Abstract
Background
Oral transmucosal fentanyl citrate (OTFC; ACTIQ) incorporates fentanyl into a lozenge allowing drug delivery through the oral mucosa resulting in rapid pain relief. OTFC is effective for breakthrough pain and could be particularly useful in patients with mucositis.
Methods
This randomized, double-blind, crossover study assessed two formulations of OTFC for tolerability in 14 patients with radiation-induced mucositis. On four separate days, patients with grade 3 or 4 mucositis received an OTFC unit 45 min before radiation treatment. Two units had a sweetened matrix formulation and two had a compressed powder formulation. One unit of each formulation contained 200 μg fentanyl and one was placebo. Tolerability, mucositis pain, and formulation preference were evaluated. Changes in oral mucosa were recorded.
Results
Both formulations of OTFC were well tolerated. There were no significant differences between formulations in tolerability, patient preference, or VAS pain scores. No changes in oral mucosa were noted. Common treatment-related adverse events included a burning sensation in the mouth, nausea, and vomiting.
Conclusions
Both formulations of OTFC are well tolerated. The presence of fentanyl in either the sweetened matrix or the compressed powder did not alter tolerability or safety. The dose of fentanyl tested did not yield analgesia greater than placebo; future studies of OTFC efficacy in mucositis should evaluate higher doses than 200 μg.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral mucositis is common problem in the cancer population. It may be associated with radiation therapy or chemotherapy, or relate to numerous other conditions, including infection. Oral mucositis is painful and may become severe enough to prevent patients from speaking, eating, drinking, or swallowing oral medications. If severe enough to warrant discontinuation of treatment, it can reduce the chance of local control or even cure.
In patients with dysphagia caused by mucositis, opioid therapy for severe pain may require a route of administration that does not rely on swallowing solid drug formulations, such as tablets or pills. Drug delivery across the oral mucosa may provide an alternative method of opioid delivery. The OTS (oral transmucosal system) is a drug delivery system that is currently available as oral transmucosal fentanyl citrate (OTFC ;ACTIQ). OTFC incorporates fentanyl citrate into a lozenge (either a cooked, sweetened matrix or a compressed powder formulation) that is attached to a handle. The OTFC unit is self-administered and delivers fentanyl (200–1,600 mcg/U) for absorption across the buccal mucosa as the lozenge dissolves. Dissolution of the lozenge typically occurs within 15 min. OTFC has been shown to deliver rapid analgesia, within 15 min, to opioid-tolerant patients who experience breakthrough pain [4, 9, 12, 7].
Currently, OTFC is available in a cooked sweetened matrix and is used in the United States for management of breakthrough pain. Although an alternative compressed powder formulation of OTFC is not currently available for use in the United States, it is bioequivalent to the cooked sweetened matrix (data on file, Cephalon, Inc.) and is currently marketed in Europe.
Neither formulation of OTFC has been studied for use in patients with oral mucositis. Due to the painful nature of this disorder and the possibility that oral lesions could alter either the pharmacokinetics or pharmacodynamics of the fentanyl contained in the OTS system, studies are needed to, first, assess tolerability and, second, evaluate effects. This pilot study was primarily conducted to determine whether cancer patients with grades 3 or 4 radiation-induced oral mucositis can tolerate OTFC when administered as either the sweetened matrix or the compressed powder. Tolerability and safety were the primary outcomes of interest; analgesic efficacy and patient preference of formulation also were recorded.
Materials and methods
The study used a randomized, double-blind, crossover design to evaluate two formulations of OTFC in cancer patients with grade 3 (n=12) or grade 4 (n=2) radiation-induced oral mucositis. Grade 3 mucositis is the presence of severe mouth ulceration, edema, pain and dysphagia, and grade 4 mucositis is defined as contiguous ulceration, severe pain, dysphagia, and erythema, and there may be the presence of infection. The two formulations (Cephalon Inc.) comprised a sweetened matrix and a compressed powder. The study was approved by the Institutional Review Board, and all patients gave written informed consent prior to participation. The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 1983.
Study population
Adult head and neck cancer patients receiving radiation therapy (with or without concomitant chemotherapy) were eligible for the study if: (a) examination revealed grades 3 or 4 oral mucositis; (b) pain was being treated for at least 1 week with an opioid equivalent to at least 60 mg oral morphine per day or 50 mcg transdermal fentanyl per hour; (c) the opioid dose had been stable for at least 48 h; and (d) an oral mucositis pain score was at least 30 mm on a visual analog scale (VAS) that ranged from 0 to 100 mm.
Patients were excluded from the study if: (a) they were using local analgesics (e.g., topically-acting suspensions) for oral mucositis as they progressed into grades 3 or 4 mucositis and this usage was likely to affect OTFC tolerability; (b) they had hypersensitivities or contraindications to any compound present in study medications; (c) they had a current history of substance abuse; or (d) they reported cardiopulmonary, neurologic, or psychiatric disease that would compromise data collection. Patients who had participated in an investigational drug study within 30 days of screening were also excluded.
Procedures
Patients with grades 3 or 4 oral mucositis were enrolled in this randomized, double-blind, crossover study. One dose of study drug was administered just prior to each of four visits for radiation treatment. Each patient received two units of a sweetened matrix formulation and two units of a compressed powder formulation of OTFC. For each formulation, one unit contained 200 mcg fentanyl and one contained placebo. A minimum of 16 h separated study visits; study treatments were given on consecutive days of radiation, and the total study duration did not exceed 14 days. Each study visit coincided with a regularly scheduled radiation therapy visit. The order in which the patient received treatments was determined by a computer-generated randomization code.
Eligible patients were screened for enrollment in the study. The investigator evaluated each patient’s oral mucositis according to the National Institutes of Health Common Toxicity Criteria [2] and performed a medical history and physical exam. Women of childbearing potential received a urine pregnancy test. Following these evaluations, the patient was assigned a randomization number and instructed in the proper use of the OTS unit. Patients were told to self-administer the OTS unit by moving it over the mucosal lining of the cheek, taking care not to bite or chew the unit. Patients were instructed that a minimum of 2 h must have elapsed between the last dose of the patient’s usual analgesic and administration of study drug.
Patients were reevaluated by an investigator during subsequent visits to the radiation therapy department. If a patient remained eligible, the first study treatment was initiated. Subsequent treatments were administered prior to three additional radiation treatments.
The procedures for the first three treatments were identical. The patients self-administered the OTS unit. The start time was recorded, and the patient provided oral mucositis pain scores at 5, 10, 15, 30, and 45 min after the start of the OTS unit administration. Vital signs were measured prior to study drug administration and at 15, 30, and 45 min after the start of study drug administration. When the patient indicated that he or she was finished with the OTS unit, the stop time was recorded and the patient provided a tolerability score. The patient’s oral mucosa was then examined for changes, and the investigator estimated the amount of the OTS unit consumed. Adverse events were elicited with an open-ended question during consumption of the drug and again after the unit was consumed. The latter assessment occurred prior to the start of the radiation treatment, which began no sooner than 45 min after the start of OTS unit administration. Patients remained in the clinic a minimum of 1.5 h after study drug administration and were discharged only after being evaluated by the investigator. For the fourth OTS administration, the same procedures were followed, except that in addition to the procedures noted above, a physical examination was performed, and patients ranked their preference for each OTS unit formulation using demonstration units.
Outcome measures
Oral mucositis was graded according to the National Institutes of Health Common Toxicity Criteria: 0=none, 1=erythema of the mucosa, 2=patchy pseudomembranous reaction, 3=confluent pseudomembranous reaction, 4=necrosis or deep ulceration. Tolerability was scored by the patient using a 4-point categorical scale (1=easily tolerated, no discomfort with use; 2=mild discomfort with use, but not enough to interfere with administration of unit; 3=moderate discomfort with use, administration of unit somewhat impaired; 4=severe discomfort with use, unable to administer unit). At 5, 10, 15, 30, and 45 min following the start of study drug administration, oral mucositis pain “right now” was scored by the patient using a 100 mm visual analog scale (VAS), reflecting no pain at 0 mm and the worst pain ever experienced at 100 mm. When the patient had finished the OTS unit, the investigator recorded the OTS administration time and visually estimated the amount of OTS unit consumed by the patient, choosing one of the following: 90–100%, 70–89%, 50–69%, or <50%. At the conclusion of the study, patients were asked to rank their preference by selecting one of the following options: preferred the sweetened matrix; preferred the compressed powder; had a similar preference (similar preference means both units tasted the same, one not better than the other), or had no preference (no preference means the patients did not have an opinion). Adverse events were recorded, and the investigator noted any changes in the oral mucosa. Vital signs (blood pressure, heart rate, and respiratory rate) were measured.
Data analysis
The study was designed as a pilot to explore for the first time the potential for adverse or beneficial effects of OTFC in mucositis. The sample size of 14 patients was selected a priori as large enough to provide useful information about tolerability and safety.
The primary outcome was the tolerability ratings for each formulation of the OTS unit, matrix versus powder. The tolerability distributions were tabulated. Because the tolerability score was ordinal, the size of the difference of the scores was not evaluated. For each patient, the tolerability score for the active powder formulation was subtracted from the tolerability score for the active matrix formulation. Likewise, for each patient, the tolerability score for the placebo powder was subtracted from the tolerability score for the placebo matrix. For these within-patient differences, a +1 was assigned for a positive difference, a 0 was assigned for no difference, and a −1 was assigned for a negative difference. The two scores were added together to create a tolerability comparison variable with defined characteristics. A Wilcoxon signed ranks test was then used to determine whether the distribution of the tolerability comparison variable was centered at 0. If the p value was <0.05 and the mean of the tolerability comparison variable was negative, then the matrix formulation was better tolerated. If the p value was <0.05 and the mean of the tolerability comparison variable was positive, then the powder formulation was better tolerated. Otherwise, there was not sufficient evidence to reject the hypothesis that the two formulations were tolerated equally well. If the better-tolerated formulation differed for active and placebo, the above test would show no advantage to either matrix or powder. This test would have decreased power if the tolerability comparison variable frequently took the value 0 [10].
A paired sign test also was used to compare tolerability scores between formulations for active and placebo treatments separately (i.e., a sign test was used to compare the tolerability scores of active matrix versus active powder, and a sign test was used to compare the tolerability scores of placebo matrix versus placebo powder). The sign test assumed that the scale of measurement for the tolerability score was ordinal and did not require it to be interval. A p value ≤0.05 was considered significant for this test.
Descriptive statistics were calculated overall and by treatment for the following variables: pain score at each evaluation, maximum change from baseline in pain score, time to maximum change in pain score, duration of OTS unit administration, amount of OTS unit consumed, and OTS unit formulation preference. The maximum change in pain score from baseline was computed by subtracting the pain VAS score at 0 min from the pain VAS score at 0, 5, 10, 15, 30, and 45 min to obtain the change from baseline at each time. The maximum change from baseline score was the change from baseline score that was largest in absolute value. A decrease in pain from baseline was expressed as a negative number, while an increase in pain from baseline was a positive number. The time from baseline to maximum change in pain score was calculated by determining the first time (0, 5, 10, 15, 30, or 45 min) associated with the maximum change from baseline pain score. The length of time required for OTS unit consumption was calculated by subtracting the start time of administration from the stop time. The Wilcoxon signed rank test was used to compare formulations separately within active and placebo (i.e., active matrix versus active powder and placebo matrix versus placebo powder) for duration of administration, maximum change from baseline in pain score, and time to maximum change in pain score. A sign test was used to evaluate the amount of OTS unit consumed and to compare changes in oral mucosa. Under the null binomial distribution with success probability of 0.50, an exact test was used to determine if, after eliminating no or similar preference groups, formulation preferences were consistent with the null hypothesis of equal preference between OTS unit formulations of powder and matrix. All statistical calculations were done using SAS (version 6.12; SAS Institute, Cary, NC, USA).
Results
Fourteen adult patients with head and neck cancer (ten men, four women) participated in this study. In accordance with the protocol, one patient requiring increased analgesics for persistent pain between treatments was withdrawn following the second treatment. The mean (±SD) patient age was 53±9 years, and 11 of the 14 patients were white (Table 1). At the time of OTS administration, the majority of patients (n=12; 86%) had an oral mucositis grading of 3, and the remainder (n=2; 14%) had a grading of 4. All patients were receiving some type of opioid analgesia for chronic pain, and five (36%) were using a laxative and/or stool softener for constipation. Six (43%) were using an oral rinse containing diphenhydramine, lidocaine, and an antacid prior to and during the study period; all stopped when mucositis reached grade 3 or 4. Other medications taken during the study included antiretrovirals (for HIV infection), antibiotics, antiemetics, and treatment for anemia.
Most patients considered all OTS units to be easily tolerated, and no patient rated any of the OTS units as producing severe discomfort with use (Table 2). The difference in tolerability ratings between the sweetened matrix and compressed powder overall was not statistically significant (p=0.063), nor were the differences between the matrix and powder for either the active formulation (p=0.375) or placebo formulation (p=0.063).
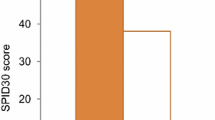
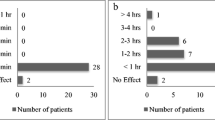
At baseline, median pain VAS scores were similar across the fur treatment conditions (56 mm and 52 mm for active and placebo sweetened matrix, and 49 and 61 mm for active and placebo compressed powder, respectively). Reductions in oral mucositis pain were observed for all four treatments as early as the first scheduled time point (5 min after the start of OTS unit administration) and at each scheduled time point thereafter. The median change from baseline at 45 min was −31 mm and −42 mm for active and placebo sweetened matrix, respectively and −30 mm and −36 mm for active and placebo compressed powder. Differences in maximum change in pain VAS scores between the active matrix and active powder formulations and between the placebo matrix and placebo powder formulations were not statistically significant (p=0.146 and p=0.186, respectively; Table 2). Median time to maximum change in pain VAS scores were similar between the four treatment groups—30 min and 38 min for active and placebo sweetened matrix, and 45 min and 30 min for active and placebo compressed powder, respectively (Table 2).
Most patients consumed between 90–100% of each OTS unit (Table 2). Consumption of the sweetened matrix was higher overall than consumption of the compressed powder for both active and placebo formulations, although the differences were not significant within either the active or placebo formulation (p=0.125 within both active and placebo). The median administration times for the sweetened matrix (18 and 17 min) were lower than the median administration times for the compressed powder (20 and 25 min) for both active and placebo formulations, respectively, although none of these differences attained statistical significance (Table 2).
More patients (seven patients; 50%) preferred the sweetened matrix than preferred the compressed powder matrix (three patients; 21%). Three patients (21%) had no preference. The difference between the proportions of patients preferring the sweetened matrix to the powder formulation was not statistically significant (p=0.343).
Both formulations were well tolerated. No changes in oral mucosa were identified for any patient. The formulations were comparable with respect to the incidence and type of adverse events reported. The most frequent study-drug-related adverse event was a burning sensation in the mouth and was reported more frequently with the compressed powder matrix (five patients each in the placebo and active groups) than the sweetened matrix formulation (two patients each in the placebo and active groups). The burning sensation in the mouth was generally mild in intensity. The only other treatment-related adverse events were nausea and vomiting in one patient when receiving the placebo powder formulation. No patient withdrew from the study due to an adverse event.
Discussion
Previous controlled trials of OTFC [4, 9, 12, 7]have not allowed conclusions about the tolerability and effects of this formulation in patients with moderate or severe oral mucositis. Given the potential for change in both pharmacokinetics and pharmacodynamics following local application of fentanyl to damaged mucosa, and the possibility of poor tolerability related either to the contact of a solid lozenge against inflamed tissue or to the active drug itself, studies of OTFC in mucositis patients must be designed to systematically assess a variety of outcomes, including local tissue changes, tolerability, adverse drug effects, and analgesic efficacy. As an initial step in this evaluation, we conducted a pilot study that had tolerability as the primary outcome but included a methodology (double-blind, placebo-controlled drug administration) that permitted exploration of drug effects.
The results of this pilot demonstrate that both sweetened matrix and compressed powder formulations of OTFC were well tolerated in 78% of patients; only 19% reported mild discomfort, which did not interfere with administration. The presence of active drug in either formulation did not alter tolerability or safety. While more patients favored the sweetened matrix formulation, this preference was not significant. All four treatments produced progressively less oral mucositis pain at each time point after receiving the OTFC unit, and reductions in pain were similar for all groups. Because the study was not powered to evaluate efficacy between the active and placebo doses, and we did not require dose adjustments, the finding of no difference is not interpretable. Although a lack of efficacy of fentanyl compared with placebo is a possible explanation, more plausible reasons for the lack of difference between active and placebo include an inadequate dose of fentanyl, a powerful, nonspecific effect such as the benefit of increased saliva produced by consuming the OTFC unit, and a large placebo effect. Future studies evaluating the efficacy of OTFC for managing oral mucositis will need to be adequately powered and will need to incorporate titration to an adequate dose into the study design.
Currently, few therapeutic options are available to effectively manage pain from oral mucositis. Magic Mouthwash, the oral rinse containing diphenhydramine, lidocaine, and an antacid, is a widely used medication for reducing pain in these patients. Amifostine, a cytoprotector, has been shown to reduce severe mucositis and the use of analgesic drugs when given prior to high dose chemotherapy [3]. Anderson et al. [1] reported that low-dose oral glutamine on painful stomatitis during bone marrow transplantation decreased the severity and duration of oropharyngeal mucositis in autologous bone marrow transplant patients but not in allogeneic bone marrow transplant patients.
As a result of the paucity of therapeutic options available for painful oral mucositis, opioids have been the mainstay of therapeutic management [5, 8, 6]. However, many patients experience mucositis that is severe enough to prevent them from drinking, swallowing, or taking oral medications. Drug delivery across the oral mucosa might provide another therapeutic option for patients with this condition. Because fentanyl is potent and highly lipophilic, it is readily absorbed from the oral mucosa and rapidly crosses the blood brain barrier. There is evidence that OTFC has a more rapid onset than oral opioids [10, 11]and this characteristic was primary in its development as a specific therapy for cancer-related breakthrough pain.
This pilot study suggests that OTFC would be tolerated by most patients with severe mucositis. Additional well-controlled efficacy trials should be pursued. Our data suggest that these future studies may use either the compressed powder or the sweetened matrix. Limitations in this pilot study, including lack of dose titration and small sample size, should be addressed in future studies. Future studies also should evaluate the absorption pharmacokinetics of fentanyl and the pharmacokinetic-pharmacodynamic relationship in this group of patients to determine whether the pharmacokinetics are altered when oral mucosa is injured and whether topical effects of the drug may be relevant. In conclusion, the data suggest that OTFC can be a well-tolerated drug when administered for pain to patients with oral mucositis.
References
Anderson PM, Ramsay NK, Shu XO, Rydholm N, Rogosheske J, Nicklow R, Weisdorf DJ, Skubitz KM (1998) Effect of low-dose oral glutamine on painful stomatitis during bone marrow transplantation. Bone Marrow Transplant 22(4):339–344
Cancer Therapy Evaluation Program (CTEP) (1999) Common Toxicity Criteria (CTC), Version 2.0. Division of Cancer Treatment and Diagnosis, National Cancer Institute, National Institutes of Health, Department of Health and Human Services, March 1998, p. 12
Capelli D, Santini G, De Souza C et al (2000) Amifostine can reduce mucosal damage after high-dose melphalan conditioning for peripheral blood progenitor cellautotransplant: a retrospective study. Br J Haematol 110(2):300–307
Christie JM, Simmonds M, Patt R et al (1998) Dose-titration, multicenter study of oral transmucosal fentanyl citrate for the treatment of breakthrough pain in cancer patients using transdermal fentanyl for persistent pain. J Clin Oncol 16:3238–3245
Coda BA, O’Sullivan B, Donaldson G, Bohl S, Chapman CR, Shen DD (1997) Comparative efficacy of patient-controlled administration of morphine, hydromorphone, or sufentanil for the treatment of oral mucositis pain following bone marrow transplantation. Pain 72(3):333–46
Collins JJ, Geake J, Grier HE, Houck CS, Thaler HT, Weinstein HJ, Twum-Danso NY, Berde CB. Patient-controlled analgesia for mucositis pain in children: a three-period crossover study comparing morphine and hydromorphone. J Pediatr 1996;129(5):722–728
Coluzzi PH, Schwartzberg L, Conroy JD et al (2001) Breakthrough cancer pain: a randomized trial comparing oral transmucosal fentanyl citrate (OTFC) and morphine sulfate immediate release (MSIR). Pain 91:123–130
Dunbar PF, Chapman CR, Buckley FP, Gavrin JR (1996) Clinical analgesic equivalence for morphine and hydromorphone with prolonged PCA. Pain 68:265–270
Farrar JT, Cleary, J, Rauck R, Busch M, Nordbrock E (1998) Oral transmucosal fentanyl citrate: randomized, double-blinded, placebo-controlled trial for treatment of breakthrough pain in cancer patients. J Natl Cancer Inst 90:611–616
Hollander M, Wolfe DA (1999) Nonparametric statistical methods. Wiley, New York p. 46
Lichtor JL, Sevarino FB, Joshi GP, Busch MA, Nordbrock E, Ginsberg B (1999) The relative potency of oral transmucosal fentanyl citrate (OTFC) compared with intravenous morphine in the treatment of moderate to severe postoperative pain. Anesth Anal 89(3):732–738
Portenoy RK, Payne R, Coluzzi P et al (1999) Oral transmucosal fentanyl citrate (OTFC) for the treatment of breakthrough pain in cancer patients: a controlled dose titration study. Pain 79:303–312
Acknowledgements
Supported by a grant from Cephalon, Inc., West Chester, Pennsylvania, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaiova, L., Lapin, J., Manco, L.S. et al. Tolerability and effects of two formulations of oral transmucosal fentanyl citrate (OTFC; ACTIQ) in patients with radiation-induced oral mucositis. Support Care Cancer 12, 268–273 (2004). https://doi.org/10.1007/s00520-004-0595-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-004-0595-4