Abstract
Background
The aim of this study was to investigate renal function and injury in infants and young children with congenital heart disease (CHD).
Methods
We prospectively enrolled 58 CHD children aged ≤3 years and 20 age-matched controls and divided these into four groups: Group I, acyanotic CHD (n = 24); Group II, cyanotic CHD with arterial oxygen saturation of >75 % (n = 20); Group III, cyanotic CHD with arterial oxygen saturation of ≤75 % (n = 14); Group IV, normal controls (n = 20). Urinary levels of microalbumin (MA), N-acetyl-ß-D-glucosaminidase (NAG), and α1-microglobulin (α1-MG) corrected by creatinine (UCr) were compared.
Results
Children with CHD had elevated urinary α1-MG/UCr levels, with Group III children having the highest level. Groups I and III children had higher urinary NAG/UCr levels than those of Groups II and IV. Urinary MA/UCr levels in the three patient groups were comparable and significantly higher than that in the control group. A α1-MG × 100/ (α1-MG + MA) of <15 %, indicative of glomerular damage, was present in two patients in Group I and one in Group III, but none in Group II.
Conclusions
Tubular injury can occur in CHD patients during infancy and early childhood. Among our patient cohort, it was most prominent in children with severe cyanosis. Glomerular injury was detected in some individuals with advanced heart failure or severe cyanosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital heart disease (CHD) can be associated with renal injury and dysfunction. Most previous studies have focused on glomerular injury in elderly patients with cyanotic congenital heart disease (CCHD). These patients can develop glomerulopathy during their second decade of life, which manifests as significant proteinuria and reduced glomerular filtration rate (GFR) [1, 2]. Renal injury progresses with age, and cyanotic nephropathy is a serious complication in adults. The incidence of moderate-to-severe GFR reduction has been reported to be 35-fold higher in adults with CCHD than in the general population, with an associated fivefold higher mortality [3, 4]. The renal function of patients with acyanotic congenital heart disease (ACHD) has been less studied, and relatively few studies have focused on renal function in infants and young children with CHD.
One method commonly used in clinical practice to evaluate early renal injury is the measurement of urinary enzymes and low-molecular-weight (LMW) proteins. This urinary diagnostic approach has the advantages of non-invasive sample collection and few interfering proteins. N-acetyl-ß-D-glucosaminidase (NAG) is a lysosomal enzyme found predominantly in proximal tubular cells, and damage to these cells increases its release into the tubular lumen and excretion in the urine. α1- microglobulin (α1-MG) is a LMW protein which is freely filtered across the glomerular capillary wall and almost completely reabsorbed by proximal tubular cells. In the case of renal tubular dysfunction, its reabsorption is reduced and urinary excretion increases. Both NAG and α1-MG reflect renal tubular injury and dysfunction. In contrast, urinary microalbumin (MA) is a well-established indicator of glomerular damage. The aim of our study was to investigate renal function and injury in infants and young children with CHD based on the measurement of these urinary biomarkers.
Methods
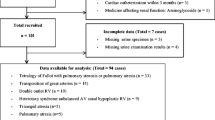
All qualified CHD children (≤3 years old) undergoing cardiopulmonary bypass surgery in Beijing Anzhen Hospital between November 2010 and April 2011 were prospectively enrolled in our study. Children who were referred to our department for innocent cardiac murmur and confirmed to be free of any heart disease by echocardiography in the same period were matched for gender and age as normal controls. All children were required to undergo normal ultrasound imaging of kidneys to determine morphology, echogenicity, and size. Children who had congenial abnormality of the urological system, known renal diseases, renal artery stenosis, urinary tract infection, severe liver dysfunction, primary blood disease, or malignant tumor, had recently used nephrotoxic drugs (including diuretics and angiotensin converting enzyme inhibitors), undergone previous cardiac surgery or been exposed to radiocontrast material prior to sample collection were excluded.
Fifty-eight patients and 20 controls fulfilled the inclusion and exclusion criteria and constituted the study population. These subjects were divided into four groups according to disease types and degrees of clinical cyanosis: Group I, ACHD (n = 24); Group II, CCHD with mild cyanosis (arterial oxygen saturation >75 %) (n = 20); Group III, CCHD with severe cyanosis (arterial oxygen saturation ≤75 %) (n = 14); Group IV, normal controls (n = 20). The grouping and diagnosis of patients are listed in Table 1.
We collected midstream urine samples from all children during early morning hours after overnight fasting, centrifuged the samples at 2,000 g for 10 min, and stored the supernatants at −4 °C until analysis. Urinary levels of MA, NAG, and α1-MG were measured within 48 h of sampling at Peking University First Hospital using immunoturbidimetry, spectrophotometry, and immunonephelometry, respectively. Concentrations of the biomarkers were expressed as ratios to urinary creatinine (UCr) to correct for variations in urine volume. As tubular dysfunction can also cause microalbuminuria owing to decreased reabsorption of filtered albumin [5], we adopted the albumin–alpha-1-microglobulin algorithm (AAA) to distinguish glomerular from tubular damage. The AAA has been shown to have the highest accuracy for profiling proteinuria and differentiating between tubular and glomerular proteinuria in children with kidney diseases [6]. The following formula was used: AAA = α1-MG × 100/ (α1-MG + MA). Only if AAA was <15 % was the microalbuminuria considered to be glomerular [6, 7].
Blood samples were taken simultaneously from patients as a routine preoperative laboratory examination to measure serum creatinine by the Jaffé assay. Estimated GFR (eGFR) was calculated by the Schwartz formula. Written informed consent was given by the parents or legal guardian of each child.
Statistical analysis
Statistical analysis was performed using SPSS ver. 13.0 (SPSS, Chicago, IL). Normally distributed variables were expressed as the mean ± standard deviation (SD) and non-normally distributed variables as the median and interquartile range. We defined the reference range of each biomarker concentration as mean ± 2 SD in the control group. Comparison of continuous variables among groups was carried out using one-way analysis of variance (ANOVA), Student–Newman–Keuls (SNK) test, and least significant difference (LSD) if normally distributed, or the Mann–Whitney U and Kruskal–Wallis H rank sum tests if not. Categorical variables were displayed as percentages and compared using the chi-square or Fisher’s exact test. Correlation was assessed with Spearman’s test. A P value of < 0.05 was considered to be statistically significant.
Results
Basic information
The patient cohort comprised 39 boys (67.2 %) and 19 girls (32.8 %), with a median age of 7.9 months (0.6–47.0 months) and a mean weight of 7.6 ± 2.9 kg. The demographic characteristics and results of the laboratory tests on the four groups are listed in Table 2. The sex, age, and weight of the children were comparable among all groups. Red blood cell counts and hematocrit were significantly different among the patient groups (Group III > Group II > Group I; P < 0.01), and hemoglobin levels were significantly higher in Group II and Group III than in Group I (P < 0.05). Serum creatinine levels were significantly higher in Group I and Group III than in Group II (Group I vs. II, P = 0.049; Group III vs. II, P = 0.022), but were not significantly different between the former two groups. Based on calculations using the Schwartz formula, Group I and Group III children did not have a significantly higher eGFR than Group II children.
Urinary biomarkers
Urinary biomarker levels of the four groups are shown in Table 3. Urinary NAG/UCr levels were higher in Groups I and III than in Group II (Group I vs. II, P = 0.037; Group III vs. II, P = 0.014, respectively) and Group IV (18.0 ± 9.7 U/g, P < 0.001). The upper limit of the NAG/UCr reference range was 37.3 U/g. An elevated NAG/UCr level was present in 14/24 patients (58.3 %) in Group I, 6/20 (30.0 %) in Group II, and 10/14 (71.4 %) in Group III (Group I vs. II, P = 0.060; Group I vs. III, P = 0.420; Group II vs. III, P = 0.017).
Urinary α1-MG/UCr levels were significantly higher in the three patient groups than in the control group (14.0 ± 9.5 mg/g, P = 0.012, 0.002, and <0.001 for Groups I, II, and III respectively). Group III children had higher levels of α1-MG/UCr than Group I and II children (P = 0.006 and 0.046, respectively). The upper limit of urinary α1-MG/UCr reference range was 33.0 mg/g. Elevated α1-MG/UCr was present in 8/24 patients (33.3 %) in Group I, 10/20 (50.0 %) patients in Group II, and 11/14 (78.6 %) patients in Group III (Group I vs. II, P = 0.263; Group I vs. III, P = 0.007; Group II vs. III, P = 0.092). Urinary NAG/UCr was positively correlated with α1-MG/UCr (r = 0.49, P < 0.05).
Urinary MA/UCr levels in the three patient groups were comparable and significantly higher than that in the control group (9.8 ± 4.5 mg/g, P < 0.001). The upper limit of the MA/UCr reference range was 18.7 mg/g. An elevated MA/UCr level was present in 18/24 patients (75.0 %) in Group I, 13/20 (65.0 %) patients in Group II, and 11/14 (78.6 %) patients in Group III (P = 0.639). An AAA of <15 %, which is indicative of glomerular damage, was present in 2/24 patients (8.3 %) in Group I and 1/14 (7.1 %) patients in Group III, but none in Group II. The urinary MA/UCr ratio was not significantly correlated with eGFR and hemoglobin levels.
Discussion
Renal injury and dysfunction are potential complications in CHD patients. Our study supplements previous studies on elderly patients and shows that infants and young children undergoing congenital heart surgery often have preoperative renal tubular injury.
Renal injury and function in CCHD
Complex CHD can be associated with congenital renal abnormality, which in turn may lead to renal dysfunction in CHD patients [8]. However, basic research and previous clinical studies suggest that hypoxia or cyanosis can result in renal injury, even in the absence of renal abnormality, and play a significant role in the pathogenesis and progression of chronic renal disease [9]. In renal cell culture models, chronic local hypoxia has been shown to influence tubular epithelial and mesangial cell proliferation, dedifferentiation, and extracellular matrix synthesis [10].
Small sample studies have shown that uncorrected CCHD patients can develop glomerular injury, with the risk of glomerulopathy increasing substantially during the second decade of life, manifested as significant proteinuria and reduced GFR. Dittrich et al. [1] studied the renal function of 26 patients with CCHD (aged 10–42 years). Ten patients showed reduced glomerular function, of whom six also had advanced glomerulopathy. The GFR was below normal in half of the patients and occurred concurrently with glomerular-type proteinuria in five of these and with tubular-type proteinuria in one. Krull et al. [2] analyzed urine samples from 23 patients with uncorrected CCHD (aged 1 day to 25 years). Only one of the nine children under 10 years of age had isolated albuminuria, seven of the ten patients between 11 and 20 years of age had an elevated proteinuria with a glomerular pattern, and all four patients above 20 years of age had a considerable glomerular proteinuria with reduced creatinine clearance.
Using sensitive urinary biomarkers, Akita et al. [11] assessed renal function in 16 patients with CCHD aged 3–28 years. Seven patients had increased levels of urinary MA, of whom six had proteinuria. Urinary levels of NAG were elevated in 14 patients, including those without proteinuria, and urinary β2-MG levels were elevated in some of these patients. These results suggest that glomerular and tubular injury were both present in patients with CCHD before glomerulopathy developed.
In contrast to previous studies, our study limited the study population to infants and young children (aged ≤3 years). Our results show that tubular injury was common in the very early course of CCHD even without glomerular damage, manifested as higher levels of urinary NAG and α1-MG than in the age-matched controls. This result is consistent with a recent study by Agras et al. (study population aged 0–13 years), which showed that tubular injury can be detected before glomerular injury occurs within the first decade of life [12]. By comparison, the strengths of our study are the diversity of disease types, more cases of severe cyanosis, and very young population.
Cyanosis could affect renal function through both direct pathological injury and secondary erythrocytosis and increased blood viscosity. In our very young population without long-standing hypoxia, we considered the hemodynamic effect of erythrocytosis to have a much greater impact on GFR. In this condition, renal plasma flow (RPF) is decreased [13, 14]. In addition, hyperviscosity could also lead to an increase in efferent glomerular arteriolar resistance, hydraulic pressure across the glomerulus, and filtration fraction, which could compensate for the reduction of RPF and preserve GFR [13, 14]. However, in severe cyanosis, the reduction in RPF would be so great that it could not be compensated for despite maximum hyperfiltration; therefore, the GFR would be reduced, as evidenced in the severely cyanotic children in our study.
CCHD with mild cyanosis versus severe cyanosis
Urinary levels of NAG and α1-MG normalized to UCr were higher in children with severe cyanosis than in those with mild cyanosis, while normalized urinary MA levels were not significantly different between these groups. The significantly increased MA levels in children with mild and severe cyanosis were tubular in nature, except for one case of severe cyanosis and significant glomerular-type microalbuminuria. This result indicates that more severe cyanosis may cause higher degrees of tubular injury. The explanation for the discrepancy between glomerular and tubular injury might be that tubular epithelial cells are more vulnerable to cyanosis and renal hypoxia.
Renal injury and function in ACHD
Few studies have evaluated renal injury in ACHD. Our study shows that tubular injury can be present in infants and young children with ACHD—two children with significant heart failure also had glomerular injury. There are several explanations for this finding.
-
(1)
We only enrolled children undergoing cardiac surgery, so the patient population on a whole is not representative of the general CHD population who might have less severe CHD. Younger children undergoing cardiac surgery often have large amounts of left-to-right shunt which could cause reduced systemic blood flow and vital organ hypoperfusion, including the kidneys. The unloading of baroreceptors within the cardiovascular system results in activation of the sympathetic nervous system (SNS), which leads to arterial vasoconstriction. The renin–angiotensin–aldosterone system is also activated by the SNS and by the stimulation of pressure and sodium receptors in the kidneys, thereby promoting tubular reabsorption of sodium and water. Although neurohormonal activation could compensate to preserve renal perfusion and GFR, the resultant fluid retention, volume overload, and arterial constriction could increase cardiac load, promote ventricular remodeling, and further deteriorate cardiac function. Persistent cardiac dysfunction can lead to renal hypoperfusion and injury [15].
-
(2)
In two patients, coronary anomalies caused coronary steal and myocardial ischemia and aggravated cardiac dysfunction.
-
(3)
A number of children suffered from anemia because of feeding intolerance and malnutrition, which could have induced renal local hypoxia and injury.
-
(4)
In nine children, coarctation of the aorta and interrupted aortic arch reduced renal perfusion pressure, leading to renal ischemia and damage. The fact that glomerular-type microalbuminuria was detected in two patients with prominent heart failure supports these cardio–renal theories and suggests glomerular damage with more advanced cardiac dysfunction. Because large amounts of left-to-right shunt, coarctation of aorta, and clinically overt heart failure can result in renal hypoperfusion, we consider the increase in serum creatinine in children with ACHD to be prerenal in nature.
We measured urinary NAG and α1-MG levels to assess renal tubular injury. The levels of both biomarkers were highest in children with severe cyanosis, but were inconsistent when children with ACHD and mild cyanosis were compared. We consider the discrepancy between these two biomarkers to be attributable to the different mechanisms between enzymes and LMW proteins. NAG is a typical lysosomal enzyme found predominantly in proximal tubular cells. Acute or chronic damage to renal tubular cells can induce the escape of enzymes physiologically present in the lysosomes, brush-border membrane, and cytoplasm of these cells into the tubular lumen. Urine enzyme excretion rates are elevated because of the release of these enzymes from damaged cells or from regenerating cells in which enzyme induction is intensified [16]. In contrast, α1-MG is a LMW protein which is freely filtered across the glomerular capillary wall and almost completely reabsorbed by proximal tubular cells. In the case of renal tubular dysfunction, its absorption is reduced and urinary excretion increases. Therefore, urinary NAG is an indicator of the structural integrity of tubular cells, while α1-MG denotes the reabsorptive function of proximal tubules. The reabsorption of α1-MG is an energy- and oxygen-consuming process, and hypoxia might reduce its absorption and increase urinary excretion even in the absence of damage to the structural integrity of tubular cells in children with mild cyanosis. Thus, urinary NAG levels might be lower in children with mild cyanosis than in those with ACHD, while urinary α1-MG levels may not be significantly different. Although differences did exist in our study, the urinary levels of the two biomarkers were positively correlated.
Study limitations and implications
Our patient population comprised infants and young children undergoing cardiopulmonary bypass surgery, and those who did not need cardiac surgery or who received off-pump cardiac surgery were excluded. Consequently, the study population is not representative of the whole CHD population. However, the younger children tended to develop acute kidney injury and renal failure after cardiopulmonary bypass surgery. Our results might have implications for the risk assessment of renal injury after surgery and perioperative management. Early surgical procedures to correct or partly relieve complex CHD could prevent or delay the process of further renal damage to irreversibility. An improvement of glomerular and tubular dysfunction has been observed in children with CCHD after palliative surgery [17]. The renal aspect should be taken into account when deciding upon the timing of cardiac surgery.
In conclusion, tubular injury can occur in CHD patients during infancy and early childhood, and among our patient group it was most prominent in children with severe cyanosis. Glomerular injury could be detected in some individuals with advanced heart failure or severe cyanosis.
References
Dittrich S, Haas NA, Buhrer C, Muller C, Dahnert I, Lange PE (1998) Renal impairment in patients with long-standing cyanotic congenital heart disease. Acta Paediatr 87:949–954
Krull F, Ehrich JH, Wurster U, Toel U, Rothganger S, Luhmer I (1991) Renal involvement in patients with congenital cyanotic heart disease. Acta Paediatr Scand 80:1214–1219
Dimopoulos K, Diller GP, Koltsida E, Pijuan-Domenech A, Papadopoulou SA, Babu-Narayan SV, Salukhe TV, Piepoli MF, Poole-Wilson PA, Best N, Francis DP, Gatzoulis MA (2008) Prevalence, predictors, and prognostic value of renal dysfunction in adults with congenital heart disease. Circulation 117:2320–2328
Flanagan MF, Hourihan M, Keane JF (1991) Incidence of renal dysfunction in adults with cyanotic congenital heart disease. Am J Cardiol 68:403–406
Birn H, Christensen EI (2006) Renal albumin absorption in physiology and pathology. Kidney Int 69:440–449
Lun A, Suslovych M, Drube J, Ziebig R, Pavicic L, Ehrich JH (2008) Reliability of different expert systems for profiling proteinuria in children with kidney diseases. Pediatr Nephrol 23:285–290
Seeman T, Dusek J, Vondrak K, Spatenka J, Feber J (2009) Profiling proteinuria in children after renal transplantation. Pediatr Nephrol 24:2439–2444
Kemper MJ, Muller-Wiefel DE (2001) Renal function in congenital anomalies of the kidney and urinary tract. Curr Opin Urol 11:571–575
Eckardt KU, Bernhardt WM, Weidemann A, Warnecke C, Rosenberger C, Wiesener MS, Willam C (2005) Role of hypoxia in the pathogenesis of renal disease. Kidney Int Suppl:S46-51
Sahai A, Mei C, Schrier RW, Tannen RL (1999) Mechanisms of chronic hypoxia-induced renal cell growth. Kidney Int 56:1277–1281
Akita H, Matsuoka S, Kuroda Y (1993) Nephropathy in patients with cyanotic congenital heart disease. Tokushima J Exp Med 40:47–53
Agras PI, Derbent M, Ozcay F, Baskin E, Turkoglu S, Aldemir D, Tokel K, Saatci U (2005) Effect of congenital heart disease on renal function in childhood. Nephron Physiol 99:10–15
Burlet A, Drukker A, Guignard JP (1999) Renal function in cyanotic congenital heart disease. Nephron 81:296–300
Inatomi J, Matsuoka K, Fujimaru R, Nakagawa A, Iijima K (2006) Mechanisms of development and progression of cyanotic nephropathy. Pediatr Nephrol 21:1440–1445
Jungbauer CG, Birner C, Jung B, Buchner S, Lubnow M, von Bary C, Endemann D, Banas B, Mack M, Boger CA, Riegger G, Luchner A (2011) Kidney injury molecule-1 and N-acetyl-beta-D-glucosaminidase in chronic heart failure: possible biomarkers of cardiorenal syndrome. Eur J Heart Fail 13:1104–1110
D’Amico G, Bazzi C (2003) Urinary protein and enzyme excretion as markers of tubular damage. Curr Opin Nephrol Hypertens 12:639–643
Awad H, El-Safty I, Abdel-Gawad M, El-Said S (2003) Glomerular and tubular dysfunction in children with congenital cyanotic heart disease: effect of palliative surgery. Am J Med Sci 325:110–114
Acknowledgments
We sincerely thank all of the children who participated in this study and their legal guardians for supporting our work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zheng, J., Yao, Y., Han, L. et al. Renal function and injury in infants and young children with congenital heart disease. Pediatr Nephrol 28, 99–104 (2013). https://doi.org/10.1007/s00467-012-2292-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-012-2292-8