Abstract
This paper uses an evidence-based approach whenever possible to formulate recommendations, emphasizing the results of controlled trials concerning the best use of antiemetic agents. We address issues of dose, schedule, and route of administration of five selective 5-HT3 antagonists. We conclude that for each of these five drugs, there is a plateau in therapeutic efficacy above which further dose escalation does not improve outcome. Furthermore, for all classes of antiemetic agents, a single dose is as effective as multiple doses or a continuous infusion. The oral route is as efficacious as the intravenous route of administration, even with chemotherapy of high emetic risk. Selective antagonists of the type 3 serotonin receptor (5-HT3) in combination with dexamethasone and aprepitant are the standard of care for the prevention of emesis following chemotherapy of high emetic risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of selective antagonists to the serotonin (5-hydroxytryptamine, 5-HT3) type 3 receptor changed the therapy of chemotherapy-induced emesis [24, 32, 64]. These agents, in combination with dexamethasone and now aprepitant, have become the standard of care to prevent acute and delayed emesis following chemotherapy of high emetic risk. Although ondansetron, granisetron, tropisetron, dolasetron, and palonosetron differ in receptor specificity, potency, and plasma half-life [2, 63], each has demonstrated equivalent efficacy and adverse effects when used to prevent emesis following chemotherapy of high emetic risk. Despite these successes and widespread acceptance of these agents, a number of controversies persist regarding the best way to use these agents in practice.
Acute emesis and nausea with chemotherapy of high emetic risk
This discussion will review issues of dose, schedule, and route of administration of the five selective 5-HT3 antagonists in the prevention of acute emesis caused by chemotherapy of high emetic risk. Double-blind randomized trials offer the most valid evidence whereas uncontrolled clinical trials, observational studies, and retrospective analyses each provide weaker evidence. This approach is consistent with recent recommendations regarding evidence-based medicine [16]. The “No Emesis” rate during the initial 24-h observation period (acute emesis) was selected as an appropriate therapeutic endpoint reported in most trials under consideration. We address issues of dose, schedule, and route of administration for dexamethasone and aprepitant as well, and make recommendations for use of these agents in practice.
Dose of 5-HT3 antagonists
The panel concluded that despite preclinical differences, the 5-HT3 antagonists are characterized clinically by a threshold effect for response, a modest dose-response curve, and a plateau in therapeutic efficacy extending over a several-fold range in dose. The therapeutic implications of these conclusions are that a higher dose or longer exposure is not necessarily better and that breakthrough emesis following the administration of a 5-HT3 antagonist is more likely mediated by another mechanism rather than inadequate 5-HT3 receptor blockade [30, 77].
For ondansetron and granisetron, there is wide variability in the “approved” single doses for the prevention of acute emesis following chemotherapy of high emetic risk. In the United States, the approved dose of ondansetron (32 mg or approximately 0.45 mg/kg) is fourfold that in Europe (8 mg) while for granisetron, exactly the opposite is true (0.01 mg/kg versus 3 mg or 0.04 mg/kg).
In view of the above considerations, analysis of the literature regarding dose was performed for five 5-HT3 antagonists in widest use. Both dose-response studies of individual agents and comparative trials between agents were considered. Study designs that incorporate issues of schedule are addressed in the next section.
Cisplatin serves as a paradigm for chemotherapy of high emetic risk. Moreover, cisplatin causes severe emesis in all patients who receive it at all doses in clinical use. For these reasons, cisplatin has become the standard emetic stimulus in clinical trials of antiemetic agents. Further, it is widely held that an agent that lessens or prevents emesis following cisplatin will be effective with other chemotherapeutic agents of similar or lesser emetic potential. Randomized studies have demonstrated the effectiveness of 5-HT3 antagonists for the prevention of acute emesis following cisplatin [7, 13, 28, 50, 76]. Furthermore, the addition of dexamethasone has consistently improved efficacy compared to a 5-HT3 antagonist alone, establishing this combination as a standard for patients receiving cisplatin-based therapy [35, 66]. Dose-ranging studies of these agents generally demonstrate evidence of a dose-response curve consistent with the hypothesis discussed earlier [26, 27, 41, 45, 55, 66, 75, 78, 80]. There are conflicting data regarding the optimal single dose of ondansetron for prevention of acute emesis from cisplatin. While a study published by Beck et al. led to the conclusion that a 32 mg dose was superior to 8 mg, particularly in patients receiving high-dose cisplatin (>100 mg/m2), a similarly designed study by Seynaeve showed that the 8 mg dose was equally effective [3, 72]. In both studies, single-dose administration was equivalent to other tested dose schedules. Further evidence in support of a single 8 mg ondansetron dose comes from the studies of the Italian Group for Antiemetic Research (IGAR) and from Ruff, an 8 mg dose showing equal efficacy to either a 32 mg dose level, or 3 mg of granisetron, respectively [37, 71].
For granisetron, the evidence from both dose-response studies of this agent and comparative trials against ondansetron supports a recommended dosing level of 0.01 mg/kg (commonly given as a 1 mg fixed dose) [54, 55, 66, 76]. The dose-ranging studies of Navari and Riviere suggest that dose levels of 0.002 or 0.005 mg/kg are suboptimal while there is a relative plateau above 0.01 mg/kg, with slightly higher but clinically insignificant no-emesis rates, at 0.04 mg/kg [55, 66]. The comparative trial by Navari adds further support in favor of the 0.01 mg/kg dose, with identical no-emesis rates for 0.01 mg/kg versus 0.04 mg/kg in comparison to an approved and effective multiple-dose schedule of ondansetron (0.15 mg/kg×3) [54].
The dose-ranging study of Van Belle and the comparative trial by Marty both support a 5 mg single-dose administration of tropisetron as effective in highly emetogenic cisplatin-based chemotherapy, with the study of Van Belle suggesting no further improvement in efficacy at dose levels up to 40 mg [49, 80].
Initial dose-ranging studies of dolasetron did not clearly define the lowest effective dose while the subsequent comparative trial of Hesketh supports a dose level of 1.8 mg/kg as effective, with no evidence of clinically significant improvement in efficacy at 2.4 mg/kg [31, 45, 78].
A dose-ranging study of palonosetron in patients receiving chemotherapy of high emetic risk (97% received cisplatin) tested intravenous doses from 0.0003 to 0.09 mg/kg and identified 0.003 and 0.0.01 mg/kg as the lowest effective palonosetron doses [15]. Three subsequent randomized trials compared a 0.25 mg fixed palonosetron dose, a 0.75 mg fixed palonosetron dose, and a standard comparator of either intravenous ondansetron 32 mg [1, 20] or intravenous dolasetron 100 mg [14]. The three studies confirmed the effectiveness and safety of palonosetron and showed no incremental benefit by increasing the single intravenous dose from 0.25 to 0.75 mg. A single intravenous dose of 0.25 mg of palonosetron is preferred and at present is the dose approved by regulatory authorities for the treatment of individuals receiving chemotherapy of high emetic risk. No oral formulation of palonosetron is available for clinical use.
Dose of dexamethasone
A range of doses of dexamethasone, given either alone or in combination with a 5-HT3 antagonist or metoclopramide, have been tested as antiemetics. Many of these studies utilized a single 20 mg dose. The IGAR has reported a comparison study of dexamethasone dosages ranging from 4 mg to 20 mg in patients receiving cisplatin [39]. They recommended a single 20 mg dose before chemotherapy based on their observations that the 20 mg dose had the highest numerical efficacy and there was no difference in adverse effects among the doses tested [39].
The concomitant use of aprepitant, however, has necessitated a change in the recommended dose of dexamethasone in clinical trials. The initial studies, which demonstrated improved antiemetic effects using aprepitant in combination with 5-HT3 antagonists and dexamethasone, administered dexamethasone at a 20 mg oral dose without difficulty [6, 9, 57]. A pharmacokinetic study in healthy subjects found that aprepitant increased dexamethasone levels approximately twofold [4]. Because the differential exposure to dexamethasone could “theoretically confound the interpretation of the efficacy of aprepitant, a 50% reduction of the oral dexamethasone dose was made” in the aprepitant arms of the randomized trials comparing a three-drug aprepitant regimen to the standard dexamethasone plus the ondansetron regimen [34, 65]. A 12 mg oral dose was given before cisplatin in the aprepitant arms in these studies. Although other dexamethasone doses may be appropriate, the 12 mg oral dose tested in two phase III studies [34, 65] is recommended.
Dose of aprepitant
Aprepitant is the first of a new class of drugs that potently and selectively block the neurokinin-1 (NK1) neurotransmitter receptor, the binding site of the regulatory peptide substance P. For the prevention of acute emesis following cisplatin, a randomized study evaluated oral prechemotherapy doses of aprepitant from 40 to 375 mg and concluded that a single 125 mg oral dose had “the most favorable benefit:risk profile” [6]. This 125 mg dose was used in the randomized phase III comparison studies of aprepitant, and it is the only dose that has been approved by regulatory authorities. Although other aprepitant doses may be appropriate, the 125 mg oral aprepitant dose tested in two phase III studies [34, 65] is recommended.
Schedule of administration of 5-HT3 antagonist antiemetics
If given at an effective dose, a single dose provides adequate 5-HT3 blockade for prevention of acute emesis. Clinical implications of this fact are that the administration of multiple doses is unnecessary and that breakthrough emesis during the acute phase may be related to other mediators/receptors. Multiple doses will only provide a better therapeutic outcome if the initial dose is suboptimal or if optimal therapeutic efficacy was dependent on either the plasma half-life or duration of receptor blockade during the acute phase.
Substantial evidence supports these conclusions, particularly with ondansetron, the first 5-HT3 antagonist developed. Early clinical trials of intravenous ondansetron with cisplatin explored a variety of schedule-related issues, including variable dosing intervals, number of doses, and schedules incorporating continuous infusion [35, 42]. In general, these studies demonstrated that shortening the dosing interval or increasing the number of doses did not improve efficacy. A continuous-infusion schedule following an 8 mg intravenous bolus was also found to be effective [50]. However, as demonstrated in the subsequent studies of Beck and Seynaeve, multiple-dose administration did not improve outcomes [3, 72]. Based on these observations, development of the other 5-HT3 antagonists quickly evolved into determining optimal levels for intravenous single-dose administration. The recommended single doses of five 5-HT3 antagonists are presented in Table 1.
Route of administration
Clinical outcomes with oral administration of 5-HT3 antagonists and dexamethasone are equivalent to intravenous administration. Since oral administration is generally simpler and less resource intensive, this route is preferable if the gastrointestinal tract is intact and compliance assured.
As a class, 5-HT3 antagonists exhibit good bioavailability when administered by the oral route, and the effectiveness of oral agents is equivalent to intravenous formulations. We recommend the administration of selective 5-HT3 antagonists by the oral route whenever appropriate. In all phase III studies comparing oral 5-HT3 antagonists with intravenous formulations of antiemetics to treat cisplatin-induced emesis, control rates are comparable [21, 29]. No oral formulation of palonosetron is available for clinical use.
Delayed emesis and nausea with chemotherapy of high emetic risk
Introduction
Nausea and vomiting developing more than 24 h after chemotherapy administration is termed delayed emesis. The syndrome was first described in patients receiving a high dose (120 mg/m2) of cisplatin [43]. Seventy-four percent of patients developed delayed vomiting in the 96-h period between days 2–5 after chemotherapy. Delayed emesis can occur following the administration of a number of chemotherapy agents with moderate to high emetogenicity. In general, delayed emesis has been less extensively studied than acute emesis. This may relate to the generally lower severity of delayed emesis compared to acute emesis and the lower degree of awareness among caregivers about this entity.
Among agents of high emetic risk, cisplatin has been the most extensively studied with respect to its potential to induce delayed nausea and vomiting and as a focus of therapeutic approaches. A number of predictive factors have been identified for the development of delayed emesis. By far the most important is the presence or absence of acute nausea and vomiting. Approximately twice as many patients experiencing emesis during the first 24h after cisplatin will develop delayed emesis as compared to patients with no acute emesis [36, 48, 67]. Other factors with prognostic importance include protection against nausea and vomiting in prior chemotherapy cycles, cisplatin dose, gender, and age [68]. Information on the potential for delayed emesis with other highly emetogenic agents, such as mechlorethamine, streptozotocin, dacarbazine and the nitrosoureas, remains largely anecdotal with a paucity of objective data.
The current 24-h cutoff for defining the beginning of delayed emesis is admittedly somewhat arbitrary. It does reflect, however, the biphasic pattern of emesis following cisplatin [22, 68]. When given placebo antiemetics or metoclopramide, an initial intense period of emesis is noted from 2 to 12 h after cisplatin. After a quiescent period, a distinct second peak is noted beginning approximately 18 h after chemotherapy. Delayed emesis after cisplatin peaks during the 24-h period from 48 to 72 h after chemotherapy and then progressively declines in frequency over the ensuing 2 days [43]. Accordingly, the time period of greatest risk for delayed emesis after cisplatin is, at minimum, hours 24–96. The majority of clinical trials assessing therapeutic approaches for delayed emesis after cisplatin have used a 24- to 120-h study period.
Pathophysiology
The physiologic mechanisms underlying delayed emesis remain poorly understood although evidence suggests distinct differences from the mechanisms of acute nausea and vomiting. Only in recent years have a number of experimental models been developed for study of delayed emesis. These include models using ferrets and piglets [52, 70]. Experimental results with these models parallel to some extent the clinical experience with at least two classes of antiemetics—the selective type 3 serotonin receptor (5-HT3) antagonists and the selective neurokinin-1 (NK1) receptor antagonists. The 5-HT3 antagonists have demonstrated their greatest efficacy both in the clinic and in experimental models with acute emesis. When used as single agents, the 5-HT3 antagonists are particularly effective during the first 12–14 h following cisplatin, with efficacy falling off thereafter. This observation has led to speculation that the true onset of delayed emesis is during this period of 12–16 h following cisplatin [59].
On the other hand, the newly introduced selective NK1 antagonist aprepitant is significantly more effective in both model systems and in practice for controlling delayed emesis after cisplatin compared to the 5-HT3 antagonists. A recent analysis of the time course of emesis following the use of 5-HT3 antagonists and NK1 antagonists also supports the hypothesis that these two classes of agents have their primary activity in distinct phases of the emetic cycle, with 5-HT3 antagonists very effective in the first 16 h and the NK1 antagonists exerting their greatest activity from hour 16 and later [34].
Antiemetic agents
Clinical trials attempting to prevent delayed nausea and vomiting have focused almost exclusively on patients receiving cisplatin. Therefore, the trials reviewed in this manuscript will share a common theme of cisplatin-based chemotherapy and will be limited to randomized studies. In addition, with some exceptions, emphasis will be placed on trials where acute antiemetic treatment was uniform across treatment arms. Many trials were not specifically designed to test treatments for delayed emesis. Because the control of acute emesis varied, and it is well established that vomiting during the initial 24 h after chemotherapy is one of the strongest factors predicting delayed emesis, the usefulness of these data for interpreting the control of delayed emesis is inherently limited.
Single agents
-
a.
Corticosteroids/metoclopramide: Corticosteroids have historically been the most commonly used single agent and are felt to have the most utility in the prevention of delayed emesis. Dexamethasone has been the corticosteroid most commonly employed. Its superiority to placebo was clearly demonstrated in patients receiving cisplatin 120 mg/m2 where 35% of patients receiving dexamethasone 8 mg twice daily for 2 days then 4 mg twice daily for 2 days had no delayed emesis as compared to 11% of patients receiving placebo [46]. In another trial, patients receiving cisplatin >50 mg/m2 were randomized to receive either dexamethasone 1 mg four times a day, metoclopramide 20 mg four times a day, or placebo starting 24 h after cisplatin, with treatment extending for 7 days [69]. A nonsignificant trend favored both active treatments over placebo with complete protection from vomiting in 56.7%, 65.4%, and 69% of patients receiving placebo, dexamethasone, and metoclopramide, respectively. Dexamethasone and metoclopramide were both significantly superior to placebo in the control of nausea.
-
b.
Adrenocorticotropic hormone (ACTH): Additional indirect support for the value of corticosteroids in delayed emesis comes from two trials evaluating adrenocorticotropic hormone (ACTH). In the first trial, patients receiving cisplatin >60 mg/m2 were randomized to receive 24 h after cisplatin either 1 mg of ACTH or placebo [61]. No-delayed-vomiting rates were 67% and 43% in the ACTH and placebo arms respectively (p=0.11). A subsequent trial also conducted in patients receiving cisplatin >60 mg/m2 randomized patients to receive either ACTH 1 mg or ACTH 2 mg 24 h after cisplatin plus an additional 1 mg on day 4 or placebo [62]. Significantly less delayed vomiting was noted in both ACTH arms.
-
c.
5-HT3 antagonists: Four randomized trials comparing a 5-HT3 antagonist to placebo for the prevention of delayed emesis after cisplatin have been reported [17, 56, 60, 74]. Prophylaxis for the prevention of acute emesis was uniform in each trial across the study arms. Fifty patients having two or fewer emetic episodes during the first 24 h after cisplatin were randomized to receive ondansetron 16 mg three times a day or placebo for 4 days [17]. Complete control of delayed emesis was noted in 40% and 33% of patients on the ondansetron and placebo arms respectively (p=0.648). In a much larger study, 533 patients receiving cisplatin (>75 mg/m2) were given granisetron 0.04 mg/kg on day 1 for acute prophylaxis [74].They were then randomized to receive either placebo or one of three doses of oral granisetron (2.5, 5, or 10 mg) twice a day beginning 6 h after cisplatin and continuing through day 7. No significant differences were noted in the frequency of delayed emesis between the arms. Another trial comparing ondansetron to placebo for prevention of delayed emesis found that patients receiving ondansetron experienced significantly fewer emetic episodes on days 2/3, 4, and 5 compared to placebo after cisplatin [56]. Complete response rates during the primary study period of day 2/3 were not significantly different. The fourth trial randomized patients to receive one of two schedules of ondansetron alone, ondansetron combined with dexamethasone, or placebo during days 2–6 after cisplatin-based chemotherapy [60]. No significant differences were noted between the ondansetron alone and placebo arms. The weight of evidence from these trials strongly suggests that 5-HT3 antagonists have minimal to modest activity in the prevention of cisplatin-induced delayed emesis.
-
d.
NK1 antagonists: Preclinical trials of selective NK1 antagonists strongly suggested possible activity for these agents in cisplatin-induced delayed emesis. Subsequent clinical trials have validated the utility of these agents in this setting. In a small trial of 53 patients receiving cisplatin >50 mg/m2, patients were randomized to receive a single intravenous dose of ondansetron 32 mg or 60 or 100 mg of the NK1 antagonist L-758,298 prior to cisplatin [8, 58]. They were followed up to 7 days following cisplatin with no additional antiemetics planned. During days 2–7, the proportion of patients without emesis was 72% and 30% in the L-758,298 and ondansetron groups, respectively (p=0.005). Of note, this superior outcome in the delayed phase with L-758,298 occurred despite patients experiencing slightly worse control of emesis in the first 24 h compared to ondansetron. L-758,298 is the intravenous prodrug of the orally active NK1 antagonist MK-869 (aprepitant). Three subsequent trials evaluating MK-869 with cisplatin-induced emesis all found significantly better control of delayed emesis with MK-869 compared to placebo [5, 58, 81]. Two of these studies [5, 81] included arms in which patients received only MK-869 combined with dexamethasone for acute emesis prophylaxis. Despite patients experiencing poorer control of acute emesis on these arms compared to arms employing a 5-HT3 antagonist for acute emesis prevention, control of delayed emesis was consistently improved on the MK-869 arms. A small phase II randomized trial evaluating a different NK1 antagonist (CJ-11,974) noted similar findings [33]. Sixty-one patients receiving cisplatin >100 mg/m2 were randomized to receive either 100 mg of CJ-11,974 twice a day or placebo during days 2–5 after cisplatin. Control of delayed emesis was significantly better with CJ-11,974 compared to placebo, with complete response rates of 67.8% and 36.6%, respectively.
Combination of agents
-
a.
Dexamethasone and metoclopramide: Prior guideline panels consistently have recommended the combination of dexamethasone and metoclopramide as the antiemetic regimen of choice for the prevention of cisplatin-induced delayed emesis. This recommendation is based almost entirely on the previously discussed trial [44] in which patients receiving cisplatin 120 mg/m2 were randomized to receive placebo, dexamethasone 8 mg twice a day for 2 days, then 4 mg twice a day for 2 days alone or combined with metoclopramide 0.5 mg/kg four times a day for 4 days. Delayed vomiting was prevented in 52% on the combination regimen versus 35% with dexamethasone alone (p=0.006). Another small trial in 63 patients compared dexamethasone alone or combined with metoclopramide or alizapride for the prevention of delayed emesis in patients receiving cisplatin >60 mg/m2 [53]. Complete protection from delayed vomiting was higher with the combination of dexamethasone-metoclopramide compared to dexamethasone alone (70% versus 44%, respectively). However, due to the different acute antiemetic treatments employed, acute complete protection rates varied markedly across the arms (65%, 25%, 35% in the metoclopramide-, alizapride-, and dexamethasone-only arms, respectively), making interpretation of the delayed period results problematic. Another small trial with 42 patients showed a nonsignificant trend favoring a combination of dexamethasone and metoclopramide compared to placebo in preventing delayed emesis on days 2–7 after cisplatin >80 mg/m2 [73]. In a trial including 322 patients receiving cisplatin >50 mg/m2, the relative activity of the dexamethasone/metoclopramide combination was compared to dexamethasone combined with ondansetron for the prevention of delayed emesis [38]. The regimens were found to have comparable efficacy. The results of this trial have been often cited to support the recommendation to consider a 5-HT3 antagonist and dexamethasone as an effective regimen and an acceptable alternative to dexamethasone and metoclopramide for the prevention of cisplatin-induced delayed emesis. This conclusion can be questioned given the results of a number of subsequent trials (see below).
-
b.
Dexamethasone and prochlorperazine: Dexamethasone has also been combined with prochlorperazine for delayed emesis prophylaxis. In a trial of 70 patients receiving cisplatin >80 mg/m2, patients were randomized to receive dexamethasone 20 mg on days 2 and 3 and prochlorperazine 5 mg 3 times a day on days 1–5 compared to placebo alone in the delayed period [51]. Complete protection from delayed emesis was obtained in 20% and 28.6% of patients in the placebo and active treatment arms, respectively.
-
c.
Dexamethasone and 5-HT3 antagonist: A number of trials have evaluated the combination of dexamethasone and a 5-HT3 antagonist compared to either agent alone. Two studies have compared 5-HT3 antagonist monotherapy to a combination with dexamethasone [23, 40]. Both studies noted superiority for the combination compared to either granisetron [40] or ondansetron [23]. Four additional trials have attempted to evaluate the relative contribution of the 5-HT3 antagonist in a 5-HT3 antagonist/dexamethasone combination to dexamethasone alone [19, 47, 60, 79]. In a previously discussed trial [60], 640 patients receiving cisplatin >70 mg/m2 were randomized to one of four arms: placebo on days 2–6; ondansetron 8 mg twice a day on days 2/3 followed by placebo; ondansetron 8 mg twice a day on days 2–6; ondansetron 8 mg twice a day and dexamethasone 4 mg twice a day on days 2–6. No emesis/no nausea rates were significantly higher in the combination arm. Results in the two ondansetron-alone arms were identical to placebo. Three additional large trials [19, 47, 79] with a total of more than 1,200 patients have compared granisetron [19, 47] or ondansetron [79] combined with dexamethasone to dexamethasone alone. In all three trials, the combination regimen was no better than dexamethasone alone. On balance, the weight of evidence would strongly suggest that the addition of a 5-HT3 antagonist to dexamethasone does not appreciably add to the efficacy of dexamethasone alone in the prevention of cisplatin-induced delayed emesis.
-
d.
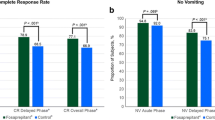
Dexamethasone and aprepitant: In a randomized phase II dose-finding study of the NK1 antagonist aprepitant with cisplatin >70 mg/m2, patients received either standard therapy with ondansetron and dexamethasone on day 1 followed by dexamethasone alone on days 2–5 versus two arms receiving the same standard therapy but combined with either 125 or 40 mg aprepitant day 1 and aprepitant 40 or 25 mg on days 2–5 [6]. Both aprepitant-containing arms were superior to the standard arm of dexamethasone alone for the day 2–5 period, with complete response rates of 72.7%, 63.9%, and 43.7%, respectively. Two phase III trials with identical design have also been reported comparing standard therapy with ondansetron 32 mg plus dexamethasone 20 mg on day 1 followed by dexamethasone 8 mg twice a day on days 2–4 with ondansetron 32 mg, dexamethasone 12 mg and aprepitant 125 mg on day 1 followed by dexamethasone 8 mg daily on days 2–4 and aprepitant 80 mg days 2 and 3 [34, 65]. The primary endpoint was complete response (no emesis, no use of rescue antiemetics) over the 5-day study period. Both studies observed an improved absolute rate of complete response of approximately 20%. During the delayed phase (days 2–5), complete response rates on the aprepitant and standard arms were 75% and 68% versus 56% and 47% in the two studies, respectively. Given the different antiemetic regimens employed for acute prophylaxis, one can question whether a significant component of the improved efficacy of the aprepitant-containing arms during the delayed phase was due to a carryover effect from the different control rates during day 1. A subsequent analysis of the combined database from these two phase II trials strongly suggested that aprepitant provided protection against delayed vomiting regardless of response in the acute phase [25]. In patients with acute vomiting, the proportion of patients with delayed vomiting was 85% and 68% on the control and aprepitant arms, respectively. In patients with no acute vomiting, the proportion with delayed vomiting was 33% and 17% on the control and aprepitant arms, respectively.
Conclusions
We have summarized the nature of delayed emesis and the need for antiemetic prophylaxis for delayed emesis following prophylaxis for acute emesis when chemotherapy regimens of high emetic risk like cisplatin are administered. This is summarized in the consensus statements on delayed emesis below.
For individuals receiving chemotherapy of high emetic risk, our prior guidelines recommended the combination of dexamethasone and a 5-HT3 antagonist to prevent acute emesis [18] and the combination of dexamethasone and either a 5-HT3 antagonist or metoclopramide to prevent delayed emesis [59]. To prevent acute emesis, we now recommend a three-drug combination of aprepitant, dexamethasone, and a 5-HT3 antagonist based on two randomized trials comparing the three-drug aprepitant-containing regimen to our previous two-drug standard of dexamethasone and a 5-HT3 antagonist [34, 65]. For the prevention of delayed emesis, however, both these trials compared the combination of aprepitant and dexamethasone to dexamethasone alone rather than our prior recommended two-drug regimen of dexamethasone plus either metoclopramide or a 5-HT3 antagonist. The combination of dexamethasone and aprepitant was superior to dexamethasone alone in both randomized trials [34, 65]. This observation has led us to recommend aprepitant and dexamethasone for the prevention of delayed emesis in these guidelines when the combination of a 5-HT3 antagonist, dexamethasone, and aprepitant has been used to control acute emesis (Table 1). To date, no trials have compared this regimen for delayed emesis to our previous standard of dexamethasone plus either metoclopramide or a 5-HT3 antagonist. This committee analyzed the randomized trials comparing a 5-HT3 antagonist plus dexamethasone with dexamethasone alone for the prevention of delayed emesis following cisplatin. This analysis revealed no conclusive evidence that the addition of any 5-HT3 antagonist improved the control of delayed emesis over dexamethasone alone [19, 23, 40, 47, 60, 79]. With these data, several committee members felt no need to initiate a trial to formally compare our prior standard delayed-emesis regimen of dexamethasone and a 5-HT3 antagonist with the current recommendation of dexamethasone and aprepitant. The question remains whether the metoclopramide plus dexamethasone regimen for delayed emesis should be compared to aprepitant plus dexamethasone. Only a clinical trial directly comparing these two regimens could definitively assess their relative efficacy.
Control of nausea and vomiting during multiple cycles of chemotherapy of high emetic risk
Many have observed that the control of vomiting and nausea declines with each subsequent chemotherapy cycle in patients receiving multiple courses of chemotherapy. Few studies have specifically investigated the decline in antiemetic control with multiple cycles of cisplatin.
De Wit and colleagues studied the antiemetic effect of tropisetron during six cycles of cisplatin 70–80 mg/m2 [11].Tropisetron was given as a 5 mg intravenous dose before cisplatin followed by 5 mg once daily, orally, on days 2–5. Outcomes were analyzed using both conditional and cumulative probability rates. Using conditional probability rates, the antiemetic efficacy seemed to be maintained through six cycles of cisplatin. When the cumulative probability rates method was used, however, the acute no-vomiting/no-nausea rate declined from 71% in cycle one to 43% in cycle six.
After evidence-based guidelines recommended the combination of a 5-HT3 antagonist plus dexamethasone to prevent emesis following cisplatin [18, 46] for antiemetic prophylaxis in patients receiving cisplatin, de Wit and colleagues studied 125 patients receiving cisplatin >70 mg/m2 [12]. All received antiemetic prophylaxis with granisetron 3 mg plus dexamethasone 10 mg intravenously on day 1 followed by oral granisetron 1 mg twice daily plus oral dexamethasone 8 mg twice daily on days 2–7. The same pattern of falling rates of antiemetic control was seen, with the acute no-vomiting/no-nausea rate declining from 66% in cycle one to 30–39% in cycle six.
In an effort to improve control in subsequent cycles, aprepitant was added to the treatment regimens. In a randomized double-blind study [9], 202 patients receiving their first course of cisplatin ≥70 mg/m2 were randomized to aprepitant 375 mg before cisplatin then 250 mg days 2–5, or aprepitant 125 mg before cisplatin then 80 mg days 2–5, or placebo. All patients received intravenous ondansetron 32 mg and oral dexamethasone 20 mg before cisplatin and oral dexamethasone 8 mg days 2–5. The primary study endpoint (the no-emesis and no-rescue rate for the entire 5-day period following cisplatin) was different from the trials discussed earlier. Patients were followed for up to six cycles. A cumulative probability model for transitional probabilities was used for analysis. In cycle one, the percentage of patients with no-emesis and no-rescue antiemetics days for 5 days after cisplatin was 70% with aprepitant 375/250 mg, 64% with aprepitant 125/80 mg, and 49% in the placebo group. By cycle six, the 5-day no-emesis/no-rescue rate for the 375/250 mg group fell to 65%, the 125/80 mg group rate fell to 59%, and the standard therapy group fell to 34%. The authors concluded that the addition of aprepitant to standard antiemetic therapy increased antiemetic control, and that the magnitude of the benefit over standard therapy was maintained over six cycles of chemotherapy.
Data from two randomized double-blind phase III studies using identical designs [34, 65] were pooled. In these patients receiving cisplatin >70 mg/m2, the addition of aprepitant to a standard ondansetron plus dexamethasone combination led to an improved level of antiemetic effectiveness that was maintained over six cycles of chemotherapy. In every cycle, the proportion of patients with no emesis and no significant nausea for the 5 days following cisplatin was significantly higher in patients receiving aprepitant. Rates for aprepitant plus standard antiemetic therapy were 61% in cycle one and 59% in cycle six versus 46% in cycle one and 40% in cycle six for standard therapy alone [10]. Once again, the percentage improvement of the aprepitant regimen over standard therapy was preserved over six treatment cycles.
Treatment recommendations
Acute emesis following highly emetogenic chemotherapy
Consensus recommendation for the prevention of acute nausea and vomiting emesis following chemotherapy of high emetic risk
To prevent acute vomiting and nausea following chemotherapy of high emetic risk, we recommend a three-drug regimen including single doses of a 5-HT3 antagonist, dexamethasone, and aprepitant given before chemotherapy:
-
MASCC level of consensus: high
-
MASCC level of confidence: high
-
ASCO level of evidence: I
-
ASCO grade of recommendation: A
Delayed emesis following high-emetic-risk chemotherapy
Consensus recommendation for the prevention of delayed nausea and vomiting emesis following chemotherapy of high emetic risk
In patients receiving cisplatin treated with a combination of aprepitant, a 5-HT3 receptor antagonist, and dexamethasone to prevent acute vomiting and nausea, the combination of dexamethasone and aprepitant is suggested to prevent delayed emesis on the basis of its superiority to dexamethasone alone:
-
MASCC level of consensus: moderate
-
MASCC level of confidence: high
-
ASCO level of evidence: II
-
ASCO grade of recommendation: A
Consensus statements: principles of 5-HT3 antagonist antiemetic use to prevent acute vomiting and nausea following chemotherapy of high emetic risk
-
Use the lowest tested fully effective dose
-
No schedule better than a single dose given before chemotherapy
-
The antiemetic efficacy and adverse effects of these agents are comparable in controlled trials
-
Intravenous and oral formulations are equally effective and safe
-
Always give with dexamethasone before chemotherapy
Principles concerning delayed vomiting and nausea following chemotherapy of high emetic risk
-
Delayed nausea and vomiting following cisplatin is a distinct syndrome defined as nausea and vomiting that starts or continues the day following chemotherapy
-
Delayed nausea and vomiting have been defined as commencing 24 or more hours after chemotherapy. However, more recent observations suggest that these syndromes can begin earlier
-
All patients receiving cisplatin should receive antiemetics to prevent delayed nausea and vomiting
-
Given the dependence of delayed emesis and nausea on acute antiemetic outcome, optimal acute antiemetic prophylaxis should be employed. For cisplatin, this includes a three-drug combination of aprepitant, a 5-HT3 antagonist, and dexamethasone.
Summary and conclusions
Consensus recommendations for the doses of each specific antiemetic agent used to prevent acute emesis from chemotherapy of high emetic risk are presented in Table 1. Whenever possible, these recommendations represent an analysis of literature using an evidence-based medicine approach. In addition, they also reflect the input of the discussants and participants during this consensus conference.
The 5-HT3 antagonists, dexamethasone, and the NK1 antagonist aprepitant have substantially improved our ability to prevent acute and delayed emesis and nausea caused by chemotherapy of high emetic risk. These three classes used in combination are the standard of care in patients receiving high-emetic-risk chemotherapy. Nevertheless, many patients continue to experience vomiting and nausea despite receiving optimal prophylaxis for both acute and delayed symptoms. It is likely that these episodes are mediated through mechanisms unaffected by the combined effects of dexamethasone along with 5-HT3 and NK1 blockade. Further improvements are likely to occur after a better understanding of the underlying pathophysiology of emesis caused by chemotherapy allows us to create new drugs that more effectively silence the neural signals that trigger nausea and vomiting. Only then will we be able to eliminate emesis caused by cancer treatment.
References
Aapro E, Selak M, Lichinitser D, Santini A, Macciocchi A, Klinik A, Blokhin NN (2003) Palonosetron (PALO) is more effective than ondansetron (OND) in preventing chemotherapy-induced nausea and vomiting (CINV) in patients receiving moderately emetogenic chemotherapy (MEC): Results of a Phase III trial. Proc ASCO 22:726
Andrews PLR, Davis CJ (1993) The mechanism of emesis induced by anti-cancer therapies. In: Andrews PLR and G.J. Sanger (eds) Emesis in anticancer therapy mechanisms and treatment. Chapman & Hall, London, pp 14–17
Beck TM, Hesketh PJ, Madajewicz S, Navari RM, Pendergrass K, Lester EP, Kish JA, Murphy WK, Hainsworth JD, Gandara DR, Bricker LJ, Keller AM, Mortimer J, Galvin DV, House KW, Bryson JC (1992) Stratified, randomized, double-blind comparison of intravenous ondansetron administered as a multiple- dose regimen versus two single-dose regimens in the prevention of cisplatin-induced nausea and vomiting. J Clin Oncol 10:1969–1975
Blum RA, Majumdar A, McCrea J, et al (2003) Effects of aprepitant on the pharmacokinetics of ondansetron and granisetron in healthy subjects. Clin Ther 25:1407–1419
Campos D, Pereira JR, Reinhardt RR, Carracedo C, Poli S, Vogel C, Martinez-Cedillo J, Erazo A, Wittreich J, Eriksson LO, Carides AD, Gertz BJ (2001) Prevention of cisplatin-induced emesis by the oral neurokinin-1 antagonist, MK-869, in combination with granisetron and dexamethasone or with dexamethasone alone. J Clin Oncol 19:1759–1767
Chawla SP, Grunberg SM, Gralla RJ, Hesketh PJ, Rittenberg C, Elmer ME, Schmidt C, Taylor A, Carides AD, Evans JK, Horgan KJ (2003) Establishing the dose of the oral NK1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting. Cancer 97:2290–2300
Chevalier B (1990) Efficacy and safety of granisetron compared with high-dose metoclopramide plus dexamethasone in patients receiving high-dose cisplatin in a single-blind study. Eur J Cancer 26:S33–S36
Cocquyt V, VanBelle S, Reinhardt RR, Decramer MLA, O’Brien M, Schellens JHM, Borms M, Verbeke L, VanAelst F, DeSmet M, Carides AD, Eldridge K, Gertz BJ (2001) Comparison of L-758,298, a prodrug for the selective neurokinin-1 antagonist, L-754-030, with ondansetron for the prevention of cisplatin-induced emesis. Eur J Cancer 37:835–842
de Wit R, Herrstedt J, Rapoport B, Carides AD, Carides G, Elmer ME, Schmidt C, Evans JK, Horgan KJ (2003) Addition of the oral NK1 antagonist aprepitant to standard antiemetics provides protection against nausea and vomiting during multiple cycles of cisplatin-based chemotherapy. J Clin Oncol 21:4105–4111
de Wit R, Herrstedt J, Rapoport B, et al (2004) The oral NK1 antagonist aprepitant given with standard antiemetics provided protection against nausea and vomiting during multiple cycles of cisplatin-based chemotherapy. A combined analysis of 2 randomized, placebo-controlled trials. Eur J Cancer 40:403–410
de Wit R, Schmitz PIM, Verweij J, et al (1996) Analysis of cumulative probabilities show that the efficacy of 5-HT3 antagonist prophylaxis is not maintained. J Clin Oncol 14: 644–651
de Wit R, van den Berg H, Burghouts J, et al (1998) Initial high antiemetic efficacy of ganisetron with dexamethasone is not maintained over repeated doses. Br J Cancer 77:1487–1491
DeMulder PH, Seynaeve C, Vermorken JB, van LPA, Mols JS, Allman EL, Beranek P, Verweij J (1990) Ondansetron compared with high-dose metoclopramide in prophylaxis of acute multicenter, randomized, double-blind, crossover study. Ann Intern Med 113:834–840
Eisenberg P, Figueroa-Vadillo J, AZamora R, Charu V, Hajdenberg J, Cartmell A, Macciocchi A, Grunberg SM (2003) improved prevention of moderately emetogenic chemotherapy-induced nausea and vomiting with palonosetron, a pharmacologically novel 5-HT3 receptor antagonist. Results of a phase III, single-dose trial versus dolasetron. Cancer 98:2473–2482
Eisenberg P, MacKintosh FR, Ritch P, Cornett PA, Macciocchi A (2004) Efficacy, safety and pharmacokinetics of palonosetron in patients receiving highly emetogenic cisplatin-based chemotherapy: a dose-ranging clinical study. Ann Oncol 15: 330–337
Evidence-Based Medicine WG (1992) Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA 268:420–425
Gandara DR, Harvey W, Moaghan GG, Perez EA, Hesketh PJ (1993) Delayed emesis following high-dose cisplatin: A double-blind randomized comparative trial of ondansetron (GR 38032F) versus placebo. Eur J Cancer 29A:35–38
Gandara DR, Roila F, Warr DG, Edelman MJ, Perez EA, Gralla RJ (1998) Consensus proposal for 5-HT3 antagonists in the prevention of acute emesis related to highly emetogenic chemotherapy. Supp Care Cancer 6:237–243
Goedhals L, Heron JF, Kleisbauer JP, Pagani O, Sessa C (1998) Control of delayed nausea and vomiting with granisetron plus dexamethasone or dexamethasone alone in patients receiving highly emetogenic chemotherapy: A double-blind placebo-controlled, comparative study. Ann Oncol 6:661–666
Gralla R, Lichinitser M, Van Der Vegt S, Sleeboom H, Mezger J, Peschel C, Tonini G, Labianca R, Macciocchi A, Aapro M (2003) Palonosetron improves prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy: results of a double-blind randomized phase III trial comparing single doses of palonosetron with ondansetron. Ann Oncol 14:1570–1577
Gralla RJ, Tyson LB, Kris MG, Clark RA (1987) The management of chemotherapy-induced nausea and vomiting. Med Clin North Am 71:289–301
Gralla RJ, Popovic W, Strup J, Culleton V, Preston A, Friedman C (1997) Can an oral antiemetic regimen be as effective as intravenous treatment against cisplatin: results of a 1054 patient randomized study of oral granisetron versus IV ondansetron. Proc ASCO 16:52b
Gridelli C, Ianniello GP, Ambrosini G, et al (1997) Multicentre, double-blind, randomized trial comparing ondansetron versus ondansetron plus dexamethasone in the prophylaxis of cisplatin-induced delayed emesis. Int J Oncol 10:395–400
Grunberg SM, Stevenson LL, Russell CA, McDermed JE (1989) Dose ranging phase I study of the serotonin antagonist GR38032F for prevention of cisplatin-induced nausea and vomiting. J Clin Oncol 7:1137–1141
Grunberg SM, Hesketh PJ (1993) Control of chemotherapy-induced emesis. N Engl J Med 329:1790-1796
Grunberg SM, Lane M, Lester EP, Sridhar KS, Mortimer J, Murphy W, Sanderson PE (1993) Randomized double-blind comparison of three dose levels of intravenous ondansetron in the prevention of cisplatin-induced emesis. Cancer Chemother Pharmacol 32:268–272
Grunberg SM, Hesketh PJ, Carides AD, et al (2003) Relationships between the incidence and control of cisplatin-induced acute vomiting and delayed vomiting: Analysis of pooled data from two phase III studies of the NK-1 antagonist aprepitant. Proc Am Soc Clin Oncol 22:2931a
Hainsworth J, Harvey W, Pendergrass K, et al (1991) A single-blind comparison of intravenous ondansetron, a selective antagonist, with intravenous metoclopramide in the prevention of nausea and vomiting associated with high-dose cisplatin chemotherapy. J Clin Oncol 9:721–728
Heron JF (1995) Single-agent oral granisetron for the prevention of acute cisplatin-induced emesis: a double-blind, randomized comparison with granisetron plus dexamethasone and high-dose metoclopramide plus dexamethasone. Semin Oncol 22:24–30
Herrstedt J (1996) New perspectives in antiemetic treatment. Support Care Cancer 4:416–419
Hesketh PJ, Murphy WK, Lester EP, Gandara DR, Khojasteh A, Tapazoglou E, Sartiano GP, White DR, Werner K, Chubb JM (1989) GR 38032F (GR-C507/75): a novel compound effective in the prevention of acute cisplatin-induced emesis. J Clin Oncol 7:700–705
Hesketh PJ, Gandara DR (1991) Serotonin antagonists: a new class of antiemetic agents. J Natl Cancer Inst 83:613–620
Hesketh PJ, Gralla RJ, Webb RT, Ueno W, DelPrete S, Bachinsky ME, Dirlam NL, Stack CB, Silberman SL (1999) Randomized phase ii study of the neurokinin 1 receptor antagonist CJ-11,974 in the control of cisplatin-induced emesis. J Clin Oncol 17:338–343
Hesketh PJ, Grunberg SM, Gralla RJ, Warr DG, Roila F, de Wit R, Chawla SP, Carides AD, Ianus J, Elmer ME, Evans JK, Beck K, Reines S, Horgan KJ (2003) The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin—the Aprepitant Protocol 052 Study Group. J Clin Oncol 21: 4112–4119
Hesketh P, Navari R, Grote T, Gralla R, Hainsworth J, Kris M, Anthony L, Khojasteh A, Tapazoglou E, Benedict C, Hahne W (1996) Double-blind, randomized comparison of the antiemetic efficacy of intravenous dolasetron mesylate and intravenous ondansetron in the prevention of acute cisplatin-induced emesis in patients with cancer. J Clin Oncol 14: 2242–2249
IGAR (1994) Italian Group for Antiemetic Research: Cisplatin-induced delayed emesis: Prognostic factors during three subsequent cycles. Ann Oncol 5:585–589
IGAR (1995) Ondansetron versus granisetron, both combined with dexamethasone, in the prevention of cisplatin-induced emesis. Ann Oncol 6:805–810
IGAR (1997) Ondansetron versus metoclopramide, both combined with dexamethasone, in the prevention of cisplatin-induced delayed emesis. J Clin Oncol 15:124–130
IGAR (1998) Double-Blind, Dose-Finding Study of Four Intravenous Doses of Dexamethasone in the Prevention of Cisplatin-Induced Acute Emesis. J Clin Oncol 16:2937–2942
IGAR (1999) A double-blind randomized study comparing intramuscular (i.m.) granisetron with i.m. granisetron plus dexamethasone in the prevention of delayed emesis induced by cisplatin. Anticancer Drugs 5:465–470
Kris MG, Gralla RJ, Clark RA, Tyson LB, OConnell JP, Wertheim MS, Kelsen DP (1985) Incidence, course, and severity of delayed nausea and vomiting following the administration of high-dose cisplatin. J Clin Oncol 3:1379–1384
Kris MG, Gralla RJ, Clark RA, Tyson LB (1988) Dose-ranging evaluation of the serotonin antagonist GR-C507/75 (GR38032F) when used as an antiemetic in patients receiving anticancer chemotherapy. J Clin Oncol 6:659–662
Kris MG, Gralla RJ, Clark RA, Tyson LB (1989) Phase II trials of the serotonin antagonist GR38032F for the control of vomiting caused by cisplatin. J Natl Cancer Inst 81:42–46
Kris MG, Gralla RJ, Tyson LB, Clark RA, Cirrincione C, Groshen S (1989) Controlling delayed vomiting: double-blind, randomized trial comparing placebo, dexamethasone alone, and metoclopramide plus dexamethasone in patients receiving cisplatin. J Clin Oncol 7:108–114
Kris MG, Grunberg SM, Gralla RJ, Baltzer L, Zaretsky SA, Lifsey D, Tyson LB, Schmidt L, Hahne WF (1994) Dose-ranging evaluation of the serotonin antagonist dolasetron mesylate in patients receiving high-dose cisplatin. J Clin Oncol 12:1045–1049
Kris MG, Roila F, de Mulder PHM, Marty M (1998) Delayed emesis following anticancer chemotherapy. Support Care Cancer 6:228–232
Latreille J, Pater J, Johnston D, Laberge F, Stewart D, Rusthoven J, Hoskins P, Findlay B, McMurtrie E, Yelle L, Williams C, Walde D, Ernst S, Dhaliwal H, Warr D, Shepherd F, Mee D, Nishimura L, Osoba D, Zee B (1998) Use of dexamethasone and granisetron in the control of delayed emesis for patients who receive highly emetogenic chemotherapy. J Clin Oncol 16:1174–1178
Louvet C, Lorange A, Letendre F, et al (1991) Acute and delayed emesis after cisplatin-based regimen: Description and prevention. Oncology 48:392–396
Marty M, Pouillart P, Scholl S, Droz JP, Azab M, Brion N, Pujade LE, Paule B, Paes D, Bons J (1990) Comparison of the 5-hydroxytryptamine 3 (serotonin) antagonist ondansetron (GR 38032F) with high-dose metoclopramide in the control of cisplatin-induced emesis. N Engl J Med 322:816–821
Marty M, Kleisbauer J-p, Fournet P, Vergnenegro A, Carics P, Loria-Kanza Y, Simonetta C, Bruijn KM (1995) Is Navoban (tropisetron) as effective as Zofran (ondansetron) in cisplatin-induced emesis? Anti-Cancer Drugs 6:15–21
Matsui K, Fukuoka M, Takada M, Kunsunoki Y, Yana T, Tamura K (1996) Randomized trial for the prevention of delayed emesis in patients receiving high-dose cisplatin. Br J Cancer 73:217–221
Milano S, Blower P, Romain D, Grelot L (1995) The piglet as a suitable animal model for studying the delayed phase of cisplatin-induced emesis. J Pharmacol Exp Ther 274:951–961
Moreno I, Rosell R, Abad A (1992) Comparison of three protracted antiemetic regimens for the control of delayed emesis in cisplatin-treated patients. Eur J Cancer 28A:1344–1347
Navari RM, Kaplan HG, Gralla RJ, Grunberg SM, Palmer R, Fitts D (1994) Efficacy and safety of granisetron, a selective 5-hydroxytryptamine-3 receptor antagonist, in the prevention of nausea and vomiting induced by high-dose cisplatin. J Clin Oncol 12:2204–2210
Navari R, Gandara D, Hesketh P, Hall S, Mailliard J, Ritter H, Friedman C, Fitts D (1995) Comparative clinical trial of granisetron and ondansetron in the prophylaxis of cisplatin-induced emesis. J Clin Oncol 13:1242–1248
Navari RMl, Hesketh PJr (1999) Use of Placebos in Delayed-Emesis Studies (letter). J Clin Oncol 17:338–343
Navari RM, Madajewicz S, Anderson N, Tchekmedyian NS, Whaley W, Garewal H, Beck TM, Chang AY, Greenberg B, Caldwell KC, Huffman DH, Gould JR, Carron G, Ossi M, Anderson EM (1995) Oral ondansetron for the control of cisplatin-induced delayed emesis: a large, multicenter, double-blind, randomized comparative trial of ondansetron versus placebo. J Clin Oncol 13:2408–2416
Navari RM, Reinhardt RR, Gralla RJ, Kris MG, Hesketh PJ, Khojasteh A, Kindler H, Grote TH, Pendergrass K, Grunberg SM, Carides AD, Gertz BJ (1999) Reduction of cisplatin-induced emesis by a selective neurokinin-1-receptor antagonist. N Engl J Med 340:190–195
Nolte MJ, Berkery R, Pizzo B, Baltzer L, Grossano D, Lucarelli CD, Kris MG (1998) Assuring the optimal use of serotonin antagonist antiemetics: The process for development and implementation of institutional antiemetic guidelines at Memorial Sloan–Kettering Cancer Center. J Clin Oncol 16:771–778
Olver I, Paska W, Depierre A, Seitz JF, Stewart DJ, Goedhals L, McQuade B, McRae J, Wilkinson JR (1996) A multicentre, double-blind study comparing placebo, ondansetron and ondansetron plus dexamethasone for the control of cisplatin-induced delayed emesis. Ann Oncol 9:945–952
Passalacqua R, Cocconi G, Bella M, Monici L, Michiara M, Bandini N, Bacchi M (1992) Double-blind, randomized trial for the control of delayed emesis in patients receiving cisplatin: comparison of placebo vs. adrenocorticotropic hormone (ACTH). Ann Oncol 3:481–485
Passalacqua R, Cocconi G, Caminiti C, Silingardi V, Bella MA, Bichisao E, Michiara M, Malavasi V, Donati D, DiCostanzo F, Rocca A, DiSarra S, Scaglione F, Fraschini F (1997) Double-blind, multicenter, randomized trial to compare the effect of two doses of adrenocorticotropic hormone versus placebo in controlling delayed emesis after high-dose cisplatin in adult patients with cancer. J Clin Oncol 15:2467–2473
Perez EA (1995) Review of the preclinical pharmacology and comparative efficacy of 5-hydroxyoyptamine-3 receptor antagonists for chemotherapy-induced emesis. J Clin Oncol 13:1036–1043
Perez EA, Hesketh PJ, Gandara DR (1991) Serotonin antagonists in the management of cisplatin-induced emesis. Semin Oncol 18: 73–80
Poli-Bigelli S, Rodrigues-Pereira J, Carides AD, Julie Ma G, Eldridge K, Hipple A, Evans JK, Horgan KJ, Lawson F (2003) Addition of the neurokinin 1 receptor antagonist aprepitant to standard antiemetic therapy improves control of chemotherapy-induced nausea and vomiting. Results from a randomized, double-blind, placebo-controlled trial in Latin America. Cancer 97:3090–3098
Riviere A, on behalf of the Granisetron Study Group (1994) Dose finding study of granisetron in patients receiving high-dose cisplatin chemotherapy. Br J Cancer 69:967–971
Roila F, Boschetti E, Tonato M (1991) Predictive factors of delayed emesis in cisplatin treated patients and antiemetic activity and tolerability of metoclopramide or dexamethasone. A randomized single-blind study. Am J Clin Oncol 14:238–242
Roila F, Tonato M, Cognetti F, Cortesi E, Favalli G, Marangolo M, Amadori D, Bella MA, Gramazio V, Donati D, Ballatori E, Del Favero A (1991) Prevention of cisplatin-induced emesis: a double-blind multicenter randomized crossover study comparing ondansetron and ondansetron plus dexamethasone. J Clin Oncol 9:675–678
Roila F, Donati D, Tamberi S, Margutti G (2002) Delayed emesis: incidence, pattern, prognostic factors and optimal treatment. Support Care Cancer 10:88–95
Rudd JA, Jordan CC, Naylor RJ (1994) Profiles of emetic action of cisplatin in the ferret: a potential model of acute and delayed emesis. Eur J Pharmacol 262:R1–R2
Ruff P, Paska W, Goedhals L, Pouiliart P, Riviere A, on behalf of the Granisetron Study Group, Vorolieof D, Bloch, Jones A, Martin L, Brunet R, Butcher, Forster J, McQuade B, on behalf of the Ondansetron and Granisetron Emesis Study Group (1994) Ondansetron compared with granisetron in the prophylaxis of cisplatin-induced acute emesis: a multicenter double-blind, randomized, parallel-group study. Oncology 51:113–118
Seynaeve C, Schuller J, Buser K, Porteder H, Van Belle S, Sevelda P, Christmann D, Schmidt M, Kitchener H, Pacs D, de Mulder PHM, on behalf of the Ondansetron Study Group (1992) Comparison of the antiemetic efficacy of ondansetron given as either a continuous infusion or a single intravenous dose, in acute cisplatin-induced emesis. A multicenter, double-blind, randomized, parallel group study. Br J Cancer 66:192–197
Shinkai T, Saijo N, Eguchi K, Sasaki Y, Tamura T, Fujiwara Y (1989) Control of cisplatin-induced delayed emesis with metoclopramide and dexamethasone: a randomized controlled trial. Jpn J Clin Oncol 19:40–44
Smyth J (1992) Delayed emesis after high-dose cisplatin--the residual problem. In: Proceedings of the Satellite Symposium to the XVII Congress of the European Society for Medical Oncology, Lyon, pp. 24–26
Soukop J, on behalf of the Granisetron Study Group (1994) A dose-finding study of granisetron, a novel antiemetic, in patients receiving high-dose cisplatin. Support Care Cancer 2:177–183
Soukop M, McQuade B, Hunter E, et al (1992) Ondansetron compared with metoclopramide in the control of emesis and quality of life during repeated chemotherapy for breast cancer. Oncology 49:295–304
Tattersall FD, Rycroft W, Hill RG, Hargreaves RJ (1994) Enantioselective inhibition of apomorphine-induced emesis in the ferret by the neurokinin receptor antagonist CP-99,994. Neuropharmacology 33:259–260
Thant M, Pendergras K, Harman G, Modiano M, Martin L, DuBois D, Cramer M, Hahne W (1996) Double-blind, randomized study of the dose-response relationship across five single doses of IV dolasetron mesylate (DM) for prevention of acute nausea and vomiting (ANC) after cisplatin chemotherapy (CCT). Proc ASCO 15:533
Tsukada H, Hirose T, Yokoyama A, Kurita Y (2001) Randomized comparison of ondansetron plus dexamethasone with dexamethasone alone for the control of delayed cisplatin-induced emesis. Eur J Cancer 37:2398–2404
Van Belle S, Lichinitser MR, Navari RM, Garin AM, Decramer MLA, Rivier A, Thant M, Brestan E, Bui B, Eldridge K, DeSmet M, Michiels N, Reinhardt RR, Carides AD, Evans JK, Gertz BJ (2002) Prevention of cisplatin-induced acute and delayed emesis by the selective neurokinin-1 antagonists, L-758-298 and MK-869. Cancer 94(11):3032–3041
Van Belle S-P, Stamatakis L, Bleiberg H, Cocquyt FJ, Michel J, de Bruijn KM (1994) Dose-finding study of tropisetron in cisplatin-induced nausea and vomiting. Ann Oncol 5:821–825
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00520-005-0833-4
Rights and permissions
About this article
Cite this article
Kris, M.G., Hesketh, P.J., Herrstedt, J. et al. Consensus proposals for the prevention of acute and delayed vomiting and nausea following high-emetic-risk chemotherapy. Support Care Cancer 13, 85–96 (2005). https://doi.org/10.1007/s00520-004-0699-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-004-0699-x