Abstract
Purpose
Only little research has been conducted on breast cancer survivors returning to work in Germany. This paper explores two questions: (1) Does breast cancer lead to an increased drop-out of paid work? (2) Do other factors, apart from their illness, help explain breast cancer survivors’ (temporary) retirement from work? To the best of our knowledge, this is the first comparative and prospective study on breast cancer survivors returning to work in Germany. We consider this work to be a relevant research for three reasons: (1) It exceeds the observation period of previous international studies by another 3 years. (2) By including the comparison with a population sample, it allows to take the specific situation of breast cancer patients into account. This refers to their illness as well as to the socio-economic context. (3) It combines qualitative and quantitative methods in order to receive patients’ individual interpretations.
Methods
The analysis is based on a sample of 227 breast cancer patients, participating in a prospective study on the role of psychosocial factors in the long-term course of breast cancer and a random sample of 647 age-matched women living in northern Germany. Employment and demographic data were observed directly before primary surgery (2002–2004), 1 year later (2003–2005) and again 5 years later (2008–2010). In addition, qualitative interviews at the three different observations served as a basis for quantitative data analyses, which were mainly performed by logistic regression models.
Results
One year after primary surgery, nearly three times as many cancer survivors had left their job as compared to the women in the reference group. For breast cancer survivors, a lower level of education, part-time employment, the severity of work-related difficulties and participation in inpatient rehabilitation correlated significantly with the failure to return to work. Six years after surgery, the probability of returning to work was still only half as high among breast cancer survivors than among controls. The main predictor for not returning to work was found to be age; tumour stage and the severity of side effects of treatment also seemed to have an impact.
Conclusions
Breast cancer survivorship in Germany increases the risk of dropping out of paid work. The influence of work- and illness-related factors varies considerably between the early and late phases of recovery after breast cancer treatment. The comparative analysis demonstrates the relevance of labour market and pension legislation in Germany.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Paid work, not only as a means of creating income but purpose in life, is seen as an important prerequisite for health and quality of life [1]. Taking this into account, it does not come as a surprise that various authors have examined the significance of return to work for cancer survivors. Breast cancer, in particular, has been given increasing attention as it constitutes the most frequent cancer type among women, and survival rates are continuing to improve [2, 3]. Re-entry to work is crucial for physical and mental health. Supposedly, it provides financial security, quality of life, a sense of normality as well as distraction, and it might offer the opportunity to return from a period of isolation during treatment [2–5]. Thus, it may contribute to recovery [4] and functions as a strong incentive for patients to return to work. At the same time, with advancing years and additional areas of responsibility—social care, domestic responsibilities and raising a family—conditions for women with breast cancer are becoming increasingly difficult.
As population-based comparative studies from the Netherlands, Finland and North America have shown, breast cancer presents an additional major challenge to working women, which may have a negative impact on employment [6–9]. Depending on the time interval after diagnosis, breast cancer survivors are less likely to work in relation to their respective reference group. According to research in the Netherlands and in France, those who return to work need an average of roughly 11-month absenteeism before going back [3, 10, 11].
Factors positively or negatively influencing the return of breast cancer survivors to work have been subject to many studies, predominantly in North America and Europe. The analysis of socio-demographic factors such as age and education has revealed inconsistent results [3, 12–14]. In contrast, the influence of medical factors such as health status [3, 15] and treatment [3, 11, 12, 16] has been proven to be pivotal, in which chemo, radiation and endocrine therapies as well as lymph oedema limit and delay a return to work. In addition, job requirements [1, 3, 15, 16], self-perceived work ability [9, 14, 17] and social support at work [1, 5, 18, 19] are also associated with resuming work.
In Germany, to our knowledge, there is little empirical evidence concerning the successful re-entry of breast cancer patients into work. In general, however, there are some studies examining the success of inpatient rehabilitation regarding the re-integration of breast cancer survivors into work [20, 21]. Mehnert and Koch [22] examined the tendency for retirement among 750 breast cancer patients participating in a rehabilitation programme; 69 % of whom had returned to work 1 year after rehabilitation. They found that physical- and illness-related factors as well as the job situation and psychosocial characteristics contributed to the desire to retire from work [22, 23]. However, no control group of non-participants or women without cancer diagnosis was included in their study.
This paper exceeds the observation period of previous studies on return to work, which so far has been 3 years [7] and explores two questions: (1) Does breast cancer lead to an increased drop-out of paid work in Germany within a period of 6 years after primary treatment? (2) What other factors, apart from illness, help explain breast cancer survivors’ (temporary) retirement from work?
Methods
Study design and subjects
The analysis is based on a sample of 227 breast cancer patients (Table 1) participating in a prospective study of the role of psychosocial factors in the long-term course of breast cancer and on a random sample of age-matched women living in northern Germany, who had never been diagnosed with cancer.
Inclusion criteria for participation in the initial longitudinal study were primary manifestation of breast cancer (stages T1–T3, N0–N2, no evidence of metastases). Women with multiple cancers, recurrences of breast cancer and psychiatric diagnoses were excluded as well as women older than 70. This age limit was introduced because the study was designed for a total term of 10 years. The inclusion of patients over 70 would have increased the likelihood of dementia and premature death due to a large variety of diseases, thus making follow-ups difficult. Three gynaecological clinics from the city of Hannover (Germany) were participating in the study. The initial response rate was 77 %. The study design was approved by the ethics committee of Hannover Medical School. Written informed consent was obtained from all patients. Patients were interviewed between 2002 and 2010, directly after primary surgery (T0), 1 year later (T1) and again 5 years later (T2). The data of 227 women, aged 25–64, were included, with 147 of them being in paid work during at least one of the three assessments. One year after surgery, 205 participants in the follow-up interview were at working age, 5 years later, 126 women were younger than 65 years and therefore eligible for data analysis (see Fig. 1).
To create a population-based comparison group, a random sample of controls nearly three times as large (n = 647, with 446 women working in 2003, 2004 or 2009) was drawn from the Socioeconomic Panel (SOEP). It is a nationwide longitudinal project designed to provide representative data for Germany in order to depict social change and stability in living conditions [24]. The reference group was made up of women who had never been diagnosed with cancer, who were living in one of the six northern federal states of Germany and who had participated in the SOEP in an analogous calendar period, i.e. in 2003, 2004 and 2009. These data were then matched for age, which led to an approximation of the educational background of SOEP respondents to study participants. Further matching for socio-economic indicators was not required because in Germany, no social inequalities in the incidence of breast cancer were reported [25].
Data collection and interpretation
The data of the longitudinal breast cancer study came from face-to-face interviews which were tape-recorded, transcribed and rated. The interview schedules and the rating system are based on the ‘Life Events and Difficulties Schedule’ (LEDS), as developed by Brown and Harris [26, 27] and Harris [28]. The LEDS contains a set of manuals with anchoring examples and interpretation rules which help to assess the severity of life events and difficulties in the individual context as reported by the respondent. Difficulties are defined as adverse situations that last a minimum of 4 weeks. Rating their severity involves evaluating the degree of unpleasantness, practical inconvenience and threat, and comparing the difficulties with the anchoring examples in the manual [30]. Considering the individual context means taking all concomitants into account that contribute to or alter the meaning of difficulties, e.g. immediate consequences, closeness of relationships, compensating factors, etc. [29–31]. Interviewing and rating were performed by specially trained investigators based on interviews with open-ended questions. At the end of the rating process, a value was assigned to each difficulty according to an ordinal scale ranging from ‘1’ (very mild) to ‘6’ (high marked), and for each patient, the researchers created a score based on the number and severity of difficulties.
Two kinds of difficulties were examined for the purpose of this study:
-
1.
Difficulties at work imply situations such as physical/mental overload, conflicts with superiors/colleagues, job insecurity or inadequate qualifications. Most women reported one (if any) difficult situation at the workplace (see Table 2); in some cases, more than one were reported, mostly occurring simultaneously with the first difficulty. Therefore, for each woman, a score was created, being composed of the highest severity rating combined with the number of additional difficulties. For example, a woman describes her work overload (‘2’ = mild) and conflicts with newly employed colleagues (‘1’ = very mild) which add on to the already existing adverse situation (score = ‘3’).
Table 2 Demographic characteristics of breast cancer patients (BCP) and their SOEP referents -
2.
Side effects of treatment include symptoms following chemotherapy, radiation therapy and endocrine therapy. Because the different treatments generally were administered in sequence, a score was created for each woman, which was identical with the mean value of severity ratings, to be considered over the whole treatment period. For example, a respondent received chemotherapy, accompanied by hair loss, nausea, arthralgia, inability to eat and to smell. This was rated as ‘6’ (high marked). The following radiotherapy caused minor skin reactions that were rated as ‘1’ (very mild). The endocrine therapy at the end led to back pain and menopausal hot flushes, and was rated as ‘2’ (mild). Taken together, this respondent scored ‘3’ on the dimension ‘side effects of treatment’.
Quantifying qualitative information was performed for two reasons: Firstly, it considers patients’ individual contexts and categorises their difficulties by means of a researcher-based rating system. Secondly, it contributes to a deeper understanding of the respondents’ experiences and motivations, which may explain their decisions beyond pre-supposed structural causes. Accordingly, brief summaries of patients’ reports are given in the ‘Results’ section in order to provide supplementary information.
In addition to the interviews, questionnaires were used for collecting treatment schemes and socio-demographic data. Analogous to the three assessments of the longitudinal study (i.e. up to 6 years after primary surgery), socio-demographic data referring to age, education, employment status, marital status and household size were drawn from the Socioeconomic Panel for 2003, 2004 and 2009. The employment status of women working less than 35 h/week was defined as part-time employment.
Statistical analysis
The comparative analysis for assessing the influence of breast cancer survivorship on return to work and possible confounders (question 1) was performed by means of a logistic regression analysis. Study participants and respondents of the Socioeconomic Panel were both considered in the regression models. These included return to work as dependent variable, while age, matrimonial status, education and fulltime/part time work as independent variables (see Table 3). Subsequently, the main reasons for retirement from work (question 2) were examined using exclusively the sample of breast cancer patients. Again, logistic regression analysis was performed. Models included socio-demographic and medical factors as well as difficulties at the work place as independent variables, and return to work as dependent variable (see Table 4). The effects are expressed as odds ratios. SPSS version 19.0 was used for all statistical analyses.
Results
A total of 874 respondents were considered for the comparative analysis over 6 years, with 227 of them being participants of a longitudinal breast cancer study and 647 women from northern Germany. Medical data of patients are presented in Table 1; socio-demographic data of patients and referents, in Table 2. The sample of breast cancer survivors differed only slightly from that of controls. Survivors were on average 4 months older (51.5 ± 8.9 years) than controls, and 75 % as opposed to 83 % were living with a partner. The relatively low average age of onset may be due to the age limit (below 65 years) and due to the fact that women in capital cities might have better access to early detection and screening programmes. Education and employment rates were nearly the same among patients and referents, with the exception that women with 10 years of schooling were under-represented among referents and women with ‘other’ education were over-represented. In the Socioeconomic Panel, women with an immigrant background were classified as ‘other’ even if they had completed 10 years of schooling. Additionally, at baseline, 61 % of women were employed in both samples, 31 % of patients worked fulltime as compared to 28 % of the control group.
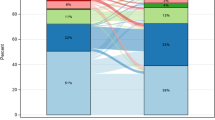
Comparing the employment changes of the two groups of respondents from 2003 to 2004 (period I), and from 2004 to 2009 (period II), major differences emerged (see Fig. 2). In period I, more than twice as many breast cancer patients left work (−23 %) as compared to their referents, and only half as many cancer survivors (5 %) (re-)entered the workforce. Breast cancer survivors in this period thus reached an exit/entry balance of −17.5 %, whereas the balance of their referents was nearly even (+0.6 %). The difference between the survivors and their referents leaving work in the first period is highly significant (Table 3). As logistic regression shows, the relative risk of not returning to work only slightly diminishes if adjusted for age, matrimonial status, education and fulltime or part time work (OR = 0.28; 95 % CI = 0.15–0.52; P = 0.000).
In period II, 6 years after primary surgery, the two groups still vary considerably in their balance of leaving and entering work, with survivors arriving at a balance of −1 % and the control group achieving +12.0 %. The probability of returning to work over a 6-year period is still only half as high among breast cancer survivors compared to their reference group (OR = 0.62; CI = 0.37–1.03; P = 0.062). The comparative analysis of the three different points in time shows that breast cancer clearly influences women’s decisions to leave or re-enter work over a 6-year period, especially in the first year.
Looking for factors inhibiting breast cancer patients’ return to work, differences become apparent between the two points in time. One year after surgery, the dominant factors were the status of previous employment (part-time vs. fulltime work; OR = 0.10; CI = 0.03–0.39; P = 0.001) and the severity of work-related difficulties (OR = 0.54; 95 % CI = 0.34–0.86; P = 0.009) which led to a higher risk of not returning. However, the exclusion of ‘employment status’ in the regression model modified the effect of ‘severity of work-related difficulties’ on the risk of not returning to work (OR = 0.72; 95 % CI = 0.50–1.03; P = 0.072). Part-time workers were not older than full-time workers, but they showed minor differences with respect to their work motivation, as the following summary of their reports displays: They returned to work for reasons of pleasure and distraction, and less for career reasons or due to financial pressures. Main sources of difficulties for part-time as well as fulltime workers were physical and mental overload (n = 19), conflicts with superiors and colleagues (n = 15), and occasionally job insecurity or inadequate qualifications. Resulting from this situation, some patients decided to stop working and set other priorities in life; others stopped working because they did not perceive sufficient support from their employer to make them stay in the company.
Surprisingly, another factor associated with the risk of not returning to work was participation in an inpatient rehabilitation (OR = 0.10; 95 % CI = 0.02–0.40; P = 0.001). Sixty-nine percent of rehabilitation participants returned to work, whereas among non-participants, the percentage of returners was 93 %. The tumour stage of patients showed no effect on their participation. The age of respondents only plays a minor role for re-entering the work place 1 year after surgery. A high school diploma as opposed to less than 10 years of schooling (P = 0.042) as well as cohabitation with a partner (P = 0.063) tends to support a return to work.
Six years after surgery, with the respondents being now on average 58 years old, age has the strongest effect on women’s return-to-work rate (OR = 0.85; 95 % CI = 0.77–0.93; P = 0.001), in the sense that with advancing years, women rather decide not to be in paid work anymore. Tumour stage (OR = 7.70; CI = 0.73–81.39; P = 0.090) and the severity of side effects of treatment (OR = 0.63; 95 % CI = 0.37–1.07; P = 0.092) fail to be statistically significant, but they show clear tendencies of influencing breast cancer survivors to retire from work. A summary of the patients’ answers shows that the side effects of treatment most often experienced were nausea (n = 59), loss of hair (n = 56) and pain (n = 26) after chemotherapy; various degrees of skin impairment after radiation therapy (n = 63); and menopausal symptoms (n = 28) and arthralgia (n = 13) after endocrine therapy. Furthermore, 15 out of 99 patients who returned to work during or after treatment reported that high workloads and lack of understanding from the part of colleagues made it quite difficult to cope with their disease.
Discussion
This paper explores the work status of breast cancer survivors at three different points in time and compares their employment history within the observation period to a control group drawn from a population panel. It thus provides validated information on the influence of breast cancer on women’s decisions to continue or stop working over a short- and medium-term period. As the information is not only based on standardised instruments but also on personal interviews, patients’ experiences and their interpretations could be considered in some more detail.
The comparative approach of the study permits us to reflect on women’s individual choices within a given socio-economic context, i.e. against the background of economic and labour market changes in Germany. These will be briefly discussed here. The proportion of working women in the population-based sample rose from 60.7 % in 2003 to 66.6 % in 2009 [32], in spite of the economic crisis in the years 2008 and 2009, and in spite of the fact that the examined group had a mean age of 57 years. Possibly, the amendments to labour market policy at the beginning of 2005 (Volume II of the German Social Insurance Code, SGB II, Sect. 65, Abs. 4) led to an intensified pressure on the elderly working population to continue or to resume working. One year later, the duration of unemployment benefits for people older than 57 years was cut down substantially (reduction from 36 to 18 months). Against this background, it does not seem surprising that between 2004 and 2009, significantly more women entered employment than left. Women with a breast cancer diagnosis, however, did not ‘benefit’ from this kind of policy. On the contrary, they not only left their jobs in significantly higher numbers, but they also refrained from taking up (new) work as compared to controls without breast cancer (as shown in Fig. 2).
The analysis of the breast cancer sample demonstrates that women in full-time employment had a significantly higher probability of returning to work as compared to part-time employees. The reports of the respondents showed a slightly different commitment to work and a different degree of financial pressure between full-time and part-time workers. Regression analyses also demonstrated that working conditions principally influence women’s choices regarding their continuation of work, even if less pronounced among full-time working survivors. This result is consistent with other studies [1, 3, 15, 16]. Women who reported distress, changes in labour requirements and bullying at work were more likely to leave their job than women who had no such difficulties. For them, the incidence of illness might have led to a secondary gain, as it allowed them to stop working.
Equally interesting, but in contrast to the results of other European studies [2, 4], is the finding that participation in inpatient rehabilitation does not increase the likelihood of returning to work after breast cancer surgery. Sixty-nine percent of rehabilitation participants - as opposed to 93 % of non-participants - returned to work, and this proportion coincides with the previous findings of Koch and Mehnert [23], based on a study with 750 breast cancer patients participating in inpatient rehabilitation. This relatively low proportion of returners among inpatient rehabilitation participants might partly be seen as a consequence of the German pension legislation. Volume VI of the German Social Insurance Code (SGB VI, Sect. 65, Abs. 4) imposes participation in a rehabilitation measure before medical experts can decide over the right to an early retirement and pension. It has to be conceded that those not returning to work tend to have higher levels of pain, depression and anxiety as well as reduced subjective work ability, as compared to returners [23]. Moreover, as research on inpatient rehabilitation in Germany has shown, rehabilitation measures may help to re-integrate people into work after a period of sickness [21]. This kind of research however should be expanded to breast cancer patients as the target group, with a specific focus on the connection between work-related difficulties and rising incidences of depression and anxiety.
Six years after primary surgery, the employment status before surgery and participation in rehabilitation no longer had any effect on survivors’ return to work. Medical factors such as an advanced tumour stage or the more severe side effects of treatment, in contrast, seem to influence women’s decision to retire at this later stage of recovery. It may be concluded that with advancing years, it might be more difficult for breast cancer survivors to cope with adverse effects of therapy.
Some limitations of this study need to be mentioned. Women who had reached the retirement age of 65 years in the course of the study were not eligible for the analysis of return to work anymore. As a consequence, the sample of breast cancer survivors was substantially reduced (see Fig. 1) which made it difficult to obtain consistent results over time. A quantitative study based on more cases might lead to robust statistical correlations between the course of illness and return to work. Moreover, one has to recognise that economic and legal conditions are changing constantly and may thus have altering influences on breast cancer patients return to work. Therefore, at another point in time, the same study might lead to different results. At the same time, this study shows that qualitative data help to consider the individual contexts of respondents and thus to understand the effect of the job situation as well as the side effects of treatment on return to work. A qualitative data analysis would give more insights into breast cancer survivors’ interpretations, which go beyond pre-conceived hypotheses.
References
Bouknight RR, Bradley CJ, Luo Z (2006) Correlates of return to work for breast cancer survivors. J Clin Oncol 24(3):345–353
Hoving JL, Broekhuizen MLA, Frings-Dresen MHW (2009) Return to work of breast cancer survivors: a systematic review of intervention studies. BMC Cancer 9:117. doi:10.1186/1471-2407-9-117
Fantoni SQ, Peugniez C, Duhamel A, Skrzypczak J, Frimat P, Leroyer A (2010) Factors related to return to work by women with breast cancer in northern France. J Occup Rehabil 20(1):49–58. doi:10.1007/s10926-009-9215-y
Tamminga SJ, De Boer AGEM, Verbeek JHAM, Frings-Dresen MHW (2010) Return-to-work interventions integrated into cancer care: a systematic review. Occup Environ Med 67(9):639–648. doi:10.1136/oem.2009.050070
Johnsson A, Fornander T, Rutqvist LE, Olsson M (2010) Factors influencing return to work: a narrative study of women treated for breast cancer. Eur J Cancer Care 19(3):317–323. doi:10.1111/j.1365-2354.2008.01043.x
Roelen CAM, Koopmans PC, van Rhenen W, Groothoff JW, van der Klink JJL, Bültmann U (2011) Trends in return to work of breast cancer survivors. Breast Cancer Res Treat 128(1):237–242. doi:10.1007/s10549-010-1330-0
Drolet M, Maunsell E, Brisson J, Brisson C, Mâsse B, Deschênnes L (2008) Not working 3 years after breast cancer: predictors in a population-based study. J Clin Oncol 23(33):8305–8312
Taskila-Abrandt TT, Martikainen R, Virtanen SV, Pukkala E, Hietanen P, Lindbohm ML (2004) The impact of education and occupation on the employment status of cancer survivors. Eur J Cancer 40(16):2488–2493
Bradley CJ, Neumark D, Bednarek HL, Schenk MJ (2005) Short-term effects of breast cancer on labor market attachment: results from a longitudinal study. J Health Econ 24(1):137–160
Roelen CAM, Koopmans PC, De Graaf JH, Balak F, Groothoff JW (2009) Sickness absence and return to work rates in women with breast cancer. Int Arch Occup Environ Health 82(4):543–546
Balak F, Roelen CAM, Koopmans PC, Ten Berge EE, Groothoff JW (2008) Return to work after early-stage breast cancer: a cohort study into the effects of treatment and cancer-related symptoms. J Occup Rehabil 18(3):267–272. doi:10.1007/s10926-008-9146-z
Johnsson A, Fornander T, Olsson M, Nystedt M, Johansson H, Rutqvist LE (2007) Factors associated with return to work after breast cancer treatment. Acta Oncol 46(1):90–96
Stewart DE, Cheung AM, Duff SF, Wong F, McQuestion M, Cheng T, Purdy L, Bunston T (2001) Long-term breast cancer survivors: confidentiality, disclosure, effects on work and insurance. Psychooncology 10(3):259–263
Bradley CJ, Bednarek HL, Neumark D (2002) Breast cancer survival, work, and earnings. J Health Econ 21(5):757–779
Johnsson A, Fornander T, Rutqvist LE, Vaez M, Alexanderson K, Olsson M (2009) Predictors of return to work ten months after primary breast cancer surgery. Acta Oncol 48(1):93–98. doi:10.1080/02841860802477899
Cavanna L, Ambroggi M, Stroppa E, Di Nunzio C, Dallanegra L, Monfredo M (2011) Return to work after treatment for breast cancer. Breast Cancer Res Treat 128(1):287–288. doi:10.1007/s10549-011-1388-3
Taskila TT, Martikainen R, Hietanen P, Lindbohm ML (2007) Comparative study of work ability between cancer survivors and their referents. Eur J Cancer 4(3):914–920
Hakanen P, Lindbohm ML (2008) Work engagement among breast cancer survivors and the referents: the importance of optimism and social resources at work. J Cancer Surviv 2(4):283–295
Taskila T, Lindbohm ML, Martikainen R, Lehto US, Hakanen J, Hietanen P (2006) Cancer survivors received and needed social support from their work place and the occupational health services. Support Care Cancer 14(5):427–435
Böttcher HM, Steimann M, Koch U, Bergelt C (2012) Rückkehr zur Arbeit—Erfahrungen und Erwartungen von Patientinnen und Patienten in der stationären onkologischen Rehabilitation. Rehabil 51(1):31–38
Mehnert A, Koch U (2007) Zur Wirksamkeit der stationären onkologischen Rehabilitation unter besonderer Berücksichtigung spezifischer psychoonkologischer Interventionen. Projektabschlussbericht. Gefördert durch die Arbeitsgemeinschaft für Krebsbekämpfung Nordrhein-Westfalen (ARGE) und die Paracelsus-Kliniken Deutschland GmbH
Mehnert A, Koch U (2012) Soziodemografische, medizinisch-funktionelle, psychosoziale, rehabilitations- und arbeitsbezogene Merkmale von Krebspatienten mit und ohne Antrag auf Berentung im Verlauf der onkologischen Rehabilitation. Deutsche Rentenversicherung Bund: 21. Rehabilitationswissenschaftliches Kolloqium. DRV-Schriften, band 98
Koch U, Mehnert A (2006) Medical rehabilitation of breast cancer patients in Germany: conditions and predictors of return to work. Psychooncology 15:S72–S73. doi:10.1002/pon.1092
Haisken-DeNew JP, Frick R (2003) DTC – Desktop companion to the German Socio-Economic Panel Study (SOEP), version 8.0. Dec 2005. http://www.diw.de/documents/dokumentenarchiv/17/diw_01.c.38951.de/dtc.409713.pdf. Accessed 29 June 2012
Geyer S (2008) Social inequalities in the incidence and case fatality of cancers of the lung, the stomach, the bowels, and the breast. Cancer Causes Control 19(9):965–974
Brown GW, Harris T (1978) Social origins of depression. Tavistock, London
Brown GW, Harris T (1989) Life events and measurement. In: Brown GW, Harris T (eds) Life events and illness. Unwin Hyman, London, pp 3–45
Harris T (ed) (2001) Where inner and outer worlds meet: psychosocial research in the tradition of George Brown. Routledge, London
Geyer S (1993) Life events, chronic difficulties and vulnerability factors preceding breast cancer. Soc Sci Med 37:1545–1555
Brown GW, Harris T (1978) The Bedford College life-events and difficulty schedule: directory of contextual threat ratings of events. Bedford College, University of London, London
Geyer S (1991) Life events prior to manifestation of breast cancer: a limited prospective study covering eight years before diagnosis. J Psychosom Res 35:355–364
Bundesagentur für Arbeit (2010) Arbeitsmarkt 2009. Amtliche Nachrichten der Bundesagentur für Arbeit. 58. Jahrgang, Sondernummer 2
Acknowledgment
This paper is supported by the German Research Association (Deutsche Forschungsgemeinschaft) under grant numbers GE1167/1-1 and GE1167/1-2.
Conflict of interest
No conflict of interest was involved in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noeres, D., Park-Simon, TW., Grabow, J. et al. Return to work after treatment for primary breast cancer over a 6-year period: results from a prospective study comparing patients with the general population. Support Care Cancer 21, 1901–1909 (2013). https://doi.org/10.1007/s00520-013-1739-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1739-1