Abstract
Idiopathic nephrotic syndrome (INS) includes three different entities: minimal change disease (MCD), focal segmental glomerulosclerosis (FSGS), and mesangial proliferative glomerulonephritis. Historically, this condition has been attributed to a T-cell disorder resulting in the secretion of a circulating factor that increases glomerular permeability to plasma proteins. The therapeutic approach to control the proteinuria of INS remains the use of drugs that have been considered to suppress the production of the “circulating factor” secreted by T cells. Recently, rituximab (RTX), a chimeric monoclonal antibody directed against the CD20 cell surface receptor expressed on B cells, has emerged as potential therapeutic agent. The number of publications reporting clinical experience with RTX in the treatment of nephrotic syndrome has greatly increased in the last few years. However, there is currently no good evidence from clinical or experimental studies that support a role of RTX in the treatment of MCD and FSGS proteinuria. In summary, there is the need for a better understanding of the pathogenesis of the proteinuria in INS and the potential role of RTX in this condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
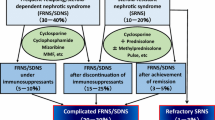
The entity idiopathic nephrotic syndrome (INS) includes patients with minimal change disease (MCD), focal segmental glomerulosclerosis (FSGS), and mesangial proliferative glomerulonephritis. Historically, this condition has been attributed to a T-cell disorder resulting in the secretion of a circulating factor that increases glomerular permeability to plasma proteins [1]. The therapeutic approach to control the proteinuria of INS remains the use of drugs that have been considered to suppress the production of the “circulating factor” secreted by T cells. Initial treatment usually consists of corticosteroids. INS is typically classified into steroid-dependent nephrotic syndrome (SDNS), frequently relapsing nephrotic syndrome (FRNS), and steroid-resistant nephrotic syndrome (SRNS).
While classically treatment of INS has involved treatment with agents that suppress T-cell function, such as corticosteroids and calcineurin inhibitors, rituximab (RTX) has recently emerged as potential therapeutic agent. RTX is a chimeric monoclonal antibody that is primarily aimed at deleting B cells by binding the CD20 cell surface receptor and inducing apoptosis [2]. A recent survey shows that the drug is commonly used worldwide to treat patients with INS [3]. In this paper we review the evidence or lack thereof on its potential efficacy and its mechanism of action for the treatment of this disorder.
RTX in idiopathic nephrotic syndrome
Since the first case report in 2004 [4], several studies on the effect of RTX in the treatment of INS have been published [3, 5–14]. These reports vary with respect to the characteristics of the patients included in the study and especially on the definition of steroid dependency. Some authors consider steroid dependency in a patient with relapse on prednisone after an initial episode of nephrotic syndrome [3, 5, 6], while others define steroid dependence if patients relapse at least two times while on prednisone [7–11]. For yet other authors, steroid dependency occurs if a patient relapses up to 2 weeks [3, 7–11] or within 4 weeks [5] after discontinuing prednisone. Neither Kamei et al. nor Guigonis et al. define steroid dependency in their studies [12, 13]. In terms of therapy, reports on the dose of RTX have varied from one to up to seven doses. Other immunosuppressive drugs were discontinued in some reports on RTX [8], whereas in other studies the patients continued with the same previous immunosuppressive regimen [3, 6, 7, 9–15].
We have classified these reports into three groups according to the strength of the obtained evidence classification developed by the U.S. Preventive Services Task Force (Tables 1–3) [15]. Of note, the stricter the study, the lower the successful response to the drug.
First level of evidence: descriptive studies
The weakest level of evidence is represented by descriptive studies. In the case of RTX, this includes single case reports or a cohort studies of patients from several centers whose information was collected via questionnaires. Two such studies using questionnaires have been published (Table 1) [3, 7].
The Ito et al. study included 74 Japanese children from 14 centers [7], of whom 80 % had MCD and only 25 % were SR. Of importance is that 40 of their patients continued the same immunosuppressive therapy and that all SD/SFR patients were treated during remission. The aim of this study was to determine if RTX prevented relapse rather than to treat relapse.
In the Ito et al. study, a complete remission (CR) (6 patients) and partial remission (PR) (6 patients) were achieved in 68 % of the SR patients after 1–12 months, with CR or PR occurring a mean of 6 months after the initiation of RTX treatment. This late time of response raises questions as to the role of RTX in inducing remission, especially for those who improved 6 months after RTX had been given. Furthermore, 28 of 55 patients relapsed, but those subjects who continued treatment with other immunosuppressive therapy were much more likely to be relapse free (60 %) than those who stopped all immunosuppressive therapy (relapse-free survival was <20 %). Thus, it would appear that the remission rate may have been related more to the continued use of immunosuppressive therapy than to the RTX itself.
Prytula et al. mailed questionnaires to nephrologists who were members of the International Pediatric Nephrology Association [3]. Seventy patients from 25 centers from all regions of the world were included, of whom 51 % had SDNS or FRNS and 49 % had SRNS. Fifteen patients had post-transplant recurrence of NS. In this last group, all patients were SR. Of the SR and SD/FR nephrotic patients in this study, 44 and 82 %, respectively were considered to have had a response to RTX; but again no data were available as to the timing of response.
Retrospective questionnaires have many inherent weaknesses, such as no comparison group, no blinding, potential of poor recall, and publication bias. In addition, the cases of eight of the patients included in the Prytula et al. database had previously been presented at national and/or international conferences as case-studies and included in previously published case reports [3]. If the current research was influenced directly or indirectly from promising earlier reports, then it is highly questionable to use the same data to “further assess the efficacy and safety of RTX in refractory NS.”
A more important issue which applies to these types of multicenter, retrospective studies included in this group (Table 1) and in the next group to be reviewed (Table 2) is the lack of standardization regarding prednisone therapeutic regimens and the limited amount of information given on concomitant medications with no analysis of how results depended on these factors. Finally, as previously mentioned, the timing of response after RTX is also often poorly documented.
Second level of evidence: cohort studies
Second level of evidence is represented by prospective and retrospective studies that include cohorts of patients from different centers (Table 2). A main characteristic in this type of study is an attempt, not always successful, to standardize the response to corticosteroids prior to RTX therapy. The number of patients and their response to corticosteroids, the underlying glomerular pathology, whether they were treated during relapse or remission, and concomitant immunosuppressive therapy varies according to the study (Table 2).
Retrospective studies
Gulati et al. [8] included both SDNS and SRNS patients in their study whereas Kemper et al. [9] and Tellier et al. [5] treated only SDNS. Therapy with other immunosuppressive agents was continued by Gulati et al.[8] and Tellier et al. [5], whereas in the Kemper et al. [9] study, most of the patients received only RTX. In all of these studies SDNS patients were treated with RTX during remission. Gulati et al. included patients with MCD, FSGS and some with unknown pathological findings. In the Kemper et al. [9] study there is no mention of renal pathology. Tellier et al. [5] included 15 MCD patients and two FSGS patients. Of note, eight of the 18 patients in the Tellier et al. study had some degree of renal failure. Gulati et al. concluded that “RTX was safe and effective in inducing and maintaining remission in a ‘significant’ proportion of patients with difficult SRNS and SDNS”, whereas the Kemper et al. [9] study reported that 69 % remained in long-term remission and 48 % off immunosuppressant but that 16 patients received more than one course of RTX (four courses in 9 patients). In contrast, in the Tellier study other immunosuppressive agents were tapered in all patients, and 14 of 18 subjects remained on at least one immunosuppressive drug 2 years after initiating RTX therapy.
These studies all have similar problems that are associated with a cohort retrospective study. The selection of patients and concomitant therapy are difficult to follow. The selection of patients in the Gulati et al. [8] study included patients in the SRNS group with quite different ages at onset and age when RTX therapy was administered. While in the Methods section of the report it is stated that all other IS agents were withdrawn except in two patients who received mycophenolate mofetil, in the Results section it is noted that one or more IS medications were withdrawn in only 12 patients. Therefore, it remains unclear if the response was due to the natural history of the disease, the presence of the concomitant medications, and/or the effect of RTX.
Prospective studies
There are four prospective studies on RTX [6, 10, 12, 13]. In these studies, most of the patients had SDNS (72 of 74 total cases) and MCD (43 of 47 total cases). As previously mentioned, there is no uniformity in the definition of steroid dependency. In each series, the numbers are small. All SDNS patients received RTX during remission and continued on “maintenance immunosuppression.” Drug efficacy was assessed by maintaining remission after withdrawal of the “maintenance immunosuppression” [13]. The latter was accomplished after variable periods of time or not at all. As shown in Table 2, the relapse rate in these patients during the follow-up was quite variable.
Third line of evidence: randomized control studies
The third line of evidence has been obtained from prospective, randomized control studies (Table 3). Two studies have been published, both from the same Italian study group, involving SDNS (first study) [11] and SRNS (second study) [14].
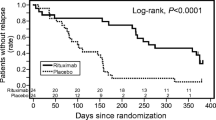
Steroid-dependent nephrotic syndrome
Ravani et al. [11] hypothesized that RTX and lower doses of prednisone and calcineurin inhibitors (PCI) were non-inferior to standard doses of corticosteroids in SDNS. The study includes ten and six (FSGS and MCD) patients in the control group and seven and 13 (FSGS and MCD) patients in the RTX group. No renal biopsy results were available for 11 of the control and seven of the RTX-treated patients. Patients were evenly split (27/27). Only SD patients were included, but subjects dependent on high-dose prednisone (0.7 mg/kg/day) were excluded. The efficacy of RTX was assessed by the percentage change in daily proteinuria at 3 months in RTX children versus “standard” therapy. The aim was to prove that the proteinuria geometric mean for the RTX group was less than threefold the geometric mean for the PCI group and by their relapse rate.
There are problems with the study. It is unclear if the power analysis is based on a non-inferiority-based model. Although the authors used stratified samples, they do not state what the sample sizes are for the four groups included in the study, namely, RTX/in patients showing steroid toxicity, RTX/in patients not showing steroid toxicity, PCI/in patients showing steroid toxicity, and PCI/in patients not showing steroid toxicity. The authors stated that RTX (375 mg/m2) was given once or twice depending on the degree of steroid toxicity. Therefore, there were two different dosing levels in the intervention group. Missing values at 3 months in those completing the study are replaced with the last available value. It is also unclear how many of the subjects with SDNS were in relapse and how many were in remission at the time of the randomization. It is evident from the Results section that some patients in both groups had massive proteinuria at the initiation of the trial, but the proteinuria results (g/day) are presented using a logarithmic scale that does not allow the reader to compare and evaluate data at the individual level. Finally, by switching 16 of the controls to the RTX group at 3 months, the authors nullified any analysis of comparative effects between the control and RTX group after 3 months.
At 3 months, the relapse rate was 18.5 % in the RTX group and 52 % in the control group. At 6 months the relapse rate in the RTX group was 50 % and at the end of 12 months it was 75 %. Of the 16 patients of the control group that received RTX after 3 months, 11 (69 %) continued relapsing despite the use of RTX. Overall, given the difficulties of interpreting the data, the gaps regarding patients’ description, the non-inferiority nature of the study, the exclusion of those patients with more severe steroid dependency, and the high relapse rate at the end of the 1 year of follow-up, it is difficult to suggest the use of RTX in SDNS patients instead of conventional therapy.
Steroid-resistant nephrotic syndrome
Magnasco et al. [14] reported an open-label, randomized, controlled trial for RTX in SRNS. All children continued prednisone and PCI at the dose prescribed before enrollment. Two doses of RTX were given to the RTX group. The study included 31 subjects (19 FSGS, 7 MCD, and 5 not determined). As in the study of Ravani et al. [11], patients were followed for 3 months. The results were rather disappointing. RTX did not did not reduce proteinuria at 3 months. The authors concluded that their data do not support the addition of RTX to a therapeutic regimen of prednisone and PCI in children with resistant INS to induce remission.
Mechanism of action
If we assume that there is a circulating factor released by T cells in INS patients, then how would a treatment that works on B cells influence the release of cytokines by the T cell?
A major problem with this approach is the fact that despite numerous efforts in the last 30 years, there is as yet no strong evidence supporting the existence of a circulating factor released by lymphocytes in MCD [16]. The case for a circulating factor is stronger in patients with FSGS. The sudden massive proteinuria immediately after transplant [17], the improvement or resolution of the proteinuria after plasmapheresis [18], and the description of serum soluble urokinase receptor (suPAR) as the pathogenic factor for proteinuria [19] support the circulating factor hypothesis for the increased glomerular permeability to plasma proteins in these patients. However, it is interesting to observe that FSGS patients, in whom the evidence for circulating factor is stronger, are found to be the least responsive to RTX therapy in the quoted studies in this review and in the work by Vicenti et al. [20]
Role of B cells on T-cell activation and regulation
There are theoretical ways that B cells could impact T-cell activation or regulation. These include (1) cytokine secretion and (2) expression of surface molecules which may provide costimulatory signals by direct B–T cell contact. B cells are known to secrete interleukin-10 (IL-10), transforming growth factor-beta (TGF-beta) (known T-regulatory cell inhibitors), tumor necrosis factor-alpha, and IL-6, a known stimulator of Th17 cell proliferation. B-cell failure to produce IL-10 and TGF-beta could lead to inhibition of T-regulatory cell function that might allow for T-cell activation [21]. Indeed, we have observed a decrease in T-regulatory cell function in MCD patients in relapse [22].
B cells also express CD80/86, MHCH, CD40, and OX40L on their cell surface. These molecules can interact with complementary molecules on the surface of the T cell, including CD28, peptide:TCR, CD40L, and OX40, respectively resulting in enhancement (CD28, CD40L, peptide:TCR) or inhibition ( OX40L) of the T-cell response [21].
B-cell function in nephrotic syndrome
Only a few studies have addressed B-cell function in nephrotic syndrome. Kemper et al. observed increased levels of both sCD23 (a marker of B-cell activation) and sCD25 (a marker of T-cell activation) during relapses of SDNS [23]. Cho et al. also found a significantly higher expression of CD23 in freshly isolated B cells from patients with active MCD [24]. These findings have been presented as evidence of an important role for B cells in the development of nephrotic syndrome. Unfortunately, they only show that B cells are activated but provide no clue if the activation induces T-cell activation to release pathogenic cytokines. It is thus not known if this represents a response to the nephrotic state, a response to concomitant infections (such as respiratory tract infection) that commonly occur in nephrotic syndrome, or whether it has a true pathogenetic role in the disease process. In summary, there is no compelling evidence in INS that the RTX effect on B cells results in the inhibition in the release by T cell of the putative circulating factor.
Could RTX be directly affecting the podocyte?
Proteinuria in MCD and FSGS is currently considered the result of a podocyte defect [25]. Indeed, several immunosuppressive agents have been shown to have direct effects on podocytes in addition to their effect on the immune system. These agents include prednisone and calcineurin agents [26, 27].
Fornoni et al. [28] recently reported that RTX also binds to human podocytes. Of special interest is that this binding is not due to the presence of CD20 receptors because cultured differentiated human podocytes do not express CD20. The binding is the result of cross-reactivity of RTX with sphingomyelin phosphodiesterase acid-like 3b (SMPDL-3b) protein. Furthermore, according to these authors, RTX regulates the activity of acid sphingomyelinase (ASMase) in raft microdomains. They postulate that RTX preserves the podocyte sphingolipid-related enzymes and thereby prevents actin cytoskeleton remodeling in these cells and subsequent proteinuria.
This evidence supports a potential direct effect of RTX on SMPDL-3b protein but does not explain the role of suPAR in FSGS nor the poor response to RTX observed in the majority of FSGS patients. In addition, Niemann–Pick disease, which is characterized by a lack of ASMase activity, presents with a glomerulopathy, but the lesion is not associated with nephrotic syndrome nor does it resemble FSGS [29]. Therefore, although there are theoretical explanations for how RTX could affect both T cells and podocytes, the direct evidence that it may block proteinuria in MCD or FSGS patients via these pathways is weak.
In summary, there is currently no good evidence from clinical or experimental studies that RTX plays a role in the treatment of MCD and FSGS proteinuria. There is a need for a better understanding of the pathogenesis of the proteinuria in these diseases and the potential role of RTX. Better performed and well-defined randomized control studies of RTX should be conducted before the use of this therapy can be recommended.
References
Shalhoub RJ (1974) Pathogenesis of lipoid nephrosis: a disorder of T-cell function. Lancet 2:556–560
Maloney DG, Smith B, Rose A (2002) Rituximab: mechanism of action and resistance. Semin Oncol 29[Suppl 2]:2–9
Prytuła A, Iijima K, Kamei K, Geary D, Gottlich E, Majeed A, Taylor M, Marks SD, Tuchman S, Camilla R, Ognjanovic M, Filler G, Smith G, Tullus K (2010) Rituximab in refractory nephrotic syndrome. Pediatr Nephrol 25:461–468
Benz K, Dotsch J, Rascher W, Stachel D (2004) Change of the course of steroid-dependent nephrotic syndrome after rituximab therapy. Pediatr Nephrol 19:794–797
Tellier S, Brochard K, Garnier A, Bandin F, Llanas B, Guigonis V, Cailliez M, Pietrement C, Dunand O, Nathanson S, Bertholet-Thomas A, Ichay L, Decramer S (2013) Long-term outcome of children treated with rituximab for idiopathic nephrotic syndrome. Pediatr Nephrol 28:911–918
Sellier-Leclerc AL, Baudouin V, Kwon T, Macher MA, Guérin V, Lapillonne H, Deschênes G, Ulinski T (2012) Rituximab in steroid-dependent idiopathic nephrotic syndrome in childhood–follow-up after CD19 recovery. Nephrol Dial Transplant 27:1083–1089
Ito S, Kamei K, Ogura M, Udagawa T, Fujinaga S, Saito M, Sako M, Iijima K (2013) Survey of rituximab treatment for childhood-onset refractory nephrotic syndrome. Pediatr Nephrol 28:257–264
Gulati A, Sinha A, Jordan SC, Hari P, Dinda AK, Sharma S, Srivastava RN, Moudgil A, Bagga A (2010) Efficacy and safety of treatment with rituximab for difficult steroid-resistant and -dependent nephrotic syndrome: multicentric report. Clin J Am Soc Nephrol 5:2207–2212
Kemper MJ, Gellermann J, Habbig S, Krmar RT, Dittrich K, Jungraithmayr T, Pape L, Patzer L, Billing H, Weber L, Pohl M, Rosenthal K, Rosahl A, Mueller-Wiefel DE, Dötsch J (2012) Long-term follow-up after rituximab for steroid-dependent idiopathic nephrotic syndrome. Nephrol Dial Transplant 27:1910–1915
Fujinaga S, Hirano D, Nishizaki N, Kamei K, Ito S, Ohtomo Y, Shimizu T, Kaneko K (2010) Single infusion of rituximab for persistent steroid-dependent minimal-change nephrotic syndrome after long-term cyclosporine. Pediatr Nephrol 25:539–544
Ravani P, Magnasco A, Edefonti A, Murer L, Rossi R, Ghio L, Benetti E, Scozzola F, Pasini A, Dallera N, Sica F, Belingheri M, Scolari F, Ghiggeri GM (2011) Short-term effects of rituximab in children with steroid- and calcineurin-dependent nephrotic syndrome: a randomized controlled trial. Clin J Am Soc Nephrol 6:1308–1315
Kamei K, Ito S, Nozu K, Fujinaga S, Nakayama M, Sako M, Saito M, Yoneko M, Iijima K (2009) Single dose of rituximab for refractory steroid-dependent nephrotic syndrome in children. Pediatr Nephrol 24:1321–1328
Guigonis V, Dallocchio A, Baudouin V, Dehennault M, Hachon-Le Camus C, Afanetti M, Groothoff J, Llanas B, Niaudet P, Nivet H, Raynaud N, Taque S, Ronco P, Bouissou F (2008) Rituximab treatment for severe steroid- or cyclosporine-dependent nephrotic syndrome: a multicentric series of 22 cases. Pediatr Nephrol 23:1269–1279
Magnasco A, Ravani P, Edefonti A, Murer L, Ghio L, Belingheri M, Benetti E, Murtas C, Messina G, Massella L, Porcellini MG, Montagna M, Regazzi M, Scolari F, Ghiggeri GM (2012) Rituximab in children with resistant idiopathic nephrotic syndrome. J Am Soc Nephrol 23:1117–1124
Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D (2001) Methods Work Group, Third US Preventive Services Task Force. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 20[3 Suppl]:21–35
Araya CE, Wasserfall CH, Brusko TM, Mu W, Segal MS, Johnson RJ, Garin EH (2006) A case of unfulfilled expectations. Cytokines in idiopathic minimal lesion nephrotic syndrome. Pediatr Nephrol 21:603–610
Hoyer JR, Vernier RL, Najarian JS, Raij L, Simmons RL, Michael AF (1972) Recurrence of idiopathic nephrotic syndrome after renal transplantation. Lancet 2:343–348
Savin VJ, Sharma R, Sharma M, McCarthy ET, Swan SK, Ellis E, Lovell H, Warady B, Gunwar S, Chonko AM, Artero M, Vincenti F (1996) Circulating factor associated with increased glomerular permeability to albumin in recurrent focal segmental glomerulosclerosis. N Engl J Med 334:878–883
Wei C, Trachtman H, Li J, Dong C, Friedman AL, Gassman JJ, McMahan JL, Radeva M, Heil KM, Trautmann A, Anarat A, Emre S, Ghiggeri GM, Ozaltin F, Haffner D, Gipson DS, Kaskel F, Fischer DC, Schaefer F, Reiser J, for the PodoNet and FSGS CT Study Consortia (2012) Circulating suPAR in two cohorts of primary FSGS. J Am Soc Nephrol 23:2051–2059
Yabu JM, Ho B, Scandling JD, Vincenti F (2008) Rituximab failed to improve nephrotic syndrome in renal transplant patients with recurrent focal segmental glomerulosclerosis. Am J Transplant 8:222–227
Ireland S, Monson N (2011) Potential impact of B cells on T cell function in multiple sclerosis. Mult Scler Int 2011:423971. doi:10.1155/2011/423971
Araya C, Diaz L, Wasserfall C, Atkinson M, Mu W, Johnson R, Garin E (2009) T regulatory cell function in idiopathic minimal lesion nephrotic syndrome. Pediatr Nephrol 24:1691–1698
Kemper MJ, Meyer-Jark T, Lilova M, Müller-Wiefel DE (2003) Combined T- and B-cell activation in childhood steroid-sensitive nephrotic syndrome. Clin Nephrol 60:242–247
Cho BS, Yoon SR, Jang JY, Pyun KH, Lee CE (1999) Up-regulation of interleukin-4 and CD23/FcepsilonRII in minimal change nephrotic syndrome. Pediatr Nephrol 13:199–204
Barisoni L, Schnaper HW, Kopp JB (2009) Advances in the biology and genetics of the podocytopathies: implications for diagnosis and therapy. Arch Pathol Lab Med 133:201–216
Faul C, Donnelly M, Merscher-Gomez S, Chang YH, Franz S, Delfgaauw J, Chang JM, Choi HY, Campbell KN, Kim K, Reiser J, Mundel P (2008) The actin cytoskeleton of kidney podocytes is a direct target of the antiproteinuric effect of cyclosporine A. Nat Med 14:931–938
Xing CY, Saleem MA, Coward RJ, Ni L, Witherden IR, Mathieson PW (2006) Direct effects of dexamethasone on human podocytes. Kidney Int 70:1038–1045
Fornoni A, Sageshima J, Wei C, Merscher-Gomez S, Aguillon-Prada R, Jauregui AN, Li J, Mattiazzi A, Ciancio G, Chen L, Zilleruelo G, Abitbol C, Chandar J, Seeherunvong W, Ricordi C, Ikehata M, Rastaldi MP, Reiser J, Burke GW 3rd (2011) Rituximab targets podocytes in recurrent focal segmental glomerulosclerosis. Sci Transl Med 3:85, ra46
Philit JB, Queffeulou G, Walker F, Gubler MC, Dupuis E, Vrtovsnik F, Mignon F (2002) Membranoproliferative glomerulonephritis type II and Niemann–Pick disease type C. Nephrol Dial Transplant 17:1829–1831
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cara-Fuentes, G., Kairalla, J.A., Ishimoto, T. et al. Rituximab in idiopathic nephrotic syndrome: does it make sense?. Pediatr Nephrol 29, 1313–1319 (2014). https://doi.org/10.1007/s00467-013-2534-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-013-2534-4