Abstract
Purpose
Cancer cachexia is a common problem among advanced cancer patients. A mixture of β-hydroxyl β-methyl butyrate, glutamine, and arginine (HMB/Arg/Gln) previously showed activity for increasing lean body mass (LBM) among patients with cancer cachexia. Therefore a phase III trial was implemented to confirm this activity.
Materials and methods
Four hundred seventy-two advanced cancer patients with between 2% and 10% weight loss were randomized to a mixture of β-hydroxyl β-methyl butyrate, glutamine, and arginine or an isonitrogenous, isocaloric control mixture taken twice a day for 8 weeks. Lean body mass was estimated by bioimpedance and skin-fold measurements. Body plethysmography was used when available. Weight, the Schwartz Fatigue Scale, and the Spitzer Quality of Life Scale were also measured.
Results
Only 37% of the patients completed protocol treatment. The majority of the patient loss was because of patient preference (45% of enrolled patients). However, loss of power was not an issue because of the planned large target sample size. Based on an intention to treat analysis, there was no statistically significant difference in the 8-week lean body mass between the two arms. The secondary endpoints were also not significantly different between the arms. Based on the results of the area under the curve (AUC) analysis, patients receiving HMB/Arg/Gln had a strong trend higher LBM throughout the study as measured by both bioimpedance (p = 0.08) and skin-fold measurements (p = 0.08). Among the subset of patients receiving concurrent chemotherapy, there were again no significant differences in the endpoints. The secondary endpoints were also not significantly different between the arms.
Conclusion
This trial was unable to adequately test the ability of β-hydroxy β-methylbutyrate, glutamine, and arginine to reverse or prevent lean body mass wasting among cancer patients. Possible contributing factors beyond the efficacy of the intervention were the inability of patients to complete an 8-week course of treatment and return in a timely fashion for follow-up assessment, and because the patients may have only had weight loss possible not related to cachexia, but other causes of weight loss, such as decreased appetite. However, there was a strong trend towards an increased body mass among patients taking the Juven® compound using the secondary endpoint of AUC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is estimated that a majority of advanced cancer patients ultimately suffer from cachexia [1]. However, there is no universally accepted definition of cancer cachexia. One accepted feature is that in cachexia there is involuntary loss of both muscle mass and fat [2]. This is in contrast to starvation, in which there is fat loss and relative sparing of muscle. Cachexia can present as a loss of appetite, but often there is weight loss despite adequate nutritional intake. According to Roubenoff, wasting is unintentional weight loss, whereas cachexia is the loss of fat-free mass with little weight loss [3]. Interventions tested against cancer cachexia in phase III trials include medroxyprogesterone [4], pentoxiphylline [5], thalidomide [6], fish oil [7], eicosapentaenoic acid [8], cannabis extract and delta-9-tetrahydrocannabinol [9], insulin [10], etanercept [11], and a mixture of β-hydroxyl β-methyl butyrate, arginine, and glutamine (HMB/Arg/Gln) [12]. Only the latter treatment has shown improvement in muscle mass, rather than fat mass.
The physiology of cachexia is not well understood. The pivotal finding in cachexia is disproportionate muscle wasting, whereas during starvation more fat than muscle is lost. The effects may be stimulated by host factors, including proinflammatory cytokines such as interleukin-1, IL-2, interferon-γ and tumor necrosis factor α [13]. Putative tumor-derived mediators include proteolysis-inducing factor (PIF) and lipid-metabolizing factor [14].
This trial was designed to evaluate the ability of HMB/Arg/Gln mixture to reverse cancer cachexia, as evidenced by loss of muscle mass. Although arginine has been shown to promote wound healing [15], and glutamine is also a regulator of muscle turnover, HMB, a leucine metabolite, is probably the most active agent in the mixture. In a recent study of HMB supplementation among critically ill trauma patients, both a HMB/Arg/Gln mixture and HMB alone attenuated the patients' negative nitrogen balance equally well when compared with placebo [16]. Eley et al. showed that HMB inhibits the effects of PIF. Whereas eicosopentaenoic acid, also a PIF inhibitor, is thought to be active by preventing the release of arachadonic acid from the cell membrane, HMB appears to attenuate phosphorylation of p42/44-mitogen-activated protein kinase by PIF [17].
A commercial formulation of this mixture, Juven®, is currently available without a prescription. A previous small randomized trial showed a statistically significant increase in both weight and lean body mass among advanced cancer patients taking HMB/Arg/Gln in the Juven® formulation [12]. Therefore, a more comprehensive, national cooperative group randomized trial of Juven® was undertaken.
Materials and methods
Eligibility
Patients receiving treatment at any RTOG full member, affiliate member, or community clinical oncology program (CCOP) member institution were candidates for inclusion in the study. Eligible patients had a stage III or IV solid cancer or currently metastatic cancer of any initial stage. They must have had at least 2% and no more than 10% weight loss over the previous 3 months. A maximum of 10% weight loss was chosen because of concern that patients with greater than 10% weight loss would deteriorate too quickly to show an effect from the intervention. They must have had a Zubrod performance status of 0–2, a life expectancy of at least 3 months and not be on any concurrent appetite-enhancing drugs.
Design
This was a randomized double-blinded trial. The patients were randomized to either active supplement for 8 weeks or placebo for 8 weeks. The active supplement consisted of 3 g of HMB, 14 g arginine, and 14 g of glutamine. The placebo was an isonitrogenous, isocaloric mixture to the HMB/Arg/Gln containing 7.72 g l-alanine, 4.28 g glycine, 2.96 g l-serine, 1.23 g l-glutamic acid, and 30.52 g gelatin. Both the placebo and HMB/Arg/Gln had an orange-drink taste. Patients took either the placebo or HMB/Arg/Gln twice a day for 8 weeks.
Lean body mass (LBM) was calculated using the Sun equations based on the reported resistance and reactance measured by bioimpedance (BIA) using the RJL Quantum II unit [18]. These equations are based on standard models of the distribution of resistance and reactance in the body tissues, and does not directly measure muscle mass. The utility of bioimpedance is its ease in use and low cost of measurement. In addition, circumference measurements were reported from the upper arm, forearm, chest, hips, and thigh. Skin-fold measurements were reported from the chest, axilla, triceps, subscapular, abdominal, suprailiac, and thigh. Videotaped instructions with measurement equipment were given to all sites. If body plethysmography (BOD POD®) was available, data from this were collected. Weight, the Schwartz Fatigue Index score, and the Spitzer Quality of Life score were also collected.
Randomization was performed using the Zelen treatment allocation scheme to balance patient factors other than institution [19]. MTI Biotech, Inc. supplied and distributed both the placebo and HMB/Arg/Gln supplements to institutions in a foil sealed packet identified by patient case number only. All study personnel and patients were blinded to treatment assignment for the duration of the study. Patients were stratified by degree of weight loss in the 3 months prior to study entry (2–5% and 6–10%), primary disease site (lung and others), concurrent chemotherapy (yes and no), and evidence of metastases (yes and no). The maximum weight loss was limited to 10% to minimize the risk that patients had progressed too far to be able to respond to therapy. Patients received an 8-week supply of the supplement at the initial visit and were scheduled to return for 4-week and 8-week follow-up visits to assess their condition. Eight weeks of supplementation was shown in previous trials to be sufficient time to see the reversal of muscle mass [12, 20].
Statistics
The primary endpoint was the percent change in LBM [baseline to 8 weeks] as measured by BIA between patients given the HMB/Arg/Gln and patients given the placebo supplement. The percent change was defined as the difference between the baseline LBM and the 8-week LBM divided by the baseline LBM multiplied by 100. Percent change was used instead of absolute change to adjust for varying baseline LBM values. Secondary endpoints were the change in fatigue (as measured by the Schwarz Fatigue Index), quality of life (as measured by the Spitzer Quality of Life Index), percent change in weight, and percent change in LBM based on body plethysmography and skin-fold measurement techniques.
The study was designed to ensure that among the subset of patients receiving concurrent chemotherapy there would be 80% statistical power to detect a 4% improvement in LBM in the HMB/Arg/Gln arm at the two-sided 5% significance level. Thirty percent of patients were expected to receive concurrent chemotherapy. Power to detect the difference in all patients would be greater than 99%.
Because of the brevity of the study, an interim analysis was not conducted. All analyses were completed as specified in the protocol. Data normality assumptions were not met requiring the use of non-parametric methods. The Wilcoxon rank sum test was used to test the null hypothesis of no difference in the percent change in LBM between the HMB/Arg/Gln and placebo treatment arms. Estimates of the median difference between the two arms were calculated using the Hodges–Lehmann estimate and non-parametric 95% confidence intervals were determined using the Moses criterion. Also tested were changes in weight, fatigue, and quality of life. Patients not completing the 8-week assessment were treated as missing data. Additionally, area under the curve (AUC) analysis was utilized for each endpoint to assess overall body composition and overall quality of life. AUC incorporates patient outcomes at the 4-week assessment and does not solely rely on change values.
Results
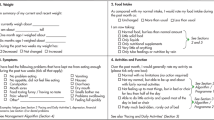
From December 2002 to October 2004, 472 patients were randomized into the trial at a rate of 21.3 patients per month. Patients were followed up for 8 weeks, the duration of the study. Patients were enrolled from 23 RTOG full member and 15 CCOP member institutions. Twenty-six patients did not meet the eligibility inclusion criteria or withdrew their consent for participation in the study (Fig. 1). Patient demographics and stratification variables were well balanced between the placebo and HMB/Arg/Gln arms (Tables 1 and 2) as expected because of randomization of the patient population. Patients receiving concurrent chemotherapy were of particular interest. Fifty-three percent of the eligible patients received concurrent therapy, 123 (54%) on the placebo arm, and 115 (52%) on the HMB/Arg/Gln arm. In the HMB/Arg/Gln arm, 22% and 1% of the patients experienced grades 1–2 or 3–4 gastrointestinal toxicity. In the placebo arm, 23% and 3% of the patients experienced grades 1–2 and 3–4 gastrointestinal toxicity. Gastrointestinal toxicity included nausea, vomiting, diarrhea, and constipation. There were no other significant levels of toxicity in either arm.
There was a high rate of patient non-compliance in the study. Only 77 (34%) patients on the placebo arm and 88 (40%) patients on the HMB/Arg/Gln arm completed the treatment as designed per protocol. The reasons for non-compliance are shown in Table 3. The majority of patients did not complete treatment because of patient preference. Since the analysis plan was based on intention-to-treat, failure to complete protocol treatment was not a valid reason for exclusion from analysis. However, patients missing the baseline or 8-week LBM assessment were excluded from analysis, rather than attempting imputation of the missing data. Because of the nature of cooperative clinical trials, consistently assessing patients during the eighth week of treatment proved difficult. Only 47 (21%) patients on the placebo arm and 37 (17%) patients on the HMB/Arg/Gln arm completed the 8-week follow-up assessment during the eighth week as scheduled. Patients who were assessed during the 7th, 8th, 9th, or 10th week of treatment completion were then included to have suitable numbers for analysis (Table 4). After including these patients, there were 91 (41%) patients on the placebo arm and 106 (48%) patients on the HMB/Arg/Gln arm that completed both the baseline and 8-week follow-up assessments of LBM necessary for inclusion in analysis (Table 5).
Although the number of analyzable patients (197) was less than the target sample size, loss of power was not an issue for the entire group analysis. The target sample size was set high to ensure that an adequate number of patients would receive concurrent chemotherapy. Since the study design and sample size were based on the subset of patients receiving concurrent chemotherapy, there was still 94% statistical power to detect a difference between the two treatment arms in all patients. Within the subset of 100 patients receiving concurrent chemotherapy, however, the analysis was slightly underpowered at 70%. After patients with missing baseline or 8-week assessments were excluded, 50 (55%) patients on the placebo arm, and 50 (47%) patients on the HMB/Arg/Gln arm received concurrent chemotherapy.
Table 2 illustrates the differences in pretreatment characteristics between patients excluded and included in analysis. Patients included in the analysis were more likely to have completed protocol treatment [p < 0.0001]. Within each treatment completion group, however, the prognostic factors did not differ between patients included and excluded from analysis. Therefore, the data can be assumed to be missing at random and excluding patients with missing data (complete case analysis) may lead to biased results (Fig. 2). Multiple imputation methods were not used since many of the patients missing the 8-week assessment also missed the 4-week assessment (Table 3). Although patients included may represent a biased subset all eligible cases, degree of weight loss prior to study entry, baseline weight, baseline LBM, and all other stratification and pretreatment variables did not significantly differ between patients excluded and included from analysis.
There was no statistically significant difference between the placebo and HMB/Arg/Gln arms in any of the primary or secondary endpoints (Table 6). The median difference in percent change in LBM as measured by bioimpedance between the two arms was 0.96 [(−0.75, 2.64); p = 0.24]. The median difference in percent change in LBM between the two arms as determined by skin-fold measurements was 0.09 [(−1.51, 1.65); p = 0.91]. There were only six cases that had LBM determined by body plethysmography. The median difference in percent change in weight between the two arms was −0.19 [(−1.58, 1.17); p = 0.78]. The median difference in change in fatigue was 0 [(−1, 2); p = 0.56]. The median difference in change in quality of life was 0 [(−1, 0); p = 0.44]. Among the subset of patients receiving concurrent chemotherapy, there was also no significant difference in the median change values for the primary or secondary endpoints. There were also no differences in outcome within the primary site (lung versus others), presence of metastases, gender, or race subgroups. Among patients with a 2% to 5% weight loss, there was a median treatment difference of 2.26% change in lean body mass favoring the active arm (p = 0.01). Among the patients with a 5% to 10% weight, the difference was 0.02 (p = 0.38).
Based on the results of the AUC analysis, patients receiving HMB/Arg/Gln had a strong trend towards a higher LBM throughout the study as measured by both bioimpedance (p = 0.08) and skin-fold measurements (p = 0.08). There was also a greater effect among patients with a smaller initial weight loss (less than 5%).
Discussion
This trial failed to show that the HMB/Arg/Gln mixture, as formulated in this study, resulted in a significant change in lean body mass among cancer patients with weight loss at the primary endpoint of lean body mass at 8 weeks (extended to the range of 7–10 weeks to allow sufficient data for analysis).
This trial had several problems. Only 37% of patients completed the trial per protocol design. The majority (45%) of these patients refused to complete the study or cited side effects as a reason for non-compliance. The high amino acid mixtures may have caused excessive gastrointestinal toxicities (nausea, constipation, and/or diarrhea). In a previous, three-institution study of HMB/Arg/Gln, 25 patients were randomized to the control group, and 24 were randomized to the HMB/Arg/Gln group. Seventeen patients (35%) withdrew from the study prior to their first 4-week follow-up visit (11 control; 6 HMB/Arg/Gln). Only 44% of patients completed the 8 week assessment of body composition. The reasons for the low compliance are not given. Despite the large number of patients missing assessments, there was sufficient power to detect a difference (11).
Bioimpedance was chosen to measure lean body mass because it was the most efficient method to use within a multi-institutional trial with limited funding resources. Body plethysmography is the “gold standard” measurement, but has very limited availability. No multi-institutional trial of skin-fold measurements had been done prior to this trial to validate its use as a primary endpoint. DEXA scans are also a reliable method, but would require that each institution arranges for these to be done, raising both financial and quality assurance problems [21]. The supplier of the HMB/Arg/Gln donated bioimpedance units to the Radiation Therapy Oncology Group for use during the trial. Centralized training was done, and all centers used the same algorithms to measure lean body mass. Both the raw data and the final data were transmitted to the Radiation Therapy Oncology Group, increasing the quality assurance of the measurements. Further, as an inducement to enroll patients, the participating centers were able to keep the units afterwards. Randomized studies have shown good agreement between DEXA scans and bioimpedance measurements [22, 23]. Thus, after consultation with the National Cancer Institute, it was decided to use the bioimpedance measurements as the primary endpoint.
The trial design hypothesized that the majority of patients would have lung, breast, or prostate cancer. The stratification by lung versus others was used as a surrogate for the type of chemotherapy they would receive, which at that time was primarily cisplatin for lung cancer and less emetogenic chemotherapy for breast cancer. It was statistically untenable to attempt to stratify by every type of chemotherapy and the manner it was given. There was no difference in outcomes between the two arms when analyzed by whether chemotherapy was given or not, or by the type of cancer (lung or others).
This trial, as do many trials studying patients with advanced cancer, had difficulties with patient compliance. There was a high percentage of missing data or delayed data. To minimize the effect of missing data, it was decided post hoc to allow to the final body mass index to be collected during a range of 7 to 10 weeks, rather than at exactly 8 weeks. This was done on the assumption that any clinically significant effect of the intervention would still be present in this time frame. Although the decision increased the risk of losing statistical significance because of muscle mass loss in the 8- to 10-week period, the lack of even a trend for improvement in the intervention arm at the “8” weeks suggests that this was not a factor. Among the patients in this time range (7–10 weeks), 84% of the patients were measured in weeks 8 or 9. Although it could be argued that there could have been a drastic weight loss over weeks 9 and 10, the lack of such a drastic weight loss in the control arm argues against this concern. Among the secondary analyses, there was a strong trend towards improved lean body mass when measured using the area under the curve (AUC) with a 0.08 p value.
This study also suggests that weight loss was not an ideal surrogate marker for cancer cachexia. Patients on both arms continued to lose weight during the trial. Patients on the placebo arm increased their LBM. The increase in LBM among the placebo patients reinforces that weight loss among cancer patients is multi-factorial and does not necessarily represent lean body mass loss secondary to cancer cachexia. Weight loss alone should not be used as a surrogate marker for the presence of cancer cachexia. Future cachexia trials will need to clearly identify the definition of cachexia being used, and use the appropriate measurements or biomarkers for that definition [24].
Conclusions
This trial was unable to show that a HMB/Arg/Gln mixture prevented lean body mass loss among cancer patients. Factors associated with this failure include the inability of patients to complete an 8-week course of treatment and return for follow-up assessment, because the patients may not have been suffering from cancer cachexia, and poor tolerance of the treatment mixtures. This study alone did not definitively determine the activity of this mixture. Future trials of this compound, and other cancer cachexia treatments, will need to prove the presence of cachexia prior to initiation of treatment. Also, for the HMB/Arg/Gln compound to be widely used, higher patient tolerance will be needed. The trend for improved lean body mass as measured using AUC suggests that further testing is warranted using stricter entry criteria. There may also be a benefit to restricting the studies to patients with a smaller amount of weight loss. Finally, efforts should be made to increase patient acceptance of the mixture.
References
Laviano A, Meguid MM, Inui A, Muscaritoli M, Rossi-Fanelli F (2005) Therapy insight: cancer anorexia-cachexia syndrome—when all you can eat is yourself. Nat Clin Pract Oncol 2:158–165
Esper DH, Harb WA (2005) The cancer cachexia syndrome: a review of metabolic and clinical manifestations. Nutr Clin Pract 20:369–376
Roubenoff R (1999) The pathophysiology of wasting in the elderly. J Nutr 129:256S–259S
Pascual Lopez A, Roque iFM, Urrutia Cuchi G et al (2004) Systematic review of megestrol acetate in the treatment of anorexia-cachexia syndrome. J Pain Symptom Manage 27:360–369
Goldberg RM, Loprinzi CL, Mailliard JA et al (1995) Pentoxifylline for treatment of cancer anorexia and cachexia? A randomized, double-blind, placebo-controlled trial. J Clin Oncol 13:2856–2859
Gordon JN, Trebble TM, Ellis RD, Duncan HD, Johns T, Goggin PM (2005) Thalidomide in the treatment of cancer cachexia: a randomised placebo controlled trial. Gut 54:540–545
Laviano A, Muscaritoli M, Rossi-Fanelli F (2005) Phase II study of high-dose fish oil capsules for patients with cancer-related cachexia: a cancer and leukemia group B study. Cancer 103:651–652
Fearon KC, Barber MD, Moses AG et al (2006) Double-blind, placebo-controlled, randomized study of eicosapentaenoic acid diester in patients with cancer cachexia. J Clin Oncol 24:3401–3407
Cannabis-In-Cachexia-Study-GroupStrasser F, Luftner D et al (2006) Comparison of orally administered cannabis extract and delta-9-tetrahydrocannabinol in treating patients with cancer-related anorexia-cachexia syndrome: a multicenter, phase III, randomized, double-blind, placebo-controlled clinical trial from the cannabis-in-cachexia-study-group. J Clin Oncol 24:3394–3400
Lundholm K, Korner U, Gunnebo L et al (2007) Insulin treatment in cancer cachexia: effects on survival, metabolism, and physical functioning. Clin Cancer Res 13:2699–2706
Jatoi A, Dakhil SR, Nguyen PL et al (2007) A placebo-controlled double blind trial of etanercept for the cancer anorexia/weight loss syndrome: results from N00C1 from the north central cancer treatment group. Cancer 110:1396–1403
May PE, Barber A, D’Olimpio JT, Hourihane A, Abumrad NN (2002) Reversal of cancer-related wasting using oral supplementation with a combination of beta-hydroxy-beta-methylbutyrate, arginine, and glutamine. Am J Surg 183:471–479
Morley JE, Thomas DR, Wilson MM (2006) Cachexia: pathophysiology and clinical relevance. Am J Clin Nutr 83:735–743
Lelbach A, Muzes G, Feher J (2007) Current perspectives of catabolic mediators of cancer cachexia. Med Sci Monit 13:168–173
Curran JN, Winter DC, Bouchier-Hayes D (2006) Biological fate and clinical implications of arginine metabolism in tissue healing. Wound Repair Regen 14:376–386
Kuhls DA, Rathmacher JA, Musngi MD et al (2007) Beta-hydroxy-beta-methylbutyrate supplementation in critically ill trauma patients. J Trauma 62:125–131
Smith HJ, Wyke SM, Tisdale MJ (2004) Mechanism of the attenuation of proteolysis-inducing factor stimulated protein degradation in muscle by beta-hydroxy-beta-methylbutyrate. Cancer Res 64:8731–8735
Sun SS, Chumlea WC, Heymsfield SB et al (2003) Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am J Clin Nutr 77:331–340
Zelen M (1974) The randomization and stratification of patients to clinical trials. J Chronic Dis 27:365–375
Clark RH, Feleke G, Din M et al (2000) Nutritional treatment for acquired immunodeficiency virus-associated wasting using beta-hydroxy beta-methylbutyrate, glutamine, and arginine: a randomized, double-blind, placebo-controlled study. JPEN J Parenter Enteral Nutr 24:133–139
Smith DE, Hudson J, Martin A et al (2003) Centralized assessment of dual-energy X-ray absorptiometry (DEXA) in multicenter studies of HIV-associated lipodystrophy. HIV Clin Trials 4:45–49
Bolanowski M, Nilsson BE (2001) Assessment of human body composition using dual-energy X-ray absorptiometry and bioelectrical impedance analysis. Med Sci Monit 7:1029–1033
Smith MR, Fuchs V, Anderson EJ, Fallon MA, Manola J (2002) Measurement of body fat by dual-energy X-ray absorptiometry and bioimpedance analysis in men with prostate cancer. Nutrition 18:574–577
Jatoi A, Egner J, Loprinzi CL et al (2004) Investigating the utility of serum cytokine measurements in a multi-institutional cancer anorexia/weight loss trial. Support Care Cancer 12(9):640–644
Wood LJ, Nail LM, Gilster A, Winters KA, Elsea CR (2006) Cancer chemotherapy-related symptoms: evidence to suggest a role for proinflammatory cytokines. Oncol Nurs Forum 33(3):535–542
Fearon KC, Voss AC, Hustead DS (2006) Definition of cancer cachexia: effect of weight loss, reduced food intake, and systemic inflammation on functional status and prognosis. Am J Clin Nutr 83(6):1345–1350
Smith HJ, Mukerji P, Tisdale MJ (2005) Attenuation of proteasome-induced proteolysis in skeletal muscle by {beta}-hydroxy-{beta}-methylbutyrate in cancer-induced muscle loss. Cancer Res 65(1):277–283
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berk, L., James, J., Schwartz, A. et al. A randomized, double-blind, placebo-controlled trial of a β-hydroxyl β-methyl butyrate, glutamine, and arginine mixture for the treatment of cancer cachexia (RTOG 0122). Support Care Cancer 16, 1179–1188 (2008). https://doi.org/10.1007/s00520-008-0403-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-008-0403-7