Abstract
Goals of work
In patients with locally advanced esophageal cancer, only those responding to the treatment ultimately benefit from preoperative chemoradiation. We investigated whether changes in subjective dysphagia or eating restrictions after two cycles of induction chemotherapy can predict histopathological tumor response observed after chemoradiation. In addition, we examined general long-term quality of life (QoL) and, in particular, eating restrictions after esophagectomy.
Materials and methods
Patients with resectable, locally advanced squamous cell- or adenocarcinoma of the esophagus were treated with two cycles of chemotherapy followed by chemoradiation and surgery. They were asked to complete the EORTC oesophageal-specific QoL module (EORTC QLQ-OES24), and linear analogue self-assessment QoL indicators, before and during neoadjuvant therapy and quarterly until 1 year postoperatively. A median change of at least eight points was considered as clinically meaningful.
Main results
Clinically meaningful improvements in the median scores for dysphagia and eating restrictions were found during induction chemotherapy. These improvements were not associated with a histopathological response observed after chemoradiation, but enhanced treatment compliance. Postoperatively, dysphagia scores remained low at 1 year, while eating restrictions persisted more frequently in patients with extended transthoracic resection compared to those with limited transhiatal resection.
Conclusions
The improvement of dysphagia and eating restrictions after induction chemotherapy did not predict tumor response observed after chemoradiation. One year after esophagectomy, dysphagia was a minor problem, and global QoL was rather good. Eating restrictions persisted depending on the surgical technique used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most patients with newly diagnosed carcinoma of the esophagus present with locally advanced disease, and the outcome at this stage is poor. Based on findings of meta-analyses [17, 18], preoperative chemoradiotherapy is commonly used in clinical practice, although adequately powered phase-III trials [13, 15, 20, 29, 30, 32] have not shown a clear statistical benefit over surgery alone. However, patients responding to neoadjuvant treatment have a better survival rate than the nonresponders [27, 30]. Whether this is due to the therapy itself or to the selection of a prognostic favorable group is yet unclear. On the other hand, neoadjuvant treatment is ineffective or even harmful for the nonresponding patients with still resectable tumors [27], as it delays a potentially curative surgery and may worsen the patient’s QoL due to its side effects. In order to avoid ineffective preoperative treatment, one should be able to reliably identify the nonresponders as early as possible.
Several methods have been used to predict response to neoadjuvant therapy. Repeated computed tomography scanning, endoscopy, and endoscopic ultrasound have not been helpful in predicting early response to therapy [6, 28]. The use of therapy-induced metabolic changes in the tumor glucose metabolism by positron emission tomography (PET) has shown some reliability in adenocarcinoma of the esophagogastric junction [22, 34]. Yet, this method has not shown enough accuracy at predicting nonresponders in squamous cell carcinoma or in patients receiving chemoradiation.
An improvement of the leading symptoms early in the treatment course may also be useful as a predictor of response. The predominant symptom for this type of tumor is dysphagia [7]. Clinical experience and data from in-depth interviews with patients [33] highlight that dysphagia is a troublesome symptom affecting all aspects of the patients’ everyday life. Relief of dysphagia is often seen already 2 to 3 weeks after start of the first chemotherapy cycle. So far, no study investigated the association between early improvement in dysphagia and tumor response. The prospective longitudinal QoL study was therefore the secondary objective of a multicenter phase II trial in Switzerland for patients with locally advanced esophageal carcinoma. The treatment in this trial consisted of two cycles of induction chemotherapy, followed by chemoradiation and surgery. The first aim was to evaluate the association between improvement of dysphagia after induction chemotherapy and histopathological response after chemoradiation in order to detect the nonresponders before the start of chemoradiation. The second aim was to evaluate the long-term outcome of patient-reported symptoms and several global QoL indicators after esophagectomy in patients without relapse.
Patients and methods
Major eligibility criteria
Eligibility criteria included resectable, locally advanced squamous cell or adenocarcinoma of the thoracic esophagus or gastroesophageal junction (Siewert type I), uT3 or/and uN+ or uT4 if deemed resectable, a WHO performance status <2, normal organ function, and age between 18 and 70 years. Patients with more extensive disease were excluded based on the determination of the tumor stage by computer tomography scan, endosonography, and in most cases PET scan. Resectability of the tumor and operability of the patient was determined by a multidisciplinary team.
Treatment schedule and evaluation plan
The treatment schedule is displayed in Fig. 1. Patients were treated with two cycles of induction chemotherapy (cisplatin and docetaxel both 75 mg/m2 administered intravenously on days 1 and 21) followed by radiotherapy (45 Gy) and concomitant chemotherapy (intravenous cisplatin 25 mg/m2 and docetaxel 20 mg/m2 administered weekly) for 5 weeks and subsequent surgery. The prospective multicenter phase-II trial is based on a two-stage design including an early stopping rule. The main endpoint was histopathological remission at the time of surgery. These results have been reported elsewhere [24]. Before surgery, QoL questionnaires were completed at registration (baseline assessment), at day 1 of cycle two of chemotherapy, and at day 1 of chemoradiation. For the assessment of long-term outcome of symptoms and global QoL indicators, patients without relapse completed questionnaires quarterly after surgery for 1 year.
Evaluation of histopathological response, dysphagia, and quality of life
The histopathological tumor regression grade (TRG) after neoadjuvant therapy, as primary endpoint of the main study, was defined according to the Mandard classification [21], as validated by the Munich group [14], and confirmed by a centrally performed histopathological review. Patients with complete regression (TRG 1) or near complete regression (TRG 2) were classified as responders, while patients with an increase in the number of residual cancer cells (TRG 3), patients with residual cancer (TRG 4), and patients with absence of regressive cancer (TRG 5) were classified as nonresponders. The regression grade was related to the T stage only and not to the N stage.
Patients completed the QoL module of the European Organization for Research and Treatment (EORTC) specific to esophageal cancer (QLQ-OES24) [8].This scale was designed for use in patients undergoing surgery, chemotherapy, radiotherapy, and/or endoscopic treatment. It comprises 24 items conceptualized as six scales and five single items. Clinical and psychometric validation of the module resulted in a revised version, the EORTC QLQ-OES18 [9]. The scales analyzed in this study, i.e., dysphagia, eating restrictions, and pain, correspond with the scales of the revised version. Contrastingly, the reflux scale comprises three items compared to only two items in the revised version. These three items address problems with belching, acid indigestion, or heartburn. All QLQ-OES-24 responses were linearly transformed to scores from 0 to 100; higher scores indicate more symptoms.
Global QoL was measured with linear analogue self-assessment (LASA) indicators for physical well-being, mood, and coping effort. Validation studies are reported elsewhere [2]. Two further global indicators were included for treatment burden [4] and functional performance [3]. LASA indicators are lines of 100 mm length anchored at both ends with words describing the two extremes of the item content. The patient is asked to mark the line according to her/his estimation. Responses on global measures assessed with single items are expected to reflect the summation of the individual meaning and importance of various factors to each patient [5]. All LASA indicators range from 0 to 100, with higher scores reflecting a better condition (i.e., better physical well-being and mood, less coping effort, less treatment burden, better functional performance).
All scales were analyzed descriptively. A change of at least eight points was considered as clinically meaningful [25].
Results
Study sample
Sixty-six patients were enrolled in the trial between July 2003 and June 2006. Patients and tumor characteristics are listed in Table 1. One patient had progressive disease (PD) after induction chemotherapy; three patients had PD after chemoradiation; another four patients could not undergo surgery due to medical reasons; one refused surgery. A total of 57 patients underwent surgery. Sixty-three out of 65 patients received two cycles of induction chemotherapy, the full-dose radiation therapy, and at least four cycles of concomitant chemotherapy. Of the 57 patients who underwent surgery, 32 were classified as responders (15 with TRG 1, and 17 with TRG 2).
QoL questionnaire submission rates
Submission rates of QoL questionnaires and reasons for missing assessments are presented in Table 2. At baseline, i.e., before treatment start, all patients (100%) completed the questionnaire. Throughout the whole study, the completion rate remained above 75%. The majority of nonsubmitted QoL questionnaires were missing due to administrative errors (i.e., questionnaire not presented to the patient). One assessment had to be excluded because it was completed outside of the assessment time frame.
Early prediction of tumor response by change of dysphagia and eating restrictions
In Fig. 2, dysphagia and eating restriction scores at baseline, day 1 of cycle two of chemotherapy, and day 1 of chemoradiation are presented for responding versus nonresponding patients, respectively. In both groups, clinical meaningful improvements were observed for dysphagia (median change −11.1) until the completion of induction chemotherapy. Similarly, median score for eating restrictions improved regardless of histopathological tumor response (median change −8.3 for responders, and −16.7 for nonresponders, respectively).
Dysphagia and eating restriction scores during induction chemotherapy. Scores are displayed according to histopathological response at baseline (BL) after one cycle of chemotherapy (1× CT) and after two cycles of chemotherapy (2× CT). Solid boxes show 25th to 75th percentiles, with horizontal lines indicating median values; whisker bars represent minimal and maximal values of a standard range. A decline in scores reflects symptom improvement
The subjective improvement in dysphagia and eating restrictions during induction chemotherapy is also reflected in the low number of feeding tubes that had to be inserted during induction therapy. Four patients received a feeding tube before the start of treatment because of eating problems. However, for two of them, it was never used for nutrition. Only two patients received a feeding tube during therapy, both before the start of the second cycle of chemotherapy.
Long-term quality of life of patients without relapse
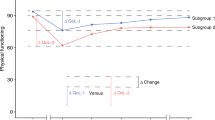
Figure 3 displays symptoms 3, 6, 9, and 12 months after multimodal treatment in patients without relapse. Dysphagia scores were low after surgery and remained on this level until 12 months after surgery, whereas eating restrictions increased after surgery and remained worse than before surgery (median score at baseline was 33.3). Taking the surgical technique into account (Fig. 4), patients with an extended transthoracic resection still suffered from considerable eating restrictions 1 year after surgery (median score 41.7). Contrastingly, patients with a limited transhiatal resection reported less eating restrictions 12 months after surgery (median 25).
Long-term course of symptoms after multimodal treatment including surgery in patients without relapse. Solid boxes show 25th to 75th percentiles, with horizontal lines indicating median values; whisker bars represent minimal and maximal values of a standard range. A decline in scores reflects symptom improvement
Eating restrictions 12 months after surgery. Scores are displayed according to the surgical technique used. Solid boxes show 25th to 75th percentiles, with horizontal lines indicating median values; whisker bars represent minimal and maximal values of a standard range. Lower scores represent a better condition (i.e., less symptoms)
In addition to eating restrictions, reflux remained a problem until 12 months after surgery with worst scores at 6 months after surgery. In contrast, pain declined continuously until the 12-month follow-up visit.
Except for physical well-being and functional performance, the median scores of the global QoL indicators were within the highest quartile 3 months after surgery and were still improving until month 12 (mood 79 to 88; coping effort 78 to 81; treatment burden 78 to 89). All three scores were higher at 12 months after surgery than at baseline. The scores for physical well-being and functional performance were slightly lower at 3 months (74 and 70, respectively) but returned to baseline levels (87 for physical well-being, 93 for functional performance) at month 12.
Discussion
Several studies evaluated the effects of different treatment modalities (i.e., combined neoadjuvant therapy followed by surgery versus surgery alone) on patient-reported dysphagia [1, 10, 19, 23, 31] or analyzed the prognostic value of baseline QoL scores for short-term outcome after surgery or survival [11]. The objective of our study was to evaluate whether the subjective estimation of an improvement in dysphagia or eating restrictions after two cycles of induction chemotherapy can predict the histopathological response observed after chemoradiation.
A clinically meaningful improvement in dypshagia and eating restrictions was found after two cycles of induction chemotherapy. This is in line with other clinical studies reporting that dysphagia and eating problems improved or stabilized during neoadjuvant therapy [1, 12, 23]. However, our results show that the improvement of these two symptoms was not associated with a histopathological response observed after chemoradiation. Therefore, the subjective symptom experience cannot accurately predict whether a patient responds to the therapy or not. One may argue that the beneficial effect of the induction therapy is caused by the steroids accompanying the chemotherapy, yet dysphagia was measured before the start of the next cycle, more than 2 weeks after the last dose of steroids. These subjective improvements in dysphagia and eating restrictions obviously led to the low number of feeding tubes needed during neoadjuvant therapy and to the high compliance with the combination of chemoradiation. Most of the patients were able to eat almost normally by the start of chemoradiation, and therefore, almost all patients completed the full chemoradiation despite the additional radiotherapy-induced mucositis. An association between changes in dysphagia or eating restrictions and long-term survival was not found either (data not shown).
A second aim of our study was to describe the subjective experience of selected symptoms and global QoL indicators over a period of 12 months after surgery in patients without relapse. Dysphagia, reflux, and pain recovered until the 12-month follow-up assessment indicating that these symptoms are minor problems 1 year after surgery. Although eating restrictions also improved postoperatively, they seem to persist at a certain level. Previous studies using identical QoL measures (i.e., QLQ-OES 18 or QLQ-OES 24) revealed mixed findings: While three studies reported that dysphagia recovered until 1 year after surgery [1, 23, 31], another study found a comparable recovery only after 3 years [19]. Regarding eating restrictions, both an improvement beyond baseline level [1] and persistent problems [19] were reported 1 year after surgery. The fact that each study used different treatments and QoL assessment timepoints may explain these inconsistent findings. Unlike our study, these studies were conducted at a single-center, and the surgical techniques were not taken into account as a comparative factor. Our results imply that the problem of persistent eating restrictions may be a side effect of the total esophagectomy. In patients who underwent extended transthoracic resection, continuous eating restrictions were more prevalent than in patients with transhiatal resection 1 year after surgery. As eating restrictions include problems enjoying meals, rapid satiety and problems with eating in general or in front of people, they can affect a person’s everyday and social life considerably. One study found no lasting differences in long-term physical and psychological QoL in patients who underwent either transhiatal or transthoracic resection [16], but the two surgical techniques were not compared against eating restrictions in particular.
With respect to the global QoL indicators, our findings confirm those of earlier studies indicating that patients still alive 1 to 5 years after surgery report on a rather good QoL [19, 23, 31]. Compared to the scores before treatment, we found a clinically meaningful improvement in mood and a decline in coping effort. This may represent an adjustment to the illness after the shock of the diagnosis or may be explained by the process of response-shift or reframing [26]. Patients change their internal standard of what means “good” or “poor” for a specific QoL domain, or they shift their personal values to a new understanding of what constitutes their QoL as a result of changing health. In contrast, physical well-being and functional performance declined 3 months after surgery indicating that patients suffer from the short-term consequences of the esophagectomy.
This is the first study investigating patient-rated dysphagia as a predictor for tumor response based on a prospective multicenter, nationwide trial with a clearly defined patient population and therapy. The risk of selection bias should be minimal. Nevertheless, some limitations deserve attention. The analyses remained descriptive due to the relatively small sample size determined by the main clinical endpoint. Yet, our findings on long-term QoL support the results of studies with larger sample sizes. A further drawback of this study is that the results reported are based on the data available from patients alive or sufficiently well to complete questionnaires. This attrition bias makes it difficult to interpret data, but it is hardly avoidable in phase II studies. We also did not consider tumor type as a potential factor contributing to the long-term outcome. In addition, follow-up data beyond 12 months after surgery are still scant.
Conclusion
This study revealed three clinically important findings. The improvement of dysphagia after two cycles of induction chemotherapy does not seem to be a useful predictor for histopathological response observed after chemoradiation. Next, the improvement in dysphagia and eating restrictions indicates that induction chemotherapy increases compliance with the subsequent chemoradiation and can avoid feeding tubes. Finally, eating restrictions seem to persist as a consequence of the esophagectomy, in particular in patients needing an extended transthoracal resection. Hence, future studies should further investigate this problem in order to inform patients about the potential sequelae of a specific surgical technique. Still, for the majority of patients, dysphagia is no longer a significant problem 1 year after esophagectomy, and the global QoL indicators recovered beyond their level at diagnosis.
References
Avery KN, Metcalfe C, Barham CP et al (2007) Quality of life during potentially curative treatment for locally advanced oesophageal cancer. Br J Surg 94(11):1369–1376 doi:10.1002/bjs.5888
Bernhard J, Hürny C, Coates AS et al (1997) Quality of life assessment in patients receiving adjuvant therapy for breast cancer: the IBCSG approach. The International Breast Cancer Study Group. Ann Oncol 8(9):825–835 doi:10.1023/A:1008269715091
Bernhard J, Lowy A, Mathys N et al (2004) Health related quality of life: a changing construct? Qual Life Res 13(7):1187–1197 doi:10.1023/B:QURE.0000037485.59681.7d
Bernhard J, Maibach R, Thurlimann B et al (2002) Patients’ estimation of overall treatment burden: why not ask the obvious? J Clin Oncol 20(1):65–72 doi:10.1200/JCO.20.1.65
Bernhard J, Sullivan M, Hurny C et al (2001) Clinical relevance of single item quality of life indicators in cancer clinical trials. Br J Cancer 84(9):1156–1165 doi:10.1054/bjoc.2001.1785
Beseth BD, Bedford R, Isacoff WH et al (2000) Endoscopic ultrasound does not accurately assess pathologic stage of esophageal cancer after neoadjuvant chemoradiotherapy. Am Surg 66(9):827–831
Blazeby JM, Alderson D, Farndon JR (2000) Quality of life in patients with oesophageal cancer. Recent Results Cancer Res 155:193–204
Blazeby JM, Alderson D, Winstone K et al (1996) Development of an EORTC questionnaire module to be used in quality of life assessment for patients with oesophageal cancer. The EORTC Quality of Life Study Group. Eur J Cancer 32A(11):1912–1917 doi:10.1016/0959-8049(96)00199-2
Blazeby JM, Conroy T, Hammerlid E et al (2003) Clinical and psychometric validation of an EORTC questionnaire module, the EORTC QLQ-OES18, to assess quality of life in patients with oesophageal cancer. Eur J Cancer 39(10):1384–1394 doi:10.1016/S0959-8049(03)00270-3
Blazeby JM, Kavadas V, Vickery CW et al (2005) A prospective comparison of quality of life measures for patients with esophageal cancer. Qual Life Res 14(2):387–393 doi:10.1007/s11136-004-0622-4
Blazeby JM, Metcalfe C, Nicklin J et al (2005) Association between quality of life scores and short-term outcome after surgery for cancer of the oesophagus or gastric cardia. Br J Surg 92(12):1502–1507 doi:10.1002/bjs.5175
Blazeby JM, Sanford E, Falk SJ et al (2005) Health-related quality of life during neoadjuvant treatment and surgery for localized esophageal carcinoma. Cancer 103(9):1791–1799 doi:10.1002/cncr.20980
Bosset JF, Gignoux M, Triboulet JP et al (1997) Chemoradiotherapy followed by surgery compared with surgery alone in squamous-cell cancer of the esophagus. N Engl J Med 337(3):161–167 doi:10.1056/NEJM199707173370304
Brucher BL, Becker K, Lordick F et al (2006) The clinical impact of histopathologic response assessment by residual tumor cell quantification in esophageal squamous cell carcinomas. Cancer 106(10):2119–2127 doi:10.1002/cncr.21850
Burmeister BH, Smithers BM, Gebski V et al (2005) Surgery alone versus chemoradiotherapy followed by surgery for resectable cancer of the oesophagus: a randomised controlled phase III trial. Lancet Oncol 6(9):659–668
de Boer AG, van Lanschot JJ, van Sandick JW et al (2004) Quality of life after transhiatal compared with extended transthoracic resection for adenocarcinoma of the esophagus. J Clin Oncol 22(20):4202–4208 doi:10.1200/JCO.2004.11.102
Gebski V, Burmeister B, Smithers BM et al (2007) Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis. Lancet Oncol 8(3):226–234 doi:10.1016/S1470-2045(07)70039-6
Graham AJ, Shrive FM, Ghali WA et al (2007) Defining the optimal treatment of locally advanced esophageal cancer: a systematic review and decision analysis. Ann Thorac Surg 83(4):1257–1264 doi:10.1016/j.athoracsur.2006.11.061
Lagergren P, Avery KN, Hughes R et al (2007) Health-related quality of life among patients cured by surgery for esophageal cancer. Cancer 110(3):686–693 doi:10.1002/cncr.22833
Le Prise E, Etienne PL, Meunier B et al (1994) A randomized study of chemotherapy, radiation therapy, and surgery versus surgery for localized squamous cell carcinoma of the esophagus. Cancer 73(7):1779–1784 doi:10.1002/1097-0142(19940401)73:7<1779::AID-CNCR2820730702>3.0.CO;2-T
Mandard AM, Dalibard F, Mandard JC et al (1994) Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer 73(11):2680–2686 doi:10.1002/1097-0142(19940601)73:11<2680::AID-CNCR2820731105>3.0.CO;2-C
Ott K, Weber WA, Lordick F et al (2006) Metabolic imaging predicts response, survival, and recurrence in adenocarcinomas of the esophagogastric junction. J Clin Oncol 24(29):4692–4698 doi:10.1200/JCO.2006.06.7801
Reynolds JV, McLaughlin R, Moore J et al (2006) Prospective evaluation of quality of life in patients with localized oesophageal cancer treated by multimodality therapy or surgery alone. Br J Surg 93(9):1084–1090 doi:10.1002/bjs.5373
Ruhstaller T, Widmer L, Balmer Majno S et al (2007) Preoperative induction chemotherapy with docetaxel-cisplatin followed by concurrent docetaxel–cisplatin and radiation therapy in patients with locally advanced esophageal cancer: a prospective, multicenter phase II trial of the Swiss Group for Clinical Cancer Research. J Clin Oncol 25:4562 (Meeting Abstracts)
Sloan JA (2005) Assessing the minimally clinically significant difference: scientific considerations, challenges and solutions. COPD 2(1):57–62 doi:10.1081/COPD-200053374
Sprangers MA, Schwartz CE (1999) Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med 48:1507–1515 doi:10.1016/S0277-9536(99)00045-3
Stahl M, Stuschke M, Lehmann N et al (2005) Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 23(10):2310–2317 doi:10.1200/JCO.2005.00.034
Swisher SG, Maish M, Erasmus JJ et al (2004) Utility of PET, CT, and EUS to identify pathologic responders in esophageal cancer. Ann Thorac Surg 78(4):1152–1160 discussion 1152-60 doi:10.1016/j.athoracsur.2004.04.046
Tepper J, Krasna MJ, Niedzwiecki D et al (2008) Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 26(7):1086–1092 doi:10.1200/JCO.2007.12.9593
Urba SG, Orringer MB, Turrisi A et al (2001) Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 19(2):305–313
van Meerten E, van der Gaast A, Looman CW et al (2008) Quality of life during neoadjuvant treatment and after surgery for resectable esophageal carcinoma. Int J Radiat Oncol Biol Phys 71(1):160–166 doi:10.1016/j.ijrobp.2007.09.038
Walsh TN, Noonan N, Hollywood D et al (1996) A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335(7):462–467 doi:10.1056/NEJM199608153350702
Watt E, Whyte F (2003) The experience of dysphagia and its effect on the quality of life of patients with oesophageal cancer. Eur J Cancer Care (Engl) 12(2):183–193 doi:10.1046/j.1365-2354.2003.00376.x
Weber WA, Ott K, Becker K et al (2001) Prediction of response to preoperative chemotherapy in adenocarcinomas of the esophagogastric junction by metabolic imaging. J Clin Oncol 19(12):3058–3065
Acknowledgements
We would like to thank Sandra Thierstein, trial coordinator of the SAKK Berne, for her tremendous administrative support for this trial, Pierluigi Ballabeni and Christian von Briel for assistance in designing this trial, Yvonne Wechsler for the development of the QoL substudy, and Jürg Bernhard and Daniela Gerber of the SAKK and Beat Thürlimann, St. Gallen, Switzerland, for editing the manuscript.
The Swiss Group for Clinical Cancer Research (SAKK) was the sponsor of the trial, and it was financially supported by the State Secretariat for Education and Research (SER) of Switzerland and Sanofi-Aventis Switzerland.
Conflict of interest
None of the authors has to declare any potential conflicts of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ribi, K., Koeberle, D., Schuller, J.C. et al. Is a change in patient-reported dysphagia after induction chemotherapy in locally advanced esophageal cancer a predictive factor for pathological response to neoadjuvant chemoradiation?. Support Care Cancer 17, 1109–1116 (2009). https://doi.org/10.1007/s00520-008-0570-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-008-0570-6