Abstract
Outdoor temperature has been reported to have a significant influence on the seasonal variations of stroke mortality, but few studies have investigated the effect of high temperature on the mortality of ischemic and hemorrhagic strokes. The main study goal was to examine the effect of temperature, particularly high temperature, on ischemic and hemorrhagic strokes. We investigated the association between outdoor temperature and stroke mortality in four metropolitan cities in Korea during 1992–2007. We used time series analysis of the age-adjusted mortality rate for ischemic and hemorrhagic stroke deaths by using generalized additive and generalized linear models, and estimated the percentage change of mortality rate associated with a 1°C increase of mean temperature. The temperature-responses for the hemorrhagic and ischemic stroke mortality differed, particularly in the range of high temperature. The estimated percentage change of ischemic stroke mortality above a threshold temperature was 5.4 % (95 % CI, 3.9–6.9 %) in Seoul, 4.1 % (95 % CI, 1.6–6.6 %) in Incheon, 2.3 % (−0.2 to 5.0 %) in Daegu and 3.6 % (0.7–6.6 %) in Busan, after controlling for daily mean humidity, mean air pressure, day of the week, season, and year. Additional adjustment of air pollution concentrations in the model did not change the effects. Hemorrhagic stroke mortality risk significantly decreased with increasing temperature without a threshold in the four cities after adjusting for confounders. These findings suggest that the mortality of hemorrhagic and ischemic strokes show different patterns in relation to outdoor temperature. High temperature was harmful for ischemic stroke but not for hemorrhagic stroke. The risk of high temperature to ischemic stroke did not differ by age or gender.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is the second leading cause of mortality worldwide and risk factors such as hypertension, current smoking, abdominal obesity, diet and physical activity were reported to account for more than 80 % of all stroke risks (Strong et al. 2007, Johnston et al. 2009). Recently, weather conditions have also been reported to have a significant influence on the seasonal variations in the incidence or mortality of stroke (Jimenez-Conde et al. 2008). However, the relationship between stroke and weather conditions is complex because of various competing factors such as geographical area and race (McArthur et al. 2010). Although many studies have examined the influence of weather factors on stroke incidence or mortality, inconsistent results have been reported on the relationship between the incidence or mortality of stroke and a unit increase of outdoor temperature (Kyobutungi et al. 2005; Chang et al. 2004; Field and Hill 2002; Oberg et al. 2000; Piver et al. 1999; Wang et al. 2009; Wang et al. 2003b). Particularly, few data are available on the different patterns of hemorrhagic and ischemic strokes in relation to high temperature. With the increased incidence of climate change-induced heat waves during the summer, a better understanding of the influence of high temperature on hemorrhagic and ischemic strokes would be very helpful to prevent and manage the illness. Hemorrhagic and ischemic strokes are different diseases although they present with a similar disease manifestation. They have common risk factors such as hypertension, but other risk factors or pathogenetic mechanism can differ. As temperature increases or decreases, blood vessels dilate or constrict, which alters the peripheral circulation resistance and blood pressure. Although some study results showed contradictory findings, such as a significant increase in the systolic blood pressure during the hottest night among the elderly under antihypertensive treatment (Modesti et al. 2006) and a higher blood pressure on warm days than on cold days during the coldest season (Morabito et al. 2008), many studies suggested that blood pressure may be inversely correlated with temperature (Barnett et al. 2007; Halonen et al. 2011). The Framingham Offspring Cohort Study supported the relationship of high temperature and decreased blood pressure by showing that flow-mediated dilation of the brachial artery was lowest in winter (Widlansky et al. 2007).
Elevated blood pressure due to increased circulation resistance during cold weather has been linked to morbidity and mortality due to cardiovascular diseases. Likewise, falling blood pressure associated with hot weather may contribute to lowering the risk of those cardiovascular diseases that depend greatly on blood pressure such as hemorrhagic stroke (Alperovitch et al. 2009). However, hot weather also causes dehydration because of excessive evaporation and sweating, which can lead to electrolyte imbalance, thermoregulatory failure, or thromboembolism (Rikkert et al. 2009; Schobersberger et al. 2009).
Therefore, although blood pressure declines with increasing temperature (Kristal-Boneh et al. 1997), other conditions favorable for ischemic stroke may remain or even worsen in hot weather. In addition, an excessively low blood pressure, when associated with dehydration in a short time period with heat wave attack, could increase the risk of ischemic stroke (Kikura et al. 2010). Actually, during the heat wave in Europe in August 2003, one of the poor prognostic factors related with increased mortality risk in the elderly was lower blood pressure (Davido et al. 2006). Therefore, the temperature effect on ischemic and hemorrhagic strokes could be different. The main goal of the study is to examine the effect of temperature on ischemic and hemorrhagic strokes, particularly at high temperature.
Methods
We used weather and stroke mortality data collected in four metropolitan cities in Korea with over one million residents—Seoul, Incheon, Daegu, and Busan—during 1992–2007. Seoul and Incheon are located in northwestern South Korea whereas Daegu and Busan are in the southeastern part. Daily stroke deaths were obtained from the mortality records of the Korea National Statistical Office. The hemorrhagic and ischemic stroke deaths were coded in the format of International Classification of Diseases revision 9 (ICD 9, 430–432 and 433–436, respectively) before 1995 and revision 10 (ICD10, I60-I62 and I63-I66, respectively) thereafter. So, we used data coded by ICD-9 for 3 years (1992–1994) and by ICD-10 for 13 years (1995–2007). This study was approved by the institutional review board at the Seoul National University School of Public Health.
There were substantial age-distribution changes in the Korean population during the study period. To adjust for these changes, we calculated the age-adjusted death rate. At first, we collected area-level information such as total and age-specific population for each year during the study periods from each city. Daily values of area-specific population were estimated by a linear interpolation of annual age-specific population counts. We calculated the daily total and cause-specific death rates for each age group (5 year intervals up to 79 years, and age 80 years and older) as the reported number of deaths divided by the daily age-specific area population. We then calculated the age-adjusted total and cause-specific death rates as the sum of the day-specific death rate for each age group weighted by the fraction of the registered residence population (each year) in that age group. This was done separately for all ages, for ages 0–64 and 65 and older, and for males and females in each area. The mortality rate was expressed in the unit of deaths per 100,000 population-days.
Korea has four distinct seasons and an annual average temperature range of 12.9 °C (Seoul) to 14.9 °C (Busan), depending on the location. Data on temperature, relative humidity and air pressure were obtained from the Korea Meteorological Administration. A weather station was located in the centre of each city. Daily average concentrations for particulate matter less than 10 μg/m3 in aerodynamic diameter (PM10) and day-time maximum ozone concentrations (O3) were collected from the Research Institute of Public Health and Environment. If two or more monitoring stations were located in a city, the average air pollution exposure of all stations was calculated. Due to the short period of data availability, PM10 and O3 were not included in the main model; however, since they have been reported as risk factors for stroke mortality in a previous study (Hong et al. 2002), a sensitivity analysis was conducted to validate the temperature effects, including both PM10 and O3, in the model using data from June 1, 2000 to December 31, 2007. Ownership and usage of air conditioning may have modified the temperature effects in this study (Ostro et al. 2010). We collected the citywide prevalence of room air conditioning to explain city-specific temperature effects. The prevalence was based on the 2004 Survey on Electricity Consumption Characteristics of Home Appliances (KPX 2004) conducted by the Korea Power Exchange (Seoul, Korea). The survey was to collect information on the ownership and usage hours of home appliances. A stratified multi-stage sample of 3,500 households was selected from 16 regions in Korea for the survey.
We used time series analysis of the age-adjusted mortality rate for ischemic and hemorrhagic strokes. The associations between temperature and stroke were visualized with a generalized additive model (GAM) (Wood 2001). A generalized linear model (GLM) with a quasi-Poisson distribution of mortality was used to estimate the linear associations between temperature and mortality. When a nonlinear association was observed between stroke mortality and temperature, piecewise linear regression models were used to estimate the threshold points and temperature effects below and above the threshold points (Muggeo 2003). Potential confounders were day of the week, season, year, daily mean relative humidity, and daily mean air pressure.
To estimate the percentage change of mortality associated with a 1 °C increase of outdoor temperature, a moving average lag structure was used. Lag days within a short-term period such as 1, 3, 5, and 7 days were selected based on the lowest unbiased risk estimator (UBRE) of GAM (Wood 2001). For example, moving average lag 03 refers to the average of the current and three previous days’ temperature. The selected disease- and city-specific lag days during 1992–2007 are 07, 07, 05, and 03 days for hemorrhagic stroke and 07, 05, 07, and 07 days for ischemic stroke in Seoul, Incheon, Daegu, and Busan, respectively (Supplemental Figure 1). The moving average lag days were used to estimate both linear and non-linear associations of mortality with temperature. A sensitivity analysis with additional adjustment of daily mean PM10 and maximum O3 using available data from 2000 to 2007 was conducted. Moving average lag days and threshold temperature points were selected depending on the model, study periods, location and subtype of stroke.
A previous study showed that the elderly and females were more susceptible to cold-induced ischemic stroke than the non-elderly and males, respectively (Hong et al. 2003). Therefore, in a stratified analysis by age (below 65 years old vs. 65 years old and older) and gender, we examined which groups were more susceptible to heat effects. All study procedures were conducted using R 2.12.1 (The Comprehensive R Archive Network: http://cran.r-project.org).
Results
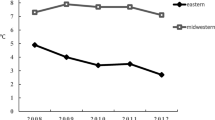
There were 149,598 deaths due to hemorrhagic and ischemic strokes in the four cities during 1992 to 2007: 57,452 hemorrhagic (38 %) and 92,146 ischemic (62 %). Table 1 shows the geographical and meteorological characteristics of the four cities. Seoul and Incheon are higher latitude areas and have a lower mean temperature than Daegu and Busan. The difference of mean temperature among the four cities was greater in winter than in summer (5.0 °C vs. 1.6 °C in winter and summer, respectively). The prevalence of a room air conditioning was highest in Daegu (0.61 per household) and lowest in Busan (0.40 per household). Supplemental Table 1 shows city-specific annual mortality counts. Figure 1 displays the stroke mortality rate per 100,000 population-days by gender and age group. There was no significant difference according to gender. However, the elderly were more susceptible to stroke mortality than the non-elderly population.
Figure 2 shows the lowess curves of seasonal trend for hemorrhagic and ischemic stroke mortality rate and temperature during 1992–2007. Stroke mortality rate was relatively low in summer, although a summer peak appeared in ischemic mortality. Figure 3 shows the relationship between mean temperature at city-specific moving average lag days and stroke mortality in the four cities. The figures present distinct patterns of stroke mortality in relation to temperature, i.e. the hemorrhagic stroke mortality risk decreased with increasing temperature without an apparent threshold, whereas the ischemic stroke mortality exhibited a V-shaped relationship with a threshold temperature in half of the cities considered. These patterns seemed to hold for all age and gender groups in the four cities (data not shown).
While high temperature exerted a beneficial effect on hemorrhagic stroke mortality, it worsened ischemic stroke mortality. Ambient temperature effects on ischemic stroke below or above a threshold are shown in Table 2. Threshold temperatures were between 23.4 °C (Incheon) and 25.3 °C (Busan) and between 17.3 °C (Daegu) and 24.8 °C (Incheon) during 1992–2007 and 2000–2007, respectively. After air pollution was controlled for in the model during 2000–2007, thresholds were between 17.3 °C (Daegu) and 23.8 °C (Incheon). The risk of ischemic stroke mortality above the thresholds was highest in Seoul at 5.4 % (95 % confidence interval (CI), 3.9–6.9) and lowest in Daegu at 2.3 % (95 % CI, −0.2 to 5.0). In 2000–2007 the effects were substantially changed even before controlling for the air pollution concentrations, at 2.5 % (95 % CI, 0.1–4.9) and 1.3 % (95 % CI, −0.1 to 2.7) in Seoul and Daegu, respectively. Below the threshold temperature, ischemic stroke mortality risk increased as temperature decreased by 0.8 % (95 % CI, 0.2–1.5), 1.0 % (95 % CI, 0.0–1.9), and 0.8 % (95 % CI, 0.1–1.5) per 1 °C decrease in Incheon, Daegu, and Busan, respectively.
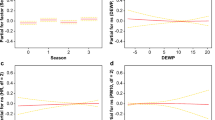
Figure 4 illustrates the percentage change of risk of ischemic strokes per 1 °C increase of mean temperature above the thresholds by age and gender during 2000–2007 after adjustment for air pollution. There was no distinction between genders. The elderly showed narrower CI than the non-elderly. However, the effect among the elderly was not different from that among the non-elderly, both below and above the thresholds. We also found little evidence of any difference of temperature effects between gender and age groups in hemorrhagic stroke mortality (data not shown).
Discussion
Hemorrhagic stroke mortality risk significantly decreased with increasing temperature without a threshold, whereas ischemic stroke mortality exhibited a V-shaped relationship with temperature in two of the four cities considered: Seoul and Incheon. The effects of high temperature on ischemic stroke mortality were slightly greater in higher latitude areas such as Seoul and Incheon than in lower latitude areas.
Consistent with our results, studies in Australia (Wang et al. 2009), Taiwan (Pan et al. 1995), China (Liu et al. 2004), and Italy (Morabito et al. 2011) have found a threshold effect of morbidity and mortality of ischemic stroke and a negative linear association for hemorrhagic stroke associated with temperature. However, other studies have shown different associations of temperature with strokes such as increased risk of ischemic stroke incidence by cold temperature (Hong et al. 2003) or null associations between any subtypes of stroke and temperature changes (Cowperthwaite and Burnett 2011). These different results might be due to different study populations, locations, and periods (Wang et al. 2009). On the other hand, the weak or non-significant association of ischemic stroke mortality with temperature in some studies may be due to the assumption of a linear relationship in the case of the existence of nonlinearity. For example, Wang et al. showed a threshold pattern of maximum temperature on ischemic stroke in summer, but the relative risk was not statistically significant since the risk was estimated based on the assumption of linearity (Wang et al. 2009).
The V-shape of the relationship between ischemic stroke and temperature compared to the negative linear association with temperature for hemorrhagic stroke may be attributable to the pathophysiological difference between the two diseases (Pan et al. 1995). Falling blood pressure associated with lowering peripheral vascular resistance in hot weather may reduce the risk of hemorrhagic stroke, whereas dehydration arising from excessive evaporation and sweating, and electrolyte imbalance from high temperature may cause thromboembolism and thereby increase the risk of ischemic stroke (Rikkert et al. 2009, Schobersberger et al. 2009).
The temperature effects on ischemic stroke mortality varied by area in this study. Certain area characteristics such as air conditioning (Ostro et al. 2010) and population density (Medina-Ramon and Schwartz 2007) may have modified the heat effects on health. For example, although Daegu and Busan had similar geographical and meteorological conditions, the high temperature effect in Daegu was slightly smaller than that in Busan. The highest prevalence of a room air conditioning of Daegu (0.62 per household) may explain the difference. Another plausible explanation for the variation by area can be physiological adaptation to temperature in lower latitude or higher temperature areas. For example, southern cities such as Daegu and Busan showed higher annual average temperature than northern cities did (around 14 °C in southern cities vs. 12 °C in northern cities). The high temperature effects were larger in the higher latitude cities (2–3 % vs. 4–5 % increase of ischemic stroke per 1 °C increase in southern and northern cities, respectively). Because temperature differences between southern and northern cities were greater in winter than in summer, we can assume that the adaptation to colder winter may have increased the risk of ischemic stroke mortality in summer. Supporting results have also been reported in US cities (Curriero et al. 2002; Medina-Ramon and Schwartz 2007; Zanobetti and Schwartz 2008). For example, Curriero et al. found a greater warmer temperature effect in northern cities and Medina-Ramón showed the largest heat effects in cities with a milder summer.
Air pollution has been reported to be associated with stroke (Wellenius et al. 2005; Tsai et al. 2003; Hong et al. 2002) and was controlled for in the present model using data from 2000 to 2007 due to the limited availability of air pollution data. Before considering air pollution in the model, we observed substantial changes in temperature threshold points and effects. For example, the threshold temperatures using the 2000–2007 data were lower in southern cities (Daegu and Busan) and higher in Incheon compared with the threshold temperatures using the 1992–2007 data. The effects above the threshold were substantially attenuated, except in Incheon during 2000–2007. The introduction of a heat-wave warning system and wide use of air conditioning may have attenuated the high temperature effect. However, it is not clear why Incheon had a higher threshold temperature and less attenuated effect in 2000–2007 than in 1992–2007. While the study period caused a difference in temperature effects, the adjustment of air pollution did not significantly influence the effects. Hence, we may conclude that temperature was an independent risk factor of stroke mortality. The elderly as a group have been reported to be susceptible to high temperature, especially in cardiovascular-related mortality (Gouveia et al. 2003). However, the present study results showed little evidence of any differences in ischemic stroke risk between the elderly and the non-elderly due to high temperature above the threshold. A study in Adelaide, Australia, also found no significant heat effect among the elderly (Nitschke et al. 2007). Although the elderly were not found to be more susceptible to a high temperature effect for ischemic stroke mortality in this study, the number of ischemic stroke deaths of the elderly attributable to high temperature was much greater than that of the non-elderly since the overall stroke incidence was much higher in the elderly.
This study has examined the mortality-temperature relationship using daily stroke mortality rate per 100,000 population-days instead of daily mortality count to compare the risk in four cities. The mortality rate was also age-adjusted, which may have overcome the different population age structures among these four cities. While other studies examined the stroke mortality-temperature relationship based on a single city or region (Wang et al. 2003a), we observed hemorrhagic and ischemic stroke associations with temperature in four major cities in Korea. This study had several limitations. First, we did not distinguish between the deceased due to newly occurred stroke and the death of preexisting stroke patients since we examined stroke mortality as a health outcome instead of investigating stroke onset or morbidity. Second, we could not distinguish whether the temperature-associated increase of stroke mortality represents a true increase of stroke mortality or only presents the earlier death of those about to die soon. Therefore, harvesting cannot be excluded for at least some of the observed association (Braga et al. 2002). Third, for the diagnosis of the two types of stroke, we relied on vital statistics with unknown accuracy. However, most of the stroke patients in Korea were known to be diagnosed after imaging studies of the brain by magnetic resonance imaging or computerized tomography (Hong et al. 2003). In conclusion, we found that the mortalities of hemorrhagic and ischemic strokes exhibit different patterns in relation to outdoor temperature and that high temperature was harmful for ischemic stroke but not for hemorrhagic stroke.
Abbreviations
- ICD:
-
International classification of diseases
- CI:
-
Confidence intervals
- PM10 :
-
Particulate matter less than 10 μg/m3 in aerodynamic diameter
- O3 :
-
Ozone
- GAM:
-
Generalized additive model
- GLM:
-
Generalized linear model
- UBRE:
-
Unbiased risk estimator
References
Alperovitch A, Lacombe JM, Hanon O, Dartigues JF, Ritchie K, Ducimetiere P, Tzourio C (2009) Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three-City study. Arch Intern Med 169(1):75–80
Barnett AG, Sans S, Salomaa V, Kuulasmaa K, Dobson AJ (2007) The effect of temperature on systolic blood pressure. Blood Press Monit 12(3):195–203
Braga AL, Zanobetti A, Schwartz J (2002) The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect 110(9):859–863
Chang CL, Shipley M, Marmot M, Poulter N (2004) Lower ambient temperature was associated with an increased risk of hospitalization for stroke and acute myocardial infarction in young women. J Clin Epidemiol 57(7):749–757
Cowperthwaite MC, Burnett MG (2011) An analysis of admissions from 155 United States hospitals to determine the influence of weather on stroke incidence. J Clin Neurosci 18(5):618–623
Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA (2002) Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 155(1):80–87
Davido A, Patzak A, Dart T, Sadier MP, Meraud P, Masmoudi R, Sembach N, Cao TH (2006) Risk factors for heat related death during the August 2003 heat wave in Paris, France, in patients evaluated at the emergency department of the Hôpital Européen Georges Pompidou. Emerg Med J 23(7):515–518
Field TS, Hill MD (2002) Weather, Chinook, and Stroke Occurrence. Stroke 33(7):1751–1758
Gouveia N, Hajat S, Armstrong B (2003) Socioeconomic differentials in the temperature-mortality relationship in Sao Paulo, Brazil. Int J Epidemiol 32(3):390–397
Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J (2011) Relationship between outdoor temperature and blood pressure. Occup Environ Med 68(4):296–301
Hong YC, Lee JT, Kim H, Kwon HJ (2002) Air pollution: a new risk factor in ischemic stroke mortality. Stroke 33(9):2165–2169
Hong YC, Rha JH, Lee JT, Ha EH, Kwon HJ, Kim H (2003) Ischemic stroke associated with decrease in temperature. Epidemiology 14(4):473–478
Jimenez-Conde J, Ois A, Gomis M, Rodriguez-Campello A, Cuadrado-Godia E, Subirana I, Roquer J (2008) Weather as a trigger of stroke. Daily meteorological factors and incidence of stroke subtypes. Cerebrovasc Dis 26(4):348–354
Johnston SC, Mendis S, Mathers CD (2009) Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol 8(4):345–354
Kikura M, Bateman BT, Tanaka KA (2010) Perioperative ischemic stroke in non-cardiovascular surgery patients. J Anesth 24(5):733–738
KPX (2004) Survey on electricity consumption characteristics of home appliances.
Kristal-Boneh E, Harari G, Green MS (1997) Seasonal change in 24-hour blood pressure and heart rate is greater among smokers than nonsmokers. Hypertension 30(3 Pt 1):436–441
Kyobutungi C, Grau A, Stieglbauer G, Becher H (2005) Absolute temperature, temperature changes and stroke risk: a case-crossover study. Eur J Epidemiol 20(8):693–698
Liu F, Zhang JL, Lu C (2004) The relationship of temperature and stroke incidence in Beijing: a time-series study. Zhonghua Liu Xing Bing Xue Za Zhi 25(11):962–966
McArthur K, Dawson J, Walters M (2010) What is it with the weather and stroke? Expert Rev Neurother 10(2):243–249
Medina-Ramon M, Schwartz J (2007) Temperature, temperature extremes, and mortality: a study of acclimatization and effect modification in 50 United States cities. Occup Environ Med. Jun 28. [Epub ahead of print]
Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, Giglio A, Bilo G, Caldara G, Lonati L, Orlandini S, Maracchi G, Mancia G, Gensini GF, Parati G (2006) Weather-related changes in 24-hour blood pressure profile: effects of age and implications for hypertension management. Hypertension 47(2):155–161
Morabito M, Crisci A, Orlandini S, Maracchi G, Gensini GF, Modesti PA (2008) A synoptic approach to weather conditions discloses a relationship with ambulatory blood pressure in hypertensives. Am J Hypertens 21(7):748–752
Morabito M, Crisci A, Vallorani R, Modesti PA, Gensini GF, Orlandini S (2011) Innovative approaches helpful to enhance knowledge on weather-related stroke events over a wide geographical area and a large population. Stroke 42(3):593–600
Muggeo VM (2003) Estimating regression models with unknown break-points. Stat Med 22(19):3055–3071
Nitschke M, Tucker GR, Bi P (2007) Morbidity and mortality during heatwaves in metropolitan Adelaide. Med J Aust 187(11–12):662–665
Oberg AL, Ferguson JA, McIntyre LM, Horner RD (2000) Incidence of stroke and season of the year: evidence of an association. Am J Epidemiol 152(6):558–564
Ostro B, Rauch S, Green R, Malig B, Basu R (2010) The effects of temperature and use of air conditioning on hospitalizations. Am J Epidemiol 172(9):1053–1061
Pan WH, Li LA, Tsai MJ (1995) Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet 345(8946):353–355
Piver WT, Ando M, Ye F, Portier CJ (1999) Temperature and air pollution as risk factors for heat stroke in Tokyo, July and August 1980–1995. Environ Health Perspect 107(11):911
Rikkert MG, Melis RJ, Claassen JA (2009) Heat waves and dehydration in the elderly. BMJ 339:b2663
Schobersberger W, Schobersberger B, Partsch H (2009) Travel-related thromboembolism: mechanisms and avoidance. Expert Rev Cardiovasc Ther 7(12):1559–1567
Strong K, Mathers C, Bonita R (2007) Preventing stroke: saving lives around the world. Lancet Neurol 6(2):182–187
Tsai S-S, Goggins WB, Chiu H-F, Yang C-Y (2003) Evidence for an association between air pollution and daily stroke admissions in Kaohsiung, Taiwan. Stroke 34(11):2612–2616
Wang Y, Levi CR, Attia JR, D'Este CA, Spratt N, Fisher J (2003a) Seasonal variation in stroke in the Hunter Region, Australia: a 5-year hospital-based study, 1995–2000. Stroke 34(5):1144–1150
Wang Y, Levi CR, Attia JR, D’Este CA, Spratt N, Fisher J (2003b) Seasonal variation in stroke in the Hunter Region, Australia: a 5-year hospital-based study, 1995–2000. Stroke 34(5):1144–1150
Wang XY, Barnett AG, Hu W, Tong S (2009) Temperature variation and emergency hospital admissions for stroke in Brisbane, Australia, 1996–2005. Int J Biometeorol 53(6):535–541
Wellenius GA, Schwartz J, Mittleman MA (2005) Air pollution and hospital admissions for ischemic and hemorrhagic stroke among medicare beneficiaries. Stroke 36(12):2549–2553
Widlansky ME, Vita JA, Keyes MJ, Larson MG, Hamburg NM, Levy D, Mitchell GF, Osypiuk EW, Vasan RS, Benjamin EJ (2007) Relation of season and temperature to endothelium-dependent flow-mediated vasodilation in subjects without clinical evidence of cardiovascular disease (from the Framingham Heart Study). Am J Cardiol 100(3):518–523
Wood S (2001) Mgcv: GAMs and generalized Ridge regression for R. R News 1(2):20–25
Zanobetti A, Schwartz J (2008) Temperature and mortality in nine US cities. Epidemiology 19(4):563–570
Acknowledgement
The work was supported by Basic Science Research Program (#2010-0009581) and Global Research Lab (#K21004000001-10A0500-00710) through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 43 kb)
Rights and permissions
About this article
Cite this article
Lim, YH., Kim, H. & Hong, YC. Variation in mortality of ischemic and hemorrhagic strokes in relation to high temperature. Int J Biometeorol 57, 145–153 (2013). https://doi.org/10.1007/s00484-012-0542-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-012-0542-x