Abstract
Acute kidney injury (AKI) is characterized clinically as an abrupt decline in renal function marked by reduced excretion of waste products, disordered electrolytes, and disrupted fluid homeostasis. The recent development of a standardized AKI definition has transformed our understanding of AKI epidemiology and outcomes. We now know that in the short term, children with AKI experience greater morbidity and mortality; additionally, observational studies have established that chronic renal sequelae are far more common after AKI events than previously realized. Many of these studies suggest that patients who develop AKI are at greater risk for the subsequent development of chronic kidney disease (CKD). The goal of this review is to critically evaluate the data regarding the association between AKI and CKD in children. Additionally, we describe best practice approaches for future studies, including the use of consensus AKI criteria, the application of rigorous definitions for CKD and renal sequelae, and the inclusion of non-AKI comparator groups. Finally, based upon existing data, we suggest an archetypal approach to follow-up care for the AKI survivors who may be at greater CKD risk, including children with more severe AKI, those who endure repeated AKI episodes, patients who do not experience full recovery, and those with pre-existing CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI), known previously as acute renal failure, is defined as an abrupt decline in renal function resulting in impaired elimination of waste products and dysregulation of electrolytes, acid–base status, and fluid balance [1]. AKI is a common complication among hospitalized children, and the incidence is rising, particularly in developed countries where AKI tends to be caused by systemic diseases or the treatments they necessitate [2,3,4]. Recent data suggest that AKI occurs in 27% of children receiving intensive care and in at least 5% of non-critically ill pediatric patients [5, 6].
AKI has been associated with poorer short-term outcomes; children who develop AKI while hospitalized experience greater mortality, longer lengths of stay, and prolonged mechanical ventilation [1, 6,7,8]. More recently, investigators have established an association between AKI and long-term sequelae as well [9]. Previously thought to be a self-limited phenomenon, newer data have linked AKI with long-term renal morbidity, including proteinuria, hypertension, and chronic kidney disease (CKD) [10,11,12,13,14,15]. The potential ramifications of this association are profound since CKD is associated with neurodevelopmental impairment, anemia, bone disease, growth failure, and cardiovascular morbidity [16, 17]. Although not conclusive, emerging evidence of this connection is compelling. However, the association remains under-recognized, and pediatric AKI survivors rarely receive follow-up care or serial monitoring of renal function [18,19,20]. For example, a recent study examined a cohort of patients who developed AKI while in the intensive care unit (ICU) [21]. Of the children with AKI who survived to be transferred out of the ICU, only 66% had a follow-up creatinine measurement obtained between ICU transfer and hospital discharge. Similarly, Greenberg et al. demonstrated that fewer than 5% of children who experienced AKI after cardiac surgery saw a nephrologist subsequent to discharge [18]. A more comprehensive understanding of the relationship between AKI and CKD, as well as a more definitive resolution to the causative question must be a high priority for the critical care and nephrology communities since it is possible to effectively treat CKD sequelae and slow progression if an accurate and early diagnosis can be made [16, 19, 22].
The goal of this educational review is to summarize the data describing the association between AKI events and the subsequent development of CKD in children and young adults. We emphasize the following: (1) the structural and parenchymal changes which occur in the kidney following AKI, (2) the best available data from adult studies, (3) the totality of the data available from pediatric studies, and (4) the gaps in the existing data and recommendations for further research studies. While a comprehensive review of the AKI/CKD relationship in neonates is beyond the scope of this manuscript, there have been several excellent manuscripts published recently which may serve as complementary references [23,24,25,26].
Pathophysiology and structural changes following AKI
Regardless of underlying disease and cause of injury, the final common pathway for progressive renal dysfunction is fibrosis of the tubulointerstitial compartment [27, 28]. Experimental models have demonstrated that AKI is indeed associated with the development of tubular atrophy, reduced peritubular capillary density, and interstitial fibrosis; inflammation, ischemia and parenchymal hypoxia, endothelial damage, capillary rarefaction, and reperfusion injury all contribute to the profibrotic environment of AKI events [9, 27,28,29,30,31,32]. Interestingly, fibrosis is a self-limited process which is designed to confine the extent of an injury; it is not progressive in its own right [27]. Thus, while an episode of AKI creates a local environment which is conducive to fibrosis, additional factors are required for progressive injury and dysfunction to develop.
Although these mechanisms are not completely understood, animal models have provided some insight. One fundamental concept is that of renal mass reduction [27, 29]. Experimental models have demonstrated that in the setting of AKI, reduced renal mass enhances injury and is associated with progressive decline in function [27, 33]. Reduced renal mass has this effect whether it is due to pre-existing CKD, recurrent episodes of injury, or a single profoundly severe episode of AKI. In the setting of reduced nephron mass, tubular repair and regeneration becomes maladaptive [9, 27, 33]. Tubules fail to differentiate, do not regain normal function, and continue to produce proinflammatory and profibrotic signals [27]. Additionally, some models suggest that medullary injury may play a significant role in progressive dysfunction. The renal medulla, which is profoundly hypoxic, is particularly sensitive to ischemic injury [27, 34]. The ischemic and inflammatory environment of AKI further reduces oxygenation within the medulla and impairs tubular regeneration and repair. This hypoxic milieu may persist beyond the initial injury and has the potential to affect large swaths of cortex through hemodynamic and obstructive mechanisms [27, 31, 34]. As tubules and endothelial cells undergo maladaptive repair and atrophy, additional stress is placed upon the remaining, functional parenchyma. Tubules undergo hypertrophy and vascular autoregulation is impaired. Systemic and intrarenal hypertension is transmitted unabated to the glomeruli, causing progressive injury and hyperfiltration [27]. Although further work is needed to completely elucidate the mechanisms behind progressive dysfunction following AKI, it does seem clear that processes independent of the initial inciting event contribute to the decline.
AKI and CKD studies in adult patients
While some controversy remains, an association between AKI and CKD has been endorsed in nearly all of the adult literature over the past decade [9]. The remaining debate centers on the causative aspect of the relationship; few authors debate that AKI and CKD are interconnected, but some remain unsure whether AKI actually causes CKD [9, 32, 35]. The association has been demonstrated in a number of observational studies. For example, in one study cohort comprising 233,803 elderly patients, the risk of end-stage renal disease (ESRD) was 13-fold higher following an episode of AKI [36]. A study involving more than 500,000 adults demonstrated that AKI severe enough to require renal replacement therapy is associated with a 28-fold higher risk of developing Stage 4/5 CKD [37]. Finally, a meta-analysis of 13 studies found that adults who survived AKI had an 8.8-fold higher risk of CKD and a 3.1-fold higher risk of ESRD [11].
While some concerns about confounding, ascertainment bias and definitional/classification issues (with both AKI and CKD) have been raised, there are a number of strong arguments which support the concept that AKI has a causative relationship with CKD [35]. The first is that while many published studies have been observational, these have found that the effect of AKI on the development of CKD remains after adjustment for demographics, potential confounders, and risk factors: these studies have found that AKI is independently associated with CKD [10, 11, 36, 37]. Secondly, there is a dose-dependent effect [10, 38, 39]. Ishani et al. examined AKI severity among nearly 30,000 adults who had undergone cardiac surgery [38]. They found that the magnitude of creatinine rise was directly related to the risk for incident CKD. Thakar et al. found that among more than 3600 diabetics, AKI was independently associated with an increased risk of Stage 4 CKD and that each subsequent AKI episode doubled that risk [39]. Thus, data support the concept that more severe AKI is associated with greater CKD risk and that subsequent AKI events increase the cumulative risk. Finally, there is clear evidence that among patients with pre-existing CKD, AKI events accelerate CKD progression [38, 40, 41]. For example, the aforementioned Ishani et al. article found that AKI was associated with progression of CKD stage and that larger creatinine changes were correlated with greater risk [38]. Thus, while it is not possible to say unequivocally that AKI causes CKD, the best data currently available among adult patients support the claim that CKD can be a sequelae of AKI events.
AKI and CKD studies in pediatric patients
The enduring effects of renal disease have been described in various circumstances. For example, post-streptococcal glomerulonephritis (PSGN) and hemolytic uremic syndrome (HUS), two of the more common acute renal disorders seen in children, have both been associated with long-term renal abnormalities [42,43,44]. Though they did not characterize the nature of the acute renal disease, Hoy et al. demonstrated that episodes of PSGN are a risk factor for albuminuria and CKD years later [42]. Similarly, Garg and colleagues demonstrated that 4 years after HUS, 25% of children experienced persistent renal sequelae [hypertension, proteinuria, and/or a reduced glomerular filtration rate (GFR)] and 3% developed ESRD [43]. This meta-analysis did not report AKI rates or describe the severity of renal involvement; however, they did find that CKD risk was higher in patients who required dialysis, echoing the dose-dependent effect described in adults.
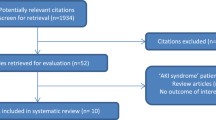
Similarly, a number of studies have demonstrated that long-term renal sequelae are highly prevalent, specifically in the setting of AKI (Table 1). Askenazi et al. examined 29 children with AKI (based upon diagnostic coding) and found that both proteinuria and hypertension occurred in more than 20% of survivors; hyperfiltration (31%) and an estimated GFR (eGFR) of < 90 mL/min/1.73 m2 (13.8%) were also common [14]. Buysse and colleagues studied 19 children who developed AKI (defined by a creatinine level of twofold the normal value) after septic shock events and found nearly identical rates of hypertension and proteinuria 10 years later [51]. Studies by Hingorani and Kist-van Holthe found that AKI is a risk factor for CKD among children receiving stem cell transplants [52, 56]. Specifically, Hingorani et al. found that AKI (doubling of serum creatinine level) increased the risk for CKD (eGFR < 60 mL/min/1.73 m2) by 70% [52]. Mammen et al. reviewed 126 AKI survivors [Acute Kidney Injury Network (AKIN) Stage 1 or greater] 1–3 years after ICU discharge. They found only moderate rates of hypertension (3.2%) and proteinuria (9.5%); however, nearly 40% of these children had an eGFR of < 90 mL/min/1.73 m2 [13]. While these data are compelling, a meta-analysis performed in 2014 underscored some of the issues plaguing available data [57], specifically noting that the studies they reviewed had widely variable follow-up timeframes, identified AKI in a variety of ways, and defined outcomes in dissimilar manners. The number of patients lost to follow-up was substantial, which raises concern for ascertainment bias. Additionally, nearly all of the studies available failed to include a non-AKI comparator group.
Since then, the majority of studies have used, at a minimum, one of the available consensus definitions for AKI. While they have continued to employ disparate definitions for long-term renal sequelae, many of these studies have compared outcomes between AKI and non-AKI cohorts. One such study examined hypertension rates among pediatric stem cell transplant survivors. The authors of this study found that while high blood pressure was common across the entire population, AKI [defined as doubling of serum creatinine level, equivalent to Kidney Disease: Improving Global Outcomes (KDIGO) Stage 2 or greater] was associated with a 2.5-fold increased risk for the development of hypertension. Menon et al. examined 100 children who developed nephrotoxic AKI (NTx-AKI) and found impressively high rates of proteinuria (68.5%), hypertension (37.6%), and an eGFR of < 90 mL/min/1.73 m2 (23.4%) [15]. When compared with matched non-AKI controls, those who experienced NTx-AKI had a significantly lower eGFR, more proteinuria, and a higher incidence of hypertension [15]. One of the few studies to use a rigorous definition for both AKI and CKD (eGFR < 60 mL/min/1.73 m2 for longer than 3 months) examined a pediatric heart transplant cohort. While the authors did not find an association between AKI and the subsequent development of CKD, they did find that patients with unrecovered AKI (a proxy for injury severity) were significantly more likely to have CKD (eGFR < 60 mL/min/1.73 m2 for more than 3 months) [47].
Two recently published studies deserve special mention since they represent two of the few truly prospective reports on the subject. The first represents a 5-year follow-up of the Translational Research Investigating Biomarker Endpoints in AKI (TRIBE-AKI) study. This analysis found that hypertension (17%), proteinuria (8%), and an eGFR of < 90 mL/min/1.73 m2 (13%) were common following cardiac surgery. However, these sequelae were not more common among the children who experienced perioperative AKI [18]. In the second study, entitled, “Follow-up Renal Assessment of Injury Long-term after AKI (FRAIL-AKI)”, the authors compared renal findings in 51 children 7 years after they had undergone cardiopulmonary bypass. The 31 AKI and 18 non-AKI patients had similar rates of proteinuria and hypertension as well as comparable eGFRs [45]. However, those with AKI did have higher urinary biomarker levels of interleukin-18 and liver-type fatty acid binding protein (L-FABP) than either the non-AKI patients or healthy controls. This result certainly suggests that patients who experience AKI may have subtle evidence of chronic renal injury even in the absence of overt CKD. Interestingly, a subsequently published study did find that cardiac surgery-associated AKI was associated with a greater risk for CKD Stage 2 or greater [46]. In that study, the 5-year cumulative incidence of CKD for patients with cardiac surgery-associated AKI was 12% [95% confidence interval (CI) 7–20%], which was significantly higher than the 3% (95% CI 1–5%) seen in those without AKI (adjusted hazard ratio 3.8; 95% CI: 1.4–10.4). While this study was retrospective in nature, it was large and used a consensus definition for AKI and a rigorous definition of CKD.
Making sense of the data
Taken in total, the best available data in children, when combined with the existing adult findings, demonstrate that chronic renal sequelae are common following episodes of AKI and suggest that AKI may predispose patients to CKD. Many studies have found incident rates of hypertension, proteinuria, and reduced GFR that far exceed those in healthy populations. Additionally, most pediatric studies have found a dose-dependent association between AKI severity and CKD risk similar to that seen in adult studies. That said, several issues have limited our ability to definitively identify a causal relationship. While the vast majority of current studies are using a consensus AKI definition, few are using a rigorous definition of CKD. In many studies, proteinuria, hypertension, eGFR < 90 mL/min/1.73 m2, eGFR < 60 mL/min/1.73 m2, and hyperfiltration are grouped into a composite outcome of “renal dysfunction.” Even in those where individual outcomes are evaluated separately, the manner in which they are assessed may differ (i.e., eGFR vs. measured GFR; spot urine sample vs. 24-h collection; casual blood pressure measurement vs. ambulatory blood pressure monitoring). This general lack of specificity and standardization makes interpretation of the available data challenging. Additionally, it is clear that the underlying disease has a tremendous impact on short-term AKI outcomes, and it would stand to reason that this would be true for CKD and other long-term sequelae. The severity of ICU-associated AKI is likely very different than that seen in non-ICU patients; more substantial injury is likely to have greater chronic ramifications for the physiologic reasons described above. This concept is related to that of the differential effect seen between AKI etiologies. It is likely that the direct tubular toxicity of profound nephrotoxic injury has a different impact than that of cardiopulmonary bypass. Given these issues and the limitations surrounding the currently available data, it is not surprising that a conclusive causative link between AKI and CKD has not been identified. What is clear, however, is that a very strong observational signal exists, and evidence suggests that certain factors confer a greater CKD risk than others (Fig. 1).
Risk for developing chronic kidney disease (CKD) across the spectrum of acute kidney injury (AKI). In the setting of AKI, observational evidence suggests that severe AKI events are more likely to be associated with chronic findings than mild events; so are repeated AKI events, independent of severity. Perhaps the greatest risk for chronic renal disease after AKI is pre-existing CKD. As the events which precipitated AKI abate, renal function begins to recover; non-recovery of AKI has been associated with greater CKD risk. Chronic renal injury has gradation as well. At its most mild form, chronic renal injury may manifest as proteinuria or hypertension. More severe injury may manifest with a mildly reduced glomerular filtration rate, and the most severe injuries may be associated with moderate/severe CKD
Summary and future directions
Available observational data raise significant concerns for chronic kidney injury and disease among AKI survivors. Given the profound consequences associated with undiagnosed and untreated CKD, it is imperative that this relationship be studied more effectively. We suggest that future studies adopt rigorous definitions for AKI, CKD, and renal sequelae (Table 2). While it is reasonable to use any of the recently developed consensus definitions for AKI [pediatric Risk, Injury, Failure, Loss of kidney function, End-stage kidney disease (pRIFLE), AKIN, KDIGO], we recommend that studies use the KDIGO definition when possible [8, 58, 61]. This is the only definition which can be used in both adults and children, and it represents the harmonization of all previously available AKI criteria [58]. We believe it is important to describe individual chronic outcomes (i.e., proteinuria, hypertension, eGFR) separately when appropriate. Certainly, proteinuria or hypertension can be a component of a CKD diagnosis; however, even in the absence of a reduced GFR these outcomes have significance and should be reported if available. Additionally, we agree that the established, consensus definition of CKD should be utilized [62]. CKD may be defined at a GFR of < 60 mL/min/1.73 m2 or at a higher GFR when there is evidence of kidney injury/damage, as long as either criteria is present at least 3 months after the AKI event (Table 2). We also advocate for an additional category which has been previously described as being “at risk” for CKD [13]. At risk for CKD is defined as a GFR which is between 60 and 90 mL/min/1.73 m2 in the absence of signs of kidney damage/injury; this may be particularly useful when no data exist to assess signs of kidney damage or injury beyond eGFR. This is an important cohort to identify and monitor since there is evidence that even mild/moderate CKD is associated with reduced health-related quality of life, poorer neurocognitive function, and cardiovascular morbidity, including left ventricular hypertrophy and elevated carotid intima-media thickness [63,64,65,66]. Finally, we recommend avoiding the use of hyperfiltration as a CKD-related outcome because its inclusion may obscure the AKI–CKD relationship, mainly due to the inaccuracies associated with GFR estimating equations and the absence of a consensus definition for hyperfiltration.
While additional, more uniform studies are necessary, we feel that there is sufficient data supporting the association between AKI and CKD that clinical assessment may be warranted in many patients who experience AKI. Currently, no guidelines exist regarding the subset of patients that should be followed, the length and frequency of the follow-up, or the parameters which should be monitored. However, the KIDGO guidelines do suggest that AKI survivors should be re-evaluated 3 months after the event to assess for resolution of AKI, the development of new onset CKD, and (if applicable) progression of pre-existing CKD [58]. Patients who have CKD should be managed according to the appropriate clinical practice parameters; patients who do not yet have CKD may benefit from being considered at higher risk for CKD. This strategy would entail heightened awareness of nephrotoxins, avoidance of additional risk factors, and repeated periodic assessment [16]. Given the frequency with which we now see AKI in hospitalized children, it may prove challenging operationally to provide follow-up care for all such patients. We may find that it is necessary to risk stratifying the AKI cohort in order to identify a subgroup which is at higher CKD risk and which would benefit more greatly from monitoring. To date, causative risk factors are unknown; however, we may find that we can prioritize follow-up care based on a number of factors, including AKI severity, non-recovery of baseline function, location of event (ICU vs. acute care), urinary biomarker data, or recurrence.
In summary, the association between AKI and CKD is well established. To identify a causal relationship, however, it will be important to apply rigorous and standard definitions for AKI and CKD-related outcomes. It will be even more important to do so within large studies across a variety of pediatric populations which include comparative cohorts without AKI. Given the currently available data, many AKI survivors are likely to benefit from longitudinal follow-up and assessment of renal disease and dysfunction.
Key summary points
-
1.
Currently available data suggest that chronic renal disease (CKD, hypertension, proteinuria) is common among AKI survivors.
-
2.
AKI survivors who are likely to be at higher risk for the development of CKD and long-term sequelae should receive appropriate investigations which may include nephrology follow-up care, assessment of renal function, urine studies, and blood pressure monitoring.
-
3.
All future studies examining the relationship between AKI and CKD should use consensus definitions for AKI, CKD, and longitudinal renal sequelae.
Review questions (answers are provided following the reference list)
-
1.
True or false. Chronic renal findings are infrequently found in patients who experience AKI and survive to hospital discharge?
-
2.
Following an episode of AKI, what is the most appropriate time to assess survivors for CKD?
-
a)
1 week
-
b)
1 month
-
c)
3 months
-
d)
3 years
-
3.
Which of the following should be monitored in a patient who has experienced AKI and is thought to be at high risk for chronic renal disease?
-
a)
Urine protein content
-
b)
Serum creatinine
-
c)
Blood pressure
-
d)
All of the above
-
4.
Which of the following are currently hampering our ability to assess the causal association between AKI and CKD?
-
a)
A lack of studies containing a non-AKI comparator group
-
b)
Inconsistent definitions of AKI
-
c)
The absence of a consensus definition for CKD
-
d)
The infrequency with which AKI is seen in hospitalized patients
-
5.
CKD in children is defined as:
-
a)
Serum creatinine of ≥ 3 mg/dL (265 umol/L)
-
b)
GFR < 60 mL/min/1.73 m2
-
c)
GFR > 180 mL/min/1.73 m2
-
d)
GFR 60–90 mL/min/1.73 m2 with evidence of kidney injury or damage
-
e)
b and d
References
Sutherland SM, Byrnes JJ, Kothari M, Longhurst CA, Dutta S, Garcia P, Goldstein SL (2015) AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin J Am Soc Nephrol 10:554–561
Hui-Stickle S, Brewer ED, Goldstein SL (2005) Pediatric ARF epidemiology at a tertiary care center from 1999 to 2001. Am J Kidney Dis 45:96–101
Williams DM, Sreedhar SS, Mickell JJ, Chan JC (2002) Acute kidney failure: a pediatric experience over 20 years. Arch Pediatr Adolesc Med 156:893–900
Goldstein SL (2011) Acute kidney injury in children: prevention, treatment and rehabilitation. Contrib Nephrol 174:163–172
McGregor TL, Jones DP, Wang L, Danciu I, Bridges BC, Fleming GM, Shirey-Rice J, Chen L, Byrne DW, Van Driest SL (2016) Acute kidney injury incidence in noncritically ill hospitalized children, adolescents, and young adults: a retrospective observational study. Am J Kidney Dis 67:384–390
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, Investigators AWARE (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20
Sutherland SM (2013) AKI in hospitalized children: epidemiology and clinical associations in a national cohort. J Pediatr 8:1661–1669
Alkandari O, Eddington KA, Hyder A, Gauvin F, Ducruet T, Gottesman R, Phan V, Zappitelli M (2011) Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit Care 15:R146
Chawla LS, Eggers PW, Star RA, Kimmel PL (2014) Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med 371:58–66
Chawla LS, Amdur RL, Amodeo S, Kimmel PL, Palant CE (2011) The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int 79:1361–1369
Coca SG, Singanamala S, Parikh CR (2012) Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int 81:442–448
Hsu CY, Hsu RK, Yang J, Ordonez JD, Zheng S, Go AS (2016) Elevated BP after AKI. J Am Soc Nephrol 27:914–923
Mammen C, Al Abbas A, Skippen P, Nadel H, Levine D, Collet JP, Matsell DG (2012) Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis 59:523–530
Askenazi DJ, Feig DI, Graham NM, Hui-Stickle S, Goldstein SL (2006) 3-5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int 69:184–189
Menon S, Kirkendall ES, Nguyen H, Goldstein SL (2014) Acute kidney injury associated with high nephrotoxic medication exposure leads to chronic kidney disease after 6 months. J Pediatr 165:522–527
Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, Kurella Tamura M, Feldman HI (2014) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis 63:713–735
Stevens PE, Levin A (2013) Kidney disease: improving global outcomes chronic kidney disease guideline development work group members. Ann Intern Med 158:825–830
Greenberg JH, Zappitelli M, Devarajan P, Thiessen-Philbrook HR, Krawczeski C, Li S, Garg AX, Coca S, Parikh CR, TRIBE-AKI Consortium (2016) Kidney outcomes 5 years after Pediatric cardiac surgery: the TRIBE-AKI study. JAMA Pediatr 170:1071–1078
Goldstein SL, Jaber BL, Faubel S, Chawla LS, Acute Kidney Injury Advisory Group of American Society of Nephrology (2013) AKI transition of care: a potential opportunity to detect and prevent CKD. Clin J Am Soc Nephrol 8:476–483
Silver SA, Goldstein SL, Harel Z, Harvey A, Rompies EJ, Adhikari NK, Acedillo R, Jain AK, Richardson R, Chan CT, Chertow GM, Bell CM, Wald R (2015) Ambulatory care after acute kidney injury: an opportunity to improve patient outcomes. Can J Kidney Health Dis 2:36
Hessey E, Ali R, Dorais M, Morissette G, Pizzi M, Rink N, Jouvet P, Lacroix J, Phan V, Zappitelli M (2017) Renal function follow-up and renal recovery after acute kidney injury in critically ill children. Pediatr Crit Care Med 18:733–740
Wong CJ, Moxey-Mims M, Jerry-Fluker J, Warady BA, Furth SL (2012) CKiD (CKD in children) prospective cohort study: a review of current findings. Am J Kidney Dis 60:1002–1011
Chaturvedi S, Ng KH, Mammen C (2017) The path to chronic kidney disease following acute kidney injury: a neonatal perspective. Pediatr Nephrol 32:227–241
Harer MW, Pope CF, Conaway MR, Charlton JR (2017) Follow-up of acute kidney injury in neonates during childhood years (FANCY): a prospective cohort study. Pediatr Nephrol 32:1067–1076
Selewski DT, Charlton JR, Jetton JG, Guillet R, Mhanna MJ, Askenazi DJ, Kent AL (2015) Neonatal acute kidney injury. Pediatrics 136:e463–e473
Nada A, Bonachea EM, Askenazi DJ (2017) Acute kidney injury in the fetus and neonate. Semin Fetal Neonatal Med 22:90–97
Venkatachalam MA, Weinberg JM, Kriz W, Bidani AK (2015) Failed tubule recovery, AKI-CKD transition, and kidney disease progression. J Am Soc Nephrol 26:1765–1776
Nath KA (1992) Tubulointerstitial changes as a major determinant in the progression of renal damage. Am J Kidney Dis 20:1–17
Venkatachalam MA, Griffin KA, Lan R, Geng H, Saikumar P, Bidani AK (2010) Acute kidney injury: a springboard for progression in chronic kidney disease. Am J Physiol Renal Physiol 298:F1078–F1094
Nath KA, Croatt AJ, Haggard JJ, Grande JP (2000) Renal response to repetitive exposure to heme proteins: chronic injury induced by an acute insult. Kidney Int 57:2423–2433
Basile DP, Donohoe D, Roethe K, Osborn JL (2001) Renal ischemic injury results in permanent damage to peritubular capillaries and influences long-term function. Am J Physiol Renal Physiol 281:F887–F899
Hsu CY (2012) Yes, AKI truly leads to CKD. J Am Soc Nephrol 23:967–969
Polichnowski AJ, Lan R, Geng H, Griffin KA, Venkatachalam MA, Bidani AK (2014) Severe renal mass reduction impairs recovery and promotes fibrosis after AKI. J Am Soc Nephrol 25:1496–1507
Basile DP, Donohoe DL, Roethe K, Mattson DL (2003) Chronic renal hypoxia after acute ischemic injury: effects of L-arginine on hypoxia and secondary damage. Am J Physiol Renal Physiol 284:F338–F348
Rifkin DE, Coca SG, Kalantar-Zadeh K (2012) Does AKI truly lead to CKD? J Am Soc Nephrol 23:979–984
Ishani A, Xue JL, Himmelfarb J, Eggers PW, Kimmel PL, Molitoris BA, Collins AJ (2009) Acute kidney injury increases risk of ESRD among elderly. J Am Soc Nephrol 20:223–228
Lo LJ, Go AS, Chertow GM, McCulloch CE, Fan D, Ordonez JD, Hsu CY (2009) Dialysis-requiring acute renal failure increases the risk of progressive chronic kidney disease. Kidney Int 76:893–899
Ishani A, Nelson D, Clothier B, Schult T, Nugent S, Greer N, Slinin Y, Ensrud KE (2011) The magnitude of acute serum creatinine increase after cardiac surgery and the risk of chronic kidney disease, progression of kidney disease, and death. Arch Intern Med 171:226–233
Thakar CV, Christianson A, Himmelfarb J, Leonard AC (2011) Acute kidney injury episodes and chronic kidney disease risk in diabetes mellitus. Clin J Am Soc Nephrol 6:2567–2572
Hsu CY, Chertow GM, McCulloch CE, Fan D, Ordonez JD, Go AS (2009) Nonrecovery of kidney function and death after acute on chronic renal failure. Clin J Am Soc Nephrol 4:891–898
Hsu RK, Hsu CY (2016) The role of acute kidney injury in chronic kidney disease. Semin Nephrol 36:283–292
Hoy WE, White AV, Dowling A, Sharma SK, Bloomfield H, Tipiloura BT, Swanson CE, Mathews JD, McCredie DA (2012) Post-streptococcal glomerulonephritis is a strong risk factor for chronic kidney disease in later life. Kidney Int 81:1026–1032
Garg AX, Suri RS, Barrowman N, Rehman F, Matsell D, Rosas-Arellano MP, Salvadori M, Haynes RB, Clark WF (2003) Long-term renal prognosis of diarrhea-associated hemolytic uremic syndrome: a systematic review, meta-analysis, and meta-regression. JAMA 290:1360–1370
Garg AX, Salvadori M, Okell JM, Thiessen-Philbrook HR, Suri RS, Filler G, Moist L, Matsell D, Clark WF (2008) Albuminuria and estimated GFR 5 years after Escherichia Coli O157 hemolytic uremic syndrome: an update. Am J Kidney Dis 51:435–444
Cooper DS, Claes D, Goldstein SL, Bennett MR, Ma Q, Devarajan P, Krawczeski CD (2016) Follow-up renal assessment of injury long-term after acute kidney injury (FRAIL-AKI). Clin J Am Soc Nephrol 11:21–29
Madsen NL, Goldstein SL, Froslev T, Christiansen CF, Olsen M (2017) Cardiac surgery in patients with congenital heart disease is associated with acute kidney injury and the risk of chronic kidney disease. Kidney Int 92:751–756
Hollander SA, Montez-Rath ME, Axelrod DM, Krawczeski CD, May LJ, Maeda K, Rosenthal DN, Sutherland SM (2016) Recovery from acute kidney injury and CKD following heart transplantation in children, adolescents, and young adults: a retrospective cohort study. Am J Kidney Dis 68:212–218
Mel E, Davidovits M, Dagan O (2014) Long-term follow-up evaluation of renal function in patients treated with peritoneal dialysis after cardiac surgery for correction of congenital anomalies. J Thorac Cardiovasc Surg 147:451–455
Viaud M, Llanas B, Harambat J (2012) Renal outcome in long-term survivors from severe acute kidney injury in childhood. Pediatr Nephrol 27:151–152. Author reply 153
Hoffmeister PA, Hingorani SR, Storer BE, Baker KS, Sanders JE (2010) Hypertension in long-term survivors of pediatric hematopoietic cell transplantation. Biol Blood Marrow Transplant 16:515–524
Buysse CM, Raat H, Hazelzet JA, Hulst JM, Cransberg K, Hop WC, Vermunt LC, Utens EM, Maliepaard M, Joosten KF (2008) Long-term health status in childhood survivors of meningococcal septic shock. Arch Pediatr Adolesc Med 162:1036–1041
Hingorani S, Guthrie KA, Schoch G, Weiss NS, McDonald GB (2007) Chronic kidney disease in long-term survivors of hematopoietic cell transplant. Bone Marrow Transplant 39:223–229
Slack R, Hawkins KC, Gilhooley L, Addison GM, Lewis MA, Webb NJ (2005) Long-term outcome of meningococcal sepsis-associated acute renal failure. Pediatr Crit Care Med 6:477–479
Shaw NJ, Brocklebank JT, Dickinson DF, Wilson N, Walker DR (1991) Long-term outcome for children with acute renal failure following cardiac surgery. Int J Cardiol 31:161–165
Georgaki-Angelaki HN, Steed DB, Chantler C, Haycock GB (1989) Renal function following acute renal failure in childhood: a long term follow-up study. Kidney Int 35:84–89
Kist-van Holthe JE, Bresters D, Ahmed-Ousenkova YM, Goedvolk CA, Abbink FC, Wolterbeek R, Bredius RG, Pauwels EK, van der Heijden AJ (2005) Long-term renal function after hemopoietic stem cell transplantation in children. Bone Marrow Transplant 36:605–610
Greenberg JH, Coca S, Parikh CR (2014) Long-term risk of chronic kidney disease and mortality in children after acute kidney injury: a systematic review. BMC Nephrol 15:184
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int 2:1–138
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM, Subcommittee On Screening and Management Of High Blood Pressure In Children (2017) Clinical practice guideline for screening and Management of High Blood Pressure in children and adolescents. Pediatrics 140(3). https://doi.org/10.1542/peds.2017-3035
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr (2017) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and Management of High Blood Pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. https://doi.org/10.1161/HYP.0000000000000065
Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL (2007) Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int 71:1028–1035
National Center for Biotechnology Information, U.S. National Library of Medicine (2013) Chapter 1: definition and classification of CKD. Kidney Int Suppl 3(2011):19–62
Brady TM, Schneider MF, Flynn JT, Cox C, Samuels J, Saland J, White CT, Furth S, Warady BA, Mitsnefes M (2012) Carotid intima-media thickness in children with CKD: results from the CKiD study. Clin J Am Soc Nephrol 7:1930–1937
Gerson AC, Wentz A, Abraham AG, Mendley SR, Hooper SR, Butler RW, Gipson DS, Lande MB, Shinnar S, Moxey-Mims MM, Warady BA, Furth SL (2010) Health-related quality of life of children with mild to moderate chronic kidney disease. Pediatrics 125:e349–e357
Hooper SR, Gerson AC, Butler RW, Gipson DS, Mendley SR, Lande MB, Shinnar S, Wentz A, Matheson M, Cox C, Furth SL, Warady BA (2011) Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin J Am Soc Nephrol 6:1824–1830
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2006) Progression of left ventricular hypertrophy in children with early chronic kidney disease: 2-year follow-up study. J Pediatr 149:671–675
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any conflicts of interest to declare.
Additional information
Answers
1, False; 2, c; 3, d; 4, a; 5, e
Rights and permissions
About this article
Cite this article
Sigurjonsdottir, V.K., Chaturvedi, S., Mammen, C. et al. Pediatric acute kidney injury and the subsequent risk for chronic kidney disease: is there cause for alarm?. Pediatr Nephrol 33, 2047–2055 (2018). https://doi.org/10.1007/s00467-017-3870-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3870-6