Abstract
This study aimed to investigate the effect of inpatient vs outpatient spa therapy on pain, quality of life, and anxiety in elderly patients with generalized osteoarthritis. A total of 150 patients were randomized into three groups. Group I was given medical treatment, group II was treated as outpatients, and group III was treated as inpatient spa therapy. Assessments were made using the Pain (VAS), EQ-5D-3L Scale, and State and Trait Anxiety Inventory (STAI) at the beginning of treatment (W0), at the end of treatment (W2), and at the fourth week after treatment (W6). The comparison of outpatient spa group and etodolac treatment group showed that outpatient spa group was superior to etodolac treatment group in all evaluated parameters at W2 vs W0 and W6 vs W0. The comparison of inpatient spa group and etodolac treatment group showed that inpatient spa group was superior to etodolac treatment group in all evaluated parameters at W2 vs W0 and W6 vs W0. The comparison of inpatient spa group and outpatient spa group showed that inpatient spa group was superior to outpatient spa group in all evaluated parameters except STAI-TXII at W2 vs W0 and in all evaluated parameters W6 vs W0. Spa therapy, either as an outpatient or inpatient basis, may have a positive effect on pain, anxiety, and quality of life in geriatric patients with generalized osteoarthritis. The inpatient spa therapy may be more beneficial than outpatient spa therapy. When the side effects of drug treatments are emphasized, spa therapy may be considered as an interesting option for elderly with osteoarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Life expectancy has increased over the past decades as a result of developments in medicine and health services, along with improving social conditions, and this is leading to a rapid rise in the elderly population. Around 10% of the global population are people aged 65 years and above, and this ratio is expected to increase to 16% by 2050 (WHO 2015).
Chronic pain is a common condition that affects 20% of the world’s general population, accounting for 15–20% of all visits to the physician (Treede et al. 2015). Chronic pain may accompany psychiatric conditions, and vice versa psychiatric conditions may occur in association with chronic pain (Bair et al. 2008). Anxiety can also increase the probability of developing chronic pain. Generalized and undiagnosed anxiety disorders are found to be less common in the elderly than in young people, despite being among the most commonly encountered psychological problems in the geriatric population (Jeste et al. 2006).
One of the most common causes of chronic pain and disability in the world are musculoskeletal disorders, and among these, osteoarthritis (OA) is the most common disease affecting the joints and is characterized by a progressive degeneration of cartilage (Woolf and Pfleger 2003). The incidence of OA is known to increase with advancing age, with pain and the loss of function due to OA were reported in 25% of individuals aged above 65 years (Breedveld 2004). The main symptoms in patients with OA are pain and loss of function, which impair quality of life and increase mortality and morbidity rates.
There are many pharmacological and non-pharmacological approaches for the management of pain and musculoskeletal disorders (Fioravanti et al. 2017), although non-pharmacological methods are becoming increasingly important in the elderly due to the increasing number of chronic diseases that are known to increase with age. Spa therapy involves many medical applications, such as balneotherapy, mud therapy, exercise, and massage; the curing environment makes spas as an ideal environment for not only physical health but also mental health, by getting away from the stress and tiredness of daily life. They are not used only for the treatment of diseases, but also by many individuals who wish to live a healthy life and slow down aging.
In this study, we aimed to investigate the effect of inpatient vs outpatient spa therapy applied at cure center on pain, quality of life, and anxiety in elderly patients with generalized OA.
Methods
Study design
This prospective, randomized, controlled, and a single-blind study was conducted in the Bolu İzzet Baysal Physical Medicine and Rehabilitation Training and Research Hospital, Spa Center, after Ethical Committee approval.
Participants
A total of 224 patients aged 65 years and above with generalized OA involving three or more joint sites, who visited the outpatient clinic between March 2016 and September 2016, were evaluated for eligibility.
A general physical and musculoskeletal system examination of the patients was carried out by the investigating physician, and the diagnoses were confirmed by the necessary laboratory and imaging techniques.
The inclusion criteria were an age of 65 to 75 years with generalized OA and a pain associated with OA lasted for more than 3 months. The exclusion criteria were a diagnosis of the psychiatric problems, an inflammatory rheumatic disease, a previous surgical intervention due to OA (e.g., total replacement of the knee), an uncontrolled arterial hypertension and diabetes mellitus, a decompensated organ failure, treatment received for malignancy, a bleeding disease condition, an infectious disease with fever, a severe trauma or a surgical operation within the last 6 months, intra-articular injection received or symptomatic drugs used, of which effects were seen in long term, within the last 6 months, and physical therapy or spa therapy received in the previous year.
Randomization and blinding
A total of 150 patients who met the study criteria and who signed the informed consent forms were randomized into three groups through a block randomization in a 1:1:1 ratio using a digital random number generator. The randomization sequence was concealed from the physicians enrolling and assessing patients. The physician who assessed the patients was unaware of the patients’ treatment group. Statistical analyses of the study were carried out by a biostatistician who was also blind to the treatment of each group.
Interventions
All patients received an active treatment for a period of 2 weeks.
The patients in group I (etodolac treatment) (n = 50) received only medical therapy in the form of 300 mg of etodolac, twice a day for a period of 14 days.
The patients in group II (outpatient spa therapy) (n = 50) received 2 weeks of spa therapy as an outpatient basis, in a daily living environment; in other words, patients continued their daily routine during the therapy period. The patients in group III (inpatient spa treatment) (n = 50) received 2 weeks of spa therapy as an inpatient basis.
In the cure center, a mineral water bath (balneotherapy) was applied in the thermal pools to the outpatient spa therapy and inpatient spa therapy for 20 min, at a temperature of 38–40 °C. After resting for 30 min, a 10-min jet shower was applied, then 80 Hz of conventional transcutaneous electrical nerve stimulation and 45 °C local hot packs for 20 min were applied to the painful joints. The patients in group II and group III were advised not to use analgesic and nonsteroidal anti-inflammatory drugs during the study. The patients in group I were advised not to use analgesic and nonsteroidal anti-inflammatory drugs during the follow-up after 2 weeks of etodolac treatment period. Patients who used these drugs were excluded from the study.
The spa water has a total mineralization of 1744.367 mg/L and a source temperature of 42 °C (Table 1); therefore, it is classified in the “thermomineral waters” group in balneological terms.
Instruments
Evaluations were made before treatment (W0), at the end of treatment (W2), and at the fourth week after treatment (W6). The Visual Analog Scale-Pain (VAS), EQ-5D-3L Scale, and State and Trait Anxiety Inventory were used for the evaluation.
The VAS is commonly used for the determination of the degree of pain. It is recorded on a 100-mm horizontal line and the distance from the lowest VAS to the point marked by the patient is measured to determine the numerical value of the pain intensity felt by the patient (Gallagher et al. 2001). The pain was assessed as a whole in the all joints affected, as similarly performed in the Cuperus et al. (2015)’s trial. The question used for measuring the pain was “How much pain, in general, do you have in your joints?”
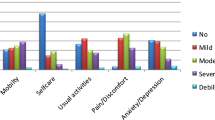
A three-level version of EQ-5D (EQ-5D-3L) was developed in 1990 by the European Quality of Life (EuroQol) group. EQ-5D-3L, the EQ-5D descriptor system, and the EQ-VAS consist of two pages. The EQ-5D contains five sub-dimensions (mobility, self-care, general activities, feelings of pain/discomfort, and anxiety/depression) within a three-level structure of “no problem, moderate problem, and advanced problem.” The scale describes 243 different health conditions, and an index score ranging from − 0.59 to 1 is calculated from the five dimensions of the scale. A score of 1 indicates perfect health, while the health state worsens with decreasing values. The EQ-VAS is marked on a 100-mm line to help individuals observe their health state. The best imaginable health condition score is 100, while 0 represents the worst health condition (EuroQolGroup 1990). In 2011, Turkish validity and reliability studies were conducted by Kahyaoglu Sut and Unsar (2011), and the approval for use in the present study was obtained from EuroQol.
The State and Trait Anxiety Inventory (STAI-TX1, STAI-TXII) was developed in 1970 by Spielberger et al. (Spielberger et al. 1970) and the scale was adapted for Turkish through validity and reliability studies by Öner and Compte (1998). The State Anxiety Inventory (STAI-TX1) identifies how an individual feels at a certain time and under certain conditions, whereas the Trait Anxiety Inventory (STAI-TXII) determines how an individual feels independent of the existing state and conditions, as a self-replenishing test. STAI-TX1 is a very sensitive tool for the assessment of excitatory reactions that show sudden changes. In STAI-TXII, it is usually aimed to measure the continuity of the anxiety to which the person has a tendency. Scores range from 20 to 80, with scores of 36 and below indicating an absence of anxiety, 37–42 indicating mild anxiety, and 43 points and above indicating high anxiety. Generally, a high state and trait anxiety score indicates high anxiety, and scores of 60 and above indicate that the individual requires professional help (Öner and Compte 1998).
All the questionnaires were self-reported by patients.
Efficacy outcome measures
The efficacy was defined as a change in outcome measures score at W2 vs W0 and at W6 vs W0.
Statistical analysis
Demographic and clinical characteristics, including frequency, the arithmetic mean, and standard deviations, were calculated using descriptive statistics. The Kruskal-Wallis test was used to compare continuous variables, and chi-squared test or the Fisher exact test was used to compare categorical variables between the groups at baseline. The efficacy analysis longitudinal data was performed using a repeated measure and generalized linear mixed model on an intention-to-treat basis. Time, group, sex, age, BMI, and interactions in general linear mixed model were used as covariates for each dependent variables. p values < 0.05 were considered statistically significant. Least square means were obtained for variables from each model. Multiple comparison adjustments for the p values were done using the Tukey-Kramer method. The fixed effects coefficient analysis was undertaken by using maximum likelihood method of estimation and spatial power covariance structures that time intervals were not equally spaced. To compute post hoc power for data, estimated parameter values and degree of freedoms from the generalized linear mixed model were used. The power for each model was found above 90%. The general linear model was used to compare groups at each time point after transformation data normalization. Data were analyzed by using SAS 9.4 software (SAS Institute Inc., Cary, NC); the procedures used were Proc Means, Proc Freq, Proc Npar1way, Proc Glimmix, and Proc Glm.
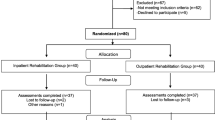
Results
The flow diagram of the study population is presented in Fig. 1. During the treatment and follow-up period, five patients in etodolac treatment group, six patients in outpatient spa therapy group, and one patient in inpatient spa therapy group did not complete the study due to knee trauma, gastrointestinal problems associated with etodolac, flu-like symptoms, and use of nonsteroidal anti-inflammatory drugs or discontinued to follow-up. Of the total, 45 patients in etodolac treatment group, 44 patients in outpatient spa therapy group, and 49 patients in inpatient spa therapy group completed the study (Fig. 1). In the analysis of groups at baseline, no statistically significant difference was identified in the sociodemographic characteristics of the patients among the groups (Table 2).
The comparison of outpatient spa group and etodolac treatment group showed that outpatient spa group was superior to etodolac treatment group in all evaluated parameters at W2 vs W0 and W6 vs W0. The comparison of inpatient spa group and etodolac treatment group showed that inpatient spa group was superior to etodolac treatment group in all evaluated parameters at W2 vs W0 and W6 vs W0. The comparison of inpatient spa group and outpatient spa group showed that inpatient spa group was superior to outpatient spa group in all evaluated parameters except STAI-TXII at W2 vs W0 and in all evaluated parameters W6 vs W0 (Table 3 and Fig. 2).
a Line chart representing changes in LSmeans of Pain (VAS) scores. b Line chart representing changes in LSmeans of EQ-5D scores. c Line chart representing changes in LSmeans of EQ-VAS scores. d Line chart representing changes in LSmeans of STAI-TX1 scores. e Line chart representing changes in LSmeans of STAI-TXII scores
Discussion
In the present study, we found that spa therapy, either as an outpatient or inpatient basis, may have had more positive effects on pain, quality of life, and anxiety than etodolac treatment in elderly patients with generalized OA. Furthermore, inpatient spa therapy may be more beneficial than outpatient spa therapy.
The results of the present controlled study extend the results of previous observational studies in elderly patients with OA (Gaal et al. 2008; Karagülle et al. 2016; Kardeş et al. 2018; Zwolińska et al. 2018). Gaal et al. (2008) prospectively investigated the effectiveness of balneotherapy—applied in a spa in a daily living environment, in other words, patients continued their daily routine during therapy period—in patients with knee or lumbar OA. Karaguülle et al. (2016) retrospectively tested the effectiveness of spa therapy, by journeying and staying at a spa resort and this led to changes in environmental and social milieu, in patients with a wide spectrum of OA subgroups including generalized OA. Kardeş et al. (2018) retrospectively investigated the effectiveness of balneological treatment (hydrotherapy and peloidotherapy), in a daily living environment, in patients with a wide range of OA subgroups including generalized OA. In the recent study with a 1-year follow-up, Zwolińska et al. (2018) prospectively tested the effectiveness of inpatient spa therapy in patients with generalized OA. These earlier studies, in general, demonstrated the beneficial effectiveness of spa therapy and balneological treatments and emphasized the need of a randomized controlled trial evaluating the efficacy of spa therapy/balneological treatments in patients with OA (Gaal et al. 2008; Karagülle et al. 2016; Kardeş et al. 2018; Zwolińska et al. 2018). Our study is the first randomized medical therapy controlled trial testing the efficacy of outpatient and inpatient spa therapies in patients with generalized OA, designed as a pilot study. Because this was the first controlled study, we could not anticipate the sample size as we had limited information about the estimated outcomes in each group. However, we calculated post hoc sample size, as similarly performed in Oosterveld et al. (2009)’s pilot study.
Old age is an inevitable process, although it is possible to stay healthy and maintain a good quality of life, and, in doing so, it reduces the social burden associated with the elderly population. Increasing one’s quality of life and developing strategies for healthy aging during old age are important ways of increasing social health. Due to physiological changes, increased comorbidity, and the use of multiple medications observed in the elderly, a special approach may be needed in the treatment. Health complementary and non-pharmacological treatment modalities are important in the management of chronic diseases when supported by Active and Healthy Aging (AHA) (Blain et al. 2016).
Diseases of the musculoskeletal system are a significant source of morbidity in geriatric patients. Elderly individuals with a chronic pain describe their health conditions as worse and are observed to use healthcare services more often than pain-free elderly individuals (Reyes-Gibby et al. 2002).
Pain can be classified into two types: nociceptive and neuropathic. Nociceptive pain occurs as a result of damage to tissue (Uyar and Köken 2017). Nociceptors are pain receptors in subcutaneous tissue like the skin, muscles, and joints. Information received is carried to the upper centers via spinal neurons. The anterior cingulate cortex (ACC) is associated with pain (Uyar and Köken 2017), and the central plasticity inhibition of ACC has been found to have an analgesic effect on chronic pain in the studies of animals (Zhuo 2014). Increased ACC activity has been detected in patients with anxiety problems (Koga et al. 2015; Zhuo 2014). Koga et al. (2015) demonstrated an interaction between anxiety and chronic pain in their study on the synaptic basis of long-term potentiation in ACC. Although the mechanism of action of balneotherapy is unclear (Fioravanti et al. 2017), Bender et al. (Bender et al. 2005) reported that nociception was destroyed through the activation of thermo- and mechanoreceptors under the influence of the temperature of water and its supporting force. Morer et al. (Morer et al. 2017), in a review of randomized controlled studies investigating the effects of chemical composition of waters used in balneotherapy, reported that mineral water or mud baths have more effect on pain reduction than non-mineralized water, although the mechanism is not fully understood. The present study demonstrates that anxiety decreases more in groups with a higher level of pain reduction, although it is largely an efficacy study rather than a study on the mechanism of action; this finding may be the evidence for a pain-anxiety interaction.
Many publications have shown that balneotherapy can provide a relief in such cases with OA-induced pain, physical function limitation, and restriction for daily life activities. In a meta-analysis conducted by Matsumoto et al. (2017), it was confirmed that balneotherapy reduced pain and joint stiffness and enhanced function in patients with OA. Karagülle et al. (2017), in their retrospective study of 819 patients, demonstrated that spa therapy was effective in the easing of pain and improving in function in patients with rheumatic and musculoskeletal diseases. Furthermore, Koyuncu et al. (2016), using the different treatment modalities in their study, demonstrated that the combined administration of balneotherapy and physical therapy had more positive effects on pain, disability, and quality of life than physical therapy treatment alone in patients with chronic neck pain. In another study, intermittent and consecutive treatments were carried out, and it was demonstrated that treatment modalities including hydrotherapy and peloidotherapy on outpatients were similarly effective when given in different periods (Ozkuk et al. 2017). In parallel to all the above, in this study involving geriatric patients with generalized OA, positive results were observed in pain levels and daily life activities in patients treated with spa therapy as an outpatient or inpatient.
Our study included both inpatient and outpatients, and so, the obtained results did evaluate not only the efficacy of spa interventions alone, but also the effect of environmental change or the cure milieu. There are different opinions in the literature regarding the treatment of inpatients and outpatients. Constant et al. (1995) reported that factors such as environmental change and moving away from environments that contribute to daily stress were positively associated with physical and mental health and mood swings. Nguyen et al. (1997) demonstrated that the withdrawal of a patient from an inhabited or working environment had a positive effect on the efficacy of treatment. In a meta-analysis conducted by Stolee et al. (2012), it was demonstrated that leaving one’s comfort zone to a distant place for treatment rather than receiving treatment as an inpatient was more effective in terms of functional and cognitive status, particularly in the elderly who suffers mostly from musculoskeletal diseases. Our study results suggest that elderly individuals may experience more positive results by leaving their environment for different environments. In our study, the reason for the more satisfactory results from the spa therapy in this group of patients may also be due to the psychological relief derived from inpatient spa therapy, in addition to the physical, mechanical, and chemical effects of the spa interventions.
Mood changes, such as depression and anxiety, have been reported to be more common in patients with chronic pain than in the normal population (Costa et al. 2015). Latore-Roman et al. (2015) found significant improvements in pain, mood, sleep quality, anxiety, and depression in geriatric patients who underwent balneotherapy, while Dubois et al. (2010) emphasized that balneotherapy might be an interesting way of treating generalized anxiety disorder, particularly in patients who do not tolerate or are reluctant to use pharmacotherapies. Several previous studies have consistently shown that spa therapy and balneotherapy are effective in reducing stress, anxiety, and depression in both in patients with anxiety/depressive disorder or healthy adults (Antonelli and Donelli 2018; Matzer et al. 2018; Naumann et al. 2017; Stier-Jarmer et al. 2016, 2017; Rapolienė et al. 2016). Our study would expand the anxiety-relieving effects of spa therapy to the elderly patients with generalized OA. Although we included geriatric OA patients with no history of psychiatric disease and with no reported mental health/emotional problems, high STAI values and low EQ-VAS values were identified during the performed tests. This suggests the possible presence of psychological problems in patients with chronic pain, even if they were not diagnosed. At the end of treatment, a significant improvement was noted in these values, particularly in the groups receiving spa therapy.
Limitations
The small sample size, the lack of long follow-up period and a placebo-control group, and the fact that no investigation was made for the other psychiatric diseases seen in geriatric age groups are the main limitations of the present study. Furthermore, the patients were aware of the treatment they received; therefore, the placebo effects caused by the belief in improvement by spa therapy and positive attention might certainly have contributed to the observed improvements (Karagülle et al. 2018a). However, in our study, blinding of the patients to the treatment allocation was not possible due to the complex nature of the spa therapy (Karagülle et al. 2018a, b).
Conclusion
The results of the study suggest that spa therapy, either as an outpatient or inpatient basis, may have a positive effect on pain, anxiety, and quality of life in geriatric patients with generalized osteoarthritis. The inpatient spa therapy may be more beneficial than outpatient spa therapy. When the side effects of drug treatments are emphasized, spa therapy may be considered as an interesting option for elderly with osteoarthritis.
References
Antonelli M, Donelli D (2018) Effects of balneotherapy and spa therapy on levels of cortisol as a stress biomarker: a systematic review. Int J Biometeorol 62:913–924
Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K (2008) Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med 70:890–897. https://doi.org/10.1097/PSY.0b013e318185c510
Bender T, Karagulle Z, Balint GP, Gutenbrunner C, Balint PV, Sukenik S (2005) Hydrotherapy, balneotherapy, and spa treatment in pain management. Rheumatol Int 25:220–224. https://doi.org/10.1007/s00296-004-0487-4
Blain H et al (2016) Combining balneotherapy and health promotion to promote active and healthy ageing: the Balaruc-MACVIA-LR ((R)) approach. Aging Clin Exp Res 28:1061–1065. https://doi.org/10.1007/s40520-016-0596-4
Breedveld FC (2004) Osteoarthritis--the impact of a serious disease. Rheumatology (Oxford, England) 43(Suppl 1):i4–i8. https://doi.org/10.1093/rheumatology/keh102
Constant F, Collin JF, Guillemin F, Boulange M (1995) Effectiveness of spa therapy in chronic low back pain: a randomized clinical trial. J Rheumatol 22:1315–1320
Costa EC, Vale S, Sobral M, Graca Pereira M (2015) Illness perceptions are the main predictors of depression and anxiety symptoms in patients with chronic pain. Psychol Health Med 21:1–13. https://doi.org/10.1080/13548506.2015.1109673
Cuperus N, Hoogeboom TJ, Kersten CC et al (2015) Randomized trial of the effectiveness of a non-pharmacological multidisciplinary face-to-face treatment program on daily function compared to a telephone-based treatment program in patients with generalized osteoarthritis. Osteoarthr Cartil 23:1267–1275
Dubois O et al (2010) Balneotherapy versus paroxetine in the treatment of generalized anxiety disorder. Complementary therapies in medicine 18:1–7. https://doi.org/10.1016/j.ctim.2009.11.003
EuroQolGroup (1990) EuroQol--a new facility for the measurement of health-related quality of life health policy (Amsterdam, Netherlands) 16:199–208
Fioravanti A, Karagülle M, Bender T, Karagülle MZ (2017) Balneotherapy in osteoarthritis: facts, fiction and gaps in knowledge. Eur J Intern Med 9:148–150. https://doi.org/10.1016/j.eujim.2017.01.001
Gaál J, Varga J, Szekanecz Z et al (2008) Balneotherapy in elderly patients: effect on pain from degenerative knee and spine conditions and on quality of life. Isr Med Assoc J 10:365–369
Gallagher EJ, Liebman M, Bijur PE (2001) Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med 38:633–638. https://doi.org/10.1067/mem.2001.118863
Jeste ND, Hays JC, Steffens DC (2006) Clinical correlates of anxious depression among elderly patients with depression. J Affect Disord 90:37–41. https://doi.org/10.1016/j.jad.2005.10.007
Kahyaoglu Sut H, Unsar S (2011) Is EQ-5D a valid quality of life instrument in patients with acute coronary syndrome? Anadolu kardiyoloji dergisi : AKD = the Anatolian Journal of Cardiology 11:156–162. https://doi.org/10.5152/akd.2011.037
Karagülle M, Kardes S, Disci R, Gurdal H, Karagulle MZ (2016) Spa therapy for elderly: a retrospective study of 239 older patients with osteoarthritis. Int J Biometeorol 60:1481–1491. https://doi.org/10.1007/s00484-016-1138-7
Karagülle M, Kardes S, Karagulle MZ (2017) Real-life effectiveness of spa therapy in rheumatic and musculoskeletal diseases: a retrospective study of 819 patients. Int J Biometeorol 61:1945–1956. https://doi.org/10.1007/s00484-017-1384-3
Karagülle M, Kardeş S, Dişçi R, Karagülle MZ (2018a) Spa therapy adjunct to pharmacotherapy is beneficial in rheumatoid arthritis: a crossover randomized controlled trial. Int J Biometeorol 62:195–205
Karagülle M, Kardeş S, Karagülle MZ (2018b) Long-term efficacy of spa therapy in patients with rheumatoid arthritis. Rheumatol Int 38:353–362
Kardeş S, Karagülle M, Geçmen İ, Adıgüzel T, Yücesoy H, Karagülle MZ (2018) Outpatient balneological treatment of osteoarthritis in older persons: a retrospective study. Z Gerontol Geriatr. doi: https://doi.org/10.1007/s00391-018-1370-3
Koga K et al (2015) Coexistence of two forms of LTP in ACC provides a synaptic mechanism for the interactions between anxiety and chronic pain. Neuron 85:377–389. https://doi.org/10.1016/j.neuron.2014.12.021
Koyuncu E, Okmen BM, Ozkuk K, Tasoglu O, Ozgirgin N (2016) The effectiveness of balneotherapy in chronic neck pain. Clin Rheumatol 35:2549–2555. https://doi.org/10.1007/s10067-016-3199-8
Latorre-Roman PA, Rentero-Blanco M, Laredo-Aguilera JA, Garcia-Pinillos F (2015) Effect of a 12-day balneotherapy programme on pain, mood, sleep, and depression in healthy elderly people. Psychogeriatrics: the official journal of the Japanese Psychogeriatric Society 15:14–19. https://doi.org/10.1111/psyg.12068
Matsumoto H et al (2017) The effect of balneotherapy on pain relief, stiffness, and physical function in patients with osteoarthritis of the knee: a meta-analysis. Clin Rheumatol 36:1839–1847. https://doi.org/10.1007/s10067-017-3592-y
Matzer F, Nagele E, Lerch N, Vajda C, Fazekas C (2018) Combining walking and relaxation for stress reduction-a randomized cross-over trial in healthy adults. Stress Health 34:266–277
Morer C, Roques CF, Francon A, Forestier R, Maraver F (2017) The role of mineral elements and other chemical compounds used in balneology: data from double-blind randomized clinical trials. Int J Biometeorol 61:2159–2173. https://doi.org/10.1007/s00484-017-1421-2
Naumann J, Grebe J, Kaifel S, Weinert T, Sadaghiani C, Huber R (2017) Effects of hyperthermic baths on depression, sleep and heart rate variability in patients with depressive disorder: a randomized clinical pilot trial. BMC Complement Altern Med 28(17):172
Nguyen M, Revel M, Dougados M (1997) Prolonged effects of 3 week therapy in a spa resort on lumbar spine, knee and hip osteoarthritis: follow-up after 6 months A randomized controlled trial. Br J Rheumatol 36:77–81
Oosterveld FG, Rasker JJ, Floors M et al (2009) Infrared sauna in patients with rheumatoid arthritis and ankylosing spondylitis. A pilot study showing good tolerance, short-term improvement of pain and stiffness, and a trend towards long-term beneficial effects. Clin Rheumatol 28:29–34
Öner N, Compte AL (1998) Süreksiz Durumluk-Sürekli Kaygı Envanteri El Kitabı. Boğaziçi Üniversitesi Yayınevi, İstanbul
Özkuk K, Gurdal H, Karagulle M, Barut Y, Eroksuz R, Karagulle MZ (2017) Balneological outpatient treatment for patients with knee osteoarthritis; an effective non-drug therapy option in daily routine? Int J Biometeorol 61:719–728. https://doi.org/10.1007/s00484-016-1250-8
Rapolienė L, Razbadauskas A, Sąlyga J, Martinkėnas A (2016) Stress and fatigue management using balneotherapy in a short-time randomized controlled trial. Evid Based Complement Alternat Med 2016(9631684):1–10
Reyes-Gibby CC, Aday L, Cleeland C (2002) Impact of pain on self-rated health in the community-dwelling older adults. Pain 95:75–82
Spielberger CD, Gorsuch RL, Lushene RE (1970) Manual for the state-trait anxiety inventory Consulting Psychologists Press, Palo Alto
Stier-Jarmer M, Frisch D, Oberhauser C, Berberich G, Schuh A (2016) The effectiveness of a stress reduction and burnout prevention program. Dtsch Arztebl Int 113:781–788
Stier-Jarmer M, Frisch D, Oberhauser C, Immich G, Kirschneck M, Schuh A (2017) Effects of single moor baths on physiological stress response and psychological state: a pilot study. Int J Biometeorol 61:1957–1964
Stolee P, Lim SN, Wilson L, Glenny C (2012) Inpatient versus home-based rehabilitation for older adults with musculoskeletal disorders: a systematic review. Clin Rehabil 26:387–402. https://doi.org/10.1177/0269215511423279
Treede RD et al (2015) A classification of chronic pain for ICD-11. Pain 156:1003–1007. https://doi.org/10.1097/j.pain.0000000000000160
Uyar M, Köken İ (2017) Kronik ağrı nörofizyolojisi. Neurophysiology of chronic pain TOTBİD Dergisi 16:70–76. https://doi.org/10.14292/totbid.dergisi.2017.12
WHO (2015) Health in older age. In: World Report on Ageing and Health. World Health Organization, Geneva, Switzerland
Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ 81:646–656
Zhuo M (2014) Long-term potentiation in the anterior cingulate cortex and chronic pain. Philos Trans R Soc Lond Ser B Biol Sci 369:20130146. https://doi.org/10.1098/rstb.2013.0146
Zwolińska J, Weres A, Wyszyńska J (2018) One-year follow-up of spa treatment in older patients with osteoarthritis: a prospective, single group study. Biomed Res Int
Acknowledgments
The authors thank Barış Kaki, Ph.D., from Usak University, for his technical help in performing statistical analysis. The authors also thank Sinan Kardeş, MD, from Istanbul Faculty of Medicine, for English editing and proofreading of the manuscript and for his critical assistance in revising the manuscript according to the reviewers’ comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Ethics Committee (25.02.2016-2015/88) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all participants prior to being included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Özkuk, K., Uysal, B., Ateş, Z. et al. The effects of inpatient versus outpatient spa therapy on pain, anxiety, and quality of life in elderly patients with generalized osteoarthritis: a pilot study. Int J Biometeorol 62, 1823–1832 (2018). https://doi.org/10.1007/s00484-018-1584-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-018-1584-5