Abstract
Due to technological advances, an increasing number of infants and children are surviving with multi-organ system dysfunction, and some are reaching end-stage renal disease (ESRD). Many have quite limited life expectancies and may not be eligible for kidney transplantation but families request dialysis as alternative. In developed countries where resources are available there is often uncertainty by the medical team as to what should be done. After encountering several of these scenarios, we developed an ethical decision-making framework for the appropriate choice of conservative care or renal replacement therapy in infants and children with ESRD. The framework is a practical tool to help determine if the burdens of dialysis would outweigh the benefits for a particular patient and family. It is based on the four topics approach of medical considerations, quality-of-life determinants, patient and family preferences and contextual features tailored to pediatric ESRD. In this article we discuss the basis of the criteria, provide a practical framework to guide these difficult conversations, and illustrate use of the framework with a case example. While further research is needed, through this approach we hope to reduce the moral distress of care providers and staff as well as potential conflict with the family in these complex decision-making situations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
End-stage renal disease (ESRD) in children is not common, with an incidence of about 10 per million pediatric population [1, 2]. In the vast majority of children with ESRD, the decision to proceed to renal replacement therapy (RRT), which may include dialysis and/or renal transplantation, is an obvious “yes” as these modalities are essential to sustain life. Each transplant center has its own transplant eligibility criteria for inclusion in its renal transplant program—with very few exceptions [3]. At the present time there are an increasing number of children in nephrology programs who survive with multiple organ impairments, but with a limited life expectancy, and are reaching ESRD or chronic kidney disease stage 5 (CKD5) [4, 5]. It is important to evaluate the potential harms and benefits of RRT for such patients as it is a physician’s primary obligation to first do no harm. When a child is not a candidate for renal transplantation, we ought to ask whether dialysis should be offered as it has the potential to prolong dying rather than prolonging the child’s quality of life.
The Renal Physicians Association (RPA) developed clinical practice guidelines for the appropriate initiation and withdrawal of dialysis that were updated in 2010. The second edition includes a pediatric section with nine recommendations for family-centered shared decision-making (Table 1) [6]. One of the recommendations is to fully inform patients and families about the prognosis and treatment options. The adult section of the document includes a toolkit that can assist physicians to make individual patient assessments and predictions on prognosis. However, there are no prognostic scoring systems available for the pediatric patient, and much of the debate and difficulty pediatricians experience relates to the uncertainty of a child’s prognosis [4, 6, 7]. The RPA guidelines make clear that it is appropriate to not initiate or to withdraw dialysis in children if the dialysis is harmful, is of no benefit, or prolongs the dying process [6]. They also provide examples, including an infant with multi-organ dysfunction or renal failure secondary to a primary condition that is terminal or children with profound irreversible neurologic impairment. In theory, these situations seem obvious, but the practical assessment of patients to determine which conditions are terminal and when the burdens outweigh the benefits is not so clear. There is therefore a great need for further practical guidance in pediatrics.
Here we provide an ethical decision-making framework for choice of conservative care or dialysis for infants and children with ESRD. It employs a four-topic approach developed by Jonsen and colleagues to aid healthcare providers in identifying, analyzing, and resolving ethical issues in clinical medicine [8]. Each topic, i.e., medical issues, quality-of-life determinants, contextual factors, and patient/family preferences/goals, is used to organize facts around a particular case. Relevant principles, such as respect for autonomy, beneficence, non-maleficence, and justice, arise in the discussion of these four topics. The aim of the framework is to help healthcare providers and families work through difficult situations systematically in order to ultimately reach treatment decisions that reflect the best balance of outcomes and values for each particular patient.
The four-topic approach has been used by physicians in assessing ethical issues concerning the treatment of adults with ESRD and serves as the foundation for the RPA guidelines [6, 9, 10]. However, while respect for patient autonomy is prioritized in healthcare decisions for adults, “the contemporary test in pediatrics for whether an intervention is ethically appropriate is the best-interest standard—a weighing of expected burdens and benefits of that intervention for a particular child” [11]. Thus, we have tailored this approach to facilitate decision-making in the pediatric context and changed the order of the topics to assess quality of life and contextual features prior to family preferences. This is done to first address factors contributing to the child’s best interest and the underlying principles of beneficence and non-maleficence. This does not mean that family preferences/goals, however, are any less important. They deserve equal attention. In addition, we have expanded family preferences/goals to address relational considerations, which are critical to determining the best interests of children and their families.
We present a case example to facilitate the following discussion of the ethical decision-making framework. It is based on a case our nephrology team managed in clinical practice. The family has given permission to include their child’s story in this report.
A 2-year-old boy with a rare mitochondrial disease and known CKD had progression of his renal failure following 1 year with multiple illnesses. He was known to the renal service since a few months of age when he presented with severe hypertension, anemia, and a tubulopathy. His comorbidities included global developmental delay, seizure disorder, sensorineural hearing loss, mild cardiomyopathy, and severe gastrointestinal dysmotility with vomiting despite continuous feeds. The renal and biochemical diseases teams met to discuss prognosis in mitochondrial disorders and assessment for renal transplantation in children with significant life-limiting conditions. The teams reached consensus that should his medical condition and quality of life not show any significant improvement, then he would not be considered as a renal transplant candidate when his kidney disease deteriorated. A similar discussion was had with the family by the primary Nephrologist on behalf of the renal team. However, as the need for renal replacement was not imminent, no changes were made to the active nephrology care. Following a series of hospital admissions for recurrent pancreatitis that was associated with significant pain and acute on chronic kidney injury, the child’s family asked for a meeting with a specific question in mind. Given his progressive mitochondrial disease and limited life expectancy, would we offer their son dialysis when his kidneys fail?
The ethical decision-making framework
Medical aspects
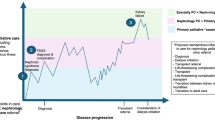
Physicians are generally most comfortable speaking about medical issues, although when it comes to a discussion of medical indications for choosing conservative care, many may not feel equally as confident in leading these conversations. Dialysis is an invasive treatment with the potential for the patient to develop undesirable symptoms and serious complications. It may also be a significant burden to the family. Yet it has the potential to provide symptom relief if the child is experiencing distress from edema or electrolyte abnormalities. Temporary dialysis may also allow for a short-term goal to be achieved, such as attending an important family event or reuniting with distant relatives. So then, how does a physician determine the potential benefits and harms of dialysis in an individual patient? The aim of medical aspects of the framework (Fig. 1) is to determine whether dialysis is technically feasible, as well as to assess the patient’s comorbidities to help with the prognosis and risk for undesirable symptoms and complications. In working through the framework questions with the family, not only will the physician gain information for their assessment, but the family will also become more aware of the technical issues of dialysis and the burdens and risks.
The technical assessment of patient suitability for dialysis will depend on the capabilities and resources at each individual medical center. When peritoneal dialysis (PD) is being considered, aspects such as the child’s size/weight, surgical incisions or stomas, abdominal wall defects, previous abdominal surgeries and intra-abdominal adhesions need to be assessed [12]. Size or weight is frequently a consideration in infants. There is a lower limit for size that will be determined by the smallest PD catheter available, the skill of the physician responsible for insertion of the catheter, the chance of catheter leak—which is higher in newborns—and the chance of survival even if the catheter does work. If hemodialysis is under consideration, technical aspects, such as size, blood pressure, medical stability, and vascular access possibilities, need to be evaluated. Again, each institution is likely to have a lower limit on size that it feels allows safe dialysis based on the smallest dialyzer and blood lines available. It is also important that families are aware that most infants and children need multiple dialysis catheter replacements, revisions, or repairs. A recent study of dialysis catheter longevity in children aged <2 years found that 22 patients required 90 catheters to maintain dialysis access [13]. Another study found that infants needed an average of five catheter-related procedures per patient [14].
If it is determined that it is technically possible to perform dialysis, then a careful review of other organ system impairment may help determine if the potential harms of dialysis are higher compared to a child with isolated kidney disease in ESRD. Non-renal comorbidities may affect prognosis or quality of life on dialysis. They may also increase the risk of complications or undesirable symptoms. In a recent analysis by the International Pediatric Peritoneal Dialysis Network of 1,830 children on chronic PD, one-third of children had at least one comorbidity [15]. The most common impairments were cognitive, motor, ocular, or auditory. Hospitalizations were more common and survival was lower when comorbidities were present.
The only specific medical situation clearly identified in the RPA guidelines as appropriate for non-initiation or discontinuation of dialysis is the presence of profound irreversible neurologic impairment [6]. If the patient does not demonstrate evidence of awareness, purposeful behavior, thought, and sensation, then dialysis should not be initiated. This can be challenging to assess, particularly in non-verbal children and in infants; accordingly, evaluation by a neurology consultant may be necessary. Pediatric nephrologists, when interviewed regarding this issue, indicated that the neurologic impairment needed to be severe enough to compromise the establishment of relationships [16]. Several studies of select patients with intellectual disability and reliable caregivers have shown equivalent dialysis and transplant outcomes to controls although possibly lower patient survival [17–20]. Intellectual disability alone is no longer considered an appropriate contraindication to RRT.
One of the most common causes of morbidity and mortality in children with ESRD is cardiovascular disease [21]. Chavers and colleagues reviewed the U.S. Renal Data System (USRDS) database of incident pediatric dialysis patients for cardiac complications and found that 31 % of all patients developed a cardiac-related event and that 38 % of all deaths were cardiac related [22]. Parekh and colleagues determined that children with ESRD have a 1,000-fold higher cardiac death rate compared to the general pediatric population [23]. Children with an uncorrected structural heart defect may not tolerate dialysis depending on cardiac disease severity [24, 25]. It is important to consider whether there is a structural and/or functional cardiac abnormality that significantly reduces the child’s life expectancy or which could be adversely affected by changes in intravascular fluid status or fluid volume shifts.
The function of the respiratory system should be assessed to help determine the child’s tolerance to PD and chance of survival. The most obvious example is a newborn with autosomal recessive polycystic kidney disease and pulmonary hypoplasia where mortality may be so high that conservative care is recommended at birth [7]. In a review of the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) database, Wood et al. found pulmonary disease or hypoplasia to be the only significant non-renal comorbidity for increased mortality in young children [26]. The increased risk may be related to intolerance of intravascular volume, likelihood of infection, or reduced pulmonary function and/or increased risk of aspiration with the increased intra-abdominal pressure during PD.
While unlikely to be a sole indication for dialysis non-initiation, gastrointestinal issues are common in children on dialysis, and pre-existing dysfunction may be exaggerated, leading to an increase in undesirable symptoms. Poor nutrition, as reflected by low serum albumin, is associated with an increased risk of mortality in children on dialysis [27–29]. In young children, up to 30 % of feeds may be lost to vomiting, and use of prokinetic medications may be needed although if gastrointestinal dysfunction is severe, children may need additional surgery for fundoplication and gastrostomy tube insertion [7, 30].
Infants, especially neonates, need special consideration when assessing suitability for dialysis. Infants with ESRD need to achieve a minimum size to be eligible for renal transplantation, and in most centers they require months or years to reach that size. If they are unlikely to survive to reach that goal, then conservative care should be chosen. Based on dialysis registries, children starting dialysis at less than 1 year of age have a poorer survival rate than older children, although the 1-year survival rate of around 90 % for the former patient group would seem to be acceptable [21, 31]. The major limitation of registry data is that infants have to survive long enough to be registered in the database. Those patients not offered RRT due to severe disease or parental wishes are not included and deaths may only be included if the child died while on dialysis, not if families chose to withdraw. Fauriel and colleagues found that a decision to withhold or withdraw life-sustaining therapy occurred in 11.5 % of all children who reached ESRD, of whom more than half were infants [16]. The majority of the decisions were made during the initial hospitalization period at birth with the infants never being discharged home. Studies that have included all infants ever started on dialysis show an overall mortality of around 50 %, with 38–48 % mortality in the first year [32–34]. Young children on PD experience more complications, including catheter leaks, hernias, peritonitis, growth failure, gastrostomy tube feeding, hypotension, developmental delay, and increased hospitalization [31, 32, 34, 35]. Mortality is most commonly due to cardiopulmonary failure, infection, or withdrawal of dialysis, and occurs more commonly in infants with non-renal comorbidities [21, 26, 31–33, 35]. Families of infants with ESRD making decisions about initiation of dialysis or conservative care must be informed of the outcomes and risks.
Quality of life
Determinations of best interest rely on assessment of present and projected future quality of life and burdens for the child and family caused by treatment. The aim of all medical interventions, including dialysis or conservative treatment, is to restore, maintain, or improve the patient’s quality of life [9]. There is general consensus that determinations of burdens and quality of life are subjective and involve value judgments [3]. Moreover, evaluation becomes particularly difficult when the interests of neonates and young children are being considered. Not only can they not speak for themselves, but it is impossible to project with any kind of certainty what kind of lives they would want for themselves.
Thus, parents are faced with making decisions based largely on their roles as protectors and providers. Burdens may be accepted with the hope not only of survival, but that the child will improve and that the intervention being considered will be the last intervention ever needed. Without experience, it is very difficult for parents to comprehend (even though informed) that their child’s life will be subject to ongoing medical interventions: there is always the hope that this intervention, this medical setback, will be the last one.
Because quality-of-life discussions can veer into the abstract, there is a great need to translate these discussions into practical concepts for patients and families. The questions which are posed to the parents are meant to generate discussion with the aim of encouraging the parents to think about the benefits and burdens of treatment in relation to their unique child’s life (Fig. 1). Not all of the questions will be applicable to every situation but are to be used at the nephrologist’s discretion. For example, “What activities give your child pleasure and/or happiness” will be more relevant to discussions concerning older children than young babies.
Contextual/ social factors
The nephrologists’ duty is to act in the best interests of the patient. In the case of a newborn or child with ESRD, this duty requires that the medical team consider the role context plays in the decision that is being made. Managing dialysis has profound and pervasive effects on family and caregivers, as well as on the child. Accordingly, family relationships and cultural, socio-economic, and religious factors should be attended to when helping families make decisions about conservative treatment or dialysis (Fig. 1). It is important that family members have access to information in a way that they can understand and give sufficient weight to the consequences that would flow from their decisions. While dialysis is clearly expensive, decisions to offer or withhold treatment should not be made on the basis of cost or resource allocation issues at the bedside [36]. Also, it is important that providers recognize that they too are part of the decision-making context and reflect on how their own personal assumptions, biases, and potential conflicts of interest (e.g., research) can shape the kind of information provided and how it is provided to families.
Patient/ family preferences
Considered the best judges of their child’s interests, parents are given the authority for making medical decisions for their children. Yet, choices regarding RRT in neonates and children are both medically and emotionally complex. Parents are struggling with the reality that their child has a serious life-threatening condition. Most parents feel it is their responsibility to advocate for “everything” to be done in hopes of prolonging their child’s life. Many experience loss, confusion, or anxiety in the face of such decisions. The thought of the death of one’s child can be paralyzing.
Ideally, decisions regarding conservative therapy or dialysis should be made by consensus between parents and the healthcare team. We recommend that nephrologists take a goal-orientated approach: framing discussions first in relation to parent’s goals and hopes for their child’s care, and then discussing treatment options, risks, and benefits of intervention or significant barriers to RRT within the context of these goals (Fig. 1). This approach will require lengthy discussion, willingness for respectful argument, and recognition that at times clear direction may be needed from the healthcare team. Indeed, in attempting to respect parental authority and choice, it is important to consider whether we ask parents to make decisions that are imponderable for them to consider, such as allowing their child to die. Clark and Dudzinksi emphasize this point in relation to seeking parental consent for Do Not Attempt Resuscitation (DNAR) orders, regardless of the prognosis or likely efficacy of cardiopulmonary resuscitation (CPR) [37]. They maintain that in requesting consent for DNAR, we fail to appreciate the special bond of the parent–child relationship and the emotional and moral difficulties of asking parents to withhold CPR from their children. “Seeking parental consent for DNAR implies that attempting CPR has potential clinical benefit that parents choose to forgo and enlists parents to determine whether CPR is good for their child. When parents of dying children consent to attempt CPR, they take on the moral responsibility for choosing a non-therapeutic intervention, thus creating a potential burden for them. This burden is unfair and insensitive to the profound suffering and loss parents of dying children experience and potentially results in attempting futile CPR…” [38].
The same could be said about withholding any life-saving treatment, including dialysis. In some situations there is agreement among the healthcare team that dialysis is not medically indicated because the disease or condition is so severe that the child’s life is unlikely to improve with dialysis. Examples include the child with an uncorrected congenital heart defect who is not a candidate for cardiac surgery due to poor health, or the infant with significant pulmonary hypoplasia who is ventilator dependent. In these situations we recommend, as do Clark and Dudzinski [38], that the healthcare providers take primary responsibility for making the decision to pursue conservative treatment [38].
Some ethicists might argue that this approach does not show respect for parental autonomy. We would argue otherwise—respect for autonomy does not require that parent be presented with options that are medically futile. Further, allowing physicians to take responsibility for decisions based on medical knowledge shows greater compassion for the suffering and vulnerability of parents faced with the potential loss of their child [38]. We are not referring to cases or situations where there is genuine uncertainty about the appropriateness of pursuing RRT either on a trial or long-term basis. Nor do we suggest that the parents are excluded from the decision-making process, but rather “respectfully include parents in these conversations through informed assent, honoring the special relationships and obligations parents have with their dying children” [38].
Discussion
There is a movement to replace the terminology of withdrawal or withholding of dialysis with the choosing of conservative care [39]. Withdrawal and withholding have a negative connotation and imply that patients are being disadvantaged by not being provided this therapy, whereas choosing conservative care is a positive act that puts the conservative care option on the same level as choosing dialysis or transplantation. In fact, conservative care usually includes providing all necessary pediatric and nephrology care and support along with palliative symptom management even though dialysis is not provided. While there are no pediatric data at present, in elderly populations and adults with multiple comorbidities, dialysis does not actually confer a survival advantage over conservative care [40]. Death used to be more recognized as part of the cycle of life but now it is often taken to represent the “defeat of technological medicine” [41]. It has been eloquently stated by Shooter and Watson in a discussion of withholding dialysis in infants that “where the quality of a baby’s life is poor, the quality of its death may be more important” [5].
A recent review on the ethics of infant dialysis by Lantos and Warady raised some important questions including “how high must the burden of dialysis, or any therapy, be in order for that burden to outweigh the life-saving benefits of the therapy” and “how, exactly, do clinicians explain the burdens that are associated with dialysis when they are seeking the family’s informed consent to such treatment” [42]. We would suggest that there is no predefined or a priori definition of burden that is too much, but that working through the ethical decision-making framework will help to determine the threshold for that individual patient and family. In addition, while discussing the questions in our decision-making tool, parents will become informed of the issues when considering dialysis therapy. Recent recommendations by the European Paediatric Dialysis Working Group also suggest that discussion with the family of infants with ESRD should address short- and long-term prognosis, including the influence of co-morbidities, medical care issues such as equipment, expertise and resources, as well as the predicted quality of life for the infant [4].
It is our hope that this ethical decision-making framework will assist teams and families reach consensus through improved communication and lessen the potential for disputes. However, there may also be times when the family and team cannot reach consensus and the family wishes to pursue dialysis even though there is a strong recommendation for conservative treatment from the medical team. This does not mean that it is acceptable to override the parent(s)’s wishes. If the family does not agree with the team, then further discussion is needed or perhaps a trial of therapy until consensus can be reached. An ethicist or clinical ethics committee can support and guide the decision-making process. It may also be prudent to involve other professionals in psychology, spiritual care, or palliative care. As Goldberg and colleagues suggest, in evaluating candidacy for kidney transplantation, emphasis should be placed on the balance of benefits and burdens to the child, not on the perceived value of the child’s life [3]. However, if the pediatric nephrologist and treating team believe that treatment will do harm and cause the child to suffer without benefit, their primary ethical obligation is to act in the best interest of the child. If a dispute is intractable and no consensus can be reached, it is the duty of the nephrologist to seek a second opinion, and as a last resort, pursue legal input.
Case example
We now return to our case example to illustrate how using this ethical decision-making framework assisted both the medical team and the family reach the same conclusion based on the child’s best interest.
In following the framework, the Nephrologist reviewed with the family the medical aspects which included an underlying progressive mitochondrial disease with developmental delay, seizures, hearing loss, and severe gastrointestinal dysmotility. The child had CKD4 when last assessed by nuclear medicine scan, but had further deterioration following recurrent pancreatitis episodes. His biochemical disease physicians advised that the additional complications indicated progression of his mitochondrial disease with an unknown but limited life expectancy. When discussing the child’s quality of life his mother said that he got enjoyment from his jolly jumper and special toys, and would have “belly laughs” when pleased. He seemed most distressed when he was nauseated or vomiting and during pancreatitis episodes, all of which were occurring more frequently. In the last year, he had spent 8 months in hospital and had regressed after each admission. His mother described a good quality of life for him as spending time at home with his family and no nausea or vomiting. His mother was a bright, loving, competent single parent with other children, trying to complete nursing school. She had a partner and extended family support as well as respite nurses but still felt stress. Initially, the mother expressed hope that her son’s metabolic and renal diseases would not progress and that he would be a candidate for renal transplantation. However, later she admitted that she did not believe her son would have many more birthdays. The mother asked that his medical teams act in his best interest, providing adequate care when he was unwell but to not pursue invasive treatments if he had little chance of recovery. No decisions were made at this point so that both parties could contemplate what the other had said.
The multidisciplinary care renal team and biochemical disease physicians then met to discuss the medical changes, prognosis, and if dialysis would fit into the family’s expectations and goals for improved quality of life. A hospital ethicist was present at the discussion as well, not because of perceived conflict, but as a regular participant in the multidisciplinary care meetings. The renal team and biochemical disease physicians reached consensus that conservative care, rather than dialysis, was in the best interest of the child. The following day the treating Nephrologist went to meet with the mother and was greeted at the doorway. However, before the Nephrologist could report on the outcome of the teams’ discussion, the mother said “I would like to meet with the palliative care team next week, can you join us for the meeting?” Allowing the parent to talk about her hopes and concerns while providing information about the future projection for her child helped her to come to the same conclusion as the medical team and move forward in revising the goals of care for her child.
The family and primary physicians met with the pediatric palliative care team the following week. The palliative team liaised with community supports, assisted with ambulance transport and resuscitation orders, and provided symptom management, respite, and family support. Renal medications were continued, but nutritional calories and fluid volumes were reduced to aim for gastrointestinal tolerance rather than optimal growth and hydration. Laboratory monitoring tests and clinic visits were at the discretion of the family and continued on a 3-monthly basis. These modifications for the child resulted in an almost 1 year period with more time spent at home with family with fewer undesirable symptoms before his mitochondrial disease progressed.
Conclusions
In this article, we offer an ethical decision-making framework for choices regarding conservative care or dialysis for infants and children with ESRD. The framework can guide the renal team and family to discuss the important medical issues, quality-of-life determinants, contextual factors, and patient and family preferences to assist in determining whether the potential benefits of dialysis would outweigh the burdens or harm. This framework is not meant to provide users with a yes/no answer but to highlight the questions and issues that need to be determined and discussed with the family in order to make an appropriate decision for each particular child. Although further research is needed, we hope this approach can reduce the moral distress of healthcare providers and potential conflicts between healthcare providers and the family which can further interfere with the already difficult decision-making process.
References
Van der Heijden B, van Dijk P, Verrier-Jones K, Jager K, Briggs J (2004) Renal replacement therapy in children: data from 12 registries in Europe. Pediatr Nephrol 19:213–221
Canadian Organ Replacement Register Annual Report (2014) Treatment of end-stage organ failure in Canada, 2003 to 2012. Canadian Institute for Health Information (CIHI), Toronto. Available at: www.cihi.ca/corr
Goldberg AM, Amaral S, Moudgil A (2014) Developing a framework for evaluating kidney transplantation candidacy in children with multiple comorbidities. Pediatr Nephrol. doi:10.1007/s00467-013-2704-4
Zurowska A, Fischbach M, Watson A, Edefonti A, Stefanidis C, European Paediatric Dialysis Working Group (2013) Clinical practice recommendations for the care of infants with stage 5 chronic kidney disease (CKD5). Pediatr Nephrol 28:1739–1748
Shooter M, Watson A (2000) The ethics of withholding and withdrawing dialysis therapy in infants. Pediatr Nephrol 14:347–351
Renal Physicians Association (RPA) (2010) Shared decision-making in the appropriate initiation of and withdrawal from dialysis: Clinical practice Guideline Recommendation Summary. Second edition. RPA, Rockville.Available at www.renalmd.org
Rees L (2008) Management of the neonate with chronic renal failure. Semin Fetal Neonatal Med 13:181–188
Jonsen A, Siegler M, Winslade W (2010) Clinical ethics: a practical approach to ethical decisions in clinical medicine, 7th edn. McGraw Hill, New York
Moss A (2011) Ethical principles and processes guiding dialysis decision-making. Clin J Am Soc Nephrol 6:2313–2317
Kodner IJ (2009) Surgeons and ethics: You bet! J Am Coll Surg 209:1–6
Diekema D, Botkin J (2009) Foregoing medically provided nutrition and hydration in children. Pediatrics 124:813–822
Schaefer F, Warady B (2011) Peritoneal dialysis in children with end-stage renal disease. Nat Rev Nephrol 7:659–669
Paul A, Fraser N, Manoharan S, Williams A, Shenoy M (2011) The challenge of maintaining dialysis lines in the under twos. J Pediatr Urol 7:48–51
Beanes S, Kling K, Fonkalsrud E, Torres M, Salusky I, Quinones-Baldrich W, Atkinson J (2000) Surgical aspects of dialysis in newborns and infants weighing less than ten kilograms. J Pediatr Surg 35:1543–1548
Neu A, Sander A, Borzych-Duzatka D, Watson A, Valles P, Ha I, Patel H, Askenazi D, Batasz-Chmielewska I, Lauronen J, Groothoff J, Feber J, Schaefer F, Warady B, on behalf of the IPPN investigators (2002) Comorbidities in chronic pediatric peritoneal dialysis patients: a report of the international pediatric peritoneal dialysis network. Perit Dial Int 32:410–418
Fauriel I, Moutel G, Moutard M, Montuclard L, Duchange N, Callies I, Francois I, Cochat P, Herve C (2004) Decisions concerning potentially life-sustaining treatments in paediatric nephrology: a multicentre study in french-speaking countries. Nephrol Dial Transplant 19:1252–1257
Benedetti E, Asolati M, Dunn T, Walczak D, Papp P, Bartholomew A, Smith Y, Washington A, Pollak R (1998) Kidney transplantation in recipients with mental retardation: clinical results in a single-center experience. Am J Kidney Dis 31:509–512
Martens M, Jones L, Reiss S (2006) Organ transplantation, organ donation and mental retardation. Pediatr Transplant 10:658–664
Galante N, Dib G, Medina-Pestana J (2010) Severe intellectual disability does not preclude renal transplantation. Nephrol Dial Transplant 25:2753–2757
Aksu N, Yavascan O, Anil M, Deniz Kara O, Bal A, Berna Anil A (2012) Chronic peritoneal dialysis in children with special needs or social disadvantage or both: contraindications are not always contraindications. Perit Dial Int 32:424–430
North American Pediatric Renal Trials and Collaborative Studies (2012) NAPRTCS 2011 annual dialysis report. Available at: www.naprtcs.org
Chavers B, Li S, Collins A, Herzog C (2002) Cardiovascular disease in pediatric chronic dialysis patients. Kidney Int 62:648–653
Parekh R, Carroll C, Wolfe R, Port F (2002) Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr 141:191–197
Laakkonen H, Holtta T, Lonnqvist T, Holmberg C, Ronnholm K (2008) Peritoneal dialysis in children under two years of age. Nephrol Dial Transplant 23:1747–1753
Rees L (2007) Long-term peritoneal dialysis in infants. Perit Dial Int 27:S180–S184
Wood EG, Hand M, Briscoe DM, Donaldson LA, Yiu V, Harley FL, Warady BA, Ellis EN, North American Pediatric Renal Transplant Cooperative Study (2001) Risk factors for mortality in infants and young children on dialysis. Am J Kidney Dis 37:573–579
Amaral S, Hwang W, Fivush B, Neu A, Frankenfield D, Furth S (2008) Serum albumin level and risk for mortality and hospitalization in adolscents on hemodialysis. Clin J Am Soc Nephrol 3:759–767
Wong CS, Hingorani S, Gillen DL, Sherrard DJ, Watkins SL, Brandt JR, Ball A, Stehman-Breen CO (2002) Hypoalbuminemia and risk of death in pediatric patients with end-stage renal disease. Kidney Int 61:630–637
Tsai H, Yang L, Chin T, Wang H, Liu C, Wei C, Chang J (2010) Outcome and risk factors for mortality in pediatric peritoneal dialysis. Perit Dial Int 30:233–239
Zaritsky J, Warady B (2011) Peritoneal dialysis in infants and young children. Semin Nephrol 31:213–224
Vidal E, Edefonti A, Murer L, Gianoglio B, Maringhini S, Pecoraro C, Sorino P, Leozappa G, Lavoratti G, Ratsch I, Chimenz R, Verrina E, Italian Registry of Paediatric Chronic Dialysis (2012) Peritoneal dialysis in infants: the experience of the Italian Registry of Paediatric Chronic Dialysis. Nephrol Dial Transplant 27:388–395
Hijazi R, Abitbol C, Chandar J, Seeherunvong W, Freundlich M, Zilleruelo G (2009) Twenty-five years of infant dialysis: a single center experience. J Pediatr 155:111–117
Feinstein S, Rinat C, Becker-Cohen R, Ben-Sahlom E, Schwartz S, Frishberg Y (2008) The outcome of chronic dialysis in infants and toddlers—advantages and drawbacks of haemodialysis. Nephrol Dial Transplant 23:1336–1345
Rheault M, Rajpal J, Chavers B, Nevins T (2009) Outcomes of infants <28 days old treated with peritoneal dialysis for end-stage renal failure. Pediatr Nephrol 24:2035–2039
Shroff R, Rees L, Trompeter R, Hutchinson C, Ledermann S (2006) Long-term outcome of chronic dialysis in children. Pediatr Nephrol 21:257–264
American Academy of Pediatrics Committee on Bioethics (1996) Ethics and the care of critically ill infants and children. Pediatrics 98:149–152
Clark J, Dudzinski D (2011) The false dichotomy: Do “everything” or give up. Am J Bioeth 11:26–27
Clark J, Dudzinski D (2013) The culture of dysthanasia: attempting CPR in terminally ill children. Pediatrics 131:572–580
Carson R (2012) Deny dialysis or “D-NI” dialysis? The case for “do not initiate; do not ignore” orders. Clin J Am Soc Nephrol 7:1924–1926
O’Connor N, Kumar P (2012) Conservative management of end-stage renal disease without dialysis: a systematic review. J Palliat Med 15:228–235
Rombola G (2002) Dialysis for everybody? At any cost? J Nephrol 15:S33–42
Lantos J, Warady B (2013) The evolving ethics of infant dialysis. Pediatr Nephrol 28:1043–1947
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dionne, J.M., d’Agincourt-Canning, L. Sustaining life or prolonging dying? Appropriate choice of conservative care for children in end-stage renal disease: an ethical framework. Pediatr Nephrol 30, 1761–1769 (2015). https://doi.org/10.1007/s00467-014-2977-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-014-2977-2