Abstract
Advances in the care of neonates to the extreme limits of viability have increased the risk of severe comorbidities in surviving preemies. The respiratory and the neurodevelopmental consequences of premature birth and/or intra-uterine growth retardation have been well described. Because of the usual clinical silence of the kidney, the long-term renal consequences of low birth weight have not been as well studied. A case report illustrates the risk factors associated with low birth weight and prematurity and discusses the pathogenesis of the late consequences of the congenital nephron deficit associated with a low birth weight. Practical recommendations are given for a tight follow-up of these newly born preemies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Limits of viability in premature infants—what about the kidney?
With advances in neonatal care, survival of premature infants at the limits of viability has significantly increased. Despite the improvement in mortality, there is a 20–50% risk of morbidities [1] in survivors born at less than 28 weeks of gestation or with birth weight less than 1000 g. Most of the articles on follow-up and outcomes for extremely low birth weight (ELBW) infants (birth weight of less than 1000 g or even lighter) provide up-to-date overviews on respiratory and neurodevelopmental consequences and address concerns for the high prevalence of pulmonary and neurosensory sequelae in infants who survive to NICU discharge [1,2,3].
Epidemiologic research and systematic reviews show that both low birth weight (LBW, birth weight of less than 2500 g) and preterm birth (birth at less than 37 weeks of gestation) are associated with childhood onset of chronic kidney disease (CKD) [4,5,6]. A national cohort study in Sweden showed that extremely preterm birth (< 28 weeks of gestation) was associated with a threefold risk of CKD from birth into mid-adulthood, as compared with full term birth [7]. In that cohort, the association between preterm birth and CKD was strongest at ages 0–9 years, thus earlier in life as compared to previous studies [4], which could in part be due to improved survival of smaller and less healthy preterm infants.
The kidney can be extremely silent: (i) kidney injury remains often unnoticed until irreversible alterations take place; (ii) a large number of patients suffering from kidney disease present symptoms which are not directly referable to that organ; (iii) the kidney works, remaining silent even when suffering from significant nephron loss.
This educational review describes the pathogenesis of the late consequences of the congenital nephron deficit associated with a LBW and discusses the need to pilot a specific program to implement kidney-protective strategies for newborn infants at the limit of viability cared for in NICU.
Effects of low birth weight and preterm birth on nephrogenesis
In humans, nephrogenesis ends prenatally at around 34–36 weeks and 60% of the nephrons are formed during the third trimester of pregnancy. Each kidney contains approximately 1 million nephrons (227,327 to 1,825,380). The number of nephrons correlates with birth weight, the count increasing by 25,743 for each 100 g of birth weight [8, 9]. In case of preterm birth, whatever the gestational age, nephrogenesis ceases by the end of the first 40 days of life and the nephron number is lower compared to full term birth [10].
The consequences of both LBW and preterm birth on nephrogenesis have been well studied. The exact relationship between gestational age at birth and abnormal kidney function in later life has however not yet been established. Most of the clinical studies on kidney development and risk of CKD in LBW infants did not report adequate information on gestational age [4, 5]. A confounding factor is that preterm birth accounts for approximately 80% of LBW.
Moreover, preterm birth may occur in various situations. Among maternal causes, a low-protein diet, gestational diabetes, administration of glucocorticoids or exposure to other drugs/toxins, deficiency of micronutrients, iron or vitamins, and hypertensive disorders may all induce adverse environments in utero, with or without associated fetal growth restriction (IUGR). As proven by human and animal studies, all these antenatal conditions per se can induce a poor nephron endowment in the neonate [11].
Especially in ELBW infants, postnatal factors, including postnatal nutrition and growth, infection and inflammatory states, and exposure to nephrotoxic drugs, may also contribute to worsen the nephron deficit. Autopsy studies have shown that in “very sick” preterm infants, the postnatal progress of the nephrogenesis can be impaired, with a greater percentage of morphologically abnormal glomeruli, compared to “healthy” gestational controls [12, 13].
Consequences of a nephron deficit
The compensatory hyperfiltration phenomenon
In 1981, Brenner et al. hypothesized that compensatory glomerular hemodynamic changes take place in response to nephron loss [14]. In case of poor nephron endowment, an adaptive response occurs, inducing increased glomerular filtration rate (GFR) at a single nephron level. Experimental studies and human models of reduced kidney mass occurring from birth showed that the increase of per nephron filtration is associated with an increase in intraglomerular pressure and filtration fraction [14]. The underlying mechanism is a predominant post-glomerular vasoconstriction, which is mediated, at least in part, by the activation of the renin–angiotensin system [15]. Increased levels of angiotensin II may in turn up-regulate the expression of growth factors and cytokines. All these compounds stimulate oxidative stress and promote cell growth and fibrosis [16].
Functional consequences of glomerular hyperfiltration
Mild albuminuria may appear as a first manifestation of hyperfiltering nephrons. Persistence of glomerular capillary hyperperfusion and hyperfiltration can lead to ongoing injury to podocytes and to the glomerular microvasculature, which contributes to proteinuria. With aging, adaptive hypertrophy of functional nephrons may create a positive feedback loop inducing tubular atrophy and interstitial fibrosis. This process is accelerated by and may lead to arterial hypertension and CKD [14]. Before progression to fibrosis or kidney failure, several abnormal renal changes can be identified, as illustrated by pathology findings and also by studies using sophisticated technologies of nephron imaging [17]: early focal and segmental glomerular sclerosis, glomerular hypertrophy, loss of glomeruli and glomerular maldevelopment. Animal models show that these abnormal changes may also occur as pathology responses following acute kidney injury (AKI) during nephrogenesis [18].
According to evolutionary nephrology [19], genotype polymorphism, epigenetics, and environment (ischemia, hypoxia, toxins, metabolic and oxidative stress) influence the performance capacity of the nephron and shape the susceptibility towards CKD in a context of nephron loss.
We now present below a clinical case illustrative of the long-term potential adverse renal consequences of preterm birth.
Case report
A 27-year-old man presented to his family doctor with fatigue, pallor, malaise, nocturia, mild arterial hypertension (130/90), and proteinuria (75 g/mol creat (N < 20)). The plasma creatinine was moderately elevated (180 μmol/l). The patient’s childhood had been uneventful, except for a difficult neonatal life after a pregnancy complicated by IUGR. He was born premature (29 weeks of gestational age), with a birth weight of 920 g and cared for in the NICU of Lausanne University Hospital. The patient had presented with severe respiratory distress syndrome (RDS), transient acute kidney injury (AKI), and a patent ductus arteriosus (PDA). He had received indomethacin for closure of the ductus and aminoglycosides to cope with the risk of infection. Thanks to effective treatment, he had left the neonatal unit in good condition, with apparent normal kidney function (plasma creatinine, 50 µmol/l). At the age of 3 years, the pediatrician had found normal growth (25 percentile) and normal urinalysis. After that visit, the infant had been lost to follow-up as his family had moved abroad. He reported neither clinical symptoms associated with arterial hypertension or abnormal kidney function nor medical visits in the meanwhile.
Following discussion with the family doctor, a treatment with angiotensin-converting enzyme inhibitor was started (ramipril 5 mg/day), which induced in a few weeks an improvement of hypertension and proteinuria. Losartan (50 mg/day) had to be added to the treatment a year later in order to maintain the benefit.
The occurrence of kidney failure at the age of 27 years was a surprise for the patient, his parents, and the family doctor. The intriguing following question is thus asked: in this case, was the kidney failure presenting at an early adult age already foretold at birth? Results open several questions related to morbidities associated with ELBW and kidney protective strategies to reduce the risk of severe nephron deficit.
Revisiting the case—kidney-protective strategies in NICU
In the case presented here, the following events and insults could have been responsible for the pathogenesis of kidney failure: hypoxia, AKI, PDA, indomethacin, IUGR, and nephrotoxic drugs.
Hypoxia and RDS
Kidney hypoperfusion with decreased glomerular filtration rate (GFR) is present in neonates with severe RDS [20]. Stimulation of the renin–angiotensin system and overactivation of intrarenal adenosine mediate the renal vasoconstriction and play a key role in the pathogenesis of the hypoxemic vasomotor nephropathy of preterm neonates [21]. Experimental studies have also shown that altered oxygen tension and oxidative stress may impair nephrogenesis by apoptotic and inflammatory phenomena. These effects are mediated by reduced expression of kidney hypoxia-inducible factor (HIF)-1α and might be responsible for smaller glomerular diameters, smaller nephrogenic zone width, glomerular crescents, and decreased creatinine clearance [22]. Finally, studies in preterm lambs showed that invasive and non-invasive respiratory support altered postnatal development of glomerular capillary surface density and glomerular surface area in the inner and outer cortex, probably by reducing renal blood flow [23]. When hypoperfusion of the kidneys is prolonged, this may lead to ischemic reactions at the cellular level with consequent necrosis of some nephrons, further aggravating the nephron deficit [24].
As with most ELBW infants, our patient presented with RDS during the first days of life. Typically, kidney hypoperfusion during hypoxia or RDS can be worsened by other associated risk factors in the stressed neonatal kidney (birth asphyxia, decrease in intravascular volume, dehydration, sepsis), and this can lead from vasomotor nephropathy to AKI [21, 25]. As AKI in NICUs is nowadays considered as a disease moving along a continuum from mild kidney dysfunction to the ultimate state of kidney failure [26], a chief challenge for neonatologists is to identify at-risk infants, from a general point of view, and from a patient-based perspective, each degree of acute reduction of kidney function. The AWAKEN study has improved our understanding of which vulnerable preterm neonates may develop AKI and when it occurs in the NICU [27]; so, a crucial point remains the identification of early markers of kidney hypoperfusion. In a recent study, low resistive index in the renal artery at Doppler ultrasound and low renal regional oxygen saturation (rSO2) on near-infrared spectroscopy during the first day of life were significantly associated with developing AKI within the first postnatal week in very preterm infants [28]. In such a context, the anticipation of AKI by hemodynamic interventions seems promising. In particular, the use of medium-dose dopamine may improve kidney function by (a) increasing cardiac output through stimulation of the β-adrenergic receptors; (b) increasing blood pressure by inotropic and vasoactive mechanisms; (c) increasing kidney perfusion via stimulation of the dopamine receptors in the renal vessels; and (d) directly inhibiting sodium reabsorption [29].
Among other kidney-protecting strategies in NICUs, methylxanthines are also very interesting options. Theophylline and caffeine are nonselective antagonists of adenosine receptors. Since enhanced intrarenal adenosine levels lead to reduced GFR, especially following hypoxia, the administration of 1 mg/kg theophylline has been investigated in a randomized controlled trial for the prevention of vasomotor nephropathy in very preterm neonates with RDS, showing a significant improvement in GFR, compared to placebo [30]. According to one study in human preterm infants, urine flow rate, water output/input ratio, and creatinine clearance increased significantly after the administration of caffeine [31]. In the AWAKEN cohort, premature infants who received caffeine had much lower rates of AKI than those who did not receive caffeine, even after adjustment for confounding variables [32].
Acute kidney injury
The incidence of AKI is up to 26% in ELBW infants. AKI may influence ongoing nephron development and also represents a condition in which nephrons can be lost. Recently an exhaustive review [33] has investigated the impact of AKI following preterm birth on development of kidney failure. In very low birth weight (VLBW) infants (birth weight of less than 1500 g) or neonates born at less than 33 weeks of gestation, conclusions from the reviewed studies suggested a relationship between AKI and increased risk of kidney failure, as proven by abnormal findings at 3–7.5 years: low GFR, low kidney volume, arterial hypertension, proteinuria, and even CKD stage 5. The main limitations of all these studies were the small numbers of participants, who were subject to bias and confounders, and the lack of information on comorbidities in NICU and on superimposed events in early childhood (catch-up growth, nephrotoxic medications, urinary tract infections, immunologic factors). Interestingly, approximately 90% of infants with neonatal AKI recover normal kidney function and survive to hospital discharge [27].
In order to minimize all the possible consequences of AKI, a crucial point is the prompt identification of kidney insufficiency in every infant cared for in NICUs.
Over the years, three definitions of AKI in critically ill patients, all based on urine output and variations of plasma creatinine levels, have been adapted to newborn infants in order to cope with the peculiar kidney physiopathology during the perinatal life: pediatric Risk Injury Failure Loss End Stage (pRIFLE), Acute Kidney Injury Network (AKIN), and Kidney Disease Improving Global Outcome (KDIGO).
In 2013, the National Institutes of Health–sponsored workshop proposed neonatal modifications from the KDIGO pediatric AKI definition, using plasma creatinine and urine output criteria, as the best available approach to define AKI [34] (Table 1). This definition has been validated in multicenter, multinational, observational studies in critically ill newborns [27] and more recently in extremely low gestational age neonates [35].
Even if the definition of AKI may need to be refined over time, the neonatal KDIGO approach allows clinicians to identify the existence and the severity of AKI and thus anticipate the associated complications, mainly water retention and hyponatremia. In situations of established AKI, the rate of glomerular filtration should be repeatedly estimated in order to adapt the dosage of medications cleared by the kidney, and detect a progression towards kidney failure [36].
Patent ductus arteriosus
PDA is a well-known factor associated with increased risk of AKI in preterm infants, with a large number of studies [37] reporting the deleterious effects of non-selective COX inhibitors, ibuprofen and indomethacin, on kidney function (decreased GFR and creatinine clearance, water retention, and hyponatremia). In a study by De Cock and colleagues, ibuprofen used for PDA closure impaired the clearance of amikacin by reducing GFR, thus presumably increasing aminoglycoside nephrotoxicity [38]. One recent study [39] showed that, independently of non-steroidal anti-inflammatory drug administration, hemodynamically significant PDA can, itself, be a major risk factor for developing AKI in VLBW infants. Increased peaks in plasma creatinine preceded ibuprofen administration in very preterm infants under care for PDA, due to pathologic shunting of blood flow decreasing kidney perfusion [40]. Kidney-protective strategies in infants with PDA should aim at avoiding volume overload and maintaining kidney perfusion.
Late deleterious effects of indomethacin
Long-standing kidney structural changes have been described at 30 days and 6 months (equivalent to human adulthood) in a rat model exposed to indomethacin during early neonatal life [41]. These consisted in persistent electron microscopy abnormalities of the glomerular basement membrane and reduced number of nephrons.
Nephrotoxic drugs
As in the reported case, ELBW infants can be concerned by several clinical scenarios, in which both the illness itself and the medications used for its treatment are risk factors for AKI. Awareness and tight collaboration between neonatologists and pediatric nephrologists are advocated in the clinical management of these situations. The reader is referred to the educational review of Murphy and colleagues [42] for a more detailed description of the concept.
IUGR—which is the best postnatal growth?
IUGR is often due to placental insufficiency which leads to chronic fetal hypoxia. Human studies have shown that, in this condition, Doppler anomalies and reduced kidney perfusion are associated with altered kidney morphology and reduced fetal kidney size at different gestational ages [43]. In our case, extreme preterm birth was associated with IUGR, and this makes it difficult to discriminate the effect of preterm birth from the effect of IUGR on nephron endowment and loss. Only one study by Keijzer-Veen et al. [44] explored the long-term consequences of IUGR on kidney size in preterm infants born at less than 32 weeks of gestation. In that cohort, kidney ultrasound revealed significantly smaller kidney length and volume in 20-year-old female individuals born prematurely compared with full term–matched controls, but did not find any difference between SGA and AGA preterm infants. In infants born at less than 1000 g or less than 30 weeks of gestation—both with IUGR and born AGA but developing extrauterine growth restriction—GFR, measured by inulin clearance at school-age, was significantly lower compared to infants of similar gestational age with appropriate pre- and postnatal growth [45]. In that study, factors associated with lower GFR were postnatal corticosteroid exposure and, in infants with extra-uterine growth restriction, lower protein intakes during the first week of life. This is consistent with animal data showing that nephron density is directly related to protein nutrition status during nephrogenesis [46]. All these data suggest that increasing protein intake during nephrogenesis could minimize the risk of long-term morbidities associated with oligonephropathy. However, animal models show contrasting results regarding long-term effects of postnatal nutrition in a context of low nephron endowment, as both overfeeding and food restriction have been associated with chronic kidney dysfunction and nephron deficit in IUGR and AGA rats [47, 48]. Similarly, if early growth failure has been proven to be deleterious for nephrogenesis in human ELBW infants, the long-term effects on kidney function of very high intakes of protein according to recent nutrition guidelines [49] deserve further investigation. Finally, the relationship between post-discharge growth trajectories and kidney function in early childhood of ELBW infants remains to be fully elucidated.
Follow-up and treatment
Validated guidelines for the identification and for starting treatment of subjects with hyperfiltration among infants born preterm and/or with LBW are not yet available. However, the need of regular monitoring of preterm and LBW individuals throughout life has been recently underlined by the Low Birth and Nephron Number Working Group [50] and, based on this report, a summary of recommendations for the follow up of at-risk preterm infants is proposed in Table 2. The adherence to these recommendations and a multidisciplinary approach to the possible consequences of low nephron endowment should become a common practice in NICUs.
Conclusion
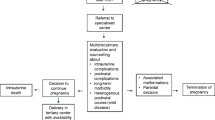
Our case report shows that, despite recovery from AKI at NICU discharge, baseline risk factors, prolonged postnatal stress, and morbidities may impair nephrogenesis and may lead to CKD at early adulthood in ELBW infants. This educational review illustrates that awareness, screening, and prevention of CKD in extremely preterm infants should start in the NICU. First, the likelihood of CKD and kidney failure should be mentioned while offering parent counseling and should be given full consideration in decision-making processes at the edge of neonatal viability. Second, the early implementation of kidney-protecting strategies should be considered starting from birth, to minimize the risk leading toward CKD in ELBW infants. Some recommended actions that could have long-term benefits on renal health in at-risk infants are clearly identified, as also suggestions for research studies needed in the field.
Key summary points
-
1.
Progresses in the care of low birth weight neonates increase the occurrence of comorbidities in the survivors. While the respiratory and the neurodevelopmental consequences are rather well defined, the late renal consequences of prematurity and/or low birth weight remain ill-defined.
-
2.
Clinical observations and experimental studies have shown that low birth weight is associated with a congenital deficit in the number of nephrons. Postnatal growth of the kidneys does not compensate for the severe deficits in nephron endowment.
-
3.
A decreased number of nephrons is compensated by the hyperfiltration of existing nephrons. While this compensatory hyperfiltration is useful in maintaining the organism homeostasis, it ultimately leads to premature death of the hyperfiltering nephrons. Progressive terminal failure occurs, the first sign of the kidney suffering being the occurrence of proteinuria.
-
4.
Angiotensin II appears to play a key role in the pathogenesis of the compensatory hyperfiltration of surviving nephrons. Blocking the renin–angiotensin system with angiotensin-converting enzyme inhibitors or angiotensin II antagonists prevents the occurrence of the glomerular compensation and protects the kidney. Interfering with the action of angiotensin II in young children is however a difficult decision.
-
5.
The optimal care of premature infants should include measures that concern all organs, including the brain, the lungs, and the kidneys. The NICU definitely needs a pilot to coordinate the various therapeutic measures taken by the relevant specialists.
Multiple-choice questions (answers are given following the references)
-
1.
Which of the following statements concerning human nephrogenesis is false?
-
a)
In infants born at term, nephrogenesis has ceased before birth.
-
b)
There is a wide range of nephron number within and among various healthy populations.
-
c)
Most of the nephrons are formed during the third trimester of pregnancy.
-
d)
In infants born at less than 32 weeks of gestation, nephrogenesis can continue up to a postconceptional age of 40 weeks in the absence of a kidney injury.
-
e)
Among infants born at term, the variability in nephron number is especially influenced by their birth weight.
-
2.
Which of the following statements regarding the compensatory hyperfiltration phenomenon is true?
-
a)
It can never concern infants born extremely preterm, as their glomerular filtration rate is very low.
-
b)
The underlying mechanism is a predominant pre-glomerular vasodilation.
-
c)
It is mediated by the overactivation of intrarenal adenosine.
-
d)
Can lead to ongoing injury to podocytes and to the glomerular microvasculature if it persists.
-
e)
It is always preceded by acute kidney injury during neonatal life.
-
3.
Acute kidney injury in ELBW infants has been associated with the following abnormal findings in childhood:
-
a)
Low glomerular filtration rate.
-
b)
Low kidney size.
-
c)
Arterial hypertension.
-
d)
Proteinuria.
-
e)
All the above.
-
4.
Animal studies regarding nutrition and nephron deficit have shown that:
-
a)
Overfeeding has been associated with chronic kidney dysfunction and nephron deficit in animals with intrauterine growth restriction (IUGR).
-
b)
Food restriction has been associated with chronic kidney dysfunction and nephron deficit in IUGR.
-
c)
Overfeeding has been associated with chronic kidney dysfunction and nephron deficit even in the absence of IUGR.
-
d)
Nephron density is directly related to protein nutrition status during nephrogenesis.
-
e)
All the above.
Change history
10 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00467-021-05412-1
References
Glass HC, Costarino AT, Stayer SA, Brett CM, Cladis F, Davis PJ (2015) Outcomes for extremely premature infants. Anesth Analg 120:1337–1351. https://doi.org/10.1213/ANE/0000000000000705
Brumbaugh JE, Hansen NI, Bell EF, Sridhar A, Carlo WA, Hintz SR, Vohr BR, Colaizy TT, Duncan AF, Wyckoff MH, Baack ML, Rysavy MA, DeMauro SB, Stoll BJ, Das A, Higgins RD; National Institute of Child Health and Human Development Neonatal Research Network (2019) Outcomes of extremely preterm infants with birth weight less than 400 g. JAMA Pediatr 173:434–445. https://doi.org/10.1001/jamapediatrics.2019.0180
Pascal A, Govaert P, Oostra A, Naulaers G, Ortibus E, Van den Broeck C (2018) Neurodevelopmental outcome in very preterm and very-low-birthweight infants born over the past decade: a meta-analytic review. Dev Med Child Neurol 60:342–355. https://doi.org/10.1111/dmcn.13675
Vikse BE, Irgens LM, Leivestad T, Hallan S, Iversen BM (2008) Low birth weight increases risk for end-stage renal disease. J Am Soc Nephrol 19:151–157. https://doi.org/10.1681/ASN.2007020252
Ruggajo P, Skrunes R, Svarstad E, Skjærven R, Reisæther AV, Vikse BE (2016) Familial factors, low birth weight, and development of ESRD: a nationwide registry study. Am J Kidney Dis 67:601–608. https://doi.org/10.1053/j.ajkd.2015.11.015
Hirano D, Ishikura K, Uemura O, Ito S, Wada N, Hattori M, Ohashi Y, Hamasaki Y, Tanaka R, Nakanishi K, Kaneko T, Honda M (2016) Association between low birth weight and childhood-onset chronic kidney disease in Japan: a combined analysis of a nationwide survey for paediatric chronic kidney disease and the National Vital Statistics Report. Nephrol Dial Transplant 31:1895–1900. https://doi.org/10.1093/ndt/gfv425
Crump C, Sundquist J, Winkleby MA, Sundquist K (2019) Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ 365:l1346. https://doi.org/10.1136/bmj.l1346
Rodríguez MM, Gómez AH, Abitbol CL, Chandar JJ, Duara S, Zilleruelo GE (2004) Histomorphometric analysis of postnatal glomerulogenesis in extremely preterm infants. Pediatr Dev Pathol 7:17–25. https://doi.org/10.1007/s10024-003-3029-2
Hughson M, Farris AB 3rd, Douglas-Denton R, Hoy WE, Bertram JF (2003) Glomerular number and size in autopsy kidneys: the relationship to birth weight. Kidney Int 63:2113–2122. https://doi.org/10.1046/j.1523-1755.2003.00018.x
Merlet-Bénichou C, Gilbert T, Vilar J, Moreau E, Freund N, Lelièvre-Pégorier M (1999) Nephron number: variability is the rule. Causes and consequences. Lab Invest 79:515–527
Simeoni U, Ligi I, Buffat C, Boubred F (2011) Adverse consequences of accelerated neonatal growth: cardiovascular and renal issues. Pediatr Nephrol 26:493–508. https://doi.org/10.1007/s00467-010-1648-1
Ryan D, Sutherland MR, Flores TJ, Kent AL, Dahlstrom JE, Puelles VG, Bertram JF, McMahon AP, Little MH, Moore L, Black MJ (2018) Development of the human fetal kidney from mid to late gestation in male and female infants. EBioMedicine 27:275–283. https://doi.org/10.1016/j.ebiom.2017.12.016
Sutherland MR, Gubhaju L, Moore L, Kent AL, Dahlstrom JE, Horne RS, Hoy WE, Bertram JF, Black MJ (2011) Accelerated maturation and abnormal morphology in the preterm neonatal kidney. J Am Soc Nephrol 22:1365–1374. https://doi.org/10.1681/ASN.2010121266
Brenner BM, Lawler EV, Mackenzie HS (1996) The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int 49:1774–1777. https://doi.org/10.1038/ki.1996.265
Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW (2012) Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol 8:293–300. https://doi.org/10.1038/nrneph.2012
Klahr S, Morrissey JJ (2000) The role of vasoactive compounds, growth factors and cytokines in the progression of renal disease. Kidney Int Suppl 75:S7-14
Charlton JR, Baldelomar EJ, Hyatt DM, Bennett KM (2021) Nephron number and its determinants: a 2020 update. Pediatr Nephrol 36:797–807. https://doi.org/10.1007/s00467-020-04534-2
Charlton JR, Baldelomar EJ, deRonde KA, Cathro HP, Charlton NP, Criswell SJ, Hyatt DM, Nam S, Pearl V, Bennett KM (2020) Nephron loss detected by MRI following neonatal acute kidney injury in rabbits. Pediatr Res 87:1185–1192. https://doi.org/10.1038/s41390-019-0684-1
Chevalier RL (2017) Evolutionary Nephrology. Kidney Int Rep 2:302–317. https://doi.org/10.1016/j.ekir.2017.01.012
Guignard JP, Torrado A, Mazouni SM, Gautier E (1976) Renal function in respiratory distress syndrome. J Pediatr 88:845–850. https://doi.org/10.1016/s0022-3476(76)81129-8
Toth-Heyn P, Drukker A, Guignard JP (2000) The stressed neonatal kidney: from pathophysiology to clinical management of neonatal vasomotor nephropathy. Pediatr Nephrol 14:227–239. https://doi.org/10.1007/s004670050048
Popescu CR, Sutherland MR, Cloutier A, Benoît G, Bertagnolli M, Yzydorczyk C, Germain N, Phan V, Lelièvre-Pegorier M, Sartelet H, Nuyt AM (2013) Hyperoxia exposure impairs nephrogenesis in the neonatal rat: role of HIF-1α. PLoS ONE 8:e82421. https://doi.org/10.1371/journal.pone.0082421
Staub E, Dahl MJ, Yost C, Bowen S, Aoki T, Blair A, Wang Z, Null DM, Yoder BA, Albertine KH (2017) Preterm birth and ventilation decrease surface density of glomerular capillaries in lambs, regardless of postnatal respiratory support mode. Pediatr Res 82:93–100. https://doi.org/10.1038/pr.2017.1
Guignard JP, Ali US (2016) Acute renal failure in the neonate. J Pediatr Intensive Care 5:42–49. https://doi.org/10.1055/s-0035-1564735
Perico N, Askenazi D, Cortinovis M, Remuzzi G (2018) Maternal and environmental risk factors for neonatal AKI and its long-term consequences. Nat Rev Nephrol 14:688–703. https://doi.org/10.1038/s41581-018-0054-y
Nada A, Bonachea EM, Askenazi DJ (2017) Acute kidney injury in the fetus and neonate. Semin Fetal Neonatal Med 22:90–97. https://doi.org/10.1016/j.siny.2016.12.001
Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, Chishti AS, Woroniecki R, Mammen C, Swanson JR, Sridhar S, Wong CS, Kupferman JC, Griffin RL, Askenazi DJ, NK Collaborative (NKC) (2017) Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health 1:184–194. https://doi.org/10.1016/S2352-4642(17)30069-X
Bonsante F, Ramful D, Binquet C, Samperiz S, Daniel S, Gouyon JB, Iacobelli S (2019) Low renal oxygen saturation at near-infrared spectroscopy on the first day of life is associated with developing acute kidney injury in very preterm infants. Neonatology 115:198–204. https://doi.org/10.1159/000494462
Guignard JP, Iacobelli S (2020) Diuretics. In: Aranda JN, Van Den Anker JV (eds) Neonatal and pediatric pharmacology: therapeutic principles in practice, 5th edn. Wolters Kluwer Health, Philadelphia, pp 765–779
Cattarelli D, Spandrio M, Gasparoni A, Bottino R, Offer C, Chirico G (2006) A randomised, double blind, placebo-controlled trial of the effect of theophylline in prevention of vasomotor nephropathy in very preterm neonates with respiratory distress syndrome. Arch Dis Child Fetal Neonatal Ed 91:F80–F84. https://doi.org/10.1136/adc.2005.073650
Gillot I, Gouyon JB, Guignard JP (1990) Renal effects of caffeine in preterm infants. Biol Neonat 58:133–136. https://doi.org/10.1159/000243252
Harer MW, Askenazi DJ, Boohaker LJ, Carmody JB, Griffin RL, Guillet R, Selewski DT, Swanson JR, Charlton JR, National Kidney Collaborative (NKC), (2018) Association between early caffeine citrate administration and risk of acute kidney injury in preterm neonates: results from the AWAKEN Study. JAMA Pediatr 172:e180322. https://doi.org/10.1001/jamapediatrics.2018.0322
Harer MW, Charlton JR, Tipple TE, Reidy KJ (2020) Preterm birth and neonatal acute kidney injury: implications on adolescent and adult outcomes. J Perinatol 40:1286–1295. https://doi.org/10.1038/s41372-020-0656-7
Zappitelli M, Ambalavanan N, Askenazi DJ, Moxey-Mims MM, Kimmel PL, Star RA, Abitbol CL, Brophy PD, Hidalgo G, Hanna M, Morgan CM, Raju TNK, Ray P, Reyes-Bou Z, Roushdi A, Goldstein SL (2017) Developing a neonatal acute kidney injury research definition: a report from the NIDDK neonatal AKI workshop. Pediatr Res 82:569–573. https://doi.org/10.1038/pr.2017.136
Askenazi DJ, Heagerty PJ, Schmicker RH, Griffin R, Brophy P, Juul SE, Mayock DE, Goldstein SL, Hingorani S; PENUT Trial Consortium (2020) Prevalence of acute kidney injury (AKI) in extremely low gestational age neonates (ELGAN). Pediatr Nephrol 35:1737–1748. https://doi.org/10.1007/s00467-020-04563-x
Iacobelli S, Guignard JP (2021) Maturation of glomerular filtration rate in neonates and infants: an overview. Pediatr Nephrol 36:1439–1446. https://doi.org/10.1007/s00467-020-04632-1
Ohlsson A, Walia R, Shah SS (2020) Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants. Cochrane Database Syst Rev 2:CD003481. https://doi.org/10.1002/14651858.CD003481
De Cock RF, Allegaert K, Schreuder MF, Sherwin CM, de Hoog M, van den Anker JN, Danhof M, Knibbe CA (2012) Maturation of the glomerular filtration rate in neonates, as reflected by amikacin clearance. Clin Pharmacokinet 51:105–117. https://doi.org/10.2165/11595640-000000000-00000
Guillet R, Selewski DT, Griffin R, Rastogi S, Askenazi DJ, D’Angio CT, National Kidney Collaborative (2021) Relationship of patent ductus arteriosus management with neonatal AKI. J Perinatol 41:1441–1447. https://doi.org/10.1038/s41372-021-01054-1
Iacobelli S, Bonsante F, Ferdinus C, Labenne M, Gouyon JB (2009) Factors affecting postnatal changes in serum creatinine in preterm infants with gestational age <32 weeks. J Perinatol 29:232–236. https://doi.org/10.1038/jp.2008.203
Kent AL, Koina ME, Gubhaju L, Cullen-McEwen LA, Bertram JF, Lynnhtun J, Shadbolt B, Falk MC, Dahlstrom JE (2014) Indomethacin administered early in the postnatal period results in reduced glomerular number in the adult rat. Am J Physiol Renal Physiol 307:F1105-1110. https://doi.org/10.1152/ajprenal.00328.2014
Murphy HJ, Thomas B, Van Wyk B, Tierney SB, Selewski DT, Jetton JG (2020) Nephrotoxic medications and acute kidney injury risk factors in the neonatal intensive care unit: clinical challenges for neonatologists and nephrologists. Pediatr Nephrol 35:2077–2088. https://doi.org/10.1007/s00467-019-04350-3
Konje JC, Okaro CI, Bell SC, de Chazal R, Taylor DJ (1997) A cross-sectional study of changes in fetal renal size with gestation in appropriate- and small for-gestational-age fetuses. Ultrasound Obstet Gynecol 10:22–26. https://doi.org/10.1046/j.1469-0705.1997.10010022.x
Keijzer-Veen MG, Devos AS, Meradji M, Dekker FW, Nauta J, van der Heijden BJ (2010) Reduced renal length and volume 20 years after very preterm birth. Pediatr Nephrol 25:499–507. https://doi.org/10.1007/s00467-009-1371-y
Bacchetta J, Harambat J, Dubourg L, Guy B, Liutkus A, Canterino I, Kassaï B, Putet G, Cochat P (2009) Both extrauterine and intrauterine growth restriction impair renal function in children born very preterm. Kidney Int 76:445–452. https://doi.org/10.1038/ki.2009.201
Yeung MY (2006) Oligonephropathy, developmental programming and nutritional management of low-gestation newborns. Acta Paediatr 95:263–267. https://doi.org/10.1080/08035250500440394
Schreuder MF, Nyengaard JR, Remmers F, van Wijk JA, Delemarre-van de Waal HA (2006) Postnatal food restriction in the rat as a model for a low nephron endowment. Am J Physiol Renal Physiol 291:F1104-1107. https://doi.org/10.1152/ajprenal.00158.2006
Boubred F, Daniel L, Buffat C, Feuerstein JM, Tsimaratos M, Oliver C, Dignat-George F, Lelièvre-Pégorier M, Simeoni U (2009) Early postnatal overfeeding induces early chronic renal dysfunction in adult male rats. Am J Physiol Renal Physiol 297:F943-951. https://doi.org/10.1152/ajprenal.90704.2008
van Goudoever JB, Carnielli V, Darmaun D, de Pipaon S, M; ESPGHAN, ESPEN, ESPR, CSPEN working group on pediatric parenteral nutrition, (2018) ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Amino acids. Clin Nutr 37:2315–2323. https://doi.org/10.1016/j.clnu.2018.06.945
Luyckx VA, Perico N, Somaschini M, Manfellotto D, Valensise H, Cetin I, Simeoni U, Allegaert K, Vikse BE, Steegers EA, Adu D, Montini G, Remuzzi G, Brenner BM; writing group of the Low Birth Weight and Nephron Number Working Group (2017) A developmental approach to the prevention of hypertension and kidney disease: a report from the Low Birth Weight and Nephron Number Working Group. Lancet 390:424–428. https://doi.org/10.1016/S0140-6736(17)30576-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Answers
1. d; 2. d; 3. e; 4. e
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: during the processing of the article, Table 1 and Table 2 were missing in the first published version of this article. The missing Tables were added to this article.
Rights and permissions
About this article
Cite this article
Iacobelli, S., Guignard, JP. When the progresses in neonatology lead to severe congenital nephron deficit: is there a pilot in the NICU?. Pediatr Nephrol 37, 1277–1284 (2022). https://doi.org/10.1007/s00467-021-05338-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05338-8