Abstract
Fentanyl buccal soluble film (Onsolis®, Breakyl®, Painkyl™) comprises two layers: a mucoadhesive layer containing the active drug, and an inactive layer with the aim of preventing the diffusion of fentanyl into the oral cavity. It is approved in several countries worldwide, including the USA and those of the EU, for the management of breakthrough cancer pain in opioid-tolerant, adult patients with cancer. This article reviews the pharmacological properties of fentanyl buccal soluble film and its clinical efficacy and tolerability in these patients. Fentanyl buccal soluble film provides an additional option for transmucosal delivery of fentanyl, with approximately half of the dose undergoing an initial, rapid absorption via the buccal mucosa (accounting for its high bioavailability). In clinical trials, fentanyl buccal soluble film was associated with significant improvements in pain intensity scores versus placebo and was generally well tolerated. The most common adverse events were typical opioid-associated adverse events, such as nausea and vomiting. Fentanyl buccal soluble film is a useful option for the treatment of breakthrough cancer pain in opioid-tolerant patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Soluble film comprising a mucoadhesive active layer and an inactive barrier layer |
Significantly improves pain intensity scores |
Generally well tolerated; the most common adverse events are typical opioid-related adverse events |
The US prescribing information carries a boxed warning regarding the increased risk of fatal respiratory depression, the differences in pharmacokinetic profiles between fentanyl formulations, and abuse potential |
1 Introduction
Breakthrough cancer pain, generally defined as any transitory pain experienced by a cancer patient who is currently receiving maintenance pain treatment controlling persistent pain levels, becomes more common as the patient progresses towards the more advanced stages of the disease [1]. It has a rapid onset and a short duration time [1–4]; thus, slower-release drugs are generally not as effective as immediate-release treatments [5]. Immediate-release, short-acting opioids are generally recommended to treat breakthrough cancer pain [6, 7].
Fentanyl is available in multiple formulations, including several immediate-release formulations [e.g. oral transmucosal fentanyl citrate, a sublingual tablet, a sublingual spray, an intranasal spray, a pectin-based nasal spray, a buccal tablet, and fentanyl buccal soluble film (Onsolis®, Breakyl®, Painkyl™)] [1–4].
Fentanyl buccal soluble film consists of two layers: a mucoadhesive layer containing the active drug, and an inactive layer with the aim of preventing the diffusion of fentanyl into the oral cavity [8]. The drug was initially approved by the US FDA in 2009 [9]; however, as a result of appearance issues in the film, manufacturing of this formulation was ceased [10], and a new formulation was granted FDA approval in 2015 [11]. The issue with the formulation did not affect the product as manufactured in other countries (e.g. in the EU) [10]. This article reviews the pharmacological properties of fentanyl buccal soluble film and its clinical efficacy and tolerability in opioid-tolerant patients with breakthrough cancer pain.
2 Pharmacodynamic Properties of Fentanyl
The pharmacodynamic properties of various formulations of fentanyl are well established [12–18], and are only briefly summarized here.
Fentanyl is a highly potent synthetic opioid [8, 13, 19]. It displays dose-dependent analgesic and sedative effects, resulting from its interaction with opioid receptors in the CNS, acting as an agonist [8, 13, 19], although the precise mechanism of action is unknown [8]. Its highest affinity is for the μ-opioid receptor [inhibition constant (Ki) of 0.7 nmol/L], with lower affinity for the δ- and κ-opioid receptors (Ki of 153 and 85 nmol/L); the Ki for the orphan-opioid receptor (an opioid-like receptor) is >10,000 nmol/L [2]. The analgesic properties of fentanyl are most likely primarily mediated by μ1-opioid receptors, according to animal data [17]. Fentanyl has an analgesic effect that is ≈75–100 times more potent than morphine [13]. Analgesia occurs at blood fentanyl concentrations of 1–2 ng/mL [19].
Fentanyl, like all opioids, induces other effects related to agonist activity at opioid receptors, including respiratory depression (potentially life-threatening), miosis, physical dependence, anxiolysis, euphoria, bradycardia and constipation (Sect. 5) [8, 13, 19]. Unlike with morphine, peripheral vasodilation and hypotension are rarely observed with fentanyl treatment; this treatment difference may be because morphine, but not fentanyl, is associated with increased plasma levels of histamine (in surgical patients), as well as the release of nitric oxide (a potent vasodilator) by endothelial cells (in vitro data) [13]. However, the US prescribing information states that fentanyl may lead to a release of histamine with or without peripheral vasodilation [8].
Fentanyl buccal soluble film 200 μg did not cause or worsen oral mucosal irritation or pain in an open-label, single-dose study in opioid-naïve cancer patients (7 patients with grade 1 oral mucositis and 7 matched controls) [8, 25].
Opioids have been shown to have effects on hormone secretion in humans; e.g. the inhibition of adrenocorticotropic hormone, cortisol and luteinizing hormone secretion and the stimulation of prolactin, growth hormone, insulin and glucagon secretion [8]. Thyroid-stimulating hormone secretion may be inhibited or stimulated by opioids [8].
The concomitant use of fentanyl with partial opioid agonists or antagonists (e.g. buprenorphine, nalbuphine, pentazocine) may induce withdrawal symptoms in opioid-dependent patients, as they have a high affinity to opioid receptors and relatively low intrinsic activity, which partially antagonizes fentanyl’s analgesic effect [19].
Severe and unpredictable potentiation by concomitant monoamine oxidase inhibitors (MAOIs) may occur with treatment, and fentanyl buccal soluble film is contraindicated [19] or not recommended [8] in patients who have recently received MAOIs. Caution is recommended when coadministering fentanyl buccal soluble film with drugs affecting the serotonergic neurotransmitter system, as there is a risk of serotonin syndrome [19]. When administered concomitantly with other CNS depressants, fentanyl buccal soluble film may cause increased depressant effects, such as hypoventilation, hypotension and profound sedation [8, 19]. Opioids, including fentanyl, are associated with impaired mental and/or physical ability to operate heavy machinery; they may also obscure the clinical course of a patient with head injury [8, 19].
3 Pharmacokinetic Properties of Fentanyl Buccal Soluble Film
The fentanyl buccal soluble film exhibits linear, dose-proportional pharmacokinetics over a dose range of 200–1200 μg [8, 19, 20] and has an absolute bioavailability of 71 % [8, 19, 21], which is approximately twice that of oral fentanyl (35 %) [21]. Absorption occurs in two stages: initial, rapid absorption via the buccal mucosa (51 % of the total dose), followed by slower absorption of swallowed fentanyl via the gastrointestinal tract [8, 19, 21]. Approximately 20 % of the total dose becomes systemically available through this slower route, escaping hepatic and intestinal first-pass elimination [8, 19]. If chewed and swallowed, fentanyl buccal soluble film would likely be associated with lower fentanyl peak concentrations (Cmax) and lower bioavailability than when applied to the buccal mucosa [8, 19].
Fentanyl buccal soluble film is associated with high inter-individual and low intra-individual variability in fentanyl absorption (demonstrating a need for individual dose titration), but a predictable dose-to-dose exposure once the optimal dose is determined [22]. The time to fentanyl Cmax ranges from 45 to 240 min, with a median of 60 min [19]. Multiple doses 1 h apart were associated with a proportional increase in fentanyl exposure [23].
In healthy volunteers, fentanyl buccal soluble film and oral transmucosal fentanyl citrate were not bioequivalent in terms of Cmax and area under the concentration–time curve from time zero to infinity (AUC∞) values, based on the established 90 % confidence interval acceptance range of 0.8–1.25 [24]. Fentanyl buccal soluble film was associated with 65 % higher fentanyl Cmax and 41 % higher AUC∞ values than oral transmucosal fentanyl citrate [24]. The US prescribing information contains a boxed warning regarding the differences in the extent of fentanyl absorption with different formulations and products, and states that fentanyl buccal soluble film should not be administered at the same μg dose as previously administered fentanyl products [8].
The application of fentanyl buccal soluble film 200 μg at an active mucositis site (grade 1) was associated with decreased fentanyl exposure compared with matched controls in an open-label, single-dose study in opioid-naïve cancer patients [8, 19, 25]. This decrease is not likely to be clinically relevant as the difference in fentanyl Cmax was less than the inter-individual variability, and dose adjustment is not required in the USA [8]; however, close monitoring of patients with grade 1 mucositis is recommended in the UK, and dose adjustment may be considered [19].
Fentanyl is highly lipophilic; according to animal studies, there is an initial rapid distribution of the drug to the brain, heart, lungs, kidneys and spleen and a slower redistribution to muscles and fat [8, 19]. A total of 80–85 % of absorbed fentanyl becomes plasma protein bound, mostly to alpha-1-acid glycoprotein, but also to albumin and lipoproteins. Acidosis induces an increase in the free fraction of fentanyl. At steady state, the mean volume of distribution is 4 L/kg [8, 19].
Fentanyl is metabolized mainly by cytochrome P450 (CYP) 3A4 to norfentanyl in the liver and intestinal mucosa; norfentanyl is not pharmacologically active, according to animal studies [8, 19]. More than 90 % of fentanyl undergoes biotransformation to N-dealkylated and hydroxylated inactive metabolites [8, 19].
Of an administered dose of fentanyl, <7 and ≈1 % is excreted unchanged in urine and feces, respectively [8, 19]. The metabolites are also mostly excreted in urine. Fentanyl has a total plasma clearance of 0.5 L/h/kg [8, 19], a clinically relevant half-life of ≈7 h [19], and a terminal elimination half-life of ≈14 h [8, 19].
There are limited pharmacokinetic data available regarding the use of fentanyl buccal soluble film in patients with renal or hepatic impairment; however, as fentanyl undergoes hepatic metabolism and renal excretion, fentanyl buccal soluble film should be used with caution in these patients, particularly those with moderate [19] or severe [8, 19] impairment.
The US prescribing information contains a boxed warning regarding the potentially increased fentanyl concentration when fentanyl buccal soluble film is coadministered with CYP3A4 inhibitors (e.g. macrolides, azole antifungals, certain protease inhibitors, calcium channel blockers, anti-emetic drugs, antidepressants, antacids), as this may increase depressant effects, potentially leading to fatal respiratory depression (Sect. 5); monitoring is recommended [8, 19]. Conversely, coadministration of fentanyl buccal soluble film with CYP3A4 inducers (e.g. barbiturates, anti-epileptic drugs, anti-inflammatory or immunosuppressant drugs, antidiabetic drugs, certain antibiotics, psychotropic drugs, certain antiviral drugs) may decrease the concentration of fentanyl; monitoring and potential dose adjustment are recommended [8, 19].
4 Therapeutic Efficacy of Fentanyl Buccal Soluble Film
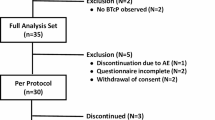
The efficacy of fentanyl buccal soluble film in adult patients with breakthrough cancer pain (receiving a stable opioid regimen for persistent pain associated with cancer or cancer treatment) was evaluated in a randomized, double-blind, placebo-controlled, crossover, multicentre, phase III study [26]. Breakthrough pain was defined as moderate to severe pain occurring at a specific site for a transitory period. Eligible patients had one to four breakthrough pain episodes per day requiring opioids for pain control, that were at least partially relieved by these opioids. Patients with rapidly escalating pain that the investigator believed may require increased background opioid treatment were excluded from the study. The opioid dosage regimen for persistent pain was required to be equivalent to 60–1000 mg/day of oral morphine or 50–300 μg/h of transdermal fentanyl [26].
Following a screening period of ≤1 week, 151 patients entered a ≤2-week, open-label titration period, during which they determined their minimum effective dose of fentanyl buccal soluble film (doses ranged from 200 to 1200 μg; the dose was increased once during each pain episode, until adequate pain relief was achieved) [26]. The 82 patients who achieved adequate pain relief for at least two pain episodes with the identified dose entered the ≤2-week double-blind period, during which they received ≤9 doses of study drug (one dose per episode; ≤6 doses of fentanyl buccal soluble film at the previously determined effective dose and ≤3 doses of placebo) in a randomized order. Rescue medication was permitted. A second dose of study drug was not permitted for 4 h; any subsequent dose was classified as being for a new pain episode, rather than an unresolved previous episode [26].
The primary endpoint was the mean time-weighted sum of pain intensity differences from baseline (SPID; summarizes treatment response over a clinically relevant period) at 30 min (SPID30) score in the modified intent-to-treat (mITT) population (n = 80) [26]. Pain intensity was measured on an 11-point scale [ranging from 0 (no pain) to 10 (worst pain)].
Baseline characteristics did not significantly differ between patients who participated in the titration period and those in the mITT population [26]. In the patients who participated in the titration period, the most common cancers were breast (23 %), lung (17 %), colorectal (11 %), gastroesophageal (7 %), pancreatic (6 %), and head and neck (5 %); approximately half of patients had somatic and/or visceral pain (both persistent and breakthrough), and a third also had neuropathic pain. Breakthrough pain was related to direct tumour involvement in 86 % of patients and to somatic/visceral lesions in 85 % of patients. A total of 56 % of patients had received chemotherapy and 25 % radiotherapy in the past 6 months. The most common opioid treatments for persistent pain were transdermal fentanyl (46 % of patients) and long-acting oral morphine (24 %) [26].
During the double-blind period, patients received a mean of 5.5 doses of fentanyl buccal soluble film and 2.8 doses of placebo; 5 % of patients received a fentanyl buccal soluble film dose of 200 µg, 19 % a dose of 400 µg, 28 % a dose of 600 µg, 24 % a dose of 800 µg, and 25 % a dose of 1200 µg [26].
The mean pain intensity score at the baseline of each pain episode was 6.9 for both fentanyl buccal soluble film- (n = 394) and placebo-treated episodes (n = 197) [26].
Fentanyl buccal soluble film was significantly more effective than placebo in treating breakthrough cancer pain in patients receiving opioids for persistent pain, with regard to SPID30 scores (primary endpoint; Fig. 1) [26]. The between-treatment difference in SPID scores reached statistical significance at 15 min post-dose (p < 0.05), and remained significant through 60 min post-dose (p < 0.001).
Mean SPID30 scores (primary endpoint) with fentanyl buccal soluble film (394 episodes) versus placebo (197 episodes) in a phase III crossover trial in patients with breakthrough cancer pain (n = 80) [26]. SPID30 time-weighted sum of pain intensity differences from baseline at 30 min post-dose. *p = 0.004 vs. placebo
Pain intensity differences from baseline were also significantly greater with fentanyl buccal soluble film than with placebo from 30 (p < 0.05) through 60 min (p < 0.001) post-dose [26]. Moreover, from 30 min post-dose, significantly more episodes treated with fentanyl buccal soluble film than placebo resulted in pain-intensity score improvements of ≥33 and ≥50 % (Fig. 2). Consistent with these findings, pain relief was significantly (p < 0.01) greater with fentanyl buccal soluble film than with placebo from 30 through 60 min post-dose.
Percentage of breakthrough pain episodes with a ≥33 or b ≥50 % reduction in pain-intensity scores at various time points post-dose of fentanyl buccal soluble film (394 episodes) versus placebo (197 episodes) in a phase III crossover trial in patients with breakthrough cancer pain (n = 80) [26]. *p < 0.01, **p < 0.001 vs. placebo
Overall, patients were more satisfied with fentanyl buccal soluble film than with placebo, based on a five-point scale (mean score 2.0 vs. 1.5; p < 0.001), and the mean percentage of episodes where patients required rescue medication was lower with fentanyl buccal soluble film than with placebo (30.0 vs. 44.6 %; p = 0.002) [26].
5 Tolerability of Fentanyl Buccal Soluble Film
Fentanyl buccal soluble film was generally well tolerated in clinical trials [8, 26, 27]. The most common adverse events that occurred with fentanyl buccal soluble film treatment in a pooled analysis of the randomized, placebo-controlled, phase III trial and a noncomparative, long-term trial were typical for opioid treatment in cancer patients, and included nausea, vomiting, dehydration, asthenia, dyspnoea, fatigue, dizziness and constipation (Fig. 3) [8]. By dose of fentanyl buccal soluble film, the most common adverse events were decreased weight (13 % of patients) with 200 μg; nausea (10 %), asthenia (10 %) and fatigue (10 %) with 400 μg; nausea (10 %) and vomiting (11 %) with 600 μg; nausea (13 %) and headache (10 %) with 800 μg; and nausea (32 %), vomiting (28 %), diarrhoea (12 %), dehydration (12 %) and dizziness (12 %) with 1200 μg [8].
Adverse events occurring in ≥10 % of recipients of fentanyl buccal soluble film 200 to >1200 μg during long-term treatment in a pooled analysis of clinical trials in opioid-tolerant patients with breakthrough cancer pain (n = 213) [8]
In the randomized, placebo-controlled, phase III trial, 15 % of the 151 patients in the safety population experienced 29 serious adverse events and four patients died during the study (mean duration of study-drug exposure of 10.1 days); no serious adverse events or deaths were considered to be drug related [26]. A total of 14 % of patients discontinued treatment as a result of 9 serious and 12 non-serious adverse events; nausea and vomiting were the most common adverse events leading to discontinuation (both 3 % of patients). A total of 50 % of 151 patients and 42 % of 81 patients experienced at least one treatment-emergent adverse event during the titration period and the double-blind period, respectively. Most (78 %) of the adverse events were not considered to be drug related (25 % of 151 patients had 56 drug-related adverse events). The most common drug-related adverse events (>5 % of patients) were somnolence (6 %) and nausea (5 %). No oral adverse events were considered to be related to study drug [26].
In a noncomparative, long-term study in patients with breakthrough cancer pain who were on a stable opioid regimen for persistent pain, 89 % of 243 recipients of fentanyl buccal soluble film 200–1200 μg up to 4 times daily reported at least one non-serious adverse event, and 50 % reported at least one serious adverse event, over an average of 126 days [27]. The most common serious adverse events (≥5 % of patients) were disease progression (11 %) and pneumonia (7 %). The most common non-serious adverse events (≥10 % of patients) were nausea (30 %), vomiting (21 %), dizziness (15 %), anaemia (13 %), disease progression (12 %), peripheral oedema (12 %), dehydration (12 %), dyspnoea (12 %), constipation (11 %), asthenia (10 %), fatigue (10 %) and pyrexia (10 %) [27].
There is a boxed warning in the US prescribing information regarding the risk of respiratory depression with fentanyl buccal soluble film [8]. Use of opioid μ-receptor agonists, including fentanyl, is associated with an increased risk of life-threatening respiratory depression; this is more likely to occur in patients with underlying respiratory disorders, patients receiving concomitant CYP3A4 inhibitors, and in elderly or debilitated patients [8, 19]. It usually occurs following large doses of opioids in opioid non-tolerant patients or after concomitant treatment with opioids and other drugs associated with depressed respiration. As a result of this risk, fentanyl buccal soluble film is contraindicated in the USA [8] and UK [19] in the management of acute or postoperative pain and in opioid non-tolerant patients, and in the UK in patients with severe obstructive lung conditions [19]. Caution is recommended in the USA and UK in patients with non-severe chronic obstructive pulmonary disease or other relevant pre-existing medical conditions [8, 19]. No patients experienced respiratory depression in the randomized, placebo-controlled, phase III trial [26].
The US prescribing information also carries a boxed warning regarding the abuse potential of fentanyl buccal soluble film [8]. It is a Schedule II controlled substance [8], and carries a risk of misuse, abuse, addiction and overdose-related adverse events (e.g. hypoventilation) [8, 19]; it is thus only available to outpatients through enrolment in a restricted program (inpatients are not required to enroll) in the USA [8].
As intravenous fentanyl has been associated with bradycardia, fentanyl buccal soluble film should be used with caution in patients with bradyarrhythmias [8, 19].
6 Dosage and Administration of Fentanyl Buccal Soluble Film
Fentanyl buccal soluble film is indicated in the USA and EU for the management of breakthrough pain in adult (aged ≥18 years [8]) cancer patients who are already receiving (and are tolerant to [8]) maintenance opioid therapy for underlying persistent cancer pain [8, 19]. Maintenance opioid therapy includes oral morphine ≥60 mg/day [8, 19], transdermal fentanyl ≥25 μg/h [8, 19], oral oxycodone 30 mg/day [8, 19], oral hydromorphone 8 mg/day [8, 19], oral oxymorphone 25 mg/day [8], or an equianalgesic dosage of another opioid [8, 19], for at least 1 week.
Dosage should be titrated to find an effective dose with manageable tolerability [8, 19]. The first breakthrough pain episode should be treated with 200 μg, applied to the inside of the cheek; if adequate pain relief is not achieved, subsequent pain episodes should be treated with 400, 600, 800 and 1200 μg, in that order, until adequate pain relief is achieved, after which patients should receive the same dose for following pain episodes [8, 19]. Single doses should be separated by at least 2 h in the USA [8] or 4 h in the UK [19], and fentanyl buccal soluble film should only be used once per episode and no more than 4 times per day [8, 19]. Rescue medication (as directed by a physician) is permitted after 30 min if required [8, 19]. Patients switching from another oral transmucosal fentanyl product should not receive a fentanyl buccal soluble film dose equal to that of the prior product, as the film formulation is not equivalent to any other fentanyl product on a μg to μg basis (Sect. 3) [8, 19].
Local prescribing information should be consulted for further, detailed information, including contraindications, precautions, drug interactions, and use in special patient populations.
7 Current Status of Fentanyl Buccal Soluble Film in Breakthrough Cancer Pain
Fentanyl buccal soluble film is approved in several countries worldwide, including the USA and the EU, for the management of breakthrough cancer pain in opioid-tolerant, adult patients with cancer [8, 19]. It is one of several immediate-release fentanyl formulations available for this indication; selection of which formulation to use is generally dependent on individual patient characteristics, likelihood of adherence, patient preference, and formulation-specific parameters (e.g. adverse events or convenience of administration), as there is a lack of head-to-head efficacy comparisons between these formulations [4]. Transmucosal formulations of fentanyl reduce the variable absorption observed with oral opioids [26].
Fentanyl buccal soluble film provides an additional option for transmucosal delivery of fentanyl, with approximately half of the dose undergoing an initial, rapid absorption via the buccal mucosa (accounting for its high bioavailability). In clinical trials, the drug was associated with significant improvements in pain intensity scores and was generally well tolerated in opioid-tolerant patients with breakthrough cancer pain. The most common adverse events were typical opioid-associated adverse events, such as nausea and vomiting. Fentanyl buccal soluble film is a useful option for the treatment of breakthrough cancer pain in opioid-tolerant patients.
Data selection sources:
Relevant medical literature (including published and unpublished data) on fentanyl buccal soluble film was identified by searching databases including MEDLINE (from 1946), PubMed (from 1946) and EMBASE (from 1996) [searches last updated 26 February 2016], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Fentanyl buccal soluble film, FBSF, Onsolis, Breakyl, Painkyl, cancer.
Study selection: Studies in opioid-tolerant adult patients with breakthrough cancer pain who received fentanyl buccal soluble film. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Chang A, Roeland EJ, Atayee RS, et al. Transmucosal immediate-release fentanyl for breakthrough cancer pain: opportunities and challenges for use in palliative care. J Pain Palliat Care Pharmacother. 2015;29(3):247–60.
Lötsch J, Walter C, Parnham M, et al. Pharmacokinetics of non-intravenous formulations of fentanyl. Clin Pharmacokinet. 2013;52(1):23–36.
Zeppetella G. Evidence-based treatment of cancer-related breakthrough pain with opioids. J Natl Compr Canc Netw. 2013;11(Suppl. 1):S37–43.
Smith HS. Considerations in selecting rapid-onset opioids for the management of breakthrough pain. J Pain Res. 2013;6:189–200.
Zeppetella G, Davies A, Eijgelshoven I, et al. A network meta-analysis of the efficacy of opioid analgesics for the management of breakthrough cancer pain episodes. J Pain Symptom Manage. 2014;47(4):772–85.e5.
Ripamonti CI, Santini D, Maranzano E, et al. Management of cancer pain: ESMO clinical practice guidelines. Ann Oncol. 2012;23(Suppl. 7):vii139–vii54.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: adult cancer pain (v1.2016). 2016. http://www.nccn.org. Accessed 2 Mar 2016.
Meda Pharmaceuticals. Onsolis® (fentanyl buccal soluble film): US prescribing information. 2011. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/022266s000lbl.pdf. Accessed 2 Mar 2016.
US FDA. FDA approves opioid pain reliever with required risk reduction plan [media release]. http://www.fda.gov. Accessed 16 Jul 2009.
BioDelivery Sciences International. Onsolis relaunch postponed pending product modification [media release]. http://www.bdsi.com. Accessed 12 Mar 2012.
BioDelivery Sciences International. BioDelivery Sciences announces FDA approval of new formulation of Onsolis® (fentanyl buccal soluble film) CII [media release]. http://www.bdsi.com. Accessed 13 Aug 2015.
Jeal W, Benfield P. Transdermal fentanyl. A review of its pharmacological properties and therapeutic efficacy in pain control. Drugs. 1997;53(1):109–38.
Muijsers RB, Wagstaff AJ. Transdermal fentanyl: an updated review of its pharmacological properties and therapeutic efficacy in chronic cancer pain control. Drugs. 2001;61(15):2289–307.
Blick SK, Wagstaff AJ. Fentanyl buccal tablet: in breakthrough pain in opioid-tolerant patients with cancer. Drugs. 2006;66(18):2387–93.
Hair PI, Keating GM, McKeage K. Transdermal matrix fentanyl membrane patch (matrifen): in severe cancer-related chronic pain. Drugs. 2008;68(14):2001–9.
Hoy SM, Keating GM. Fentanyl transdermal matrix patch (Durotep MT patch; Durogesic DTrans; Durogesic SMAT): in adults with cancer-related pain. Drugs. 2008;68(12):1711–21.
Chwieduk CM, McKeage K. Fentanyl sublingual: in breakthrough pain in opioid-tolerant adults with cancer. Drugs. 2010;70(17):2281–8.
Lyseng-Williamson KA. Fentanyl pectin nasal spray: in breakthrough pain in opioid-tolerant adults with cancer. CNS Drugs. 2011;25(6):511–22.
Meda Pharmaceuticals. Breakyl® (fentanyl buccal soluble film): UK summary of product characteristics. 2015. https://www.medicines.org.uk/emc. Accessed 2 Mar 2016.
Finn AL, Vasisht N, Stark JG. Dose proportionality and pharmacokinetics of fentanyl buccal soluble film in healthy subjects: a phase I, open-label, three-period, crossover study. Clin Drug Investig. 2012;32(1):63–71.
Vasisht N, Gever LN, Tagarro I. Single-dose pharmacokinetics of fentanyl buccal soluble film. Pain Med. 2010;11:1017–23.
Davies A, Finn A, Tagarro I. Intra- and interindividual variabilities in pharmacokinetics of the fentanyl buccal soluble film in healthy subjects: a cross-study analysis. Clin Drug Investig. 2011;31:317–24.
Vasisht N, Gever LN, Tagarro I, et al. Evaluation of the single- and multiple-dose pharmacokinetics of fentanyl buccal soluble film in normal healthy volunteers. J Clin Pharmacol. 2010;50(7):785–91.
Vasisht N, Gever LN, Tagarro I. Formulation selection and pharmacokinetic comparison of fentanyl buccal soluble film with oral transmucosal fentanyl citrate: a randomized, open-label, single-dose, crossover study. Clin Drug Investig. 2009;29(10):647–54.
Finn AL, Hill WC, Tagarro I, et al. Absorption and tolerability of fentanyl buccal soluble film (FBSF) in patients with cancer in the presence of oral mucositis. J Pain Res. 2011;4:245–51.
Rauck R, North J, Gever LN, et al. Fentanyl buccal soluble film (FBSF) for breakthrough pain in patients with cancer: a randomized, double-blind, placebo-controlled study. Ann Oncol. 2010;21(6):1308–14.
BioDelivery Sciences International. Study of the safety of BEMA™ fentanyl use for breakthrough pain in cancer subjects on chronic opioid therapy [NCT00293020]. 2012. http://www.clinicaltrials.gov. Accessed 2 Mar 2016.
Acknowledgments
During the peer review process, the manufacturer of fentanyl buccal soluble film was also offered an opportunity to review this article. Any changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflicts of interest
Karly P. Garnock-Jones is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
The manuscript was reviewed by: D. L. Anghelescu, Division of Anesthesia, St. Jude Children’s Research Hospital, Memphis, TN, USA; D. Taylor, Comprehensive Pain Care, P.C., Marietta, GA, USA.
Rights and permissions
About this article
Cite this article
Garnock-Jones, K.P. Fentanyl Buccal Soluble Film: A Review in Breakthrough Cancer Pain. Clin Drug Investig 36, 413–419 (2016). https://doi.org/10.1007/s40261-016-0394-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-016-0394-y