1998) Insulin and related factors in premenopausal breast cancer risk. Breast Cancer Res Treat 47(2):111–120
Bjorge T, Lukanova A, Jonsson H, Tretli S, Ulmer H, Manjer J, Stocks T, Selmer R, Nagel G, Almquist M et al (2010) Metabolic syndrome and breast cancer in the me-can (metabolic syndrome and cancer) project. Cancer Epidemiol Biomarkers Prev 19(7):1737–1745
Goodwin PJ, Ennis M, Pritchard KI, Trudeau ME, Koo J, Taylor SK, Hood N (2012) Insulin- and obesity-related variables in early-stage breast cancer: correlations and time course of prognostic associations. J Clin Oncol 30(2):164–171
Brochu M, Tchernof A, Dionne IJ, Sites CK, Eltabbakh GH, Sims EA, Poehlman ET (2001) What are the physical characteristics associated with a normal metabolic profile despite a high level of obesity in postmenopausal women? J Clin Endocrinol Metab 86(3):1020–1025
Irwin ML, McTiernan A, Bernstein L, Gilliland FD, Baumgartner R, Baumgartner K, Ballard-Barbash R (2005) Relationship of obesity and physical activity with C-peptide, leptin, and insulin-like growth factors in breast cancer survivors. Cancer Epidemiol Biomarkers Prev 14(12):2881–2888
Pierce BL, Neuhouser ML, Wener MH, Bernstein L, Baumgartner RN, Ballard-Barbash R, Gilliland FD, Baumgartner KB, Sorensen B, McTiernan A et al (2009) Correlates of circulating C-reactive protein and serum amyloid A concentrations in breast cancer survivors. Breast Cancer Res Treat 114(1):155–167
Thomson CA, Thompson PA, Wright-Bea J, Nardi E, Frey GR, Stopeck A (2009) Metabolic syndrome and elevated C-reactive protein in breast cancer survivors on adjuvant hormone therapy. J Womens Health (Larchmt) 18(12):2041–2047
Fairey AS, Courneya KS, Field CJ, Bell GJ, Jones LW, Mackey JR (2003) Effects of exercise training on fasting insulin, insulin resistance, insulin-like growth factors, and insulin-like growth factor binding proteins in postmenopausal breast cancer survivors: a randomized controlled trial. Cancer Epidemiol Biomarkers Prev 12(8):721–727
Ligibel JA, Campbell N, Partridge A, Chen WY, Salinardi T, Chen H, Adloff K, Keshaviah A, Winer EP (2008) Impact of a mixed strength and endurance exercise intervention on insulin levels in breast cancer survivors. J Clin Oncol 26(6):907–912
Irwin ML, Varma K, Alvarez-Reeves M, Cadmus L, Wiley A, Chung GG, Dipietro L, Mayne ST, Yu H (2009) Randomized controlled trial of aerobic exercise on insulin and insulin-like growth factors in breast cancer survivors: the Yale Exercise and Survivorship study. Cancer Epidemiol Biomarkers Prev 18(1):306–313
Schmitz KH, Ahmed RL, Hannan PJ, Yee D (2005) Safety and efficacy of weight training in recent breast cancer survivors to alter body composition, insulin, and insulin-like growth factor axis proteins. Cancer Epidemiol Biomarkers Prev 14(7):1672–1680
Cheema BS, Gaul CA (2006) Full-body exercise training improves fitness and quality of life in survivors of breast cancer. J Strength Cond Res 20(1):14–21
Rahnama N, Nouri R, Rahmaninia F, Damirchi A, Emami H (2010) The effects of exercise training on maximum aerobic capacity, resting heart rate, blood pressure and anthropometric variables of postmenopausal women with breast cancer. J Res Med Sci 15(2):78–83
Wilson DB, Porter JS, Parker G, Kilpatrick J (2005) Anthropometric changes using a walking intervention in African American breast cancer survivors: a pilot study. Prev Chronic Dis 2(2):A16
Schneider CM, Hsieh CC, Sprod LK, Carter SD, Hayward R (2007) Effects of supervised exercise training on cardiopulmonary function and fatigue in breast cancer survivors during and after treatment. Cancer 110(4):918–925
Irwin ML, Alvarez-Reeves M, Cadmus L, Mierzejewski E, Mayne ST, Yu H, Chung GG, Jones B, Knobf MT, DiPietro L (2009) Exercise improves body fat, lean mass, and bone mass in breast cancer survivors. Obesity (Silver Spring) 17(8):1534–1541
Frank LL, Sorensen BE, Yasui Y, Tworoger SS, Schwartz RS, Ulrich CM, Irwin ML, Rudolph RE, Rajan KB, Stanczyk F et al (2005) Effects of exercise on metabolic risk variables in overweight postmenopausal women: a randomized clinical trial. Obes Res 13(3):615–625
Friedenreich C, Neilson HK, Woolcott CG, Wang Q, Stanczyk FZ, McTiernan A, Jones CA, Irwin ML, Yasui Y, Courneya KS (2010) Alberta Physical Activity and Breast Cancer Prevention Trial: Inflammatory Marker Changes in a Year-long Exercise Intervention among Postmenopausal Women Cancer Prev Res (Phila).J. Clin Oncol 28(9):1458–1466
Irwin ML, Yasui Y, Ulrich CM, Bowen D, Rudolph RE, Schwartz RS, Yukawa M, Aiello E, Potter JD, McTiernan A (2003) Effect of exercise on total and intra-abdominal body fat in postmenopausal women: a randomized controlled trial. JAMA 289(3):323–330
Lynch BM, Dunstan DW, Healy GN, Winkler E, Eakin E, Owen N (2010) Objectively measured physical activity and sedentary time of breast cancer survivors, and associations with adiposity: findings from NHANES (2003–2006). Cancer Causes Control 21(2):283–288
Courneya KS, Katzmarzyk PT, Bacon E (2008) Physical activity and obesity in Canadian cancer survivors: population-based estimates from the 2005 Canadian Community Health Survey. Cancer 112(11):2475–2482
Lynch BM, Friedenreich CM, Winkler EA, Healy GN, Vallance JK, Eakin EG, Owen N (2011) Associations of objectively assessed physical activity and sedentary time with biomarkers of breast cancer risk in postmenopausal women: findings from NHANES (2003–2006). Breast Cancer Res Treat 131(1):183–194
Courneya KS, Friedenreich CM (2001) Framework PEACE: an organizational model for examining physical exercise across the cancer experience. Ann Behav Med 23(4):263–272
Conflict of interest
Disclosures: None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guinan, E., Hussey, J., Broderick, J.M. et al. The effect of aerobic exercise on metabolic and inflammatory markers in breast cancer survivors—a pilot study. Support Care Cancer 21, 1983–1992 (2013). https://doi.org/10.1007/s00520-013-1743-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1743-5