Abstract
In this review we summarize the world-wide epidemiology of acute kidney injury (AKI) in children with special emphasis on low-income countries, notably those of the sub-Saharan continent. We discuss definitions and classification systems used in pediatric AKI literature. At present, despite some shortcomings, traditional Pediatric Risk Injury Failure Loss and End Stage Kidney Disease (pRIFLE) and Kidney Disease Improving Global Outcomes (KDIGO) systems are the most clinically useful. Alternative definitions, such as monitoring serum cystatin or novel urinary biomarkers, including cell cycle inhibitors, require more long-term studies in heterogenous pediatric AKI populations before they can be recommended in routine clinical practice. A potentially interesting future application of some novel biomarkers could be incorporation into the “renal angina index”, a concept recently introduced in pediatric nephrology. The most reliable epidemiological data on AKI in children come from high-outcome countries and are frequently focused on critically ill pediatric intensive care unit populations. In these patients AKI is often secondary to other systemic illnesses or their treatment. Based on a recent literature search performed within the framework of the “AKI 0by25” project of the International Society of Nephrology, we discuss the scarce and often inaccurate data on AKI epidemiology in low-income countries, notably those on the African continent. The last section reflects on some of the many barriers to improvement of overall health care in low-income populations. Although preventive strategies for AKI in low-income countries should essentially be the same as those in high-income countries, we believe any intervention for earlier detection and better treatment of AKI must address all health determinants, including educational, cultural, socio-economic and environmental factors, specific for these deprived areas.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Until recently, the absence of consensus about the definition of acute renal failure (ARF) resulted in a wide variation of estimates on the prevalence of the disease (1–25 %) and mortality attributable to it (15–60 %) [1, 2].
Several definitions and classification systems of ARF have been proposed to resolve this confusion [3]. All of these systems are based on reports that even small absolute increases in serum creatinine (SCr) are linked to worsening short-term and long-term prognosis [4, 5]. The first international interdisciplinary consensus criteria for a diagnosis of ARF were the Risk, Injury, Failure, Loss, and End-stage kidney disease (RIFLE) criteria [6] proposed by the Acute Dialysis Quality Insurance (ADQI) group. Modifications to these criteria have been proposed to better account for pediatric populations (pRIFLE) [7] and for small changes in SCr not captured by RIFLE by the Acute Kidney Injury Network (AKIN) criteria [8]. In parallel, the re-naming of ARF to acute kidney injury (AKI), which encompasses the entire spectrum of disease from small changes in function to the requirement for renal replacement therapy (RRT), has created a new descriptive system and extended the number of potentially affected patients.
Changes in the definitions of AKI in adults and children
Table 1 summarizes the definition and staging criteria of AKI as proposed by the Kidney Diseases: Improving Global Outcomes (KDIGO) clinical practice guidelines workgroup [9], and the adaptation of the RIFLE criteria [6] to pediatric populations, the pRIFLE classification [7].
Both SCr and urinary ouput criteria are important predictors of AKI, and the use of these definitions without any assessment of urinary output underestimates the incidence and grade of AKI, possibly delaying diagnosis [10–13]. Although it is recognized that AKI can be non-oliguric, SCr may not increase as rapidly as urine output falls; consequently, it is advisable to have data on both criteria [14]. However, it should be noted that numerous studies, both in adults and children, that have used large observational datasets from administrative or registry databases have omitted the urinary output contribution in the definition of AKI [15]. Measuring or monitoring daily urine output could, at least theoretically, be an easy and cheap method for early detection of AKI in countries with limited resources.
The KDIGO classification includes an acute decrease in estimated glomerular filtration rate (eGFR) to <35 mL/min per 1.73 m2 in the stage 3 criteria in individuals younger than 18 years [9]. The pRIFLE [7] uses the original Schwartz equation [16] to calculate estimated creatinine clearance. The Schwartz formula takes the expected normal changes in SCr into account that accompany somatic growth and is still the most popular formula for the estimation of GFR in children (for review [17]). The pRIFLE modification quantitates the change in estimated creatinine clearance rather than absolute changes in SCr as used in the adult version of RIFLE (Table 1).
The eGFR-based pRIFLE classification appears to be more sensitive in detecting mild functional impairment than the AKIN or KDIGO criteria [18–20]. In the study of Lex et al. [19], a significant number of patients were identified by pRIFLE criteria but missed by the AKIN criteria, while 5 % of children who were missed by the adult definitions of both the KDIGO and AKIN guidelines were identified using the pRIFLE classification. Several studies have assessed the prognostic value of these classification systems (in terms of length of hospital stay, costs, morbidity, and mortality) for pediatric patients [21]. Similarly, as in adult studies, higher pRIFLE stages are associated with unfavorable outcomes [22]. To the contrary, Sanchez-Pinto et al. [23] recently used the KDIGO AKI staging criteria in a heterogeneous pediatric intensive care unit (PICU) population to analyze the dynamic change in severity of AKI. An independent association between the development, progression, and improvement of AKI and mortality was found even after controlling for severity of illness and other organ dysfunctions.
Although both the pRIFLE and KDIGO definitions and staging criteria can be used in clinical practice, we believe that the KDIGO criteria should be preferred, if only because KDIGO is now increasingly used in the adult AKI literature, thereby facilitating long-term studies from AKI in childhood to the evolution of kidney function in adult life. It should be noted that the KDIGO guidelines refer only to children who are older than 1 month; they are not recommended for neonates. However, before the publication of the KDIGO guidelines for AKI, a number of neonatal studies were performed using the RIFLE and AKIN definitions of AKI [24, 25].
All current classification systems are based on consecutive assessments of SCr and, therefore, suffer from a number of general disadvantages in terms of AKI detection, particularly in children. Staging may be influenced by age and body composition, nutritional and fluid status, the integrity of muscle turnover, and the use of diuretics. For example, during the first days of life SCr values in the neonate represent the maternal values, with the levels depending on the degree of prematurity. There is a considerable delay between the initial renal tissue damage and subsequent functional impairment, and calculation of the eGFR formally requires steady-state conditions which are often not present in patients with AKI. Also, absolute changes in SCr may be of limited use in the pediatric population where the SCr concentration is strongly age dependent. Also, oligo-anuria, the other constituent of the KDIGO, AKIN, and pRIFLE classifications, is of limited sensitivity, particularly in neonates, since up to 60 % of neonatal AKI is non-oliguric [26].
Prior to the establishment of the RIFLE definition and classification, an assortment of more than 35 definitions for AKI was used [27], including those based on changes in SCr, absolute levels of SCr, changes in urine output or blood urea or blood urea nitrogen concentrations, or the need for dialysis. The wide variation in definitions made it difficult to compare information across studies and populations. The newer definitions bring uniformity to the diagnostic criteria of AKI that allows comparison between studies and populations. They facilitate healthcare providers in realizing that AKI has to be considered a spectrum of injury which extends from less severe forms of injury characterized by a minimal rise in SCr to more advanced injury when the patient with AKI may require RRT. In general, these criteria have been found to be clinically relevant, not only for diagnosing and classifing the severity of AKI but also for monitoring its progression, as well as to have a predictive capacity for short- and long-term prognosis. However, certain limitations, as summarized above, still remain to be resolved.
Despite the limitations and reservations about the KDIGO and pRIFLE definitions and classifications, we believe that their introduction in clinical practice has been and will continue to be useful.
Cystatin C
In view of the limitations associated with SCr as a marker of GFR, particularly in AKI, other markers, such as cystatin C (CysC) are increasingly being used. CysC is synthesized and released into plasma by all nucleated cells at a constant rate, and its small size (13 kDa) and positive charge at physiologic pH enables it to be freely filtered by the glomerulus. It is neither secreted nor reabsorbed but undergoes almost complete catabolism by proximal tubular cells, and thus little appears in the urine. With a half-life of about 2 h, serum CysC reflects the GFR better than creatinine. Unlike SCr, CysC concentrations are unaffected by muscle mass or sex, and they are much less age-dependent than those of SCr. CysC concentrations are higher in preterm than in at-term infants and decline during the first month of life, with the normal range of adults attained soon after the first year of life. In neonates, CysC, unlike SCr, has the particular advantage of being independent of maternal values [28, 29]. Although the CysC level is generally considered less subject to the non-renal variables that impact creatinine, recent studies suggest that its levels may be affected by various anthropometric measures as well as by inflammatory processes, use of corticosteroids, and changes in thyroid function, thereby potentially confounding interpretation [30, 31].
Several studies conducted both in adults and children [32–37] have used acute change in the CysC level to define AKI applying the same approach of calculating percentage changes as in methods based on SCr, but excluding the equivalent of “0.3 mg/dL rise from baseline” of the AKI stage 1 SCr criterion. A recent analysis [38] found that SCr-defined versus CysC-defined pediatric postcardiac surgery AKI incidence differed substantially (43.6 vs. 20.6 %). The CysC-based definition was more strongly associated with the concentrations of a number of novel tubular injury biomarkers in the urine, such as urine interleukin 18 (IL18) and kidney injury molecule 1 (KIM-1). To the contrary, in studies involving children admitted to a PICU, a baseline (pre-PICU) CysC value was estimated by using the Schwartz formula-estimated baseline eGFR using a validated CysC GFR formula [39, 40]. Lagos-Arevalo et al. reported that CysC-AKI was not more strongly associated with clinical outcomes, and these authors did not support replacing SCr by CysC to define AKI [41]. We suggest that in the context of defining AKI in children, CysC should be further evaluated and that information on changes in both SCr and CysC may be useful in future studies or in clinical care in which it is most desirable to specify AKI diagnosis (e.g. new drug trials, determination of preoperative risk, or decision to stop treatment with a nephrotoxic agent).
Novel biomarkers
Essentially three types of novel biomarkers have been identified in the field of AKI. The first group are inflammatory biomarkers, including neutrophil gelatinase-associated lipocalin (NGAL) and proinflammatory cytokines, such as IL6 and IL18. The second group includes cell injury biomarkers, such as KIM-1, liver fatty acid binding protein, sodium/hydrogen exchanger 3, and netrin 1. The third, more recently identified group consists of cell cycle markers, such as urinary tissue inhibitor of metalloproteinases-2 (TIMP-2), and insulin-like growth factor-binding protein 7 (IGFBP-7). Many recent in-depth reviews have summarized the characteristics, the advantages, and the limitations of these biomarkers [42–47]. It is sufficient to say that many biomarkers reflect a general degree of severity of disease, rather than being specific for kidney injury, or suffer from difficulties in the analytic methodology [48]. Furthermore, biomarker studies vary in their cut-offs between positive and negative results [49]. As a result, potential harm may occur if important interventions (i.e., computed tomography with contrast or necessary administration of aminoglycosides) are delayed or withheld based on false positive biomarker results.
The most recently developed G1 cell cycle inhibitors, [TIMP-2]•[IGFBP7], have been identified as promising biomarkers for the prediction of adverse outcomes, including RRT and mortality in critically ill patients. Meersch et al. [50] prospectively studied 51 children undergoing cardiac surgery with cardio-pulmonary bypass. Twelve children (24 %) developed AKI, and these children had a significant higher urinary [TIMP-2]•[IGFBP7] concentration as early as 4 h after the procedure, compared to children who did not develop AKI, with an area under the receiver-operating characteristic curve (ROC) of 0.85. Similar to other previously developed biomarkers, such as NGAL [51], the cell cycle inhibitors are good predictors of AKI in a homogenous patient population with few or no comorbidities. Using a commercially available immunoassay, (NephroCheck™; Astute Medical, San Diego, CA), Westhoff et al. [52] assessed a prospective cohort of 133 subjects aged 0–18 years, including 46 patients with established AKI according to pRIFLE, 27 patients without AKI (non-AKI group I), and 60 apparently healthy neonates and children (non-AKI group II). Patients in the “Failure” stage had a median 3.7-fold higher urinary [TIMP-2]• [IGFBP7] concentration than non-AKI subjects (P <0.001). When analyzed for AKI etiology, the highest [TIMP-2]•[IGFBP7] values were found in patients with septic shock (P <0.001 vs. non-AKI I + II). ROC analyses in the AKI group revealed that [TIMP-2]•[IGFBP7] performed well in terms of predicting 30-day and 3-month mortality, but only modestly for predicting RRT (area under the time-concentration curve (AUC) 0.67; 95 % confidence interval (CI) 0.50–0.84].
However, Bell et al. [53] recently found that in adult patients admitted to the ICU, biomarker values, including the cell cycle markers, did not predict AKI within 12–48 h and were significantly affected by comorbidities, even in the absence of AKI. Thus, these findings challenge the robustness and utility of cell cycle arrest biomarkers for the prediction of AKI in general ICU patients with heterogeneous diagnoses, differing comorbidities, and multiple sources of inflammation [53].
As concluded in a recent excellent review [47], the use of individual biomarkers for decision-making is currently not defined and still measured “bench-work” and not “bed-side.” Although some of the biomarkers are highly sensitive and specific, larger, multicenter, and long-term trials are still necessary to make the transition from the analytical laboratory to the clinic possible and eventually allow reliable decisions upon their positivity.
The concept of renal angina in pediatric AKI
The concept of “renal angina” (RA) has been developed in analogy with the diagnostic performance of troponin as an early, correct diagnosis of cardiac ischemia. This concept is based on the combination of AKI risk factors and early signs of kidney injury, both in children and adults [54]. The initial RA proposal has a pediatric and adult definition (pRA and aRA, respectively), with the pRA using criteria congruent with pRIFLE and the aRA using RIFLE.
In the pediatric construct, besides clinical risk factors, the measures of injury are based on small increases in SCr and percentage fluid overload. The renal angina index (RAI) is then a multiplicative result of escalating “risk” (sepsis, history of transplant, use of vasoactives, and/or invasive mechanical ventilation) and early signs of kidney dysfunction (small changes from baseline SCr, relatively short periods of oliguria, and/or accumulated fluid overload) (for detailed description of the concept, see [54, 55]).
Basu and colleagues recently evaluated this concept in four cohorts of critically ill pediatric patients and assessed the performance of RA using the RAI [56] for predicting severe AKI 3 days after ICU admission. The performance of the RAI in each of these pediatric cohorts was remarkably consistent, with a risk prediction performance of the AUC of 0.74–0.81 and a negative predictive value of 92–99 %. Despite AUCs comparable to those seen with many of the biomarkers which have been examined, the positive predictive value of the RAI was only modest during validation, partially reflecting the lower prevalence between 10 and 19 % of severe AKI (stage 2 or 3 KDIGO on day 3 after ICU admission) in these critically ill children. Even among patients with the highest RAI scores, only 41–67 % developed severe AKI, suggesting that caution is still warranted before treatment decisions should be based on the presence of RA alone [57]. It has been suggested that the addition of novel biomarkers into the RAI may complement and improve the performance of the RAI [57]. Basu et al. [58] tested this hypothesis in a series of 214 children with sepsis. The incorporation of biomarkers significantly added to the RA model and AKI prediction (AUC = 0.80, increased to 0.84–0.88; P < 0.05 for each). Based on these results, the authors of this study suggest thus that incorporation of AKI biomarkers into the RAI improves discrimination for severe AKI in a heterogeneous, critically ill pediatric patient population. However, the improved discrimination based on a statistically significant increase in AUC may be less impressive in real numbers in view of the rather low incidence of AKI in this study.
Epidemiology of AKI in the pediatric population
Dramatic rises in the incidence of AKI have been reported over the past two decades throughout the world. Such increases cannot only be explained by the introduction of more sensitive SCr values for the diagnosis AKI, changes in coding and reimbursement, or the increasingly availability and more liberal use of dialysis [59]. As in adults, before the consensus pRIFLE definition became regularly used, the description of pediatric AKI epidemiology lacked concordance [60].
In this section we first focus on the most recently published epidemiological studies on AKI in pediatric populations. Whenever possible, separate data on studies with mixed populations, hospitalized but not critically ill and ICU patients will be analyzed. For reasons of space the epidemiology of AKI in neonates will not be discussed. Excellent recent reviews on this topic are available in the literature [61–63]. Second, AKI as a global concern and the role of the International Society of Nephrology (ISN) in the prevention of this dramatic disease will be described. Finally, difficulties encountered in the analysis of epidemiological data on AKI in low-income countries will be illustrated by means of a discussion of recent studies originating from a number of sub-Saharan countries.
AKI in mixed populations (critically ill and non-critically ill patients)
Hsu and Symons [64] summarized six epidemiological studies on pediatric, mostly critically ill patients with AKI published between 2007 and 2009. Apart from a single study by Bailey et al. [65] in which AKI was defined as a doubling of SCr, resulting in a low incidence of AKI of 4.5 %, pRIFLE criteria were applied, resulting in an incidence between 35.9 and 82 %.
Based on an observational, electronic medical record-enabled study of 14,795 hospitalizations between 2006 and 2010, Sutherland et al. [66] applied the pRIFLE, AKIN, and KDIGO criteria—but no urine output criteria—to compare AKI incidence and outcomes in ICU and non-ICU pediatric populations. The reported incidences of AKI accross the cohort according to pRIFLE, AKIN, and KDIGO were 51.1, 37.3, and 40.3 %, respectively. Mortality was higher among patients with AKI according to all definitions [pRIFLE 2.3 %; AKIN 2.7 %; KDIGO 2.5 %; P <0.001 vs. no AKI (0.8–1.0 %)]. The largest disparities between the different classification systems were found in AKI stages 1 and 3. Incidences of stage 3 AKI were 10.8, 6.7, and 11.7 %, respectively. The incidences of AKI in the ICU and non-ICU populations were similar across all three definitions. Within the ICU, pRIFLE, AKIN, and KDIGO demonstrated progressively higher mortality at each higher AKI severity stage. However, AKI stage by any definition was not associated with differences in mortality outside the ICU. Different definitions thus resulted in differences in diagnosis and staging of AKI, with the staging disagreement ranging from 7.5 to 23.3 %.
AKI in hospitalized but non-critically ill children
Studies on community-acquired AKI in children remain scarce; for example, few national reports or nationwide studies are available on the incidence of AKI in children, as studies on this patient population are usually performed at specific centers or regions. These studies are based on limited surveillance networks and registries and focus on the incidence in hospital populations [67, 68].
Zappitelli et al. [69] studied the incidence, severity, and risk factors for AKI and the factors associated with longer hospitalization and higher costs in 489 hospitalized but non-critically ill children receiving aminoglycosides. AKI was defined by the pRIFLE and AKIN definitions. The AKI rate was 33 and 20 % by the pRIFLE and AKIN definitions, respectively. Longer treatment, higher baseline eGFR, being on a medical (vs. surgical) treatment, and prior aminoglycoside treatment were independent risk factors for AKI development. The results of this study suggest that nephrotoxin-AKI represents a significant healthcare burden for hospitalized children. As a follow-up of this study a systematic electronic health record (EHR) screening and decision support process was implemented; this nephrotoxin-AKI surveillance process was associated with a 42 % reduction in AKI intensity from 33.6 to 19.5 days in AKI per 100 exposure days, suggesting the earlier withdrawal of nephrotoxins in AKI patients led to the decrease in AKI intensity [70]. Rheault et al. [71] applied the pRIFLE definition in their review of medical records in 17 pediatric nephrology centers across North America, reporting an incidence of AKI of 58.6 % in 336 children with nephrotic syndrome. After multivariant adjustment, nephrotoxic medication exposure days and intensity of medication exposure remained significantly associated with AKI in these children. AKI was associated with longer hospital stay and increased need for ICU admission. Misurac et al. [72] screened a hospitalized population aged ≤18 years and found that in 2.7 % of AKI cases, the patients suffered from non-steroidal anti-inflammatory drug (NSAID)-associated AKI. Of the 20 children for whom dosing data were available, 15 (75 %) received NSAIDs within the recommended dosing limits. These authors found that patients aged <5 years were more likely to require dialysis, to be admitted to the ICU, and to have a longer length of stay [72].
Based on a cross-sectional analysis of the 2009 Kids Inpatient Database in the USA, Sutherland et al. [73] found an AKI incidence of 3.9/1000 pediatric admissions. Although 19 % of the AKI cohort was ≤1 month old, the highest incidence was seen in children aged 15–18 years (6.6/1000 admissions); 49 % of the AKI cohort was white, but AKI incidence was higher among African Americans (4.5 vs. 3.8/1000 admissions). In-hospital mortality of AKI patients was 15.3 %, but higher among children aged ≤1 month. Several associations with AKI were found, including children requiring critical care or dialysis, shock, septicemia, intubation/mechanical ventilation, circulatory disease, cardiac congenital anomalies, and extracorporeal support. Those risk factors suggest that, at least in the USA, it is more common for pediatric AKI to occur in association with systemic/multiorgan disease than to be due to primary renal disease [73].
A more recent U.S. study [74] calculated the AKI frequency over a 2-year period in a tertiary care children’s hospital using KDIGO SCr criteria. The results show that a minimum of 5 % of all non-critical inpatients without chronic kidney disease (CKD) in pediatric wards have an episode of AKI during routine hospital admission.
A Norwegian national survey in hospitals providing specialized care in pediatric AKI estimated an average annual incidence rate of 3.3 cases per 100,000 children (population numbers) and a median annual occurrence of 33 cases [75]. In contrast with the U.S. data just described [74], nephritic syndromes were the major specific cause (44 %) of AKI, followed by hemolytic-uremic syndrome (15 %).
AKI in critically ill children
Hospital- and PICU-acquired AKI rates appear to have increased by over ninefold from the 1980s through 2004 due to increasing use of more invasive management and higher illness severity [76]. In contrast with the literature on adult critically ill patients, current information on pediatric patients with AKI lacks prospective extensive multicenter and international studies on AKI. The study of Schneider et al. [77] did not use the pRIFLE criteria to define AKI, and the results from that study are therefore difficult to compare with those of other studies.
In a single-center study of 8260 ICU patients, 529 (6.4 %) had AKI on ICU admission while 974 (11.8 %) developed AKI during their ICU course. The 28-day ICU mortality was 2.7 % for patients with no AKI and 25.3 % for patients with AKI. Progression of AKI was independently associated with increased mortality in the PICU, while its improvement was associated with a stepwise decrease in mortality [23].
In a study of 60,338 critically ill children whose clinical data were compiled in the Taiwanese National Health Insurance program [78], AKI was identified in 850, yielding an average incidence rate of 1.4 %. Overall, 46.5 % of the AKI cases were due to sepsis, 36.1 % of the patients underwent RRT, and the mortality rate was 44.2 %. Multivariate analysis showed that the use of vasopressors, mechanical ventilation, and hemato-oncological disorders were independent predictors of mortality in AKI patients. Of the 474 patients who survived, 32 (7 %) progressed to CKD or end-stage renal disease (ESRD).
Based on data compiled in the University of Michigan Pediatric Critical Care Database, which registers all discharges from the PICU and cardiac ICUs (CIKU), and using the KDIGO SCr-based criteria, Selewski et al. identified AKI in 737 (24.5 %) of 3009 discharges [79]. In the multivariate analysis AKI was associated with increased ICU length of stay, increased odds of ICU mortality, and increased length of mechanical ventilation when needed. Worsening stages of AKI were associated with increased ICU length of stay [79].
The on-going Assessment of Worldwide Acute Kidney Injury, Renal Angina and Epidemiology (AWARE) study is an attempt to fill the gap in global pediatric studies. The hypotheses of this study are that: (1) “renal angina”, a composite of early injury signs and risk of disease, will predict subsequent severe AKI in critically ill children and (2) the incorporation of urinary biomarkers into the renal angina scoring system will improve the prediction of severe injury. The AWARE study will provide the first prospective international pediatric all-cause AKI data warehouse and biological sample repository [80] (ClinicalTrials.gov: NCT01987921). The data collection was completed in February 2015, but no results are as yet available.
Many recent but small-sized studies have described the incidence and sequelae of AKI in young patient populations in specific high-risk settings. Cohort studies have reported AKI due to nephrotoxic medications [20, 69, 81–84], cardiac surgery/bypass [19, 85], and sepsis [56, 86], or AKI after admission to an ICU [7, 20, 87–89].
Although prospective international studies on pediatric AKI are scarce, this short overview of studies focusing mainly on high-income countries (HICs) confirms that pediatric AKI has evolved from a primary single renal disease to a syndrome secondary to other systemic illnesses or its treatment. Advances in medical management, including solid organ and stem cell transplantation, corrective congenital heart surgery, sepsis, and septic shock, have depended on medicinal and mechanical therapeutic interventions that sometimes have nephrotoxic side effects. Postcardiac surgery, sepsis, multiorgan failure, hemato-oncological diseases, trauma, and exposure to nephrotoxic agents (drugs, contrast media) are the main causes of AKI in the critically ill child, while in the hospitalized, non-critically ill child, exposure to nephrotoxins (aminoglycosides, NSAIDs) is a major cause of AKI [90]. The prognosis of AKI in the economically developed part of the world is most often dependent on the associated underlying non-renal illness. Finally, the effects of AKI are also long lasting in survivors, with almost one-half of patients at the 3- to 5-year follow-up having developed CKD, suggesting permanent alteration of the renal parenchyma [90, 91].
Overall, the variation in AKI incidence is determined by differences in clinical settings (e.g., community, hospital, or ICU), but even in HICs the true incidence of AKI on a broad international scale is not well known. Community-acquired AKI might have only one cause, whereas the disease can result from several pathways in hospitalized patients, especially among those who are severely ill. The mortality risk increases in a stepwise fashion in accordance with the stage of disease. Many patients die from underlying comorbidities, and the previously accepted pattern of almost complete recovery of kidney function in survivors of AKI has been replaced by the notion that partial recovery or non-recovery can occur, potentially leading to CKD and even ESRD.
Global study on AKI—role of international organizations
As described in the preceding sections of this review, a number of international studies on the epidemiology and impact of AKI have been published, but global data are not available. In particular, reliable epidemiological data on AKI in both adults and children in middle- and low-income countries are scarce [92–95]. The burden of AKI may be most significant in developing countries [96, 97] with limited resources for the care of these patients once the disease progresses to kidney failure necessitating RRT. Addressing the unique circumstances and needs of developing countries, especially in the detection of AKI in its early and potentially reversible stages to prevent its progression to kidney failure requiring dialysis, is of paramount importance.
The lack of worldwide data has inspired the International Society of Nephrology to establish the “0 by 25” AKI initiative, with the aim to prevent all avoidable deaths from AKI worldwide by 2025 [98]. During the preparation and organization of this initiative, the Saving Young Lives (SYL) project was started in September 2012 with a generous grant from the Recanati-Kaplan Foundation [99] and is managed cooperatively by the International Society of Nephrology (ISN), the International Society of Peritoneal Dialysis (ISPD), the International Pediatric Nephrology Association (IPNA), and the Sustainable Kidney Care Foundation (SKCF). This program is not intended to collect direct data on the epidemiology of AKI, but to provide the necessary training and educational support for physicians and nurses in low-resource settings to develop and establish sustainable programs to treat patients with AKI, with an emphasis on the use of peritoneal dialysis for those who need dialytic therapy.
The SYL consortium has, thus far, helped develop programs in Tanzania, Benin, Cameroon, and two sites in Ghana, and has signed memoranda of understanding to initiate programs in Cambodia, Ethiopia, Uganda, and Ivory Coast. It is very clear that these programs save lives and without the support from SYL at these centers, children with AKI who need dialytic support would die.
To explore the burden of AKI around the globe, a group of investigators belonging to the Acute Kidney Injury Advisory Group of the American Society of Nephrology, performed a systematic review (2004–2012) of large cohort studies to estimate the world incidence of adult and pediatric AKI and its stages of severity and associated mortality and to describe geographic variations according to countries, regions, and their economies [100]. A total of 312 studies were identified (n = 49,147,878 patients), primarily in hospital settings. Of the total of 154 studies (n = 3,585,911 patients) in the meta-analysis that adopted a KDIGO-equivalent AKI definition, only 24 studies in children were included. The pooled incidence of AKI and pooled AKI-associated mortality rates in children were 33.7 % (95 % CI 26.9–41.3 %) and 13.8 % (95 % CI 8.8–21.0 %), respectively. The overall AKI-associated mortality rate declined over time and was inversely related to income of countries and percentage of gross domestic product spent on total health expenditure. Although this systematic review was the first successful attempt to approach the global epidemiology of AKI, it had several limitations. The pooled AKI incidence and mortality rates were not standardized or normalized to at-risk periods. Most studies originated from HICs situated in North America, Northern Europe, and Eastern Asia that spent at least 5 % of the gross domestic product on total health expenditure, and they involved hospitalized and often critically ill patients. Assumptions were required to harmonize definitions of AKI according to one classification and staging system and to generate pooled estimates, possibly introducing biases. A large sample size was a criterion for study inclusion, which likely excluded reports of community-acquired AKI originating from developing countries, especially in children, that involved small numbers of patients. Although 85 % of the world’s younger population lives in low- and middle-income countries (LMICs), systematic prospective studies from those regions are limited by problems with communication between centers and absence of mechanisms to collect accurate data [96, 97, 101–104].
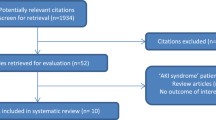
To further refine the estimation of the worldwide epidemiology of AKI, the meta-analysis by Susantitaphong and colleagues [100], was updated by Mehta et al. by searching for papers using the same definitions and inclusion and exclusion criteria [95]. The data in these latter publications were added to the reports identified by Susantitaphong et al. [100], resulting in a new total of 499 published studies which used all definitions of AKI and 266 studies which used KDIGO or KDIGO-equivalent definitions of AKI. As a result, the sample size increased from 49 million to more than 77 million individuals.
Preliminary analysis of the pooled incidence by KDIGO stage in the 266 studies that used this definition (4,502,158 patients) revealed that 21 % of hospital admissions were affected and that the overall proportion of patients with AKI who needed dialysis in KDIGO-defined studies was small (2 % of hospital admissions; 11 % of all AKI), whereas 12 % of hospital admissions (80 % of all AKI cases) had KDIGO stage 1. The overall pooled mortality of these 21 % of patients is probably due to the predominance of mild stages of AKI. However, patients with the more severe KDIGO stage 3 or those who required dialysis had a high mortality (42 vs. 46 %, with unadjusted odds ratio of 12.5 and 19.7, respectively), which is in agreement with other studies.
Many reports from LMICs were not included in the meta-analysis because they did not satisfy the inclusion or exclusion criteria (187 papers, 89,325 patients). These reports were aggregated into three LMIC regions, namely, Africa (61 studies and 55,309 patients), Asia (92 studies and 6,993 patients), and Latin America (33 studies and 7,023 patients). Reports on pediatric AKI were included in the more recent meta-analysis of Mehta et al. [95] but unfortunately not separately analyzed so that the global epidemiology of AKI in children could not be estimated.
Since one of the authors (NL) was responsible for the literature search on AKI in Africa, more detailed data on AKI on this continent are provided in the following sections of this review.
The number and age range of patients with AKI in the African studies published between 2000 and June 2014 that were included in the meta-analysis of Mehta et al. [95] are shown in Table 2. The mean age of AKI patients in the adult studies (36.7 years; range 14–96 years) is dramatically lower than that of adult AKI patients reported in HICs (63.7 years; range 44.9–82.5 years) [95]. Despite a lower number of African studies on pediatric AKI patients, the sample size (number of AKI patients per report) was higher than that in the adult AKI studies. The mean age of children in the pediatric AKI studies was 4.1 (range 0–18) years.
To illustrate the difficulties in extracting useful overall data from these studies, Table 3 summarizes the distribution of causes of AKI in the 21 African studies on pediatric AKI published between 2000 and 31 July 2014. Africa is the continent with the highest number of LICs.
Table 3 illustrates that nine papers out of 21 (43 %) describe AKI as a complication of one single disease. Half of the papers describing AKI due to a specific disease have malaria as the major cause, followed by intoxications due to paraphenyldiamine and diethylglycerol.
Pediatric AKI in sub-Saharan countries
Olowu et al. very recently analyzed the outcomes of AKI in children and adults in sub-Saharan Africa [105]. The majority of the studies included in their analysis were also included in the section of the ISN meta-analysis on Africa [95] so that the interpretation and conclusions of Olowu et al. [105] overlap to some extent those of Mehta et al. [95]. It should be noted, however, that the number of countries and the study periods analyzed by Olowu et al. [105] differ from those reported in this review.
It is notable from Fig. 1, which is based on data from Olowu et al. [105], that the spectrum of diseases associated with AKI in countries of sub-Saharan Africa differs from that in Western countries. While in countries of sub-Saharan Africa, as in Western countries, sepsis is a major cause of AKI (90 % of the infection causes), in the former malaria, severe dehydration due to infectious gastroenteritis, and glomerular diseases, probably also infection-induced, are the more prominent causes. Despite intense global and African efforts to combat malaria, in particular the more severe forms of this disease, such as black water fever, it still remains an important and lethal cause of AKI in young children. A number of publications from the Democratic Republic of Congo, Togo, and Ghana illustrate the dramatic impact of this major problem [106–110].
Summary of the most important etiologies of pediatric acute kidney injury in sub-Saharan countries (South Africa included) based on data from Olowu et al. [105]. Numbers in bars are percentages
Only two publications from Nigeria report the proportions of community-acquired and hospital-acquired AKI—72.8 and 82.9 %, respectively [110, 111]. However, it may be assumed that community-acquired AKI in children [i.e., patients are admitted to the hospitals with (sometimes) severe AKI] accounts by far for the majority of AKI cases. Furthermore, practically all publications originate from large university hospitals with a nephrology service, and there are almost no data on the incidence of AKI in vast rural areas, making the magnitude and outcome of community-acquired AKI in Africa virtually unknown. Most studies report a single-center experience, with a large minority describing AKI due to a single disease, such as specific infections [malaria, tuberculosis, and human immunodeficiency virus (HIV)], or exposure to toxins or traditional remedies, without reference to the underlying population [95].
The difficulty in estimating the incidence of AKI in African populations is further illustrated in the recent paper by Abdelraheem et al. [112] on AKI in Sudanese children. Over a 7-year period 363 children living in Khartoum state and ranging from neonates to adolescents were admitted for AKI to the pediatric nephrology unit of Soba University Hospital, Khartoum. The population of cosmopolitan Khartoum is about 5.3 million, giving an estimated incidence of AKI in the Khartoum area of 9.8 patients/million population/year, while the estimated incidence of AKI for the whole country of Sudan was estimated to be 2.6 patients/million population per year. The much lower reported incidence of AKI for the whole country is due to the very small number of children with AKI from the provinces outside the capital and living in rural areas who have no access to advanced medical services. The majority of the patients were neonates (27.1 %).
Many epidemiological results are skewed because of late presentation of patients to mostly tertiary centers, underreporting, and a reduced capacity to provide intensive care, including RRT, to severely ill and/or late stage AKI patients. An important weakness of all epidemiological reports in Africa is the high selection bias in the described populations; the studies are almost always retrospective and mostly based on data from university hospitals where a pediatric nephrology service is present. Virtually no data on the incidence of pediatric AKI in the vast rural areas of Africa are available. There is also a large variability in the distribution of risk factors between the different countries on a given continent, as well as large differences in healthcare facilities in terms of diagnostic capacities and accessibility to services.
Finally, most reports are difficult to find in mainstream journals and are therefore not readily accessible using the usual search strategies. The recently published report of Olowu et al. [105] is a laudable effort to highlight these shortcomings and difficulties and may hopefully result in better and more accurate data in the future.
Table 4 summarizes data on access to RRT for pediatric AKI patients in sub-Saharan countries between 2010 and 2014, compiled from 11 studies and adapted from Olowu et al. [105].
As summarized in the study of Oluwu et al. [105], the overall mortality in pediatric AKI in sub-Saharan countries (studies between 2010 and 2014) was 34 % but rose to 79 % when dialysis was needed but not received. The mortality among children with AKI on dialysis was 31 %. Many dialysis-requiring patients are managed conservatively either because of the lack of dialysis equipment or because of financial constraints. Of all sub-Saharan countries, only in Sudan and South Africa is dialysis as RRT funded by the government and thus offered to all AKI patients when it is indicated. In Rwanda, dialysis is covered by social security for a duration of 6 weeks after the initiation of RRT. When the patient does not recover within that period RRT is stopped (N. Lameire, personal experience).
Discussion and conclusions
Data derived from HICs, using standardized definitions for diagnosis and staging of AKI, have facilitated comparisons of AKI incidence and outcomes in different clinical settings. In developed countries, AKI is usually a very severe complication of critical disease, and the majority of children dying with AKI occur among very sick patients in the ICU. Abundant information is available on this topic.
As we have tried to demonstrate in our review, there is a paucity of information on the prevalence, course, and outcomes of pediatric AKI in African—mainly sub-Saharan—countries, and we have no reason to believe that many of the described results are different in LICs in other developing regions of Asia and Latin America. AKI occurring in the community (e.g., due to diarrheal states, malaria) remains under-recognized. We have a very imperfect knowledge of how common or how costly AKI is in LMICs. Two recent global meta-analyses [95, 100] and a very recent survey covering sub-Saharan countries [105] have clearly demonstrated that AKI registries are imperfect or even non-existent in these countries. In large areas of Africa under-reporting is pervasive, but also quite common. Moreover, most of the available studies on AKI burden in LMICs are limited because they seldom provide population-based data; rather, they focus on high-level medical centers, often the only ones offering dialysis and other advanced care, and thus do not reflect the reality of the country as a whole. While scientifically valuable, ICU-based studies from LMICs are not helpful in providing data which allows a reliable estimation of the population burden of AKI in these settings. Although it may be assumed that the majority of cases of AKI in these countries are community-acquired, the use of registries which only compile data on hospital-acquired cases in high-level medical centers leads to under-reporting and skewed views on prevalence and incidence. This limitation has important consequences because these community-acquired forms of AKI are the most amenable to early, inexpensive yet very effective interventions, which are the focus of the ISN “0 by 25” initiative.
In spite of this likelihood of frequent community-acquired AKI, there is no reason to believe that the incidence of AKI in LMICs is lower than that in the developed world and that the mortality is dramatically lower [95]. In comparison to AKI patients in HICs, the majority of individuals affected by AKI in LMICs are younger, and many more are children. Although the mortality among these latter patients may be lower than that of the older, critically ill patients in HICs, AKI still creates a huge burden of disease, not only in terms of number of deaths, but also in terms of the development of severe, often progressive CKD and ESRD and decreased quality of life. In the majority of cases, families in LMICs cannot afford dialysis, and many patients die untreated, while also the loss of family members due to death or invalidity may be accompanied by a huge socio-economic burden in those countries where social security systems are often less efficient, if not largely lacking.
Although dialysis must become more available to patients with AKI, it is unlikely that the limited resources of such countries will be able to afford dialysis on a large scale in the short term. Therefore, effective, conservative and inexpensive management of AKI should be the primary goal of intervention. While efforts at decreasing morbidity and mortality of AKI in rich countries has been very difficult, the incidence and severity of AKI in poor countries may be significantly decreased or altogether avoided by simple, inexpensive measures that can be implemented by unsophisticated caregivers.
Preventive strategies for AKI in LICs are essentially the same as those in HICs, but their implementation in the former pose additional and unique ethical problems. Because health care is affected by social and economic factors, any intervention needs to address all health determinants, including educational, economic, and environmental factors [93]. Expensive interventions to prevent or treat AKI could affect the ability of a healthcare system to meet other and more frequent needs. Conversely, the high mortality associated with primary diseases, such as malaria, HIV/acquired immune deficiency syndrome (AIDS), infectious gastro-enteritis, and toxic self-medication, is frequently caused by serious AKI that cannot be treated due to the lack of dialysis facilities. Because of the scarcity of resources and the presence of overwhelming health-related and other problems in these countries, prevention of AKI injury ought to target eradication of the most common causes (i.e., tropical and non-tropical infections), improve education and socio-economic conditions, and support healthcare infrastructure and the access to healthcare facilities. In rural centers, primary-care physicians need to be able to treat common causes of AKI and to organize the transfer of individuals requiring critical care at the right time to hospitals with the secondary and tertiary capacity to deal with AKI, including RRT [93, 95]. AKI is often, at least in the beginning, clinically associated with aspecific symptoms, and diagnosis is largely based on laboratory measurements which are rarely available in remote areas. Consequently, AKI often goes unrecognized during a first examination by non-specialist healthcare providers. Caregivers in the community might not have the knowledge needed for early recognition, timely intervention, and effective follow-up [113]. Innovative strategies, such as outreach programs, improved transportation, involvement of community healthcare workers, and strengthening of first-level health units, are needed to decrease the physical barriers encountered by marginalized populations when attempting to access healthcare services. Many of the initiatives that could lead to a decreased incidence and better outcomes of AKI can be integrated into larger interventions to manage pervasive regional problems. Such is the case with campaigns to decrease the incidence of severe malaria or campaigns to manage diarrheal disease with oral rehydration. Special attention needs to be given to the promotion of planned pregnancies with appropriate antenatal care by skilled midwives. Overall, most preventive efforts should focus at the primary healthcare level. In this regard, two infrequently discussed issues related to the generous foreign aid donated to LICs should be mentioned here. First, most aid is allocated to disease-specific projects (termed “vertical programming”) rather than to broad based investments in healthcare infrastructure, human resources, and community-oriented primary healthcare services (“horizontal programming”). This unbalanced distribution of healthcare funding (e.g., HIV, malaria) occurs across sub-Saharan Africa. Thus, although HIV-positive patients receive free care, others with more routine diseases receive poor care and still have to pay out of pocket. Second, the salaries of healthcare providers working for donor-funded vertical programs are often much higher than those of equally trained government workers in the fragile public healthcare sector in these countries. This attracts government workers to the higher paying vertical programs and creates an internal “brain drain”. But it is the underfunded primary healthcare clinics and healthcare centers that treat all diseases, including common illnesses such as diarrhoea, malnutrition, prenatal care, and respiratory tract infections, and these diseases cost more individuals their lives than do HIV, tuberculosis, and malaria.
The designers of external interventions must take into consideration the local and regional customs and traditions; otherwise, the interventions are bound to failure. Such is the case, for example, of interventions to decrease the use of often nephrotoxic traditional medications. Such interventions must often deal not only with the toxic effects of those products, but also with the distrust of local populations towards “Western medicine”. Not uncommonly, public health interventions are hampered by local and cultural distrust of public health initiatives, or by the impediments generated by discrimination.
Until appropriate studies accurately measure the incidence and consequences of AKI in LMICs, resulting in sufficient awareness among local populations, AKI will remain largely unrecognized in these countries. Such under-recognition results in very low attention being paid to the problem by public healthcare workers, as well as impaired implementation of region-wide initiatives destined to avoid the development of AKI. Pulled in different directions by many requests and dealing with limited economies, politicians and administrators do not give the problem adequate attention and resources, and the condition remains poorly managed. Poor recognition also extends to primary caregivers, who have insufficient awareness of the diagnosis and the management of AKI and thus fail to rapidly implement the simple, inexpensive measures that would have the highest beneficial impact.
References
Liano F, Pascual J (1996) Epidemiology of acute renal failure: a prospective, multicenter, community-based study. Madrid Acute Renal Failure Study Group. Kidney Int 50:811–818
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294:813–818
Bellomo R, Kellum JA, Ronco C (2012) Acute kidney injury. Lancet 380:756–766
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW (2005) Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16:3365–3370
Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M (2004) Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 15:1597–1605
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8:R204–R212
Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL (2007) Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int 71:1028–1035
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A (2007) Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:R31
Kidney Diseases Improving Global Outcomes (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int 2[Suppl 1]:1–138
Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD, Clermont G (2015) Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol 26:2231–2238
Macedo E, Malhotra R, Bouchard J, Wynn SK, Mehta RL (2011) Oliguria is an early predictor of higher mortality in critically ill patients. Kidney Int 80:760–767
Vanmassenhove J, Glorieux G, Hoste E, Dhondt A, Vanholder R, Van Biesen W (2013) Urinary output and fractional excretion of sodium and urea as indicators of transient versus intrinsic acute kidney injury during early sepsis. Crit Care 17:R234
Wlodzimirow KA, Bu-Hanna A, Slabbekoorn M, Chamuleau RA, Schultz MJ, Bouman CS (2012) A comparison of RIFLE with and without urine output criteria for acute kidney injury in critically ill patients. Crit Care 16:R200
Kellum JA (2015) Diagnostic criteria for acute kidney injury: present and future. Crit Care Clin 31:621–632
Rewa O, Bagshaw SM (2014) Acute kidney injury—epidemiology, outcomes and economics. Nat Rev Nephrol 10:193–207
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Schwartz GJ, Work DF (2009) Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol 4:1832–1843
Kavaz A, Ozcakar ZB, Kendirli T, Ozturk BB, Ekim M, Yalcinkaya F (2012) Acute kidney injury in a paediatric intensive care unit: comparison of the pRIFLE and AKIN criteria. Acta Paediatr 101:e126–e129
Lex DJ, Toth R, Cserep Z, Alexander SI, Breuer T, Sapi E, Szatmari A, Szekely E, Gal J, Szekely A (2014) A comparison of the systems for the identification of postoperative acute kidney injury in pediatric cardiac patients. Ann Thorac Surg 97:202–210
Zappitelli M, Parikh CR, Kcan-Arikan A, Washburn KK, Moffett BS, Goldstein SL (2008) Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin J Am Soc Nephrol 3:948–954
Alkandari O, Eddington KA, Hyder A, Gauvin F, Ducruet T, Gottesman R, Phan V, Zappitelli M (2011) Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit Care 15:R146
Plotz FB, Bouma AB, van Wijk JA, Kneyber MC, Bokenkamp A (2008) Pediatric acute kidney injury in the ICU: an independent evaluation of pRIFLE criteria. Intensive Care Med 34:1713–1717
Sanchez-Pinto LN, Goldstein SL, Schneider JB, Khemani RG (2015) Association between progression and improvement of acute kidney injury and mortality in critically ill children. Pediatr Crit Care Med 16:703–710
Askenazi DJ, Griffin R, McGwin G, Carlo W, Ambalavanan N (2009) Acute kidney injury is independently associated with mortality in very low birthweight infants: a matched case–control analysis. Pediatr Nephrol 24:991–997
Gadepalli SK, Selewski DT, Drongowski RA, Mychaliska GB (2011) Acute kidney injury in congenital diaphragmatic hernia requiring extracorporeal life support: an insidious problem. J Pediatr Surg 46:630–635
Karlowicz MG, Adelman RD (1995) Nonoliguric and oliguric acute renal failure in asphyxiated term neonates. Pediatr Nephrol 9:718–722
Kellum JA, Levin N, Bouman C, Lameire N (2002) Developing a classification system for acute renal failure. Curr Opin Crit Care 8:509–514
Cataldi L, Mussap M, Bertelli L, Ruzzante N, Fanos V, Plebani M (1999) Cystatin C in healthy women at term pregnancy and in their infant newborns: relationship between maternal and neonatal serum levels and reference values. Am J Perinatol 16:287–295
Fanos V, Mussap M, Plebani M, Cataldi L (1999) Cystatin C in paediatric nephrology. Present situation and prospects. Minerva Pediatr 51:167–177
Grubb AO (2000) Cystatin C—properties and use as diagnostic marker. Adv Clin Chem 35:63–99
Laterza OF, Price CP, Scott MG (2002) Cystatin C: an improved estimator of glomerular filtration rate? Clin Chem 48:699–707
Briguori C, Visconti G, Rivera NV, Focaccio A, Golia B, Giannone R, Castaldo D, De MF, Ricciardelli B, Colombo A (2010) Cystatin C and contrast-induced acute kidney injury. Circulation 121:2117–2122
Ebru AE, Kilic A, Korkmaz FS, Seker R, Sasmaz H, Demirtas S, Biyikli Z (2014) Is cystatin-C superior to creatinine in the early diagnosis of contrast-induced nephropathy?: a potential new biomarker for an old complication. J Postgrad Med 60:135–140
Quintavalle C, Fiore D, De MF, Visconti G, Focaccio A, Golia B, Ricciardelli B, Donnarumma E, Bianco A, Zabatta MA, Troncone G, Colombo A, Briguori C, Condorelli G (2012) Impact of a high loading dose of atorvastatin on contrast-induced acute kidney injury. Circulation 126:3008–3016
Ricci Z, Luciano R, Favia I, Garisto C, Muraca M, Morelli S, Di CL, Cogo P, Picardo S (2011) High-dose fenoldopam reduces postoperative neutrophil gelatinase-associated lipocaline and cystatin C levels in pediatric cardiac surgery. Crit Care 15:R160
Tanaga K, Tarao K, Nakamura Y, Inoue T, Jo K, Ishikawa T, Miyazaki A (2012) Percutaneous coronary intervention causes increase of serum cystatin C concentration even in the patients with a low risk of contrast-induced nephropathy. Cardiovasc Interv Ther 27:168–173
Zappitelli M, Krawczeski CD, Devarajan P, Wang Z, Sint K, Thiessen-Philbrook H, Li S, Bennett MR, Ma Q, Shlipak MG, Garg AX, Parikh CR (2011) Early postoperative serum cystatin C predicts severe acute kidney injury following pediatric cardiac surgery. Kidney Int 80:655–662
Zappitelli M, Greenberg JH, Coca SG, Krawczeski CD, Li S, Thiessen-Philbrook HR, Bennett MR, Devarajan P, Parikh CR (2015) Association of definition of acute kidney injury by cystatin C rise with biomarkers and clinical outcomes in children undergoing cardiac surgery. JAMA Pediatr 169:583–591
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Zappitelli M, Parvex P, Joseph L, Paradis G, Grey V, Lau S, Bell L (2006) Derivation and validation of cystatin C-based prediction equations for GFR in children. Am J Kidney Dis 48:221–230
Lagos-Arevalo P, Palijan A, Vertullo L, Devarajan P, Bennett MR, Sabbisetti V, Bonventre JV, Ma Q, Gottesman RD, Zappitelli M (2015) Cystatin C in acute kidney injury diagnosis: early biomarker or alternative to serum creatinine? Pediatr Nephrol 30:665–676
Alge JL, Arthur JM (2015) Biomarkers of AKI: a review of mechanistic relevance and potential therapeutic implications. Clin J Am Soc Nephrol 10:147–155
Chen LX, Koyner JL (2015) Biomarkers in Acute Kidney Injury. Crit Care Clin 31:633–648
de Geus HRH, Betjes MG, Bakker J (2012) Biomarkers for the prediction of acute kidney injury: a narrative review on current status and future challenges. Clin Kidney J 5:102–108
Endre ZH, Kellum JA, Di SS, Doi K, Goldstein SL, Koyner JL, Macedo E, Mehta RL, Murray PT (2013) Differential diagnosis of AKI in clinical practice by functional and damage biomarkers: workgroup statements from the tenth Acute Dialysis Quality Initiative Consensus Conference. Contrib Nephrol 182:30–44
Endre ZH, Pickering JW (2014) Acute kidney injury: cell cycle arrest biomarkers win race for AKI diagnosis. Nat Rev Nephrol 10:683–685
Wasung ME, Chawla LS, Madero M (2015) Biomarkers of renal function, which and when? Clin Chim Acta 438:350–357
Vanmassenhove J, Vanholder R, Nagler E, Van Biesen W (2012) Urinary and serum biomarkers for the diagnosis of acute kidney injury:an in depth review of the literature. Nephrol Dial Transplant 28:254–273
Ostermann M, Joannidis M (2015) Biomarkers for AKI improve clinical practice: no. Intensive Care Med 41:618–622
Meersch M, Schmidt C, Van AH, Rossaint J, Gorlich D, Stege D, Malec E, Januszewska K, Zarbock A (2014) Validation of cell-cycle arrest biomarkers for acute kidney injury after pediatric cardiac surgery. PLoS One 9:e110865
Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, Ruff SM, Zahedi K, Shao M, Bean J, Mori K, Barasch J, Devarajan P (2005) Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet 365:1231–1238
Westhoff JH, Tonshoff B, Waldherr S, Poschl J, Teufel U, Westhoff TH, Fichtner A (2015) Urinary tissue inhibitor of metalloproteinase-2 (TIMP-2) • insulin-like growth factor-binding protein 7 (IGFBP7) predicts adverse outcome in pediatric acute kidney injury. PLoS One 10:e0143628
Bell M, Larsson A, Venge P, Bellomo R, Martensson J (2015) Assessment of cell-cycle arrest biomarkers to predict early and delayed acute kidney injury. Dis Markers 2015:158658
Goldstein SL, Chawla LS (2010) Renal angina. Clin J Am Soc Nephrol 5:943–949
Chawla LS (2015) Introduction: sepsis-associated AKI. Semin Nephrol 35:1
Basu RK, Zappitelli M, Brunner L, Wang Y, Wong HR, Chawla LS, Wheeler DS, Goldstein SL (2014) Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int 85:659–667
Siew ED, Furth SL (2014) Acute kidney injury: a not-so-silent disease. Kidney Int 85:494–495
Basu RK, Wang Y, Wong HR, Chawla LS, Wheeler DS, Goldstein SL (2014) Incorporation of biomarkers with the renal angina index for prediction of severe AKI in critically ill children. Clin J Am Soc Nephrol 9:654–662
Siew ED, Davenport A (2015) The growth of acute kidney injury: a rising tide or just closer attention to detail? Kidney Int 87:46–61
Zappitelli M (2008) Epidemiology and diagnosis of acute kidney injury. Semin Nephrol 28:436–446
Jetton JG, Askenazi DJ (2012) Update on acute kidney injury in the neonate. Curr Opin Pediatr 24:191–196
Selewski DT, Symons JM (2014) Acute kidney injury. Pediatr Rev 35:30–41
Selewski DT, Charlton JR, Jetton JG, Guillet R, Mhanna MJ, Askenazi DJ, Kent AL (2015) Neonatal acute kidney injury. Pediatrics 136:e463–e473
Hsu CW, Symons JM (2010) Acute kidney injury: can we improve prognosis? Pediatr Nephrol 25:2401–2412
Bailey D, Phan V, Litalien C, Ducruet T, Merouani A, Lacroix J, Gauvin F (2007) Risk factors of acute renal failure in critically ill children: A prospective descriptive epidemiological study. Pediatr Crit Care Med 8:29–35
Sutherland SM, Byrnes JJ, Kothari M, Longhurst CA, Dutta S, Garcia P, Goldstein SL (2015) AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin J Am Soc Nephrol 10:554–561
Duzova A, Bakkaloglu A, Kalyoncu M, Poyrazoglu H, Delibas A, Ozkaya O, Peru H, Alpay H, Soylemezoglu O, Gur-Guven A, Bak M, Bircan Z, Cengiz N, Akil I, Ozcakar B, Uncu N, Karabay-Bayazit A, Sonmez F (2010) Etiology and outcome of acute kidney injury in children. Pediatr Nephrol 25:1453–1461
Pundziene B, Dobiliene D, Rudaitis S (2010) Acute kidney injury in pediatric patients: experience of a single center during an 11-year period. Medicina (Kaunas) 46:511–515
Zappitelli M, Moffett BS, Hyder A, Goldstein SL (2010) Acute kidney injury in non-critically ill children treated with aminoglycoside antibiotics in a tertiary healthcare centre: a retrospective cohort study. Nephrol Dial Transplant 26:144–150
Goldstein SL, Kirkendall E, Nguyen H, Schaffzin JK, Bucuvalas J, Bracke T, Seid M, Ashby M, Foertmeyer N, Brunner L, Lesko A, Barclay C, Lannon C, Muething S (2013) Electronic health record identification of nephrotoxin exposure and associated acute kidney injury. Pediatrics 132:e756–e767
Rheault MN, Zhang L, Selewski DT, Kallash M, Tran CL, Seamon M, Katsoufis C, Ashoor I, Hernandez J, Supe-Markovina K, Essandri-Silva C, Jesus-Gonzalez N, Vasylyeva TL, Formeck C, Woll C, Gbadegesin R, Geier P, Devarajan P, Carpenter SL, Kerlin BA, Smoyer WE (2015) AKI in children hospitalized with nephrotic syndrome. Clin J Am Soc Nephrol 10:2110–2118
Misurac JM, Knoderer CA, Leiser JD, Nailescu C, Wilson AC, Andreoli SP (2013) Nonsteroidal anti-inflammatory drugs are an important cause of acute kidney injury in children. J Pediatr 162:1153–1159
Sutherland SM, Ji J, Sheikhi FH, Widen E, Tian L, Alexander SR, Ling XB (2013) AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin J Am Soc Nephrol 8:1661–1669
McGregor TL, Jones DP, Wang L, Danciu I, Bridges BC, Fleming GM, Shirey-Rice J, Chen L, Byrne DW, Van Driest SL (2016) Acute kidney injury incidence in noncritically ill hospitalized children, adolescents, and young adults: a retrospective observational study. Am J Kidney Dis 67:384–390
Jenssen GR, Hovland E, Bangstad HJ, Nygard K, Vold L, Bjerre A (2014) The incidence and aetiology of acute kidney injury in children in Norway between 1999 and 2008. Acta Paediatr 103:1192–1197
Vachvanichsanong P, Dissaneewate P, Lim A, McNeil E (2006) Childhood acute renal failure: 22-year experience in a university hospital in southern Thailand. Pediatrics 118:e786–e791
Schneider J, Khemani R, Grushkin C, Bart R (2010) Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med 38:933–939
Chang JW, Jeng MJ, Yang LY, Chen TJ, Chiang SC, Soong WJ, Wu KG, Lee YS, Wang HH, Yang CF, Tsai HL (2015) The epidemiology and prognostic factors of mortality in critically ill children with acute kidney injury in Taiwan. Kidney Int 87:632–639
Selewski DT, Cornell TT, Heung M, Troost JP, Ehrmann BJ, Lombel RM, Blatt NB, Luckritz K, Hieber S, Gajarski R, Kershaw DB, Shanley TP, Gipson DS (2014) Validation of the KDIGO acute kidney injury criteria in a pediatric critical care population. Intensive Care Med 40:1481–1488
Basu RK, Kaddourah A, Terrell T, Mottes T, Arnold P, Jacobs J, Andringa J, Goldstein SL (2015) Assessment of Worldwide Acute Kidney Injury, Renal Angina and Epidemiology in critically ill children (AWARE): study protocol for a prospective observational study. BMC Nephrol 16:24
Lindle KA, Dinh K, Moffett BS, Kyle WB, Montgomery NM, Denfield SD, Knudson JD (2014) Angiotensin-converting enzyme inhibitor nephrotoxicity in neonates with cardiac disease. Pediatr Cardiol 35:499–506
McKamy S, Hernandez E, Jahng M, Moriwaki T, Deveikis A, Le J (2011) Incidence and risk factors influencing the development of vancomycin nephrotoxicity in children. J Pediatr 158:422–426
Moffett BS, Goldstein SL (2011) Acute kidney injury and increasing nephrotoxic-medication exposure in noncritically-ill children. Clin J Am Soc Nephrol 6:856–863
Moffett BS, Hilvers PS, Dinh K, Arikan AA, Checchia P, Bronicki R (2015) Vancomycin-associated acute kidney injury in pediatric cardiac intensive care patients. Congenit Heart Dis 10:E6–E10
Moffett BS, Goldstein SL, Adusei M, Kuzin J, Mohan P, Mott AR (2011) Risk factors for postoperative acute kidney injury in pediatric cardiac surgery patients receiving angiotensin-converting enzyme inhibitors. Pediatr Crit Care Med 12:555–559
Joo EJ, Peck KR, Ha YE, Kim YS, Song YG, Lee SS, Ryu SY, Moon C, Lee CS, Park KH (2013) Impact of acute kidney injury on mortality and medical costs in patients with meticillin-resistant Staphylococcus aureus bacteraemia: a retrospective, multicentre observational study. J Hosp Infect 83:300–306
Basu RK, Andrews A, Krawczeski C, Manning P, Wheeler DS, Goldstein SL (2013) Acute kidney injury based on corrected serum creatinine is associated with increased morbidity in children following the arterial switch operation. Pediatr Crit Care Med 14:e218–e224
Cao Y, Yi ZW, Zhang H, Dang XQ, Wu XC, Huang AW (2013) Etiology and outcomes of acute kidney injury in Chinese children: a prospective multicentre investigation. BMC Urol 13:41
Mammen C, Al AA, Skippen P, Nadel H, Levine D, Collet JP, Matsell DG (2012) Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis 59:523–530
Fortenberry JD, Paden ML, Goldstein SL (2013) Acute kidney injury in children: an update on diagnosis and treatment. Pediatr Clin N Am 60:669–688
Askenazi DJ, Feig DI, Graham NM, Hui-Stickle S, Goldstein SL (2006) 3–5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int 69:184–189
Cerda J (2008) World Kidney Day and acute kidney injury. Kidney Int 73:1441
Lameire NH, Bagga A, Cruz D, De Maeseneer J, Endre Z, Kellum JA, Liu KD, Mehta RL, Pannu N, Van Biesen W, Vanholder R (2013) Acute kidney injury: an increasing global concern. Lancet 382:170–179
Lewington AJ, Cerda J, Mehta RL (2013) Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int 84:457–467
Mehta RL, Cerda J, Burdmann EA, Tonelli M, Garcia-Garcia G, Jha V, Susantitaphong P, Rocco M, Vanholder R, Sever MS, Cruz D, Jaber B, Lameire NH, Lombardi R, Lewington A, Feehally J, Finkelstein F, Levin N, Pannu N, Thomas B, Ronoff-Spencer E, Remuzzi G (2015) International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet 385:2616–2643
Cerda J, Bagga A, Kher V, Chakravarthi RM (2008) The contrasting characteristics of acute kidney injury in developed and developing countries. Nat Clin Pract Nephrol 4:138–153
Cerda J, Lameire N, Eggers P, Pannu N, Uchino S, Wang H, Bagga A, Levin A (2008) Epidemiology of acute kidney injury. Clin J Am Soc Nephrol 3:881–886
Remuzzi G, Horton R (2013) Acute renal failure: an unacceptable death sentence globally. Lancet 382:2041–2042
Finkelstein FO, Smoyer WE, Carter M, Brusselmans A, Feehally J (2014) Peritoneal dialysis, acute kidney injury, and the Saving Young Lives program. Perit Dial Int 34:478–480
Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, Jaber BL, for the Acute Kidney Advisory Group of the American society of Nephrology (2013) World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol 8:1482–1493
Jha V, Parameswaran S (2013) Community-acquired acute kidney injury in tropical countries. Nat Rev Nephrol 9:278–290
Lameire N, Van Biesen W, Vanholder R (2006) The changing epidemiology of acute renal failure. Nat Clin Pract Nephrol 2:364–377
Lombardi R, Yu L, Younes-Ibrahim M, Schor N, Burdmann EA (2008) Epidemiology of acute kidney injury in Latin America. Semin Nephrol 28:320–329
Naicker S, Aboud O, Gharbi MB (2008) Epidemiology of acute kidney injury in Africa. Semin Nephrol 28:348–353
Olowu WA, Niang A, Osafo C, Ashuntantang G, Arogundade FA, Porter J, Naicker S, Luyckx VA (2016) Outcomes of acute kidney injury in children and adults in sub-Saharan Africa: a systematic review. Lancet Glob Health 4:e242–e250
Aloni MN, Nsibu CN, Meeko-Mimaniye M, Ekulu PM, Bodi JM (2012) Acute renal failure in Congolese children: a tertiary institution experience. Acta Paediatr 101:e514–e518
Balaka B, Agbere D, Bonkoungou P, Gnamey D, Kessie K, Assimadi K (2003) Post-hemolytic renal failure in children with glucose-6-phosphate dehydrogenase deficiency at the University Hospital Center in Lome. Med Trop (Mars) 63:151–154
Bodi JM, Nsibu CN, Aloni MN, Lukute GN, Kunuanuna TS, Tshibassu PM, Pakasa N (2014) Black water fever associated with acute renal failure among Congolese children in Kinshasa. Saudi J Kidney Dis Transpl 25:1352–1358
Burchard GD, Ehrhardt S, Mockenhaupt FP, Mathieu A, Gana-Nsiire P, Anemana SD, Otchwemah RN, Abel W, Brattig N (2003) Renal dysfunction in children with uncomplicated, Plasmodium falciparum malaria in Tamale, Ghana. Ann Trop Med Parasitol 97:345–350
Olowu WA, Adefehinti O, Bisiriyu AL (2012) Hospital-acquired acute kidney injury in critically ill children and adolescents. Saudi J Kidney Dis Transpl 23:68–77
Esezobor CI, Ladapo TA, Osinaike B, Lesi FE (2012) Paediatric acute kidney injury in a tertiary hospital in Nigeria: prevalence, causes and mortality rate. PLoS One 7:e51229
Abdelraheem M, Ali ET, Osman R, Ellidir R, Bushara A, Hussein R, Elgailany S, Bakhit Y, Karrar M, Watson A, Abu-Aisha H (2014) Outcome of acute kidney injury in Sudanese children—an experience from a sub-Saharan African unit. Perit Dial Int 34:526–533
Perico N, Remuzzi G (2016) Acute kidney injury in low-income and middle-income countries: no longer a death sentence. Lancet Glob Health 4:e216–e217
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Norbert Lameire and Raymond Vanholder are emeritus professor of medicine.
Rights and permissions
About this article
Cite this article
Lameire, N., Van Biesen, W. & Vanholder, R. Epidemiology of acute kidney injury in children worldwide, including developing countries. Pediatr Nephrol 32, 1301–1314 (2017). https://doi.org/10.1007/s00467-016-3433-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3433-2