Abstract
Purpose
This study presents data on the feasibility and possible benefits of a psychological intervention that uses virtual reality to induce positive emotions on adult hospitalized patients with metastatic cancer. The patient’s satisfaction and perceived utility was also examined.
Method
The sample was composed of 19 patients (53 % men, aged from 29 to 85 years old; x = 60.9; standard deviation = 14.54). The intervention consisted of four 30-min sessions during 1 week in which patients navigated through virtual environments designed to induce joy or relaxation. Mood was assessed before and after each session using the Visual Analog Scale. Patient satisfaction was assessed after each session and at the end of the intervention. Qualitative data were also collected with open-ended questions.
Results
There were no major difficulties with the use of devices, and any difficulties that did arise were solved through practice. There were adequate levels of pleasantness and perceived utility of the proposed intervention. The main perceived benefits were distraction, entertainment, and promotion of relaxation states. Regarding mood changes, an increase in positive emotions and a decrease in negative emotions were also detected.
Conclusions
The intervention was positively assessed and rated as minimally uncomfortable. Future actions are discussed as well as the need to implement brief interventions that take into account the patients’ medical state and physical discomfort level, especially with those in the advanced stages of disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although substantial progress has been made with psychological interventions in improving the mood state of patients, this line of work has been conducted mainly with ambulatory patients and, to a lesser extent, with inpatients (e.g. [1–3]). Most psychological programs oriented to individuals with cancer have been designed and evaluated in contexts that do not include hospitalization; therefore, it is necessary to develop interventions adapted to such conditions, thereby taking into account the physical and emotional discomfort suffered by inpatients.
Emotional well-being is not only related to the decrease of negative emotions, but also to the intensity and frequency of positive emotions. Positive psychology establishes the importance of considering positive experiences and personal resources to improve quality of life [4]. In oncology, there are some interventions that include positive psychology elements, which have displayed encouraging preliminary results [5, 6]. A promising approach is one that focuses on the induction of positive emotions, especially for the benefits which these emotional experiences have in the short-term as well as in the medium- and long-term [7–12]. According to Fredrickson’s theory [9], promotion and training of positive emotions can create and strengthen useful personal resources to cope with difficult moments.
To our knowledge, there are very few studies that focus on mood induction in a clinical population, and none of them have been implemented with cancer inpatients. Some of these studies show that an induced positive affect is associated with better self-evaluations of health [13], lower sensitivity to pain [14, 15], and better emotional well-being during radiotherapy in breast cancer patients [16].
More recently, one of the tools being used to implement more efficient psychological interventions is virtual reality (VR). This technology has been utilized in the treatment of different psychopathologies and medical conditions. Specifically, in behavioral medicine, VR has been utilized with very positive results in acute pain management [17–19] and neuropsychological assessment and rehabilitation [20, 21]. In the case of cancer, VR has been employed mainly to help manage pain and anxiety associated with painful medical procedures [22–25] as well as to handle distress symptoms during chemotherapy [26–30]. Oyama [31–33] has described a VR system to help alleviate patient stress and concern during hospitalization, but so far, there are only very preliminary results. Thus, most studies have focused on the use of VR for acute or short-term distress, obtaining good results in decreasing pain, anxiety, and fear during medical procedures and making chemotherapy sessions more tolerable.
Our team has developed a mood induction procedure (MIP) using VR [34]. MIPs are experimental procedures designed to provoke transitional mood states in non-natural situations in a controlled manner [35–37]. This MIP through VR (MIP-VR) could be considered as a “positive technology” concept that combines the objectives of positive psychology with the enhancement of information and communication technologies [38, 39]. Positive technologies include those designed to increase well-being and to generate strengths and resilience in individuals, organizations, and society [38, 39]. In this sense, MIP-VR is a positive technology, as it is designed to help users achieve a positive emotional state and well-being.
In order to fulfill their purpose, it is necessary to bring these technologies to the users and contexts where they can be most useful. In hospital settings, it is necessary to consider not only the usual dynamics and working routines but also the infrastructure and the users’ conditions (medical and psychological states, visits, etc.). Considering all of this, it is relevant to assess not just the efficacy of these technologies but also to what extent its implementation in this type of context is feasible. One key aspect is the cost of the technologies. The equipment required to implement the intervention proposed in this study is easily accessible and inexpensive. It consists only of a TV and a computer with a keyboard and earphones. Furthermore, the system is intuitive and very easy to use, making it feasible for self-application and thereby lowering personnel costs.
Thus, the present study was aimed at exploring the feasibility of a psychological intervention that uses VR techniques and is focused on the induction of positive emotional states in oncology inpatients with advanced stages of disease in a usual hospital setting. The inpatients’ level of acceptance and perceived utility as well as possible benefits of this intervention were also examined. It was designed as a single-group descriptive pilot study in order to explore if this intervention could be carried out in a hospital context, if it could be applied to inpatients in advanced stages of disease, if it would be assessed as pleasant and useful by inpatients, and if it would show any preliminary evidence of efficacy in increasing positive moods. The long-term goal is to conduct a randomized clinical trial to test the efficacy of VR-based mood induction strategies that could improve well-being in oncologic patients in acute or short-term distress.
Method
Participants
Eligible patients were adults diagnosed with metastatic cancer who were hospitalized for at least 1 week, with a Karnofsky functional state ≥50, indicators of adequate organ function, and life expectancy ≥ 2 months. Exclusion criteria were serious psychopathology, legal incapacity, or brain metastasis. This study was approved by the Ethical Committee of Clinical Research of the Hospital Clínica Benidorm. Each participant signed an informed consent before starting his/her participation in this study.
Among 26 eligible patients, written consent was obtained from 20 (76.9 %), and the final sample was composed of 19 inpatients (one patient did not go through any sessions due to clinical deterioration). Age ranged from 29 to 85 years (x = 60.9; standard deviation [SD] = 14.54), 53 % were men, mostly married or living with a partner (63.2 %), and 68.4 % had an elementary educational level (26.3 % knew only how to read and write, while 42.1 % had completed 8 years of formal education as well). The most frequent causes of hospitalization were acute crisis (42.1 %) and clinical deterioration (21.1 %). The most frequent diagnoses were breast (26.3 %), lung (15.8 %), stomach (10.5 %), rectum (10.5 %), and bladder (10.5 %) cancer. Concerning emotional state, 10.5 % of patients (N = 2) were taking antidepressant medication and 10.5 % were taking anxiolytics (none of them changed their medication dosage during the intervention).
Measures
Visual analog scale: mood
This consisted of seven items. Five items assessed the intensity of several emotions (joy, sadness, anxiety, relax, and vigor) in a scale from 1 (“not at all”) to 7 (“completely”). One item assessed general mood state (a scale of 1–7, where 7 was equivalent to positive mood and well-being). Finally, a question assessed subjective mood change after the session. Participants compared their current state with how they felt before the session, from “much worse” (−3) to “much better” (+3).
Visual analog scale: physical discomfort
This consisted of three items to assess the level of fatigue, pain, and physical discomfort before and after each session, using a 0 (“not at all”) to 10 (“completely”) scale.
Visual analog scale: satisfaction
This consisted of two post-session items to assess satisfaction degree with each session (“Did you like today’s activity?” and “Do you think that today’s session has been useful or beneficial?”) using a 0 (“not at all”) to 10 (“very much so”) scale.
Satisfaction with intervention scale
This was an adapted version of Borkovec and Nau’s (1972) instrument [40]. It assessed the level of intervention satisfaction regarding five aspects: logic (“How logical does this psychological program seem to you?”), satisfaction (“How satisfied are you with the psychological program?”), recommendation (“How confident would you be in recommending this psychological program to a friend who is experiencing a similar situation?”), utility (“How useful do you think this program has been for you?”), and discomfort (“How annoying or uncomfortable has this program been for you?”), using a 0 (“not at all”) to 10 (“completely”) scale. This instrument was applied at the end of the program.
Open-ended questions
Once each session had ended, the clinician asked patients open-ended questions about the level of involvement, difficulties experienced, presence of side effects, emotionally significant events, medical conditions that interfered with the session, and other assorted comments.
Intervention
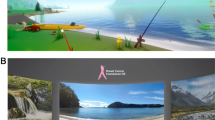
Intervention was focused on the induction of joy and relaxation, and it was composed of four sessions administered during 1 week. Each session lasted approximately half an hour. The first and third sessions were oriented to joy induction and the second and fourth to relaxation induction. To induce joy and relaxation, two virtual environments were used: “emotional parks” [34, 41] and “walk through nature” [42] (see Fig. 1).
The “emotional parks” environment represents an urban park where participants can walk. The same environment with different formal aspects (colors, lighting, etc.) and activity content is used for both emotions (joy and relaxation). The activities are guided by narratives: go to a bandstand where some self-statements and self-images (from the International Affective Picture System [43]) appear and visit an open air cinema where a brief video can be watched (for a more comprehensive description, see [34, 41]).
The “walk through nature” environment represents a walk in a forest and includes variations to induce joy or relaxation. Users follow a predetermined path where it is possible to stop and look around. Besides this, there are several exercises depending on the emotion to be induced: slow breathing, mindfulness, autobiographical memories, and a walk to a lake (for a more comprehensive description, see [42]).
Equipment
Virtual environments were shown on a 32-in. LCD television connected to a computer, both were installed on a trolley that allowed movement from one room to another (see Fig. 2). A keyboard and mouse were used as interaction devices and participants used headphones.
Procedure
All sessions were administered in the participants’ rooms by the psychologist. Before starting the program, participants were shown how to navigate through the virtual environments. In the first two sessions, patients could choose the environment (“emotional park” or “walk through nature”); however, the first session was focused on joy and the second one was focused on relaxation. In the following sessions, participants visited the alternate environments (third session for joy and fourth one for relaxation). Before and after sessions, mood and physical discomfort were assessed, and at the end of every session, patients also rated their degree of satisfaction. At the end of the program, the patients’ satisfaction with the intervention was assessed.
Results
Although the intervention was composed of four sessions, eight patients received fewer sessions (five patients received one session, two patients received two sessions, and one patient received three sessions). The reasons were discharge (N = 4), high physical discomfort (N = 2), presence of other worries (N = 1), and voluntary withdrawal (N = 1).
Efficacy of emotional induction through VR
Descriptive statistics of mood and physical discomfort are shown in Table 1. In order to analyze the differences between pre-session and post-session scores, t tests were applied. Although after each session increments in joy and relaxation as well as reductions in sadness and anxiety intensity could be observed, statistically significant differences were only detected in the second session (increases in general mood [t = −4.616, p < 0.001, η 2 = 0.621] and relaxation [t = −2.110, p < 0.05, η 2 = 0.255] and a decrease in sadness [t = 3.580, p < 0.003, η 2 = 0.496]) and the fourth session (increase in joy [t = −3.202, p < 0.009, η 2 = 0.506]).
A Pearson correlation was also applied to analyze possible relations between emotional state, physical discomfort, and changes from pre-session to post-session. First, there were positive and statistically significant correlations between pre-session and post-session measures (in emotional and physical discomfort measures) (r = 0.503 to r = 0.962). Considering this, low levels of sadness or pain pre-session were related to low levels of these states post-session. However, after sessions, no clear trends were detected either between physical discomfort and improvement or between emotional state and improvement (see Tables 2 and 3).
Satisfaction with the intervention program
Levels of satisfaction were moderately positive (see Table 4). All scores were higher than 5 (on a 0–10 scale) and participants did not rate the intervention as uncomfortable (x = 0.65).
Regarding qualitative data, participants commented that they had liked the proposed activities and that they had been fun. Participants found the program to be meaningful, purposeful, entertaining, and pleasant. Participants found it nice due to the possibility to enjoy nature and the chance to reminisce over their lives and because the details were rewarding. One patient commented: “this would cheer anyone up,” “there should be one [television] in every room…today I am going to the forest, tomorrow I am going to the beach…” Participants also pointed out the distraction effect and the possibility to perform an activity out of the ordinary (“at least my state of mind changes a little”).
Regarding negative comments, two users complained about navigation restrictions and two participants suggested that some elements were lacking (people, vegetation, etc.). One participant emphasized the importance of taking into account the patients’ willingness and that it should not be an obligatory activity.
Reasons for recommending the program were distraction (“for a few moments you forget about a lot of things”), the pleasantness of walking through the virtual environments, its purposefulness, usefulness, and ability to increase relaxation state (“it is well made, well developed and well planned, I was skeptical at first… I would recommend it”).
Despite the positive views of the participants, it is important to bear in mind that the quantitative ratings were moderate.
First session
Participants indicated that it was pleasant (Visual Analog Scale [VAS] = 6.97) and moderately useful (VAS = 5.50) (on a 0–10 scale). At the end of the session, 11 users rated their mood as “a little better,” one user rated it as “much better,” and four users reported that their mood did not change (“the same”). The walk had to be shortened for these four participants (two users experienced physical discomfort, one user felt drowsiness, and one user received a family visit).
Second session
This session obtained the best appraisal in pleasantness (VAS = 7.11) and utility (VAS = 6.43). At the end of the session, only two users reported that their mood did not change (“the same”), eight users rated it as “a little better,” and four users rated it as “better.” Only one user felt discomfort. Three users decided to end the activity early: two participants reported that it was nice, but they were tired and preferred to finish and one participant did not want to bother her roommate during her mealtime.
Third session
This session was positively assessed both on pleasantness (VAS = 6.54) and utility (VAS = 6.29). At the end of the session, five users rated their mood as “a little better,” one user rated it as “better,” and another one as “much better.” Only two participants decided to finish early due to physical discomfort. However, one of them enjoyed the session.
Fourth session
Levels of pleasantness (VAS = 6.1) and perceived utility (VAS = 4.3) were moderately positive. Six users reported that their mood did not change (“the same”), two users rated it as “a little better,” two users rated it as “better,” and one user rated it as “much better.” Four participants reported tiredness and discomfort during the session.
Usage difficulties
Participants reported that the system was relatively easy to use. The only difficulty was with the interaction devices in the two first sessions when users explored the virtual environments for the first time. Performance improvements were observed during sessions and all difficulties were solved with practice. In general, users were willing to learn and faced any difficulty experienced with a good attitude and humor. Only twice did the clinician use interaction devices for the participants: for a woman hospitalized in the intensive care unit and for a user who felt a high level of discomfort. In both cases, participants made the movement and action decisions.
Participants’ posture did not facilitate interaction with the environments because some patients were lying in bed. This posture made mouse movements difficult and provoked involuntary key strokes. Once, the VR program had to be started three times because the patient accidentally pressed the keyboard (however, the patient rated the session positively).
Other difficulties came from the hospital room context. On several occasions, sessions were disturbed by visits from relatives (for the patient or for his/her roommate), staff entering, telephone calls, roommates watching TV, and so on. Nevertheless, participants did not complain about these interferences. Most of the time, the patients were momentarily distracted, but were then able to refocus.
Regarding side effects, four participants reported tiredness related to the uncomfortable position during the session. Only one user reported a slight increase of preexisting dizziness.
Conclusions
The present study offers data about user satisfaction and feasibility of VR-based psychological interventions with patients with serious medical conditions in a hospital setting. Overall, the intervention was positively assessed by participants. Patients rated it as pleasant and somewhat useful, and they said that they would recommend it to others. In addition, a relevant percentage of patients reported that they felt better after the session, and in the second and fourth sessions, mood change scores even reached statistical significance. However, it must be noted that the quantitative reports were less positive than the qualitative ones. Although through quantitative means patients indicated that they were satisfied with the intervention and they rated is as useful, it was during their spontaneous comments and explanations that the more detailed information arose. The main perceived benefits were distraction, entertainment, and relaxation. Furthermore, participants reported that it was easy to learn, and although at several times the conditions were not favorable and the patients’ preexisting level of physical discomfort was high, users found the experience rewarding. Almost all participants said that they would willingly repeat it. Only four participants refused to continue the intervention: two participants because of a high degree of physical discomfort (related to the illness), one participant because he was worried about the evolution of his illness, and one patient who said that one session was enough.
Results from the present study suggest that a VR-based positive mood induction program was feasible to implement in a real hospital setting. Its short duration (half an hour) made its incorporation within the hospital routine possible, and the mobile equipment simplified participants’ access.
Although these are very preliminary data, results are encouraging and the information obtained will be very useful in improving the content and implementation of sessions. For instance, given the advanced phase of the participants’ diseases, it would be convenient to shorten sessions and schedule them for the time of day at which patients feel least discomfort (in this study, intervention sessions followed a fixed schedule) to help prevent tiredness and improve attention and engagement. Regarding interaction devices, it would be preferable to use a rumble pad instead of a keyboard.
The present study has some limitations that should be noted. Firstly, the size of the sample is small, which makes data mostly qualitative and descriptive. It will be necessary to contrast the present findings with larger samples in order to corroborate the results detected in this group. Secondly, the study did not include a control group (which, for example, might watch a TV program or listen to music) with which to compare. Thirdly, to shorten assessment time and to facilitate measurement before and after sessions, we chose to simplify the assessment using VAS. These measurements are useful but also have their limitations. Fourthly, this intervention is technology dependent, which broadens intervention possibilities but also implies additional aspects to consider when implementing it. Finally, the duration of the intervention was only 1 week. Longer interventions may achieve better results by reducing the effects of the lack of familiarity with the devices. Future research should determine the optimal duration of these interventions and their usefulness with long-term inpatients. Related to this issue, the duration of the effect of mood induction is also unknown. In future studies, it could be worthwhile to incorporate several assessments of mood and physical discomfort (immediately after sessions but also several hours later, or more, if possible) given that this could provide valuable information about emotional fluctuations.
So far, VR has been used mainly as a distraction procedure in oncology patients with less severity. To our knowledge, the only studies that deal with the implementation of VR techniques on hospitalized patients with advanced cancer are those by Oyama [31, 33]; however, he only described a VR system and presented very preliminary data about patients’ preferences. The present study is a step forward in exploring new possibilities of psychological intervention through VR in oncology. It pursues the promotion of positive emotional states during hospitalization with a standardized, brief, and simple method. Although in this group of patients emotional changes were quantitatively small, they are encouraging when the elevated discomfort while using the program and their advanced stages of disease are taken into account.
In the case of patients with advanced stages of disease, it is necessary to find alternative ways (not only pharmacological ones) to promote positive moods. This kind of emotion is not only related to well-being but also to the enhancement of self-efficacy and coping [7, 8, 12, 44].
Taking into account the benefits of positive emotions on health [10–12], VR positive mood induction would also be useful for patients with less advanced stages of disease. At the moment, our group is assessing the intervention response on inpatients with different stages of disease in order to discover if medical severity is an influencing factor.
In conclusion, VR-based mood induction strategies are a feasible procedure for promoting positive mood in cancer inpatients in a hospital context and are worthy of further study. To undertake a randomized controlled trial of this intervention, further developments are needed regarding interaction devices, content diversity of the VR program, timing and duration of the intervention, and medical status of patients (cancer stages). Since offering integral care to oncology patients is fundamental, it becomes necessary to have strategies oriented to promote well-being, especially when patients have to cope with hospitalization. In this sense, “positive technologies” can be a resource worthy of consideration by health care professionals.
References
Bellver A, Sánchez-Cánovas J, Santaballa A, Munárriz B, Pérez-Fidalgo J, Montalar J (2009) Mujeres con cáncer de mama: evaluación del afecto positivo y negativo y valoración de un programa de intervención psicológica en el ámbito hospitalario. Psicooncol 6:139–154
León-Pizarro C, Gich I, Barthe E, Rovirosa A, Farrús B, Casas F, Veger E, Biete A, Craven-Bartle J, Sierra J, Arcusa A (2007) A randomized trial of the effect of training in relaxation and guided imagery techniques in improving psychological and quality-of-life indices for gynecologic and breast brachytherapy patients. Psycho Oncol 16:971–979. doi:10.1002/pon.1171
Robb S, Clair A, Watanabe M, Monahan P, Azzouz F, Stouffer J, Ebberts A, Darsie E, Whitmer C, Walker J, Nelson K, Hanson-Abromeit D, Lane D, Hannan A (2008) Randomized controlled trial of the active music engagement (AME) intervention on children with cancer. Psycho Oncol 17:699–708. doi:10.1002/pon.1301
Seligman M, Csikszentmihalyi M (2000) Positive psychology. Am Psychol 55:5–14
Ochoa C, Sumalla E, Maté J, Castejón V, Rodríguez A, Blanco I, Gil F (2010) Psicoterapia positiva grupal en cáncer. Hacia una atención psicosocial integral del superviviente de cáncer. Psicooncol 7:7–34
Ramachandra P, Booth S, Pieters T, Vrotsou K, Huppert F (2009) A brief self-administered psychological intervention to improve well-being in patients with cancer: results from a feasibility study. Psycho Oncol 18:1323–1326. doi:10.1002/pon.1516
Cohn M, Fredrickson B, Brown S, Mikels J, Conway A (2009) Happiness unpacked: positive emotions increase life satisfaction by building resilience. Emotion 9:361–368
Folkman S, Moskowitz J (2000) Positive affect and the other side of coping. Am Psychol 55:647–654
Fredrickson B (2001) The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. Am Psychol 56:218–226
Lyubomirsky S, King L, Diener E (2005) The benefits of frequent positive affect: does happiness lead to success? Psychol Bull 131:803–855
Pressman S, Cohen S (2005) Does positive affect influence health? Psychol Bull 131:925–971
Tugade M, Fredrickson B, Barrett L (2004) Psychological resilience and positive emotional granularity: examining the benefits of positive emotions on coping and health. J Pers 72:1161–1190
Salovey P, Birnbaum D (1989) Influence of mood on health-relevant cognitions. J Pers Soc Psychol 57:539–551
Adams E, McGuire F (1986) Is laughter the best medicine? A study of the effects of humor on perceived pain and affect. Act Adapt Aging 8:157–175
Pickett C, Clum G (1982) Comparative treatment strategies and their interaction with locus of control in the reduction of postsurgical pain and anxiety. J Consult Clin Psychol 50:439–441
Schnur J, David D, Kangas M, Green S, Bovbjerg D, Montgomery G (2009) A randomized trial of a cognitive–behavioral therapy and hypnosis intervention on positive and negative affect during breast cancer radiotherapy. J Clin Psychol 65:443–455
Hoffman H, Patterson D, Carrougher G, Nakamura D, Moore M, García-Palacios A, Furness T III (2001) The effectiveness of virtual reality pain control with multiple treatments of longer durations: a case study. Int J Hum Comput Interact 13:1–12
Wiederhold M, Wiederhold B (2007) Virtual reality and interactive simulation for pain distraction. Pain Med 8:S182–S188
Li A, Montaño Z, Chen V, Gold J (2011) Virtual reality and pain management: current trends and future directions. Pain Manag 1:147–157
Schultheis M, Himelstein J, Rizzo A (2002) Virtual reality and neuropsychology: upgrading the current tools. J Head Trauma Rehabil 17:378–394
Flanagan S, Cantor J, Ashman T (2008) Traumatic brain injury: future assessment tools and treatment prospects. Neuropsychiatr Dis Treat 4:877–892
Gershon J, Zimand E, Pickering M, Rothbaum B, Hodges L (2004) A pilot and feasibility study of virtual reality as a distraction for children with cancer. J Am Acad Child Adolesc Psychiatr 43:1243–1249
Nilsson S, Finnstrôm B, Kokinsky E, Enskâr K (2009) The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. Eur J Oncol Nurs 13:102–109
Windich-Biermeier A, Sjoberg I, Dale J, Eshelman D, Guzzetta C (2007) Effects of distraction on pain, fear, and distress during venous port access and venipuncture in children and adolescents with cancer. J Pediatr Oncol Nurs 24:8–19
Wolitsky K, Fivush R, Zimand E, Hodges L, Rothbaum B (2005) Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychol Health 20:817–824
Oyama H, Kaneda M, Katsumata N, Akechi T, Oshuga M (2000) Using the bedside wellness system during chemotherapy decreases fatigue and emesis in cancer patients. J Med Syst 24:173–182
Schneider S, Ellis M, Coombs W, Shonkwiler E, Folsom L (2003) Virtual reality intervention for older women with breast cancer. CyberPsychol Behav 6:301–307
Schneider S, Hood L (2007) Virtual reality: a distraction intervention for chemotherapy. Oncol Nurs Forum 34:39–46
Schneider S, Kisby C, Flint E (2011) Effect of virtual reality on time perception in patients receiving chemotherapy. Support Care Canc 19:555–564
Schneider S, Prince-Paul M, Allen M, Silverman P, Talaba D (2004) Virtual reality as a distraction intervention for women receiving chemotherapy. Oncol Nurs Forum 31:81–88
Oyama H (1998) Virtual reality for palliative medicine. In: Riva G, Wiederhold B, Molinari E (eds) Virtual environments in clinical psychology and neuroscience: methods and techniques in advanced patient therapist interaction. IOS Press, Amsterdam. Available at http://www.cybertherapy.info/pages/book2.htm. Accessed 20 August 2010
Oyama H, Ohsuga M, Tatsuno Y, Katsumata N (1999) Evaluation of the psycho-oncological effectiveness of the bedside wellness system. CyberPsychol Behav 2:81–84
Oyama H, Wakao F, Okamura H (1997) Virtual reality for the palliative care of cancer. In: Riva G (ed) Virtual reality in neuro-psycho-physiology. IOS Press, Amsterdam, pp 87–94
Baños RM, Liaño V, Botella C, Alcañiz M, Guerrero B, Rey B (2006) Changing induced moods via virtual reality. In: Ijsselsteijn WA, de Kort Y, Mldden C, Eggen B, van der Hoven E (eds) Persuasive technology: lecture notes in computer science. Springer, Berlin, pp 7–15
Gerrard-Hesse A, Spies K, Hesse FW (1994) Experimental inductions of emotional states and their effectiveness: a review. Br J Psychol 85:55–78
Martin M (1990) On the induction of mood. Clin Psychol Rev 10:669–697
Westermann R, Spies K, Stahl G, Hesse FW (1996) Relative effectiveness and validity of mood induction procedures: a meta-analysis. Eur J Soc Psychol 26:557–580
Riva G, Baños RM, Botella C, Wiederhold BK, Gaggioli A (2012) Positive technology: using interactive technologies to promote positive functioning. CyberPsychol Behav 15:69–77
Botella C, Riva G, Gaggioli A, Wiederhold BK, Alcaniz M, Baños RM (2012) The present and future of positive technologies. CyberPsychol Behav 15:78–84
Borkovec TD, Nau SD (1972) Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatr 3:257–260
Baños RM, Botella C, Rubio I, Quero S, García-Palacios A, Alcañiz M (2008) Presence and emotions in virtual environment: the influence of stereoscopy. CyberPsychol Behav 11:1–8
Botella C, Etchemendy E, Castilla D, Baños RM, García-Palacios A, Quero S, Alcañiz M, Lozano JA (2009) An e-health system for the elderly (Butler Project): a pilot study on acceptance and satisfaction. Cyberpsychol Behav 12:255–262
Lang PJ, Bradley MM, Cuthbert BN (2008) International affective picture system (IAPS): affective ratings of pictures and instruction manual. Technical Report A-8, University of Florida, Gainesville, Florida
Ong A, Bergeman C, Bisconti T, Wallace K (2006) Psychological resilience, positive emotions and successful adaptation to stress in later life. J Pers Soc Psychol 91:730–749
Acknowledgments
This work was partially funded by Generalitat Valenciana, PROMETEO (2008/157), Ministerio de Ciencia y Tecnología (PSI2010-09568-E). CIBER Fisiopatología de la Obesidad y Nutrición is an initiative of ISCIII.
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose. The authors have no financial relationship with the organization that sponsored the research. The authors have full control of all the primary data and agree to allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baños, R.M., Espinoza, M., García-Palacios, A. et al. A positive psychological intervention using virtual reality for patients with advanced cancer in a hospital setting: a pilot study to assess feasibility. Support Care Cancer 21, 263–270 (2013). https://doi.org/10.1007/s00520-012-1520-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1520-x