Abstract
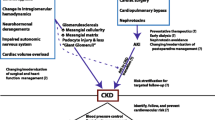
Cyanotic nephropathy (CN) is often accompanied by congenital cyanotic heart diseases (CCHD). The purpose of this study was to clarify the risk factors and the mechanisms of involved in the development and progression of CN. Thirty patients with CCHD were examined. We analyzed the risk factors for the development of CN on the basis of the clinical and laboratory findings. We also examined ten renal biopsy specimens obtained from patients with CN. Patients with CN showed significantly higher hematocrit levels than those without CN (P=0.025), although there was no difference between the two groups in terms of oxygen saturation. The renal plasma flow (RPF) in patients both with and without CN was low. However, the filtration fraction (FF) was significantly lower in patients with CN than in those without CN (P=0.001). The glomeruli of biopsy specimens with significant proteinuria (n=7) were larger than those of biopsy specimens without significant proteinuria, and there were more capillaries per glomerulus in the former than in the latter (n=3) and the control specimens (n=6) (glomerular size: P<0.01; number of glomerular capillaries: P<0.01). In conclusion, hyperviscosity by polycythemia may be responsible for the development of CN. This pathological condition may induce an angiogenic increase in the glomerular capillary beds, in turn leading to glomerulomegaly. In addition, the failure of a compensatory mechanism to respond to reduced RPF by hyperfiltration may be accompanied by the development and progression of CN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephropathy has long been recognized as a potential complication of cyanotic congenital heart disease (CCHD) [1, 2]. Due to advances in cardiovascular surgery, an increasing number of patients with CCHD are now surviving longer into adulthood and, consequently, may be at risk for developing renal abnormalities that may significantly influence any future clinical course [3]. It has been postulated that increased shear stress caused by polycythemic glomerular perfusate induces the release of NO, resulting in vascular dilatation and glomerulomegaly [4]. This hypothesis has received support from experimental evidence showing that normoxemic erythropoietin-induced polycythemia induces histological changes in the glomeruli that are similar to those associated with cyanotic nephropathy (CN) [5]. However, only a small number of clinical studies have been conducted with the aim of clarifying this hypothesis [6, 7]. Tubular injury as well as glomerular injury have also been reported [8]. One of the aims of the present study, therefore, was to retrospectively analyze clinical and laboratory findings in order to clarify the risk factors and the mechanisms of the development and progression of CN.
Previous studies have revealed that the kidneys of patients with CCHD show pathological changes, including glomerulomegaly, capillary dilatation, an increase in the number of capillary loops, a thickening or destruction of capillary walls, and mesangial proliferation [2, 4, 9]. However, most of these studies described findings obtained primarily from necropsies. Therefore, it is possible that the conclusions based on such findings are not necessarily reflective of the lesions during the early stage of CN. In addition, the relationship between clinical and pathological findings has not yet been sufficiently addressed in the literature. As a result, it has remained difficult to elucidate the mechanisms of the development and progression of CN. We have therefore examined the relationship between clinical findings, including proteinuria, and the pathological findings as a second approach to clarifying the mechanisms involved in the development and progression of CN.
Methods
Patients
We examined 30 patients with CCHD (16 males and 14 females) who were treated in the National Center for Child Health and Development. All patients or their parents gave their informed consent for participation in the study. The age of the patients at the time of the study was 20.2±1.4 years (range: 9–29 years). The underlying diseases among these patients were as follows: tetralogy of Fallot (n=6), tricuspid atresia (n=6), single ventricle (n=5), pulmonary atresia with ventricular septal defect (n=5), double outlet right ventricle (n=3), Eisenmenger syndrome (n=3), total anomalous pulmonary venous return (n=1), and double inlet left ventricle (n=1). We defined CN as the presence of significant proteinuria (urinary protein to creatinine ratio: >0.25) or renal dysfunction (24-h creatinine clearance: <80 ml/min/1.73 m2). To identify the risk factors for the development of CN, we compared the following data between two groups (CN and no CN): duration of the disease (age), oxygen saturation measured by pulse oxymeter (SpO2), hemoglobin, hematocrit, mean corpuscular volume (MCV), mean corpuscular hemoglobin concentration (MCHC), serum creatinine, uric acid, blood urea nitrogen (BUN), creatinine clearance, effective renal plasma flow (eRPF) as calculated by MAG3 renoscintigram, calculated renal blood flow (cRBF), filtration fraction (FF), and cardiothoracic ratio (CTR) observed on plain chest X ray.
Histological evaluation
Percutaneous renal biopsy was performed if the following criteria were satisfied: (1) patients were diagnosed with CN according to the above criteria, (2) no apparent congestive heart failure, (3) platelet count >1.0×105/μl, and (4) patients provided written informed consent. We divided the patients into groups according to the range of proteinuria (i.e., a urinary protein to creatinine ratio of more than 0.25 was considered to be significant). Kidney tissues obtained from autopsied patients without renal or cardiac disease served as controls. We compared the two main groups (CN with and without significant proteinuria, respectively) in terms of the following parameters: the cross-sectional area of the glomeruli, the cross-sectional area of the mesangium, and the number of capillaries per glomerulus. In each case, we prepared a periodic acid-Schiff (PAS) stain and a periodic acid methenamine silver (PAM) stain. An investigator (J.I.) who was blinded to the clinical status reviewed the renal biopsy and autopsy specimens.
The cross-sectional area of the glomeruli and the mesangium were measured using the point-counting method [10]. Briefly, each glomerulus was photographed under a light microscope (magnification: 400×). A 144-point grid was placed over the image of the sample, and the number of crosses of the grid on the glomerulus or the mesangium was counted. We observed all of the glomeruli in each specimen, except in those cases which had been cut along the peripheral planes and those which exhibited global sclerosis or severe shrinkage. In addition, we counted the number of glomerular capillaries per glomerulus. Glomerular capillary size was assessed as the ratio of glomerular size to the number of glomerular capillaries.
Statistical analysis
The values are expressed as mean ± standard error. For the univariate analyses, we used the Mann-Whitney U-test to compare unpaired two-group means. We used Fisher’s exact test to evaluate the association between categorical variables. We used ANOVA to compare means in three or more groups. For the multivariate analyses, we used the forward, stepwise logistic-regression model to identify the risk factors. The differences were evaluated using Stat-View ® J-5.0 software (Abacus Concepts, Berkeley, Calif.) and assessed to be significant at a difference of P<0.05.
Results
Clinical findings associated with CN
Seventeen of the patients included in this study had CN, whereas 13 did not. The univariate analysis revealed that compared to patients without CN, those with CN had significantly higher hematocrit levels (62.6±2.5 vs.53.9±1.8%, P=0.025; normal: 38.2–42.0%), whereas no difference was observed between the two groups with respect to oxygen saturation. Creatinine clearance and urinary protein levels differed between the two groups because the patients had been divided into groups based on whether or not they had renal dysfunction or significant proteinuria.
The RPF of both groups of patients (with and without CN, respectively) was lower than the normal value (365.2±24.9 and 363.9±19.6 ml/min, respectively; normal: 385–639). However, the FF was significantly lower in patients with CN than in patients without CN (0.219±0.029 vs. 0.359±0.031, P=0.001; normal: 0.20–0.22), while cRBF was significantly higher in patients with CN than in those without CN. The logistic regression analysis revealed that only the hematocrit levels (P=0.049) and FF (P=0.045) were significant and independent risk factors for the development of CN (Tables 1, 2).
Pathological analysis
Ten renal biopsy specimens obtained from patients with CN were examined. Seven patients had significant proteinuria, but three had no significant proteinuria (Table 3). Renal function (creatinine clearance) of the both groups were similar (69.6±9.0 ml/min/1.73 m2 (with significant proteinuria) vs. 64.4±7.0 ml/min/1.73 m2 (without significant proteinuria), P=0.732). Biopsy specimens showing significant proteinuria (n=7; age of patient: 17.6±2.5 years) also showed a significantly larger glomerular size and significantly more glomerular capillaries than both specimens lacking significant proteinuria (n=3, age of patient: 18.7±4.9 years) and control specimens (n=6, age of patient: 18.3±0.2 years) (glomerular size: 76.8±4.9 vs. 53.4±3.3 vs. 48.5±3.9 points, respectively, P<0.01 vs. the other two groups; number of glomerular capillaries: 104.4±5.6 vs. 67.8±9.3 vs. 58.8±3.9, respectively, P<0.01 vs. the other two groups). However, no differences were observed among the three groups in terms of glomerular capillary diameter and the degree of mesangial proliferation. Images representative of samples from each group are shown in Fig. 1.
a A kidney tissue sample obtained upon autopsy of a case without renal or cardiac disease (Control; magnification: 400×). b A renal biopsy specimen obtained from a patient with cyanotic nephropathy (CN) without significant proteinuria (magnification: 400×). c A renal biopsy specimen obtained from a patient with CN with significant proteinuria (magnification: 400×)
Only biopsy specimens with significant proteinuria showed global glomerular sclerosis (1/9 glomeruli = 11%), whereas none of the biopsy specimens showed segmental sclerosis, adhesion, or changes of vasculature. Four biopsy specimens with significant proteinuria (4/7) showed mild-to-moderate interstitial fibrosis, whereas none of the biopsy specimens without significant proteinuria (0/3) showed interstitial fibrosis. Creatinine clearance of the patients with interstitial fibrosis was lower than that of the patients without interstitial fibrosis, although the difference was not statistically significant [53.1±7.8 ml/min/1.73 m2 (with interstitial fibrosis) vs. 78.0±7.2 ml/min/1.73 m2 (without interstitial fibrosis), P=0.055].
Discussion
Patients with persistent CCHD have a substantial risk of developing glomerulopathy. In a previous report, more than 70% of CCHD patients over 10 years of age had significant glomerular proteinuria [11]. In the present study, we demonstrated that hematocrit levels were higher in patients with CN than in those without CN, whereas no difference was observed between these groups in terms of oxygen saturation. Therefore, we conclude that polycythemia, rather than hypoxia, is a risk factor for the development of CN, and our results provide support for the previously reported hypothesis that increased sheer stress induced by polycythemia is the primary cause of CN.
Long-standing CCHD has been reported to be a risk factor for glomerulopathy, although we did not detect any age-specific differences between the two groups in the present study. However, it should be noted that such differences would not necessarily have been observed by us as only relatively older patients (>9 years) were included in our study.
Upon observation of the MAG3 renoscintigram, RPF was found to be decreased in both groups of patients, whereas the FF was increased only among those patients without CN. These findings suggest that renal perfusion is decreased even at the early stage of this disease, i.e., at stages during which hyperfiltration compensates for decreased RPF, thus preserving the glomerular filtration rate (GFR). Failure of this putative compensatory mechanism is likely to be the reason for the development and progression of CN. However, the lower FF in CN groups may be the result – but not the cause – of CN, since FF is calculated from GFR/RPF and creatinine clearance is already lower in patients with CN.
What is the cause of this lower creatinine clearance? Glomerulomegaly per se is unlikely to be a cause of the lower GFR. Of interest is our observation that creatinine clearance was lower in patients with interstitial fibrosis than in those without interstitial fibrosis. Therefore, in at least some of the patients with CN, the decreased GFR was due to interstitial fibrosis. Moreover, more than one half of the biopsy specimens with significant proteinuria showed mild-to-moderate interstitial fibrosis, whereas none of the biopsy specimens without significant proteinuria showed interstitial fibrosis. These findings suggest that long-term proteinuria per se induces the interstitial fibrosis and indicate the degree of the relationship between proteinuria and the severity of CN.
In most of the published findings that have addressed these issues, autopsied kidneys were examined [2, 4, 9]. In contrast, only a few case reports have been published in which renal biopsy findings are discussed [12, 13]. This provided us with the reason to examine ten biopsy specimens and quantitatively analyze the range of glomerulomegaly and mesangial proliferation. Our CN patients showed glomerular enlargement and capillary proliferation, thus providing support for the findings reported in the previous studies. We did not observed any differences in the ratio of glomerular size to the number of glomerular capillaries between the CN and non-CN groups, thus indicating that there was no significant difference between these groups with respect to glomerular capillary size. Furthermore, there was no difference with respect to the size of mesangial matrix between the two groups. It should be noted that these latter findings are not consistent with those reported in earlier publications. However, as mentioned, in most of the studies reported autopsied specimens were examined, and approximately one half of the patients considered in those studies died of heart failure [2, 4]. Therefore, it is possible that heart failure-induced glomerular congestion resulted in the pathological findings reported. Capillary enlargement and/or engorgement or increases in the size of the mesangial matrix may be signs of progressive nephropathy, and these signs may not be present during the early phases of CN. Collectively, the glomerulomegaly seen at an early stage of CN may be primarily due to glomerular capillary angiogenesis caused by glomerular endothelial cell proliferation.
Although the mechanisms of the development of proteinuria in patients with CN are still unknown, there are several possibilities. First, the hyperviscosity-induced decrease in peritubular capillary blood flow might lead to an increase in glomerular capillary pressure, in turn resulting in proteinuria, as previously hypothesized by Dittrich and colleagues [6]. Second, a marked increase in the glomerular capillary surface area may impair podocyte function, in turn resulting in proteinuria. Mature podocytes are growth-arrested due to the expression of cyclin-dependent kinase inhibitors. Under pathological conditions, podocytes may undergo mitosis, but not cell division. Thus, an increase in the glomerular capillary surface area may induce podocyte stress, resulting in podocyte hypertrophy. However, under such conditions, hypertrophic podocytes can no longer compensate for a markedly increased glomerular surface area, thereby leading to podocyte dysfunction, in turn resulting in proteinuria. In a study by Fogo et al. [14], the presence of glomerular hypertrophy in biopsied tissues of patients with minimal change disease suggested an increased risk for progression to focal segmental glomerulosclerosis (i.e. podocyte injury) [15, 16]. In the present study, we demonstrated that the development of proteinuria correlated well with both glomerular size and the number of glomerular capillaries and, consequently, the present findings provide additional support for the latter possibility.
Similar levels of hypoxia in CN and non-CN result in different hematocrit levels. What factor involves in hematocrit levels in CCHD? Although we did not examine the serum levels of erythropoietin in this study, Eckardt et al. reported that in children with heart disease, serum immunoreactive erythropoietin values were inversely correlated to the arterial oxygen content [17]. However, in our study, hematocrit levels were significantly higher in the patients with CN, whereas SpO2 levels in the patients with CN were not different from those in the patients without CN. Therefore, it is unlikely that the higher hematocrit levels seen in the patients with CN are due to the increased levels of erythropoietin. Further studies are needed to clarify the mechanisms of polycythemia seen in CN.
In conclusion, hyperviscosity due to polycythemia may be responsible for the development of CN. This pathological condition might induce an angiogenic increase in the size of glomerular capillary beds, leading in turn to glomerular hypertrophy. Moreover, the failure of a compensatory mechanism to respond to reduced RPF by hyperfiltration may be accompanied by the development and progression of CN. However, we were unable to provide clear-cut evidence supporting the premise that the hypervascularity causes glomerulomegaly. To elucidate the contribution of hypervascularity as a cause of glomerulomegaly, the cause of hypervascularity itself, such as some humoral factors, should be elucidated.
References
Spear GS (1964) The glomerulus in cyanotic congenital heart disease and primary pulmonary hypertension. A review. Nephron 1:238–248
Spear GS (1960) Glomerular alterations in cyanotic congenital heart disease. Bull Johns Hopkins Hosp 106:347–367
Tanaka J, Yasui H, Nakano E, Sese A, Matsui K, Takeda Y, Tokunaga K (1980) Predisposing factors of renal dysfunction following total correction of tetralogy of Fallot in the adult. J Thorac Cardiovasc Surg 80:135–140
Perloff JK, Latta H, Barsotti P (2000) Pathogenesis of the glomerular abnormality in cyanotic congenital heart disease. Am J Cardiol 86:1198–1204
Wilcox CS, Deng X, Doll AH, Snellen H, Welch WJ (1993) Nitric oxide mediates renal vasodilatation during erythropoietin-induced polycythemia. Kidney Int 44:430–435
Dittrich S, Kurschat K, Lange PE (2001) Abnormal rheology in cyanotic congenital heart disease–a factor in non-immune nephropathy. Scand J Urol Nephrol 35:411–415
Dittrich S, Haas NA, Buhrer C, Muller C, Dahnert I, Lange PE (1998) Renal impairment in patients with long standing cyanotic congenital heart disease. Acta Paediatr 87:949–954
Agras PI, Derbent M, Ozcay F, Baskin E, Turkoglu S, Aldemir D, Tokel K, Saatci U (2005) Effect of congenital heart disease on renal function in childhood. Nephron Physiol 99:10–15
Hagley MT, Murphy DP, Mullins D, Zarconi J (1992) Decline in creatinine clearance in a patient with glomerulomegaly associated with a congenital cyanotic heart disease. Am J Kidney Dis 20:177–179
Weibel ER (1979) Stereological methods: practical methods for biological morphometry, vol. 1. Academic Press, London, pp 40–160
Krull F, Ehrich JH, Wurster U, Toel U, Rothganger S, Luhmer I (1991) Renal involvement in patients with congenital cyanotic heart disease. Acta Paediatr Scand 80:1214–1219
Burke JR, Glasgow EF, McCredie DA, Powell HR (1977) Nephropathy in cyanotic congenital heart disease. Clin Nephrol 7:38–42
Hida K, Wada J, Yamasaki H, Nagake Y, Zhang H, Sugiyama H, Shikata K, Makino H (2002) Cyanotic congenital heart disease associated with glomerulomegaly and focal segmental glomerulosclerosis: remission of nephrotic syndrome with angiotensin converting enzyme inhibitor. Nephrol Dial Transplant 17:144–147
Fogo A, Hawkins EP, Berry PL, Glick AD, Myra LC, MacDonell RC, Ichikawa I (1990) Glomerular hypertrophy in minimal change disease predicts subsequent progression to focal glomerular sclerosis. Kidney Int 38:115–123
Fries JW, Sandstrom DJ, Meyer TW, Rennke HG (1989) Glomerular hypertrophy and epithelial cell injury modulate progressive glomerulosclerosis in the rat. Lab Invest 60:205–218
Nagata M, Kriz W (1992) Glomerular damage after uninephrectomy in young rats. II. Mechanical stress on podocytes as a pathway to sclerosis. Kidney Int 42:148–160
Eckardt KU, Hartmann W, Vetter U, Pohlandt F, Burghardt R, Kurtz A (1990) Serum immunoreactive erythropoietin of children in health and disease. Eur J Pediatr 149:459–464
Acknowledgment
This study was partially supported by a Health and Labor Sciences Research Grant (H16-Kodomo-015 to Dr. Iijima) and a Grant for Child Health and Development (16C-2 to Dr. Iijima).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inatomi, J., Matsuoka, K., Fujimaru, R. et al. Mechanisms of development and progression of cyanotic nephropathy. Pediatr Nephrol 21, 1440–1445 (2006). https://doi.org/10.1007/s00467-006-0220-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0220-5