Abstract
Background
Autosomal recessive polycystic kidney disease (ARPKD) constitutes an important cause of pediatric end stage renal disease and is characterized by a broad phenotypic variability. The disease is caused by mutations in a single gene, Polycystic Kidney and Hepatic Disease 1 (PKHD1), which encodes a large transmembrane protein of poorly understood function called fibrocystin. Based on current knowledge of genotype–phenotype correlations in ARPKD, two truncating mutations are considered to result in a severe phenotype with peri- or neonatal mortality. Infants surviving the neonatal period are expected to carry at least one missense mutation.
Case-Diagnosis/Treatment
We report on a female patient with two truncating PKHD1 mutations who survived the first 30 months of life without renal replacement therapy. Our patient carries not only a known stop mutation, c.8011C>T (p.Arg2671*), but also the previously reported c.51A>G PKHD1 sequence variant of unknown significance in exon 2. Using functional in vitro studies we have confirmed the pathogenic nature of c.51A>G, demonstrating activation of a new donor splice site in intron 2 that results in a frameshift mutation and generation of a premature stop codon.
Conclusions
This case illustrates the importance of functional mutation analyses and also raises questions regarding the current belief that the presence of at least one missense mutation is necessary for perinatal survival in ARPKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autosomal recessive polycystic kidney disease (ARPKD) is a rare disorder with an estimated incidence of 1 in 20,000. Autosomal recessive polycystic kidney disease (ARPKD) is a rare disorder with an estimated incidence of 1 in 20,000 and one of the most severe conditions leading to end stage renal disease in childhood. The ARPKD phenotype is characterized by collecting duct tubular dilatations and progressively developing renal cysts that result in bilateral massive renal enlargement. There is also congenital hepatic fibrosis due to ductal plate malformation [1, 2]. Current treatment approaches are aimed at treating symptoms and are based on expert recommendations [3]. ARPKD is caused by mutations in a single gene, Polycystic Kidney and Hepatic Disease 1 (PKHD1), which encodes a ciliary protein of poorly understood function called fibrocystin [4]. Genotype–phenotype correlations in ARPKD remain loosely defined, and interpretation of genotypes is challenged by the large number of more than 700 known—mostly private—mutations [5, 6] and a complex PKHD1 splicing pattern [7, 8]. The widely accepted current understanding is that patients with two truncating mutations show a severe phenotype with peri- or neonatal mortality, whereas patients surviving the neonatal period carry at least one milder non-truncating missense mutation. However, the presence of two missense mutations does not guarantee neonatal survival [5, 9].
Case report
We report on a patient with an unexpected genotype–phenotype correlation. The female patient was born as the fourth child of healthy, non-consanguineous Turkish parents (mother G7P4) after 31 + 1 weeks of pregnancy by spontaneous delivery. Birth weight was 2010 g with APGAR scores of 6/8/8 after 1, 5 and 10 min, respectively. After 26 weeks of gestation oligohydramnion and enlarged echogenic kidneys with cysts had become evident. Due to pulmonary hypoplasia with pulmonary hypertension, the patient required high-frequency oscillation ventilation with nitric oxide.
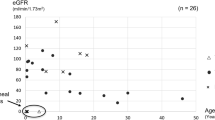
Despite the complicated clinical course with massively enlarged kidneys (Fig. 1a), pulmonary hypoplasia, progressive portal fibrosis, arterial hypertension, multiple episodes of sepsis and renal mycosis within the first year of life, renal function remained relatively stable without the need of renal replacement during the first 30 months of life (Fig. 1b). Platelet counts showed a slow continuous decrease compatible with portal hypertension (Fig. 1b). At age 30 months body weight was between the 50th and 75th percentile and height was at the 10th percentile. In summary, the patient showed a satisfactory clinical development despite her severe renal, hepatic and pulmonary phenotype.
a Magnetic resonance imaging (coronal fat-suppressed and contrast-enhanced T1-FFE-sequence) of the abdomen shows pronounced renal hyperplasia, hepatomegaly and dilatation of intrahepatic bile ducts. b Serum creatinine levels (μmol/l; red line) and platelet counts (counts/nl; gray line) during the first 30 months of life. Peaks of serum creatinine levels were detected during infections. c Functional study approach of the Polycystic Kidney and Hepatic Disease 1 (PKHD1) c.51A>G mutation. PCR amplification of wild-type (WT) cDNA shows the normal functionally spliced fragment; mutated cDNA (Mut) shows aberrant splicing. d Sequencing confirms the point mutation. Aberrant splicing is expected to result in a truncated protein due to an early stop codon in intron 2 (AA amino acids). e Pedigree of the family with PKHD1 genotypes indicates that the phenotype segregates with the genotype. n.a. Not available, wt wild type
Review of the family history revealed a male infant had been born with Potter’s sequence at 34 + 6 weeks of gestational age in another major hospital in Germany 12 years earlier. Anhydramnios and enlarged kidneys were detected several days prior to birth. The postnatal course was complicated by unilateral tension pneumothorax, contralateral atelectasis of the lung and progressive renal insufficiency with anuria. The infant died at 2 weeks of age. Two other children are currently clinically healthy.
A gene panel analysis of the patient for 4813 known genes (including PKD1, PKD2, Hepatocyte Nuclear Factor-1Beta, and multiple ciliopathy genes) causing Mendelian disorders was performed using a next generation sequencing approach (TruSight One Sequencing Panel; Illumina Inc., San Diego, CA). Two compound heterozygous mutations were detected in the PKHD1 gene: a previously reported nonsense mutation c.8011C>T (p.Arg2671*) in exon 50 [4] and a potential splice site mutation c.51A>G close to the splice donor site of exon 2 that had also already been reported [5]. However, the functional relevance of this second mutation remained unclear [5].
To provide functional clarification of this potential splice site mutation, we performed in silico analysis and in vitro minigene assays. The results of the in silico studies suggested an effect on PKHD1 splicing that resulted in the use of an alternative splice site located 31 bp downstream into intron 2. To assess the functional effect of the c.51A>G mutation, we then performed a minigene assay in human embryonic kidney 293 T cells. In short, cells were transfected with cloned wild-type (WT) or mutated PKHD1 DNA covering the genomic PKHD1 region from intron 1 to intron 3. PCR amplification of the WT cDNA showed a normal functionally spliced section with a 129-bp amplicon compared to a 160-bp amplicon of the mutant. Sequencing of the larger mutant cDNA fragment demonstrated activation of the alternative downstream splice donor site (Fig. 1c, d). The use of this downstream splicing site leads to a frameshift and an early stop codon in intron 2 which is expected to result in loss-of-function of the protein either by a heavy truncation or by nonsense-mediated decay.
To analyze the molecular penetrance of the splice site mutation and to exclude remaining activity of the mutated splice site we performed PCR on cDNA of cultivated primary urinary cells obtained from the patient and from an appropriate sex- and age-matched control using the primers described for the minigene assay. PCR confirmed our minigene assay results. Subsequently, we transformed the WT-sized DNA fragment of the patient and the control into bacteria and sequenced 189 or 100 clones, respectively. Of 189 patient clones we found that all WT-sized clones were sequenced as WT. Not a single WT-sized clone carrying the splice site mutation could be detected. As expected, the examined 100 clones of the control were shown to be WT. These findings suggest that the splice site mutation is highly relevant and most likely leads to a loss-of-function of fibrocystin.
Sequencing of familial DNA confirmed segregation of the phenotype with the PKHD1 mutations. We detected the stop mutation on maternal alleles and the splice-site mutation on paternal alleles. DNA sequencing of DNA of the deceased brother showed both mutations, whereas the healthy sister born in 2004 carries no mutations. No further mutations in known ciliopathy genes were detected by the next generation sequencing analysis in our patient (Fig. 1e).
Discussion
The phenotypic scope of ARPKD ranges from fetal mortality or severely affected newborns with a persistent high mortality to mildly affected adults [5, 9–11]. Although substantial knowledge on ciliopathies has emerged, fibrocystin function and the pathophysiologic basis for the phenotypic variability in ARPKD remain unclear. Interpretation of PKHD1 gene mutations is hampered by its large size, with >700 known PKHD1 mutations (http://www.humgen.rwth-aachen.de/) in the entire gene, and an extensive pattern of alternative splicing. The function of the alternative transcripts remain unclear [5, 9, 11, 12]. Limited genotype–phenotype correlations have been proposed. It has been suggested that patients with two truncating mutations show severe phenotype with neo- or perinatal mortality, whereas at least one milder missense mutation would be required for an infant to survive the neonatal period [5, 13].
The case presented in this study challenges this prevailing belief. We report a female child with progressive chronic kidney disease and signs of portal hypertension at the age of 1.5 years but without the need of renal replacement therapy during the first 30 months of life despite the occurrence of two truncating mutations. The case also emphasizes the importance of functional analysis of mutations with unknown relevance. However, analyses of the functional consequences of a specific mutation are not performed on a routine basis, but generally within the context of research, explaining why a large number of variants remain with an unproven or uncertain pathogenicity.
Several aspects need to be considered when presenting possible explanations for the unexpected clinical course of the patient described herein. Clearly, medical progress plays a role in the current management of ARPKD patients. There have been major advances in the fields of neonatal intensive care and pediatric nephrology. Perinatal outcome of severely affected preterm infants in general and ARPKD patients specifically has improved. The course of our patient may represent refinement of the possibilities, especially when the deceased sibling is taken into consideration.
Furthermore, differences in the severity of clinical manifestation, especially between siblings with the identical genotype, might be much more attributable to alternative or dysregulated splicing of PKHD1 than previously assumed [6, 14]. Alternatively, co-occurring mutations in other PKD-associated genes or epigenetic alterations may modify the phenotype. The identified splice site mutation c.51A>G, which was initially reported as synonymous missense variant p.Ala17Ala [5], leads to the disruption of the natural splice donor site of exon 2 at position c.52, causing retention of nucleotides from intron 2 with subsequent generation of a premature stop codon (p.Val18Glyfs*3). Nonsense-mediated decay is the most likely fate of the mRNA from both parental PKHD1 copies. Since our functional studies point to usage of an alternative downstream splice site resulting in a frameshift with protein truncation with high penetrance, we suggest changing the nomenclature for this mutation to c.51A>G (p.Val18Glyfs*3).
A recent publication reported the survival of four unrelated patients with homozygous truncating mutations in association with parental consanguinity [6]. In contrast to these patients, our patient is a child of non-consanguineous Turkish parents with compound heterozygous PKHD1 mutations, thus adding important evidence for a potential wider occurrence of biallelic truncating mutations.
Our case shows that considerable prudence is called for when the concept of neo- or perinatal mortality in patients with two truncating mutations is taken into genetic counseling. Furthermore, prenatal and genetic counseling must keep pace with growing understanding of functional ciliary biology. While neonatal mortality or survival is of obvious importance in ARPKD, severity of hepatorenal involvement in early childhood with a potential need for dialysis or transplantation of kidney, liver or both, may also be an important aspect of genetic counseling. Detailed observations of large deeply phenotyped ARPKD cohorts will be needed to add profound evidence for future recommendations on treatment and predictions of clinical courses. We have therefore recently established a web-based registry study that may give valuable insights within the next years [15].
References
Harris PC, Torres VE (2009) Polycystic kidney disease. Annu Rev Med 60:321–337
Hartung EA, Guay-Woodford LM (2014) Autosomal recessive polycystic kidney disease: a hepatorenal fibrocystic disorder with pleiotropic effects. Pediatrics 134:e833–e845
Guay-Woodford LM, Bissler JJ, Braun MC, Bockenhauer D, Cadnapaphornchai MA, Dell KM, Kerecuk L, Liebau MC, Alonso-Peclet MH, Shneider B, Emre S, Heller T, Kamath BM, Murray KF, Moise K, Eichenwald EE, Evans J, Keller RL, Wilkins-Haug L, Bergmann C, Gunay-Aygun M, Hooper SR, Hardy KK, Hartung EA, Streisand R, Perrone R, Moxey-Mims M (2014) Consensus expert recommendations for the diagnosis and management of autosomal recessive polycystic kidney disease: report of an international conference. J Pediatr 165:611–617
Ward CJ, Hogan MC, Rossetti S, Walker D, Sneddon T, Wang X, Kubly V, Cunningham JM, Bacallao R, Ishibashi M, Milliner DS, Torres VE, Harris PC (2002) The gene mutated in autosomal recessive polycystic kidney disease encodes a large, receptor-like protein. Nat Genet 30:259–269
Bergmann C, Senderek J, Windelen E, Küpper F, Middeldorf I, Schneider F, Dornia C, Rudnik-Schöneborn S, Konrad M, Schmitt CP, Seeman T, Neuhaus TJ, Vester U, Kirfel J, Büttner R, Zerres K, APN (Arbeitsgemeinschaft für Pädiatrische Nephrologie), (2005) Clinical consequences of PKHD1 mutations in 164 patients with autosomal-recessive polycystic kidney disease (ARPKD). Kidney Int 67:829–848
Frank V, Zerres K, Bergmann C (2014) Transcriptional complexity in autosomal recessive polycystic kidney disease. Clin J Am Soc Nephrol 9:1729–1736
Nagasawa Y, Matthiesen S, Onuchic LF, Hou X, Bergmann C, Esquivel E, Senderek J, Ren Z, Zeltner R, Furu L, Avner E, Moser M, Somlo S, Guay-Woodford L, Büttner R, Zerres K, Germino GG (2002) Identification and characterization of Pkhd1, the mouse orthologue of the human ARPKD gene. J Am Soc Nephrol 13:2246–2258
Onuchic LF, Furu L, Nagasawa Y, Hou X, Eggermann T, Ren Z, Bergmann C, Senderek J, Esquivel E, Zeltner R, Rudnik-Schöneborn S, Mrug M, Sweeney W, Avner ED, Zerres K, Guay-Woodford LM, Somlo S, Germino GG (2002) PKHD1, the polycystic kidney and hepatic disease 1 gene, encodes a novel large protein containing multiple immunoglobulin-like plexin-transcription-factor domains and parallel beta-helix 1 repeats. Am J Hum Genet 70:1305–1317
Denamur E, Delezoide A-L, Alberti C, Bourillon A, Gubler MC, Bouvier R, Pascaud O, Elion J, Grandchamp B, Michel-Calemard L, Missy P, Zaccaria I, Le Nagard H, Gerard B, Loirat C, Société Française de Foetopathologie, Barbet J, Beaufrère AM, Berchel C, Bessières B, Boudjemaa S, Buenerd A, Carles D, Clemenson A, Dechelotte P, Devisme L, Dijoud F, Espérandieu O, Fallet C, Gonzalès M, Hillion Y, Jacob B, Joubert M, Kermanach P, Lallemand A, Laquerrière A, Laurent N, Liprandi A, Loeuillet L, Loget P, Martinovic J, Ménez F, Narcy F, Roux JJ, Rouleau-Dubois C, Sinico M, Tantau J, Wann AR (2010) Genotype–phenotype correlations in fetuses and neonates with autosomal recessive polycystic kidney disease. Kidney Int 77:350–358
Guay-Woodford LM, Desmond RA (2003) Autosomal recessive polycystic kidney disease: the clinical experience in North America. Pediatrics 111:1072–1080
Adeva M, El-Youssef M, Rossetti S, Kamath PS, Kubly V, Consugar MB, Milliner DM, King BF, Torres VE, Harris PC (2006) Clinical and molecular characterization defines a broadened spectrum of autosomal recessive polycystic kidney disease (ARPKD). Medicine (Baltimore) 85:1–21
Gunay-Aygun M, Tuchman M, Font-Montgomery E, Lukose L, Edwards H, Garcia A, Ausavarat S, Ziegler SG, Piwnica-Worms K, Bryant J, Bernardini I, Fischer R, Huizing M, Guay-Woodford L, Gahl WA (2010) PKHD1 sequence variations in 78 children and adults with autosomal recessive polycystic kidney disease and congenital hepatic fibrosis. Mol Genet Metab 99:160–173
Bergmann C, Senderek J, Sedlacek B, Pegiazoglou I, Puglia P, Eggermann T, Rudnik-Schöneborn S, Furu L, Onuchic LF, De Baca M, Germino GG, Guay-Woodford L, Somlo S, Moser M, Büttner R, Zerres K (2003) Spectrum of mutations in the gene for autosomal recessive polycystic kidney disease (ARPKD/PKHD1). J Am Soc Nephrol 14:76–89
Boddu R, Yang C, O’Connor AK, Hendrickson RC, Boone B, Cui X, Garcia-Gonzalez M, Igarashi P, Onuchic LF, Germino GG, Guay-Woodford LM (2014) Intragenic motifs regulate the transcriptional complexity of Pkhd1/PKHD1. J Mol Med 92:1045–1056
Ebner K, Feldkoetter M, Ariceta G, Bergmann C, Buettner R, Doyon A, Duzova A, Goebel H, Haffner D, Hero B, Hoppe B, Illig T, Jankauskiene A, Klopp N, König J, Litwin M, Mekahli D, Ranchin B, Sander A, Testa S, Weber LT, Wicher D, Yuzbasioglu A, Zerres K, Dötsch J, Schaefer F, Liebau MC, ESCAPE Study Group; GPN Study Group (2015) Rationale, design and objectives of ARegPKD, a European ARPKD registry study. BMC Nephrol 16:22
Acknowledgments
MCL was supported by grants of the German Society for Pediatric Nephrology, the European Society for Paediatric Nephrology, the German PKD foundation, the Koeln Fortune program, the GEROK program of the Medical Faculty of University of Cologne and the Marga and Walter Boll-Foundation. MCL and BS are supported by the German Federal Ministry of Research and Education (BMBF grant 01GM1515; NEOCYST consortium.). KE was supported by the Koeln Fortune program of the Medical Faculty of University of Cologne. BS was supported by the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG SCHE 1562/6).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosure
All authors report that they have no financial relationships relevant to this article to disclose.
Conflict of interest
All authors report that they have no potential conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Ebner, K., Dafinger, C., Ortiz-Bruechle, N. et al. Challenges in establishing genotype–phenotype correlations in ARPKD: case report on a toddler with two severe PKHD1 mutations. Pediatr Nephrol 32, 1269–1273 (2017). https://doi.org/10.1007/s00467-017-3648-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3648-x