Abstract
Background
Cirrhotic patients admitted to the intensive care unit (ICU) usually have multi-organ failure. Multiple organ failure entails a very poor outcome in all intensive care patients. Cirrhotic patients show high morbidity and mortality rates compared with other critically ill patients. Severity scores have been developed for cirrhotic patients admitted to ICU. The main aim of this study was to determine whether lactate level gives any predictive value for mortality in cirrhotic elderly patients admitted to the ICU.
Methods
In all the patients enrolled, a diagnosis of cirrhosis was confirmed either histologically or by resorting to clinical, laboratory, and ultrasonographic findings. During this period, patients with cirrhosis were admitted to the ICU with varying indications. Child-Turcotte-Pugh (CTP), Model for End-stage Liver Disease (MELD), Acute Physiology and Chronic Health Evaluation (APACHE II) and Sequential Organ Failure Assessment (SOFA) scores and lactate were compared between deceased and discharged patients.
Results
A total of 90 consenting patients were enrolled in this study. The mean age of all the patients was 69 ± 5.919. We detected etiological factors for cirrhosis as HBV, HCV, alcohol, and cryptogenic cirrhosis. Hepatorenal syndrome and spontaneous bacterial peritonitis were significantly higher in patients who died than in those who were discharged from the ICU (p values were 0.01 and 0.028, respectively). Lactate level, CTP, APACHE II, MELD and SOFA scores were significantly higher in patients who died than in those who were discharged from the ICU (p values were 0.002, < 0.001, < 0.001, and < 0.001, respectively).
Conclusions
Many factors may be useful as a predictor of mortality in ICU in elderly patients with cirrhosis. In terms of prognostic value, the lactate level and APACHE II score are the two best predictive factors in cirrhotic elderly patients admitted to the ICU.
Zusammenfassung
Grundlagen
An eine Intensivstation (ICU) zugewiesene Patienten mit Leberzirrhose haben meistens ein Multiorganversagen, was bei allen Intensivpatienten mit einem schlechten Outcome verknüpft ist. Es wurden Schweregrad-Skalen für an die ICU zugewiesene Leberzirrhose Patienten entwickelt. Ziel dieser Stuide war es, zu prüfen, ob Laktatspiegel auch einen prädiktiven Wert hinsichtlich Mortalität bei älteren zirrhotischen Patienten haben.
Methodik
Die Diagnose einer Zirrhose war bei allen in die Studie aufgenommenen Patienten entweder histologisch oder durch die Kombination typischer klinischer, ultrasonographischer und Laborergebnisse gesichert. Die Zuweisung der Patienten an die ICU erfolgte aus verschiedenen Indikationen. Folgende Scores wurden bei den entlassenen beziehungsweise verstorbenen Patienten mit den Laktatwerten verglichen: Child-Turcotte-Pugh (CTP), Model for End-stage Liver Disease (MELD), Acute Physiology und Chronic Health Evaluation (APACHE II) und das Sequential Organ Failure Assessment (SOFA).
Ergebnisse
Insgesamt wurden 90 Patienten in die Studie aufgenommen (mittleres Alter 69 ± 5.919), wobei die Ätiologie der Leberzirrhose entweder HBV, HCV, Alkohol oder kryptogen war. Ein hepatorenales Syndrom und eine spontane bakterielle Peritonitis waren bei den verstorbenen Patienten signifikant häufiger als bei den von der ICU entlassenen Patienten (p 0,01 respektive 0,028). Die Laktatspiegel, sowie die Scorewerte von CTP, APACHE II, MELD und SOFA waren bei den verstorbenen signifikant höher als bei den von der ICU entlassenen Patienten (p 0,002, beziehungsweise < 0,001, < 0,001 und < 0,001).
Schlussfolgerungen
Viele Faktoren haben einen guten Voraussagewert bezüglich Mortalität an der ICU von älteren Patienten mit Leberzirrhose. Die Laktatspiegel und der APACHE II Score sind unserer Erfahrung nach aber die diesbezüglich besten.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cirrhotic patients admitted to the intensive care unit (ICU) generally have multi-organ failure. Multiple organ failure entails a very poor outcome in all intensive care patients [1, 2]. Patients with cirrhosis have a poor prognosis, especially when they develop complications [3, 4]. The prognosis of cirrhotic patients admitted to the ICU is grave. Cirrhotic patients who need critical care support show high morbidity and mortality rates compared with other critically ill patients. The use of prognostic models for patients admitted to ICU is of great importance, since they provide an objective evaluation for a group of patients with potentially high mortality rates and cost. The advanced stage of liver failure and the presence of cirrhotic complications contribute to the poor prognosis of cirrhotic patients admitted to the ICU. Clinicians and investigators have been persistently looking for objective scoring systems capable of providing accurate information on disease severity and prognosis. Risk stratification helps differentiate patients who would not benefit from admission to the ICU from those who could achieve better outcomes once aggressively treated.
Severity scores have been developed for cirrhotic patients admitted to ICU based on combinations of prognostic indicators. Of the models in use, the Child-Turcotte-Pugh (CTP) and Model for End-stage Liver Disease (MELD) scores have been designed exclusively for patients with liver disease, while the Acute Physiology and Chronic Health Evaluation (APACHE II) and Sequential Organ Failure Assessment (SOFA) scores are valid for use in different patient groups admitted to the ICU [5, 6].
Previous studies demonstrated that lactate levels were associated with a poor outcome in non-cirrhotic patients but not yet in cirrhotic patients. The aim of this study was to determine lactate level, APACHE II, MELD, CTP and SOFA scores any predictive value for mortality in cirrhotic elderly patients admitted to the ICU.
Patients and methods
This study was undertaken in the medical ICU department of our hospital between 2009 and 2011 with the approval of the local ethics committee. Informed consent was obtained from lucid patients or from the next of kin of incapacitated patients. Elderly patient has been defined as a chronological age of 65 years old or older. Patients aged below 65 and patients with a diagnosis other than cirrhosis were excluded from the present study. In all of the patients enrolled, a diagnosis of cirrhosis was confirmed either histologically or by resorting to clinical, laboratory, and ultrasonographic findings. During this period, patients with cirrhosis were admitted to the ICU with varying indications (hepatorenal syndrome, spontaneous bacterial peritonitis, hepatic coma, esophageal varices bleeding). Hepatorenal syndrome (HRS) as defined in the joint meeting of American Association for Study of the Liver Disease [7]. The diagnosis of SBP was based upon criteria recommended by the International Ascites Club and published in 2000 [8]. The West Haven criteria were used in grading the encephalopathy [9].
Blood samples were obtained 24 h after admission into the ICU for the determination of blood urea nitrogen, creatine, total bilirubin, direct bilirubin, prothrombin time, albumin, and lactate. The plasma lactate concentration as determined on arterial blood samples by a blood gas analyzer (ABLTM700 analyzer, Denmark) according to the manufacturer’s instructions. Arterial blood samples were taken within 6 h of presentation and the blood gas analyzer routinely measured the plasma lactate concentration. In addition, the 24 h APACHE II, MELD, CTP, and SOFA score were calculated for each ICU patient. APACHE II, MELD, CTP, and SOFA score and lactate were compared between dead and discharged patients. Once again, age comparison was made between men and women, as well as between dead and discharged patients.
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 18 software (SPSS Inc., Chicago, IL, United States of America). Depending on the parameter involved, the Anova, Mann-Whitney U, and Chi-square tests were used. Results were given as mean ± standard deviation. A p value below 0.05 was considered statistically significant. The area under the Receiver Operating Characteristic curve (AUROC) was calculated for each of the prognostic models, which was used to determine the model with the most significant prognostic power.
Results
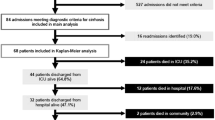
A total of 90 consenting patients were enrolled in this study, 52 (57.8 %) of which were men and 38 (42.2 %) were women. All of the patients with a mean age of 69 ± 5.919 were enrolled in the study. The mean age of patients who were discharged was 70.47 ± 6.562, compared to a mean age of 69.81 ± 4.915 in patients who died. Blood urea nitrogen, creatine, total bilirubin, direct bilirubin, protrombin time, and lactate levels were significantly higher in patients who died than in those who were discharged from the ICU. Albumin level was significantly lower in patients who died than in those who were discharged from the ICU (Table 1).
We detected etiological factors for cirrhosis as HBV, HCV, alcohol, and cryptogenic cirrhosis. We determined complications for cirrhosis as hepatic coma, esophageal varices bleeding, spontaneous bacterial peritonitis, hepatorenal syndrome, and hepatocellular carcinoma. Hepatorenal syndrome and spontaneous bacterial peritonitis were significantly higher in patients who died than in those who were discharged from the ICU (p values were 0.01 and 0.028 respectively). Lactate level, CTP, APACHE II, MELD, and SOFA scores were significantly higher in patients who died than in those who were discharged from the ICU (p values were 0.002, < 0.001, < 0.001, and < 0.001, respectively). There was no significant difference between the duration of cirrhosis in patients who died than in those who were discharged from the ICU. The duration of ICU admission and mechanical ventilation rates were statistically high in died patients compared to those who were discharged from ICU (p values were < 0.001 and 0.018, respectively; Table 2).
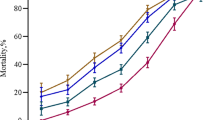
Cut-off values were ³ 2.75 mmol/L, ³ 16.5, ³ 5.5, ³ 19.5, and ³ 10.5 for lactate, APACHE II, SOFA, MELD, and CTP scores, respectively. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and area under the curve of each scoring system in predicting mortality was shown in Table 3 and Fig. 1.
Discussion
In this study, high APACHE II, MELD, SOFA, and CTP scores as well as increase of lactate were all found to be associated with a higher mortality rate in cirrhotic elderly patients in intensive care patients. This is the first study showing that lactate levels are predictors in cirrhotic elderly patients to ICU.
Results of our study have shown the APACHE II score to be the best prognostic model, among the scoring systems studied, at predicting prognosis in cirrhotic patients admitted to the ICU. The APACHE II score is the most commonly used predictor of mortality in intensive care patients. The validity of the APACHE II model in predicting prognosis in critical cirrhotic patients admitted to the ICU has been demonstrated in several studies [5, 10–19]. In a study by Chiavone et al. on 94 patients admitted following emergency who required intensive care, higher APACHE II scores were reported to be associated with higher mortality rates [16]. In a study by Ho et al. on 135 patients with complicated cirrhosis who required intensive care, higher CTP and APACHE II scores were both found to be correlated with increased mortality, the APACHE II score being of better prognostic value [10]. The studies by Cholongitas E et al. (312 cirrhotic patients admitted to the ICU)and Arabi et al. (129 cirrhotic patients admitted to the ICU), a statistically significant relationship between APACHE II score and prognosis was established in [15, 17]. In a study by Juneja et al. on 104 patients admitted to a speciality liver ICU in India, higher APACHE II is good prognostic model in predicting 30-day mortality [18]. Our study also demonstrated a link between high APACHE II scores and mortality.
The MELD score has been shown to be equivalent or even superior to the CTP score to estimate short-term survival among cirrhotic patients. MELD is a new liver-specific prognostic model, currently used to predict short-term survival in cirrhotics and to prioritize recipients for transplantation [20]. The MELD score includes parameters such as bilirubin, creatinine, and INR, making it more objective and easily reproducible [12, 21, 22]. Previous studies have demonstrated the accuracy of the MELD score in predicting prognosis [21, 23, 24]. Tu et al. demonstrated on 202 critically ill cirrhotic patients as a prognostic model, the MELD score was superior to the CTP and SOFA score [25]. Papeatheodoridis et al. and Sumskiene et al. also demonstrated that MELD score was better than CTP score at predicting short-term prognosis [26, 27]. Cholongitas et al. demonstrated that MELD scores showed high discrimination, almost the same as SOFA and superior to APACHE II [28]. Similarly, Botta et al. demonstrated that as a prognostic model, the MELD score was superior to the CTP score at predicting one-year survival in cirrhotic patients [21]. Our study showed link between high MELD scores and mortality but APACHE II score was superior to the MELD and CTP score.
The SOFA score is an excellent model which provides an easy to apply scoring system which may be used to provide objective information to patients and their relatives regarding the prognosis of the disease. SOFA is currently the most often used score for evaluation of multiple organ dysfunction. Its sequential use demonstrated optimal accuracy to predict mortality in several scenarios, including subgroups of cirrhotic patients [24, 29]. A lot of studies have demonstrated that the SOFA score is not only useful in grading organ dysfunction in cases with sepsis, trauma or after surgery, but that it is also the best prognostic indicator that could be used for cirrhotic patients [2, 11, 12, 18, 24, 30]. In a study on 160 patients with cirrhosis admitted to the ICU, Tsai et al. demonstrated that the SOFA score was better than the CTP score in predicting mortality as in our study [2]. An excellent discriminatory power to predict the short-term prognosis of 143 cirrhotic patients admitted to the ICU was demonstrated by Wehler et al. In this study, the overall predictive accuracy of the SOFA was greater than that of the APACHE II and CTP systems [31]. In a study by Cholongitas et al. on 128 patients admitted to ICU, SOFA score (baseline, at 48 h) had the best discriminative ability (higher AUC), compared to the other scores (APACHE II, CTP, MELD) and at 48 h had the best calibration ability [30]. In a study on 104 patients admitted to a specialty liver ICU, higher SOFA is good prognostic model in predicting 30-day mortality [18]. In a study by Juneja et al. on 104 patients admitted to a specialty liver ICU in India, higher APACHE II is good prognostic model in predicting 30-day mortality [18]. Chen et al. reported a mortality rate of 68.6 % among 102 cirrhotic patients admitted to the ICU. They also reported the SOFA score to be an excellent predictor of prognosis in comparison to the CTP score as in our study [32]. In another study, the superiority of SOFA in comparison with APACHE II or CTP scores in predicting short-term mortality in cirrhotic patients admitted to the ICU has also been shown by Cholongitas et al. [28]. Our study, the overall predictive accuracy of the SOFA was greater than that of the CTP systems but reported the APACHE II and MELD scores to be an excellent predictor of prognosis in comparison to the SOFA and CTP score.
CTP score indicates the severity of liver disease but were originally developed to assess the risk in undergoing surgical portacaval shunting and oesophageal transection, respectively, using bilirubin, prothrombin time, albumin, severity of ascites and hepatic encephalopathy. Child-Turcotte score has been used for more than two decades for determining prognosis in cirrhotic patients [33]. The prognostic value of the CTP score has been evaluated in several ICU studies, but it was found to be somewhat limited in patients with advanced liver dysfunction [28, 34]. The CTP scoring system has some subjective components but does not score factors such as cardiovascular, renal and pulmonary dysfunction, which may explain its low prognostic efficiency in patients with liver cirrhosis admitted in intensive care [1, 3, 24]. Despite involving numerous subjective parameters and its limited scope of definition, CTP is still the most commonly used scoring system in the determination of prognosis in cirrhotic patients. Some investigators (Botta et al., Ho et al. and Wehler et al.) have suggested that higher CTP scores and the presence of more complications were associated with higher mortality rates [4, 5, 6]. In addition, a metaanalysis on 118 studies show that higher CTP scores were associated with higher mortality rates [34]. Our study results show a link between a high CTP and mortality in ICU patients with cirrhosis.
Cellular metabolism under anaerobic conditions converts to lactate from pyruvate. Lactic acid levels relate to the oxygen debit corresponding to the extent of tissue hypoperfusion [35]. Hyperlactemia at the time of admission to the ICU has been proposed to be a potential marker for postoperative morbidity and mortality with a high sensitivity and specificity for adverse effects. The lactate level has been associated with mortality among patients admitted to the ICU in previous studies but not yet in cirrhotic patients. [36]. Plasma lactate levels are currently used in risk stratification of patients with sepsis, trauma and pulmonary embolism [37, 38, 39]. In a study by Noval-Padillo et al. on 16 patients, increased lactic acid that occurs is an early predictor of postoperative complications among heart transplant patients [40]. The other study by Hajjar et al. on 1,129 patients with cancer who required intensive care, higher lactate level was found to be correlated with increased mortality [41]. A study by Lee et al. on a total of 272 patients who were admitted to the emergency department with acute paraquat poisoning shows that the arterial lactate had similar discriminative power to the APACHE II system as in our study [42].
In conclusion, many factors may be useful as a predictor of mortality in ICU on elderly patients with cirrhosis. In terms of prognostic value, the lactate level and APACHE II score are superior to the SOFA, MELD and CTP scores.
References
Tsai MH, Chen YC, Ho YP, et al. Organ system failure scoring system can predict hospital mortality in critically ill cirrhotic patients. J Clin Gastroenterol. 2003;37(3):251–7.
Tsai MH, Peng YS, Lien JM, et al. Multiple organ system failure in critically ill cirrhotic patients. A comparison of two multiple organ dysfunction/failure scoring systems. Digestion 2004;69(3):190–200.
Shellman RG, Fulkerson WJ, DeLong E, et al. Prognosis of patients with cirrhosis and chronic liver disease admitted to the medical intensive care unit. Crit Care Med. 1988;16(7):671–8.
Cooper GS, Bellamy P, Dawson NV, et al. A prognostic model for patients with end-stage liver disease. Gastroenterology 1997;113(4):1278–88.
Cholongıtas E, Senzolo M, Patch D, et al. Review article: scoring systems for assessing prognosis in critically ill adult cirrhotics. Aliment Pharmacol Ther. 2004;24(3):453–64.
Zauner C, Schneeweiss B, Schneider B, et al. Short-term prognosis in critically ill patients with liver cirrhosis: an evaluation of a new scoring system. Eur J Gastroenterol Hepatol. 2000;12(5):517–22.
Salerno F, Gerbes A, Gines P, et al. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut 2007;56(9):1310–18.
Rimola A, Garcia-Tsao G, Navasa M, et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. International Ascites Club. J Hepatol. 2000;32(1):142–53.
Ferenci P, Lockwood A, Mullen K, et al. Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: Final report of the working party at the 11th World congresses of gastroenterology, Vienna, 1998. Hepatology 2002;35(3):716–21.
Ho YP, Chen YC, Yang C, et al. Outcome prediction for critically ill cirrhotic patients: a comparison of APACHE II and child-pugh scoring systems. J Intensive Care Med. 2004;19(2):105–10.
Wehler M, Kokoska J, Reulbach U, et al. Short-term prognosis in critically ill patients with cirrhosis assessed by prognostic scoring systems. Hepatology 2001;34(2):255–61.
Cholongıtas E, Senzolo M, Patch D, et al. Risk factors, Sequential organ failure assessment and model forend-stage liver disease scores for predicting short term mortality in cirrhotic patients admitted to intensive care unit. Aliment Pharmacol Ther. 2006;23(7):883–93.
Taş A, Köklü S, Beyazit Y, et al. Thyroid hormone levels predict mortality in intensive care patients with cirrhosis. Am J Med Sci. 2011 Dec 2. [Epub ahead of print]
Zauner CA, Apsner RC, Kranz A, et al. Outcome prediction for patients with cirrhosis of the liver in a medical ICU: a comparison of the APACHE scores and liver-specific scoring systems. Intensive Care Med. 1996;22(6):559–63.
Arabi Y, Ahmed QA, Haddad S, et al. Outcome predictors of cirrhosis patients admitted to the intensive care unit. Eur J Gastroenterol Hepatol. 2004;16(3):333–39.
Chiavone PA, Rasslan S. Influence of time elapsed from end of emergency surgery until admission to intensive care unit, on apache II prediction and patient mortality rate. Sao Paulo Med J. 2005;123(4):167–74.
Cholongitas E, Senzolo M, Patch D, et al. Cirrhotics admitted to intensive care unit: the impact of acute renal failure on mortality. Eur J Gastroenterol Hepatol. 2009;21(7):744–50.
Juneja D, Gopal PB, Kapoor D, et al. Outcome of patients with liver cirrhosis admitted to a specialty liver intensive care unit in India. J Crit Care. 2009;24(3):387–93.
Tas A, Tetiker T, Beyazit Y, et al. Thyroid hormone levels as a predictor of mortality in intensive care patients: a comparative prospective study. Wien Klin Wochenschr. 2012 Feb 15. [Epub ahead of print]
Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91–6.
Botta F, Giannini E, Romagnoli P, et al. MELD scoring system is useful for predicting prognosis in patients with liver cirrhosis and is correlated with residual liver function: a European study. Gut 2003;52(1):134–39.
Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology 2001;33(2):464–70.
Huo TI, Wu JC, Lin HC, et al. Evaluation of the increase in model for end-stage liver disease (DMELD) score over time as a prognostic predictor in patients with advanced cirrhosis: risk factor analysis and comparison with initial MELD and child--turcotte--pugh score. J Hepatol. 2005;42(6):826–32.
Filloux B, Chagneau-Derrode C, Ragot S, et al. Short-term and long-term vital outcomes of cirrhotic patients admitted to an intensive care unit. Eur J Gastroenterol Hepatol. 2010;22(12):1474–80.
Tu KH, Jenq CC, Tsai MH, et al. Outcome scoring systems for short-term prognosis in critically ill cirrhotic patients. Shock 2011;36(5):445–50.
Papatheodoridis GV, Cholongitas E, Dimitriadou E, et al. MELD vs child-pugh and creatinine-modified child-pugh score for predicting survival in patients with decompensated cirrhosis. World J Gastroenterol. 2005;11(20):3099–3104.
Sumskiene J, Kupcinskas L, Pundzius1 J, et al. Prognostic factors for short and long-term survival in patients selected for liver transplantation. Medicina 2005;41(1):39–46.
Cholangitas E, Senzolo M, Patch D, et al. Risk factors SOFA and MELD scores for predicting short term mortality in cirrhotics admitted to intensive care unit. Aliment Pharmacol Ther. 2006;23(7):883–93.
Rocco RJ, Soares M. Outcome of patients with cirrhosis admitted to intensive care unit. Rev Bras Intensiva. 2010;22(1):11–18.
Cholongitas E, Betrosian A, Senzolo M, et al. Prognostic models in cirrhotics admitted to intensive care units better predict outcome when assessed at 48 h after admission. J Gastroenterol Hepatol. 2008;23(8 Pt 1):1223–7.
Wehler M, Kokoska J, Reulbach U, et al. Short-term prognosis in critically ill patients with cirrhosis assessed by prognostic scoring systems. Hepatology 2001;34(2):255–61.
Chen YC, Tıan YC, Lıu NJ, et al. Pospective cohort study comparing sequential organ failure assessment and acute physiology, age, chronic health evaluation III scoring systems for hospital mortality prediction in critically ill cirrhotic patients. J Clin Pract. 2006;60(2):160–66.
Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646–9.
Aggarwall A, Ong JP, Younossi ZM, et al. Predictors of mortality and resource utilization in cirrhotic patients admitted to the medical ICU. Chest 2001;119(5):1489–97.
Ranucci M, De Toffol B, Isgro G, et al. Hyperlactatemia during cardiopulmonary bypass: determinants and Impact on postoperative outcome. Crit Care 2006;10(6):R167.
Hatherill M, Salie S, Waggie Z, et al. The lactate: pyruvate ratio following open cardiac surgery in children. Intensive Care Med. 2007;33(5): 822–9.
Shapiro NI, Trzeciak S, Hollander JE, et al. A prospective, multicenter derivation of a biomarker panel to assess risk of organ dysfunction, shock, and death in emergency department patients with suspected sepsis. Crit Care Med. 2009;37(1):96–104.
Vanni S, Socci F, Pepe G, et al. High plasma lactate levels are associated with increased risk of in-hospital mortality in patients with pulmonary embolism. Acad Emerg Med. 2011;18(8):830–5.
Guyette F, Suffoletto B, Castillo JL, et al. Prehospital serum lactate as a predictor of outcomes in trauma patients: a retrospective observational study. J Trauma. 2011;70(4):782–6.
Noval-Padillo JA, Serra-Gomez C, Gomez-Sosa L, et al. Changes of lactate levels during cardiopulmonary bypass in patients undergoing cardiac transplantation: possible early marker of morbidity and mortality. Transplant Proc. 2011;43(6):2249–50.
Hajjar LA, Nakamura RE, de Almeida JP, et al. Lactate and base deficit are predictors of mortality in critically ill patients with cancer. Clinics (Sao Paulo). 2011;66(12):2037–42.
Lee Y, Lee JH, Seong AJ, et al. Arterial lactate as a predictor of mortality in emergency department patients with paraquat intoxication. Clin Toxicol (Phila). 2012;50(1):52–6.
Conflict of interest
Authors declare no conflict of interest related to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tas, A., Akbal, E., Beyazit, Y. et al. Serum lactate level predict mortality in elderly patients with cirrhosis. Wien Klin Wochenschr 124, 520–525 (2012). https://doi.org/10.1007/s00508-012-0208-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-012-0208-z