Abstract
Previous studies show that the lack of information about cancer-related topics (e.g., diagnosis, treatments) and the impact of treatment toxicity on patients’ life, may undermine cancer patients’ psychological well-being. Psycho-educational interventions are therefore implemented to support the oncological population. This systematic review aims to explore the state of art and effectiveness of psychological and educational interventions implemented using Virtual Reality and designed for pediatric and adult cancer patients. The review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA), and it was registered with the PROSPERO international prospective register of systematic reviews (registration number CRD42022308402). Twenty studies were included in the review. Our findings show that psychological interventions predominantly use emotion-focused strategies (i.e., distraction) to reduce patients’ emotional distress; educational studies prefer, on the contrary, cognitive-behavioral strategies (i.e., exposure) to restructure patients’ beliefs, increasing their understanding of the procedure, and reducing situational anxiety. VR could be a promising and effective tool for supporting cancer patients’ needs. However, since most of these VR interventions assign the patient a passive role in coping with his or her diagnosis, future research should develop psychological and educational VR interventions that have the primary goal of rendering people with a cancer diagnosis active characters in their psychological well-being, supporting in this way patients’ empowerment.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Virtual Reality
- Cancer
- Psychological intervention
- Educational intervention
- Systematic review
- Emotion regulation
- Well-being
1 Introduction
Cancer is a life-threatening disease that leads patients to experience emotional distress [1, 2]. The impact of cancer treatments on patients’ functionality and appearance adds an extra source of stress in patients’ lives [3], contributing to a further decline in their mental health [4]. These combined factors undermine patients’ well-being (e.g., [5,6,7]), threaten their compliance [8, 9], endanger treatment outcomes [10], and increase their risk of mortality [11,12,13]. Additionally, the lack of information about cancer experience and treatment side effects may jeopardize to a greater extent patients’ mental health [14], representing one of the unmet needs of this clinical population [15, 16]. Therefore, to support patients’ mental health [17], educational (e.g., [18, 19]) and psychological interventions (e.g., [20,21,22]) are implemented. Psychological interventions buffer patients’ emotional distress and reduce negative mood states using emotional, cognitive, or behavioral strategies [23]. Educational interventions are, on the other hand, based on the premise that exposure to care-related information provides coping assistance to patients, by offering answers to their search for information. This process restructures how the cognitive assessment of events is perceived (e.g., being stressful) and, consequently, reduces the associated situational anxiety [24].
Over the last decades, thanks to technological advancement and to the possibility to have affordable devices, health care has witnessed a switch, passing from in-person interventions to therapies that use technological devices. Thus, it is not surprising that the usage of virtual reality (VR) in the medical field has gradually increased [25, 26]. Recent studies have shown that VR is not only broadly used in treating mental health problems [27], but that it is also effective in health care [28]. VR allows the user to navigate and interact in real-time with a 3D environment [29], making it possible for patients to experience situations that would otherwise be impractical or difficult to access [30]. These characteristics are particularly pertinent in the oncological setting, where treatment toxicity (e.g., pain, fatigue, nausea) impairs physical functioning [31, 32] and leads to hospitalizations [33], rendering it complicated for cancer patients to attend in-person therapies or educational training. VR appears as a possible solution to overcome the barriers that oncological treatments create: thanks to VR patients can face situations, as well as receive interventions, without leaving their room, with the quality of an in vivo experience [30], and feeling present in the situation [34]. VR is a particularly suitable tool also for its capability to visually show realistic scenarios to users, through an experiential form of imagery [35]. This quality, combined with a well-structured narrative [36], is very helpful when patients have difficulties picturing the situations they are told to imagine [35], for example when staff explains how the surgical procedure will be performed or how radiotherapy works. Therefore, VR may assist nurses and surgeons in visually showing to patients the steps of the oncological procedure, avoiding misinterpretations, and reducing procedural anxiety [18]. Misunderstandings about treatment benefits and harms can, in fact, lead patients to regret the decision taken and the treatment accepted [37]: when patients do not fully understand the implications of the procedure or have incomplete information about outcomes are more susceptible to regret [38], risking to make poorly informed decisions about their oncological journey. The uncertainty in a negative situation makes the situation more unpleasant [39], potentially causing distress and poor health outcomes [40]. For this reason, being able to overcome this problem would be extremely valuable for patients’ well-being. VR is already used in oncological settings. However, its major application is planning or simulating surgeries (e.g., resection of the tumor mass), as well as training residents or medical specialists to implement oncological procedures (e.g., surgery, radiotherapy, etc.) (e.g., [41,42,43,44,45,46]).
Since VR has the potential to support cancer patients’ well-being, this systematic review aims to explore the state of the art of psychological and educational interventions among adult and pediatric cancer patients. It seems, in fact, essential to create an accessible understanding of how VR is used in the psycho-oncological setting, and which are its possible future uses. Hence, our research questions are:
-
RQ1: Which are the current educational and psychological interventions for cancer patients that use VR for their implementation?
-
RQ2: Which is the effectiveness of such VR interventions?
Interventions will be considered effective when there is a statistically significant improvement in the measures of interest for the intervention group compared to the control group.
2 Methods
A systematic review of scientific literature has been performed to identify studies that report the employment of psychological and educational VR intervention on cancer patients. This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [47], and the study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) in 2022 (CRD42022308402). The detailed protocol is available upon request.
2.1 Data Sources and Search Strategy
Data sources were collected on the 14th of January 2022 through a selective computer search in the following databases: PubMed, PsycINFO, and Web of Science (Web of Knowledge). The current systematic review wants to offer a broad panoramic of the current literature: for this reason, we did not define a beginning year of publication for the articles to be included. Each database was searched independently, according to a specific iteration research string:
-
(Virtual Reality) AND (“Cancer” OR “Oncology” OR “Chemotherapy” OR “Cancer treatment” OR “Cancer care” OR “Cancer support”).
To make this study repeatable in the future, detailed results are available in Table 1. The selection of these strings was made in the attempt to capture an extensive range of features regarding VR interventions and cancer patients. This systematic review focused on immersive VR, which comprehends technologies in which users wear head-mounted displays and are surrounded by enclosed virtual environments [48]. In other words, virtual environments are immersive when the user experiences a sense “of being there”: the person feels in the virtual environment even if they are physically situated in another place [34]. Citations were retrieved independently for each iterative search crossing all databases. A complete list of citations and abstracts for each database was exported and imported into Rayyan [49] for the title and abstract screening.
2.2 Study Selection and Inclusion Criteria
Two reviewers (M.S. and C.M.) independently screened all non-duplicate titles and abstracts, searching for eligible articles. The same reviewers retrieved, and analyzed the full text for all relevant articles, resolving discrepancies by consensus. G.R. was designated as the third reviewer to arbitrate potential differences in agreement.
Participants
We included patients (both pediatric and adult) diagnosed by a practitioner with cancer (all cancer diagnoses and stages were included). Both female and male participants were included. Patients with metastases or undergoing palliative care were included, too. We did not include studies focused on caregivers of cancer patients, oncological professionals (e.g., nurses, surgeons, etc.), or with a mixed sample of participants (i.e., studies that also included cancer patients, but that were not limited to them). In addition to this, we did not include interventions implemented on patients with benign neoplasms, or who have not received a cancer diagnosis yet (e.g., waiting for the biopsy result).
Interventions
We focused on interventions tailored both for cancer treatments (e.g., chemotherapy) and procedures (e.g., subcutaneous port access). We included studies that considered behavioral, emotional, educational, and cognitive interventions (e.g., cognitive restructuring), including those that targeted cancer fatigue and cancer pain. Studies that focused only on the assessment of psychological (e.g., anxiety) or educational (e.g., health literacy) dimensions were not included in the systematic review, but we did include interventions that aimed to improve those features. We did not include studies that focused on neuropsychological functions (e.g., sleep, attention, memory, etc.), and treatments’ side effects (e.g., lymphedema, memory impairment, etc.). We excluded studies that were developed to improve surgeons’ skills or training, focused on detecting or removing the tumor mass (e.g., computer-assisted surgery, VR to plan post-surgery reconstruction, VR to plan tumor resection, etc.), cancer screening interventions or medical procedures to diagnose cancers (e.g., biopsy).
Methodological Characteristics of the Studies
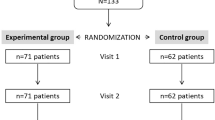
We included both cross-sectional studies and studies with repeated measures. We included randomized controlled trials, but randomization was not a requirement since it can be difficult to implement within social science intervention research (e.g., ethical reasons) [50]. We did not include qualitative studies. We excluded non-English published studies, studies that used animals, and articles in which the full text was not available. We also excluded the following types of manuscripts: reviews, meeting abstracts, conference proceedings, notes, case reports, letters to the editor, research protocols, patents, editorials, books or chapters, and other editorial materials. We excluded studies that did not use validated measures, and studies that used only some of the items of the validated measure (i.e., when the items used do not allow to calculate the total score or a subscale of the validated measure). In the case of studies with a pediatric population, we only included papers that also provided a self-report measure of the minor. We only included studies that presented a control group of healthy subjects or cancer patients, or studies with repeated measures of the same group of participants (e.g., within-subject design). The included studies needed to compare the experimental condition with a group of participants undergoing the same type of intervention, a different type of intervention, non-intervention, or standard care to point out the effectiveness of the VR condition (Fig. 1).
2.3 Risk of Bias Assessment
To assess the risk of bias, the reviewers used the Downs and Black checklist [51]. This checklist provided an overall quality index and four subscales of quality assessment: reporting, external quality, internal validity bias, and internal validity confounding. After assigning the scores to each of the 27 items (answers are scored 0 or 1, except for one item that scored 0–2), a total score was provided. Scores could be “excellent” (24–28 points), “good” (19–23 points), “fair” (14–18 points), or “poor” (14 points or less) [51]. Two reviewers (M.S. and C.M.) independently evaluated the studies for risk of bias, and disagreements were resolved through consensus or the help of the third reviewer (G.R.).
2.4 Data Extraction
Two reviewers (M.S. and C.M.) independently extracted the following data: type of population, duration of the VR intervention, type of VR intervention, construct assessed, the content of the VR intervention, delivery modality, study design, and effectiveness compared to the control group.
3 Results
Of 4975 studies retrieved from PubMed, PsycINFO, and Web of Science, 1902 were non-duplicate. After screening all non-duplicate titles and abstracts, the full text of 105 articles was retrieved, and the studies were analyzed for the specific inclusion criteria. Of 105 studies, 25 were identified as suitable for our review. However, during the extraction process, we decided to exclude five additional studies. Reasons for removal were lack of clarity of the VR procedure and device used (n = 2), lack of immersion of the VR environment (n = 1), lack of clarity about the participants’ clinical diagnosis (n = 1), and absence of specific outcomes for the VR intervention (n = 1). Therefore, in the end, twenty studies were included in the review. Detailed information about study characteristics, including the target population, duration, and type of the VR intervention, assessed construct, content of the intervention, delivery modality, study design, and outcome measures are presented in Table 2. For the aim of this systematic review, only the results that contained psychological variables (e.g., anxiety, depression, well-being, etc.) were presented and reported in Table 2. Since only a few of the studies included physiological measures, we did not include these kinds of variables in the results and the table either.
3.1 Study Characteristics
The studies took place in eleven countries: one study took place in Japan [52], one in Spain [53], one in France [54], one in Jordan [55], one in Iran [56], and another in Canada [57]. Two studies took place in China [58, 59], Italy [60, 61], Turkey [62, 63] and Australia [64, 65]. Lastly, six studies took place in the United States [66,67,68,69,70,71]. There was a variation in sample size between the studies, ranging from 11 [67] to 126 participants [53]. Papers were published within the past 23 years (1999–2022), with over fifteen studies published in the past 3 years [52,53,54,55,56,57,58,59,60,61,62,63,64,65,66]. About the study design, ten studies were randomized controlled trials (RCT) [53, 55,56,57,58,59, 62,63,64, 71], two were characterized by a within-subjects design (i.e., repeated measures) [61, 65], four were crossover studies [66, 68,69,70], one was an observational study [54], one a prospective single-arm study [52], one an externally controlled trial [60], and one an interrupted time series study [67].
Sample Characteristics
The mean ages of participants ranged from 10 [59] to 72 years [52]. Participants of the studies were both adults [52,53,54,55, 58, 60, 61, 66, 68,69,70] and children/adolescents [56, 57, 59, 62,63,64,65, 67, 71]. Only one study [68] specifically focused on older cancer patients of at least 50 years. Most studies were conducted with female and male samples: only five studies were conducted only with female participants [54, 55, 60, 68, 69]. Of all studies, two [52, 61] recruited patients undergoing palliative care, and three focused on patients who were about to start their treatment (e.g., surgery) [53, 58, 65]. Most studies focused on patients on active treatments (e.g., chemotherapy) [54,55,56, 60, 64, 66,67,68,69,70], and patients undergoing oncological procedures (e.g., access to the venous port) [57, 59, 62, 63, 71]. In terms of diagnosis, nearly all studies enrolled patients with different cancers. Six studies enrolled only a specific oncological population, focusing on people with cervical [54], breast [55, 60, 68, 69], and colon cancer [53].
Characteristics of VR Interventions
The duration of the VR interventions was variable, going from 4–7 min in Tennant et al. [65], to eight sessions of 30-min each, once a week for 2 months in the study by Sharifpour, Manshaee, and Sajjadian [56]. Nearly all studies were psychological interventions (n = 17). These interventions shared the same underlying psychological strategy known as distraction. Distraction was implemented through different scenarios (e.g., naturalistic, games, etc.): some of them were interactive (e.g., [57]), and others were not (e.g., [59]). In general, interventions were tailored to participants’ age. Some VR interventions simulated pleasant activities or exposed the person to a relaxing virtual environment. This is the case of Niki and colleagues [52], in whose study the adult patients simulated a trip, visiting a memorable place (e.g., a shrine in Japan where one of the participants had his wedding) or a destination (e.g., a city) that they wanted to explore, but that had never the occasion to. A similar approach was used by Tennant and colleagues [64], who proposed to their young participants a trip to Australian national parks, zoos, or global city tourist spots. The study of Wolitzky and colleagues [71] also offered as a distraction a visit to a zoo. In particular, in this scenario children went to the Zoo Atlanta, and virtually explored the gorilla habitat. Varnier and colleagues [54] used as a distraction a virtual dive with a whale swimming in a peaceful environment. The authors invited the patient to slow down their breathing following the moves of the whale’s tale. This type of distraction was tailored for adult participants. Sharifpour and colleagues [56] opted for a VR video showing the young participants a stroll along the beach and a journey to the depth of the oceans. In the study by Semerci, Akgün Kostak, Eren, and Avci [63], always tailored for children, the authors opted for a roller coaster that speeded up and then slowed down in the forest accompanied by slow music. In other scenarios, the type of distraction was chosen by the participants among different options, according to their interests: Schneider, Prince-Paul, Allen, Silverman, and Talaba [69] allowed their participants to choose between a scuba diving experience, a walk into an art museum or a resolution of a mystery. Two studies by Schneider [68, 70], in addition to the scenarios mentioned above, also added the possibility to explore ancient worlds. These three studies were tailored for adult participants. Schneider [67] proposed different options when implementing the study on the pediatric population: the young patients could, in fact, choose between the experience of riding a magic carpet, solving a mystery, or staying in a haunted mansion. Moscato and colleagues [61] proposed two scenarios that adult participants could watch: the first one was a non-interactive virtual environment characterized by natural and relaxing scenarios (i.e., seascape, park, waterfall, London Bridge, mountain landscape). The second environment was an interactive scenario that consisted of a skill game where the user, surrounded by a calm underwater landscape, had to reproduce an ideogram that represented concepts like friendship, courage, or strength. Mohammed and Ahmad [55] offered as a distraction two scenarios from which adult participants could choose: deep sea diving or sitting on the beach while listening to the “Happy Place” track. Chirico and colleagues [60] opted for interaction with relaxing virtual environments: the participant explored an island, walked through a forest, observed different animals, climbed a mountain, and swam in the sea. Also this type of scenario was tailored to adult participants. Ashley Verzwyvelt, McNamara, Xu, and Stubbins [66] proposed to their adult participants nine different scenarios. They could explore tropical beaches, underwater oceans, take to the stars, discover over sixty different animals, command the weather, take control of the night, or create and shape their own world. Gerçeker and colleagues [62] offered to the children that took part in their study three different environments: swimming with marine animals underwater, riding a roller coaster, and exploring the forest through the eyes of woodland species. Some scenarios implemented the distraction through a game to play with or by watching a video without interacting with it. Hundert [57] and colleagues, for example, proposed as a distraction a game that consisted of aiming rainbow balls at sea creatures as they explored an underwater scenario in search of a treasure. In the study by Wong and colleagues [59], on the contrary, two animated videos of Minions were shown to the patients during the medical procedure to distract them. Both these types of distraction were tailored to children.
Three educational interventions were included in the systematic review. These studies focused on preparing pediatric or adult patients for therapy. In particular, Gao and colleagues [58] focused on radiation therapy, showing to the adult participants the entire radiotherapy process, from the accelerator functioning to the equipment used, while patients lay down on a couch. Tennant and colleagues [65] proposed a similar scenario by showing their young participants a 360° video displaying the radiotherapy procedure. Turrado and colleagues [53] focused on surgery instead. These authors proposed to their adult participants a scenario that revealed the various steps of admission to surgery, from the first interview with the surgeon to the operating room and postoperative recovery.
Regardless of whether they were psychological or educational, the focus of the included studies was mostly pain [52, 54,55,56,57, 59, 61,62,63,64, 66, 71] and anxiety [52,53,54,55,56, 58,59,60,61,62, 64, 65, 67,68,69,70,71]. Some studies also assessed depression [52, 53, 60, 61], anger [60, 64], fear [57, 58, 62], distress [57, 66, 71], as well as fatigue and tiredness [52, 60, 61, 68,69,70]. A few studies considered well-being [52, 61], positive mood [64], and other mood states such as tension, vigor, and confusion [60]. For more information about how the studies targeted each of the psychological dimensions, please see Table 2.
Effectiveness of VR Interventions
Four studies reported no significant differences between the VR and the control condition or between the pre-post VR intervention [57, 66, 67, 70]. Other four studies reported mixed results [58, 61, 68, 69], displaying significant improvements for some clinical dimensions but not for others. In particular, Gao and colleagues [58] reported significantly lower anxiety in the VR condition compared to the control group, but they did not find a significant reduction in the fear scores of the VR condition: the fear was lower but not significant. Schneider and colleagues [69] observed a similar trend in their study: a significant decrease in the fatigue scores was observed in the VR condition, but not in the anxiety, which was lower but not significant. Moscato and colleagues [61] reported a significant improvement in pain, depression, anxiety, and well-being scores assessed through the Edmonton Symptom Assessment System. However, no statistical difference was found in depression, anxiety, and pain scores when they used different assessment measures (i.e., Hospital Anxiety and Depression Scale and Brief Pain Inventory). Another study reported mixed results [54]: however, since the authors did not use inferential statistical analysis, it was not possible to describe the results in terms of statistical difference. What we can say is that these authors observed a greater decrease in anxiety in the control condition compared to the VR and a larger improvement in pain in the VR group. According to these findings, VR worked better in the management of pain than anxiety. Eleven studies showed a significant improvement in the VR condition compared to the controls or to the pre-VR assessment [52, 53, 55, 56, 59, 60, 62,63,64,65, 71]. Tennant and colleagues [65] showed a significant reduction of anxiety in their pediatric patients. However, this improvement did not last for long and increased again just before the beginning of the cancer treatment.
3.2 Methodological Quality of Studies
As shown in Table 3, the Downs and Black checklist [51] revealed that the methodological quality of studies was mixed. Most studies were classified as “fair” [52, 54, 56, 58, 60,61,62, 65, 66, 67, 69, 71] implying a medium risk of bias. One study [68] was classified as “poor” implying a high risk of bias, and seven other studies [53, 55, 57, 59, 63, 64, 70] were classified as “good”, implying a mild risk of bias. None of the studies was classified as “excellent” with a poor risk of bias.
4 Discussions
To the best of our knowledge, this is the first systematic review to offer a comprehensive panoramic of VR interventions implemented both with adult and pediatric cancer patients. Twenty studies were eligible for the review, and they included both educational and psychological VR interventions. The majority of these interventions showed complete or partial effectiveness of VR, demonstrating that this technology is an optimal delivering modality for psycho-educational interventions. Most studies we included in the systematic review carried out psychological interventions. The common thread between these interventions is the use of distraction as a strategy to reduce patients’ distress during medical procedures and treatments. VR distraction has been identified as a promising emotion-focused method aiming at improving tolerance during medical procedures, mostly by reducing the distress and pain that patients experience [72]. According to Lazarus and Folkman’s stress and coping model, when people acknowledge that there is nothing they can do to change a stressful situation, they tend to adopt emotion-focused coping strategies (e.g., distraction) to regulate their emotional response [73]: distraction diverts attention away from unpleasant stimuli toward intriguing ones, reducing tension and anxiety [70]. The mechanism behind the functioning of distraction is that human beings have the cognitive resources to process a limited pool of information: using the capacity for one activity limits their availability for another task, preventing other information from being processed and accessing consciousness [74]. VR is a tool of choice in achieving this goal thanks to the possibility of visually showing to the participant the distractor, and offering a sense of presence in the situation. When in the virtual environment, participants have the opportunity to interact with the distractor (e.g., playing the role of a character in the distracting virtual environment), or to just be receptive to the virtual world without interacting with it (e.g., watching a relaxing scuba dive in the ocean). In both cases the individual makes changes in their mental health in a passive way: VR distraction works due to the inability of our mind to manage so much information at the same time, not because the individual is actively involved in improving their own mental health (e.g., by learning how to cope with anxiety or self-regulate emotional distress). The perception of control over a patient’s own change improves disease management, health status, and medication adherence [75], variables that are particularly important in cancer care. For this reason, further research should compare VR distraction with other coping strategies that engage patients in a more active way, in order to investigate which is the most effective and has long-term effects on patients’ well-being. Problem-focused coping, for example, includes adaptive strategies that focus on reducing or eliminating stressors through the implementation of active behaviors [76]. In this context, problem-focused coping renders the individual actively engaged in the promotion of their mental health, and could be an important factor to develop interventions that make patients feel empowered. Another important element that emerges from this review is that educational tasks represented only a small part of the interventions implemented using VR. Even if the lack of information has been identified as an unmet need of the cancer population [15, 16], educational interventions are still limited. Results from this review show that VR educational interventions are effective both for children and adults and that they can reduce patients’ emotional distress by improving patients’ knowledge and understanding. Johnson and colleagues [77] underline that patients themselves identify VR as an appropriate and important educational tool to include in cancer care for improving patients’ understanding. Specifically, patients consider VR particularly effective in reducing anxiety thanks to the ability to recreate the spatial and acoustic aspects of cancer therapy. Educational studies generally exploit the cognitive-behavioral strategy known as exposure. Exposure-based techniques are broadly used in treating anxiety disorders: by confronting the feared stimuli and incorporating corrective information in the memory, exposure-based techniques decrease the distress experienced, disconfirming the dysfunctional associations [78]. In the educational studies we included, the authors used what we could define as an “informative exposure”. Patients are exposed through VR to a simulation of the real experience they will face once the treatment will start: by doing that, they not only reduce the uncertainty associated with the procedure but also acquire the knowledge to predict the steps they will go through. This exposure process allows the patients to restructure their expectancies, reducing the anxiety experienced before the beginning of the treatment. In medical settings where the in vivo exposure (e.g., doing with the patients a tour of the surgical room) may be time-consuming and not always possible, the benefits of adopting VR are numerous. This technology creates an immersive experience, giving the patient the feeling of being in the treatment: the patient can wander around the virtual room and view the therapy from various perspectives. Using VR also decreases the risks (e.g., contamination) associated with physically going to a sterile operating room, radiotherapy vault, or chemotherapy chair, it decreases the amount of time needed in doing the same process in person, and the human and economic resources necessary to do that. VR exposure has recognized effectiveness, greater than in vivo exposure [79], and similar to the classical evidence-based interventions with no VR exposure [80]. By virtue of exposure effectiveness, and the importance that educational interventions have in rendering patients empowered and involved in their treatment, it is extremely important to include psycho-education in cancer care and the optimal tool to reach this goal is VR.
The studies included in this review are not without their limitations. First, only half of the studies included an assessment of the adverse events that may have taken place during the VR intervention. This appears as an extremely important element to incorporate in VR interventions due to the cybersickness (i.e., nausea, headache, and dizziness) that users may experience during or after VR immersion [81]. Secondly, the studies often did not include visual material (e.g., photos, screenshots, videos) to offer more insights into the VR environments used for the intervention. The absence of a clear understanding of how the scenario looks and its specific characteristics may affect the replicability of the results, and increase the risk of bias. A third limitation is the small sample size that characterized some of the studies. Although the difficulties that clinical researchers have in recruiting patients are well recognized, when the samples are very small it is hard to draw firm findings. Thus, to assess effectiveness in a variety of therapeutic contexts, and to make concrete and stable conclusions to refer to the population of interest, future large-scale research comparing VR to other technologies is needed. Lastly, an additional limitation to these studies is that confounders are often not made explicit nor taken into account during the analysis, increasing the risk of bias of the studies. This is especially true when VR interventions are implemented for the length of the medical procedure because VR exposure is performed “as long as the procedure execution”. Being implemented from a human being on another human being, a medical procedure rarely lasts the same amount of time for different people, leading participants to different exposures both to the VR and to the control condition. Therefore, it would be essential to keep this element into account both in the analysis and in the confounders’ assessment in order to increase the methodological quality of these interventions.
In conclusion, VR seems to be a promising tool for supporting cancer patients’ well-being. Two main focuses emerged from this systematic review: psychological interventions predominantly used emotion-focused strategies (i.e., distraction) to reduce patients’ emotional distress, while educational studies employed cognitive-behavioral strategies (i.e., exposure) to restructure patients’ beliefs towards oncological treatments and reduce their anxiety. However, if on the one hand educational VR interventions support cancer patients in actively acquiring skills for coping with their diagnosis, on the other hand, psychological VR interventions surprisingly do not, assigning a passive role to the patient. For a greater adherence to medical treatments and a meaningful enhancement of patients’ psychological and physical well-being, psychological VR interventions need to switch their locus of control from an external to an internal focus, empowering patients. Psychological VR interventions have the potential to become the means to achieve patients’ empowerment, assisting them in discovering and using their own intrinsic potential to master their cancer diagnosis. When patients receive a cancer diagnosis, they feel powerless and hopeless: psycho-oncological VR interventions need to fit into this point, accompanying the patient in regaining a perception of control over their life. This will allow the clinical research to have a real impact on the clinical practice and on patients’ well-being. Therefore, future research should focus not only on improving the methodological quality of the studies but also on developing new interventions that can fulfill this essential and profound switch. It is the will of our team to develop VR experiences that embrace this change of mindset: starting from the results of this systematic review, we will harmonize psychological and educational tasks within the same VR intervention, with the aim of making the patient an active character of their own well-being [82].
References
Linden, W., et al.: Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J. Affect. Disord. 141(2–3), 343–351 (2012)
Akechi, T., et al.: Major depression, adjustment disorders, and post-traumatic stress disorder in terminally Ill cancer patients: associated and predictive factors. J. Clin. Oncol. 22(10), 1957–1965 (2004)
Rhoten, B.A., Murphy, B., Ridner, S.H.: Body image in patients with head and neck cancer: a review of the literature. Oral Oncol. 49(8), 753–760 (2013)
Bacon, C.G., et al.: The impact of cancer treatment on quality of life outcomes for patients with localized prostate cancer. J. Urol. 166(5), 1804–1810 (2001)
Taghian, N.R., et al.: Lymphedema following breast cancer treatment and impact on quality of life: a review. Crit. Rev. Oncol. Hematol. 92(3), 227–234 (2014)
Vakalopoulos, I., Dimou, P., Anagnostou, I., Zeginiadou, T.: Impact of cancer and cancer treatment on male fertility. Hormones 14(4), 579–589 (2015). https://doi.org/10.14310/horm.2002.1620
Vonk-Klaassen, S.M., de Vocht, H.M., den Ouden, M.E.M., Eddes, E.H., Schuurmans, M.J.: Ostomy-related problems and their impact on quality of life of colorectal cancer ostomates: a systematic review. Qual. Life Res. 25(1), 125–133 (2015). https://doi.org/10.1007/s11136-015-1050-3
Greer, J.A., et al.: Behavioral and psychological predictors of chemotherapy adherence in patients with advanced non-small cell lung cancer. J. Psychosom. Res. 65(6), 549–552 (2008)
Markovitz, L.C., Drysdale, N.J., Bettencourt, B.A.: The relationship between risk factors and medication adherence among breast cancer survivors: what explanatory role might depression play? Psychooncology 26(12), 2294–2299 (2017)
Pham, H., Torres, H., Sharma, P.: Mental health implications in bladder cancer patients: a review. Urol. Oncol. Semin. Orig. Investig. 37(2), 97–107 (2019)
Karvonen-Gutierrez, C.A., et al.: Quality of life scores predict survival among patients with head and neck cancer. J. Clin. Oncol. 26(16), 2754–2760 (2008)
Satin, J.R., Linden, W., Phillips, M.J.: Depression as a predictor of disease progression and mortality in cancer patients a meta-analysis reply. Cancer 116(13), 3304–3305 (2010)
Pinquart, M., Duberstein, P.R.: Depression and cancer mortality: a meta-analysis. Psychol. Med. 40(11), 1797–1810 (2010)
Mesters, N., et al.: Measuring information needs among cancer patients. Patient Educ. Couns. 43(3), 253–262 (2001)
Harrison, J.D., et al.: What are the unmet supportive care needs of people with cancer? A systematic review. Support. Care Cancer 17(8), 1117–1128 (2009)
Stead, M.L., et al.: Lack of communication between healthcare professionals and women with ovarian cancer about sexual issues. Br. J. Cancer 88(5), 666–671 (2003)
Singer, S., Das-Munshi, J., Brahler, E.: Prevalence of mental health conditions in cancer patients in acute care-a meta-analysis. Ann. Oncol. 21(5), 925–930 (2010)
Wang, L.J., Casto, B., Luh, J.Y., Wang, S.J.: Virtual reality-based education for patients undergoing radiation therapy. J. Cancer Educ. (2020). https://doi.org/10.1007/s13187-020-01870-7
Lovell, M.R., et al.: A randomized controlled trial of a standardized educational intervention for patients with cancer pain. J. Pain Symptom Manage. 40(1), 49–59 (2010)
Barrera, I., Spiegel, D.: Review of psychotherapeutic interventions on depression in cancer patients and their impact on disease progression. Int. Rev. Psychiatry 26(1), 31–43 (2014)
Guo, Z., et al.: The benefits of psychosocial interventions for cancer patients undergoing radiotherapy. Health Quality Life Outcomes 11 (2013)
Zhang, M.F., et al.: Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer a meta-analysis. Medicine 94(45) (2015)
Jassim, G.A., et al.: Psychological interventions for women with non-metastatic breast cancer. Cochrane Datab. Syst. Rev. 5 (2015)
Belleau, F.P., Hagan, L., Masse, B.: Effects of an educational intervention on the anxiety of women awaiting mastectomies. Can Oncol Nurs J 11(4), 172–180 (2001)
Pensieri, C., Pennacchini, M.: Virtual reality in medicine. In: Handbook on 3d3c Platforms: Applications and Tools for Three Dimensional Systems for Community, Creation and Commerce, pp. 353–401 (2016)
Riva, G.: Applications of virtual environments in medicine. Methods Inf. Med. 42(5), 524–534 (2003)
Kim, S., Kim, E.: The use of virtual reality in psychiatry: a review. J. Korean Acad. Child Adolesc. Psychiatry 31(1), 26–32 (2020)
Chirico, A., et al.: Virtual reality in health system: beyond entertainment. A mini-review on the efficacy of VR during cancer treatment. J. Cell. Physiol. 231(2), 275–287 (2016)
Riva, G.: Virtual reality in psychotherapy: review. Cyberpsychol. Behav. 8(3), 220–230 (2005)
Riva, G.: Virtual reality: an experiential tool for clinical psychology. Br. J. Guid. Couns. 37(3), 337–345 (2009)
Abrahams, H.J.G., et al.: Risk factors, prevalence, and course of severe fatigue after breast cancer treatment: a meta-analysis involving 12 327 breast cancer survivors. Ann. Oncol. 27(6), 965–974 (2016)
Murphy, B.A., Gilbert, J., Ridner, S.H.: Systemic and global toxicities of head and neck treatment. Expert Rev. Anticancer Ther. 7(7), 1043–1053 (2007)
Feliu, J., et al.: Prediction of unplanned hospitalizations in older patients treated with chemotherapy. Cancers 13(6) (2021)
Riva, G., Davide, F., Ijsslsteijn, W.: Being there: Concepts, effects and measurements of user presence in synthetic environments. In: Studies on New Technologies & Practices in Communication, 2003 edn. (2003)
Botella, C., et al.: Virtual reality and psychotherapy. Stud. Health Technol. Inform. 99, 37–54 (2004)
Gorini, A., et al.: The role of immersion and narrative in mediated presence: the virtual hospital experience. Cyberpsychol. Behav. Soc. Netw. 14(3), 99–105 (2011)
Diefenbach, M.A., Mohamed, N.E.: Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Invest. 25(6), 449–457 (2007)
Stryker, J.E., et al.: Understanding the decisions of cancer clinical trial participants to enter research studies: factors associated with informed consent, patient satisfaction, and decisional regret. Patient Educ. Couns. 63(1–2), 104–109 (2006)
Wallis, J.D.: Orbitofrontal cortex and its contribution to decision-making. Annu. Rev. Neurosci. 30, 31–56 (2007)
Gustafson, A.: Reducing patient uncertainty implementation of a shared decision-making process enhances treatment quality and provider communication. Clin. J. Oncol. Nurs. 21(1), 113–115 (2017)
Beyer-Berjot, L., et al.: A virtual reality training curriculum for laparoscopic colorectal surgery. J. Surg. Educ. 73(6), 932–941 (2016)
Lee, C., Wong, G.K.C.: Virtual reality and augmented reality in the management of intracranial tumors: a review. J. Clin. Neurosci. 62, 14–20 (2019)
Mazur, T., et al.: Virtual reality-based simulators for cranial tumor surgery: a systematic review. World Neurosurg. 110, 414–422 (2018)
Quero, G., et al.: Virtual and augmented reality in oncologic liver surgery. Surg. Oncol. Clin. North Am. 28(1), 31 (2019)
Schreuder, H.W.R., et al.: An “intermediate curriculum” for advanced laparoscopic skills training with virtual reality simulation. J. Minim. Invasive Gynecol. 18(5), 597–606 (2011)
van Ginkel, M.P.H., et al.: Bimanual fundamentals: validation of a new curriculum for virtual reality training of laparoscopic skills. Surg. Innov. 27(5), 523–533 (2020)
Moher, D., et al.: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PloS Medicine 6(7) (2009)
Mills, S., Noyes, J.: Virtual reality: an overview of user-related design issues revised paper for special issue on “Virtual reality: User issues” in interacting with computers, May 1998. Interact. Comput. 11(4), 375–386 (1999)
Ouzzani, M., et al.: Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 5 (2016)
Deeks, J.J., et al.: Evaluating non-randomised intervention studies. Health Technol. Assess. 7(27), iii–x, 1–173 (2003)
Downs, S.H., Black, N.: The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Commun. Health 52(6), 377–384 (1998)
Niki, K., et al.: A novel palliative care approach using virtual reality for improving various symptoms of terminal cancer patients: a preliminary prospective, multicenter study. J. Palliat. Med. 22(6), 702–707 (2019)
Turrado, V., et al.: Exposure to virtual reality as a tool to reduce peri-operative anxiety in patients undergoing colorectal cancer surgery: a single-center prospective randomized clinical trial. Surg. Endosc. 35(7), 4042–4047 (2021)
Varnier, R., et al.: Virtual reality distraction during uterovaginal brachytherapy applicators’ removal: a pilot comparative study. Brachytherapy 20(4), 781–787 (2021)
Mohammad, E.B., Ahmad, M.: Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat. Support. Care 17(1), 29–34 (2019)
Sharifpour, S., Manshaee, G., Sajjadian, I.: Effects of virtual reality therapy on perceived pain intensity, anxiety, catastrophising and self-efficacy among adolescents with cancer. Couns. Psychother. Res. 21(1), 218–226 (2021)
Hundert, A.S., et al.: A pilot randomized controlled trial of virtual reality distraction to reduce procedural pain during subcutaneous port access in children and adolescents with cancer. Clin. J. Pain 38(3), 189–196 (2022)
Gao, J., et al.: Pilot study of a virtual reality educational intervention for radiotherapy patients prior to initiating treatment. J. Cancer Educ. (2020). https://doi.org/10.1007/s13187-020-01848-5
Wong, C.L., et al.: Virtual reality intervention targeting pain and anxiety among pediatric cancer patients undergoing peripheral intravenous cannulation a randomized controlled trial. Cancer Nurs. 44(6), 435–442 (2021)
Chirico, A., et al.: Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J. Cell. Physiol. 235(6), 5353–5362 (2020)
Moscato, S., et al.: Virtual reality in home palliative care: brief report on the effect on cancer-related symptomatology. Front. Psychol. 12 (2021)
Gerçeker, G.O., et al.: The effect of virtual reality on pain, fear, and anxiety during access of a port with huber needle in pediatric hematology-oncology patients: randomized controlled trial. Eur. J. Oncol. Nurs. 50 (2021)
Semerci, R., et al.: Effects of virtual reality on pain during venous port access in pediatric oncology patients: a randomized controlled study. J. Pediatr. Oncol. Nurs. 38(2), 142–151 (2021)
Tennant, M., et al.: Exploring the use of immersive virtual reality to enhance psychological well-being in pediatric oncology: a pilot randomized controlled trial. Eur. J. Oncol. Nurs. 48 (2020)
Tennant, M., et al.: Effects of immersive virtual reality exposure in preparing pediatric oncology patients for radiation therapy. Tech. Innov. Patient Supp. Radiat. Oncol. 19, 18–25 (2021)
Ashley Verzwyvelt, L., et al.: Effects of virtual reality v. biophilic environments on pain and distress in oncology patients: a case-crossover pilot study. Sci. Rep. 11(1), 20196 (2021)
Schneider, S.M., Workman, M.L.: Effects of virtual reality on symptom distress in children receiving chemotherapy. Cyberpsychol. Behav. 2(2), 125–134 (1999)
Schneider, S.M., et al.: Virtual reality intervention for older women with breast cancer. Cyberpsychol. Behav. 6(3), 301–307 (2003)
Schneider, S.M., et al.: Virtual reality as a distraction intervention for women receiving chemotherapy. Oncol. Nurs. Forum 31(1), 81–88 (2004)
Schneider, S.M., Hood, L.E.: Virtual reality: a distraction intervention for chemotherapy. Oncol. Nurs. Forum 34(1), 39–46 (2007)
Wolitzky, K., et al.: Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychol. Health 20(6), 817–824 (2005)
Indovina, P., et al.: Virtual reality as a distraction intervention to relieve pain and distress during medical procedures: a comprehensive literature review. Clin. J. Pain 34(9), 858–877 (2018)
Lazarus, R.S., Folkman, S.: Stress, Appraisal, and Coping (1984)
Kahneman, D.: Attention and Effort, vol. 1063 (1973)
Nafradi, L., Nakamoto, K., Schulz, P.J.: Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS ONE 12(10), e0186458 (2017)
Morris, N., et al.: The relationship between coping style and psychological distress in people with head and neck cancer: a systematic review. Psychooncology 27(3), 734–747 (2018)
Johnson, K., et al.: Learning in 360 degrees: a pilot study on the use of virtual reality for radiation therapy patient education. J. Med. Imaging Radiat. Sci. 51(2), 221–226 (2020)
Kaczkurkin, A.N., Foa, E.B.: Cognitive-behavioral therapy for anxiety disorders: an update on the empirical evidence. Dialog. Clin. Neurosci. 17(3), 337–346 (2015)
Bouchard, S., et al.: Virtual reality compared with in vivo exposure in the treatment of social anxiety disorder: a three-arm randomised controlled trial. Br. J. Psychiatry 210(4), 276–283 (2017)
Opris, D., et al.: Virtual reality exposure therapy in anxiety disorders: a quantitative meta-analysis. Depress. Anxiety 29(2), 85–93 (2012)
Caserman, P., Garcia-Agundez, A., Gámez Zerban, A., Göbel, S.: Cybersickness in current-generation virtual reality head-mounted displays: systematic review and outlook. Virtual Reality 25(4), 1153–1170 (2021)
Sansoni, M., et al.: Mitigating negative emotions through virtual reality and embodiment. Front. Hum. Neurosci. 16, 916227 (2022). https://doi.org/10.3389/fnhum.2022.916227
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this paper
Cite this paper
Sansoni, M., Malighetti, C., Riva, G. (2022). Psychological and Educational Interventions Among Cancer Patients: A Systematic Review to Analyze the Role of Immersive Virtual Reality for Improving Patients’ Well-Being. In: De Paolis, L.T., Arpaia, P., Sacco, M. (eds) Extended Reality. XR Salento 2022. Lecture Notes in Computer Science, vol 13446. Springer, Cham. https://doi.org/10.1007/978-3-031-15553-6_30
Download citation
DOI: https://doi.org/10.1007/978-3-031-15553-6_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-15552-9
Online ISBN: 978-3-031-15553-6
eBook Packages: Computer ScienceComputer Science (R0)