Abstract
The aim of this study was to evaluate the final stature of adults with childhood-onset steroid-responsive idiopathic nephrotic syndrome (INS) and the influence of disease-related issues on the achievement of their target heights. We analyzed 60 (41 male) patients and/or their records, with a minimum age of 19 years or at a Tanner’s pubertal stage 4 for boys or status postmenarche for girls, and normal glomerular filtration rate. Mean age at first and last consultation was 5.3 ± 2.4 years and 20.5 ± 3.1 years, respectively. Mean follow-up period was 15.10 years. Mean cumulative dose of prednisone was 1254 ± 831.40 mg/kg. Mean initial and final height Z scores (HtZ) were, respectively, −0.60 ± 1.0 and −0.64 ± 0.92 (p = 0.72). The final HtZ showed a significant correlation only with the initial HtZ and the target HtZ (THZ). Six patients achieved a final HtZ below −2, which in male patients correlated strongly to the initial HtZ and THZ. A strong correlation was demonstrated between final HtZ, initial HtZ, and THZ. INS-related issues did not prevent the final stature to reach the predicted target height.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome (INS) is characterized by massive urinary protein loss (>40 mg/h/m2 or urinary protein to urinary creatinine ratio >2 mg protein per milligram creatinine), associated with hypoalbuminemia (<2.5 g/100 ml), generalized edema, and hyperlipidemia [1]. The vast majority of children with NS respond to oral prednisone, which is currently the universally accepted treatment of choice for INS. However, although steroid responsive, about 60% of patients have frequent relapses or become steroid dependent, requiring high doses of prednisone for long periods, which is a potential risk for growth retardation [1–3]. Normal growth is influenced by familial genetic characteristics and different environmental factors, such as climate, nutrition, and social aspects, among others [4, 5]. INS is a chronic disease that may affect normal growth negatively, infrequently resulting in short stature [2, 6–9].
The aim of this study was to evaluate the final stature of adults with childhood-onset steroid-responsive INS and the influence of patient characteristics, INS course, steroid therapy, use of additional immunosuppressive agents, kidney histology, and associated infectious comorbidities on the achievement of their predicted target heights.
Patients and methods
Patients
-
A.
Retrospective analysis of medical records
The medical records of previously described 85 steroid-responsive INS patients were analyzed according to the following inclusion criteria: minimum age of 19 years or Tanner pubertal stage 4 for boys/status postmenarche for girls [10] and normal glomerular filtration rate. According to these criteria, 60 patients from the original cohort could be evaluated. Data collection included gender, serial anthropometric measurements, age at onset of INS, age at first clinic visit, age at last clinic visit, kidney histology, INS course according to response to steroids, total prednisone dose, duration of steroid therapy, associated immunosuppression, necessity of other medications, comorbidities, description of hospital admissions, and parental heights and target height.
-
B.
Prospective patient evaluation
In addition to medical records data analysis, the selected patients were invited by letter to schedule a clinic appointment at the outpatient clinic of the Pediatric Nephrology Unit of “Instituto da Criança” of “Hospital das Clínicas” of the Medical School of the University of São Paulo. After informed consent, an interim clinical history evaluation was performed that included INS activity, steroid utilization and comorbidities since the last clinic visit, a detailed physical examination, and blood and urine laboratory tests.
Methods
Initial and final heights were defined as the height evaluation obtained at the first/last clinic visit, respectively. The weight at the second clinic visit was defined as initial weight to avoid weight overestimation secondary to edema. Final weight was defined as the weight at the last clinic visit. The anthropometric parameters were collected sequentially at 6 months interval. The target height was calculated based on parental heights, as follows: {[father’s stature (cm) + mother’s stature (cm)] plus 13 cm in males or minus 13 cm in females, divided by 2} [4]. Based on height measurements at the final clinic visit, the difference between the initial and final height Z score (HtZ) was calculated for each patient and named delta stature Z score.
With the EpiInfo™ Nutrition Program, initial and final measurements of weight, height, and body mass index (BMI) of each patient were classified according to Centers for Disease Control CDC 2000 anthropometric parameters [10]. The upper and lower limits of normal stature were considered to be those at the 95th and 5th percentiles of the CDC National Center for Health Statistics (NCHS) curves, respectively. BMI was calculated by the formula: weight (kg)/stature (m2) [11]. BMI Z-score values between −2 and +1 were considered appropriate; between +1 and +2 were considered overweight; >+2 were classified as obesity and <−2 as malnutrition [10]. Pubertal development was evaluated according to Tanner stages of pubertal development [12]. The Z score was calculated using the formula Z score = Vo-M/SD, where Vo = value of weight or height, M = mean weight or height; SD = standard deviation [13].
Total dose of prednisone and time span of its utilization were calculated for each patient. The average dose of prednisone and the average time of prednisone utilization were also calculated for the whole patient group and for subgroups of patients classified according to steroid response and/or growth pattern. Recurrent upper airway infection was defined as at least six episodes of upper respiratory infection per year. The following laboratory parameters were obtained from the records/patients at the last clinic visit: serum creatinine (processed by a modified Jaffé reaction), total serum proteins albumin and globulin (performed by means of the biuret reaction), and a urinary protein/creatinine ratio. Creatinine clearance was calculated using the Cockcroft and Gault formula (reference value 80–120 ml/min/1.73 m2) [14].
INS was classified as steroid responsive according to the criteria of the International Study of Kidney Disease in Children (ISKDC) [15, 16]. Patients were treated with prednisone and other immunosuppressive agents following treatment protocols accepted in the literature [1, 15]. The study was approved by the Ethics Committee of Hospital das Clinicas of the Medical School of the University of São Paulo and supported by a research grant from FAPESP (process number 2007/00509-0).
Statistical analysis
The database was built using the Statistical Package for Social Science (SPSS) for Windows, version 11.0. The Kolmogorov-Smirnov test was performed to confirm that the anthropometric variables presented a normal distribution. The paired t test was used to compare the mean Z score for stature at the first and last evaluations in the total sample and various subgroups. The chi-squared test, Fisher’s exact test, and analysis of variance (ANOVA) were used to compare in both genders, in the total sample, and in the clinical subgroups qualitative variables such as renal biopsy results, type of response to steroids, use of other immunosuppressive medications, and associated comorbidities. Student’s t test and Pearson’s correlation test were used to compare in both genders, in the total sample, and in the clinical subgroups the continuous variables: initial and final age, initial and final BMI, age at discontinuation of prednisone use, duration of prednisone use, cumulative dose of prednisone, initial and final HtZ, and target height Z scores (THZ). Confidence limits were set at 5% to exclude the null hypothesis [13].
Results
We evaluated 60 patients, and/or their records, with steroid-responsive INS diagnosed in childhood/adolescence and followed at the Pediatric Nephrology Unit of “Instituto da Criança” of “Hospital das Clínicas” of the Medical School of the University of São Paulo, with a minimum age of 19 years or Tanner pubertal stage 4 for boys or status postmenarche for girls. Of these, 41 (68.3%) were male patients; the male:female ratio was 2.1:1, chi square (p = 0.00). The target height could be obtained for 36/60 (60%) patients. At the last clinic visit, patients were all in INS remission with a normal glomerular filtration rate measured by creatinine clearance. A renal biopsy was performed in 40 (66.7%) patients. Associated comorbidities were present in 35 (58.3%) patients.
Mean cumulative dose of prednisone was 1,254 mg/kg [SD 831.4 (mg/kg)]. The average time between the last dose of prednisone and the final patient evaluation was 8 years (SD 5 years). At the time of final evaluation, a 27-year-old patient was under a prednisone dose-reducing schedule secondary to a steroid-sensitive relapse. Mean BMI at the first evaluation was 17.3 (SD 2.1) with a mean Z score of 0.77 (SD 1.1). On that first evaluation, 17/60 patients (28.3%) were classified as overweight and 7/60 (11.7%) as obese. Mean BMI at the final evaluation was 22.4 (SD 3.9) with a mean Z score −0.12 (SD 1.0). At the last evaluation, 2/60 patients (3.3%) were classified as malnourished, 5/60 (8.3%) as overweight, and 1/60 (1.6%) as obese. Comparison between the mean initial and final HtZ, by paired t test, showed no statistical significance (p = 0.72). Mean delta stature Z score for the whole group was −0.04 (SD 1.0). Analysis of each patient growth pattern allowed the definition of three subgroups: subgroup A, composed of patients who achieved growth improvement; subgroup B, composed of patients who showed growth retardation in comparison to the initial HtZ score; and subgroup C, composed of patients who had a final HtZ score < −2.
Subgroup A (improved growth)
This group was composed of 27 (45%) patients; 20 were male, and seven were female. Mean initial HtZ score was −1.2 (SD 0.67), and the final HtZ score was −0.44 (SD 0.90) (paired t test p = 0.00) with a mean delta stature Z score of 0.82 (SD 0.72). The THZ, obtained in 16/27 (59%) patients, was −1.00 (SD 0.96). Five patients (four male and one female) of subgroup A had an initial HtZ < −2. These patients gained growth percentiles during the observation period and achieved a final HtZ ≥ −2.
Subgroup B (loss of growth percentiles)
This group was composed of 27 (45%) patients; 17 were male and ten were female. Their mean initial HtZ was 0.18 (SD 0.73), and the final HtZ was −0.49 (SD 0.63) (paired t test p = 0.00), with a mean delta stature Z score of −0.68 (SD 0.46). The THZ, obtained in 15/27 (55%) patients, was −0.70 (SD 0.7).
Subgroup C (final stature Z score < −2)
This group was composed of six (four male and two female) patients whose mean initial HtZ was −1.19 (SD 0.82) and final HtZ was −2.28 (SD 0.29) (paired t test p = 0.03), with a mean delta stature Z score of −1.09 (SD 0.88). In this group, one male patient gained growth percentiles, whereas five patients lost growth percentiles during the follow-up period. The THZ, obtained in 5/6 (83%) patients, varied between −1.72 and −2.34. Table 1 describes the individual characteristics of group C patients.
Tables 2 and 3 show a summary of patient variables in the patient group as a whole and in the A, B, and C subgroups. Each variable was compared between the patients who gained and those who lost growth percentiles during study period (Analysis 1) and between patients whose final HtZ was ≥-2 and <−2 (Analysis 2).
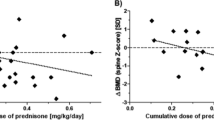
The influence of the variables described in Tables 2 and 3, on the final HtZ, was evaluated by Pearson’s correlation test (quantitative data) or by ANOVA (qualitative data) and was significant for initial HtZ and THZ. A separate analysis was also performed with data on HtZ at 11.8 years of age, patients’ mean age at the time of our previous study [3], which also correlated significantly with THZ. Figures 1, 2, and 3 present, respectively, the scatter plots demonstrating the linear relationship between THZ and initial HtZ, THZ and final HtZ, and THZ and HtZ at 11.8 years.
Discussion
The growth of children with INS is influenced by the same factors that affect the general population, added to INS-related factors, especially the degree of proteinuria and, after remission, the dosing and timing of corticotherapy. In this study, we evaluated the final height of 60 steroid-sensitive INS patients previously described by us [3]. In our previous study, we described 85 steroid-sensitive NS patients and analyzed the influence of several associated factors on their statural growth. Our results at that time showed that steroid-responsive pediatric INS patients, especially boys, may gain growth percentiles with appropriate control of the disease and discontinuity of steroids in preadolescence, favoring the growth spurt. On the other hand, we observed loss of growth percentiles in patients who used higher doses of steroids for a longer time span, which may have contributed to a blockage or retardation of pubertal growth. Six male patients developed short stature during the follow-up. These patients had, at the end of the study, a mean age of 11.8 years, and consequently had not reached the final stature. At that occasion, data on the patients’ target height was lacking. This piece of information was added for the majority of patients described in the study presented here.
This analysis shows that for our patient population, there was no difference between the mean initial and final HtZ score (p = 0.72, t test), as the individual gains and losses of growth percentiles were compensated in the total sample. These findings confirm most of the data of similar clinical studies in the literature [6–9, 17], which analyzed their patient series as a group, even after high doses of prednisone were used. An analysis of each individual patient allowed the definition of three subgroups, as in the previous study. Subgroup A, which achieved growth improvement; subgroup B, which showed growth retardation; and subgroup C, which showed a final HtZ score < −2.
Which factors could have influenced the gain or loss of growth percentiles in relation to the initial stature in these patients? The loss of growth percentiles could not be foreseen by the patients’ past clinical history prior to admission to our service, as they did not show any evidence of chronic diseases before the onset of INS. Malnutrition can also be ruled out as a cause of lower HtZ scores in the first clinic visit, as 60% of the patients presented with an adequate BMI and 40% were diagnosed as overweight or obese. The duration of INS symptoms prior to the first clinic visit to our service, which was <6 months for the majority of patients, did not show an association with the initial (p = 0.20) or the final (p = 0.64) HtZ score or with the gain or loss of growth percentiles during the study period (p = 0.30).
The existence of a group of steroid-sensitive INS patients who gain growth percentiles during follow-up was described in our previous study [3] and is supported by the literature [6, 7]. In 1994, Martinelli el al. [18] demonstrated, in normal children, that in physiological conditions, there is a significant positive correlation between secretion of cortisol and growth hormone (GH) over 24 h. Glucocorticoids (GC) increase the synthesis and release of GH from pituitary cells in vitro, activating the gene transcription of GH and increasing the number of receptors of growth-hormone-releasing hormone (GHRH) [19]. In contrast, chronic administration of GC in vivo may inhibit secretion of GH [20] but, curiously, depending on the time of exposure and the presence of other hormones such as triiodothyronine (T3), it may also cause stimulation of transcription of these genes [21].
Periods of hypercortisolism induce an increase of insulin-like growth-factor-binding protein (IGFBP)-1 levels, a decrease of IGFBP-2 levels, in association with an increase in the production of fragments resulting from IGFBP-3 proteolysis. This combination of events might be responsible for the decrease in the bioavailability or bioactivity of insulin-like growth factors (IGF). The reduced bioactivity of IGF might, in turn, reduce the negative feedback on hypothalamic−pituitary level, stimulating GH secretion. This could be the mechanism involved for the parallel and concordant changes in the secretion of cortisol and GH [18]. In some children, the response to the increased production of GH could be so effective that satisfactory growth would result. In others, secondary hormonal changes such as hyperinsulinism secondary to hypercortisolism may unfavorably influence growth. A negative influence on growth, induced by prolonged exposure to supraphysiological concentrations of GC, could also result from a reduced release of GHRH and/or increase in the somatostatinergic tonus, or by a direct inhibition of somatotroph responsiveness to GHRH leading to a decreased pituitary secretion of GH [18].
Another important factor to be considered is compensatory growth. Periods of growth retardation reduce the proliferation of chondrocytes. When the causes for growth retardation are solved, these cells show increased proliferative potential [22]. In some children, INS remission, resulting in improvement of general health conditions and normalization of serum albumin, and of the hypoalbuminemia-related hormonal disturbances, could trigger bone-plate compensatory growth despite ongoing GC therapy, especially if GC were administered on alternate days [23–25].
The analysis of data presented in Tables 2 and 3 show that the variables significantly related to loss of growth percentiles were lower mean initial HtZ, use of cyclophosphamide in male patients (p = 0.04 Fisher’s test and Pearson’s correlation test), and diagnosis of chronic hepatitis C (p = 0.04 Fisher’s test; p = 0.03 Pearson’s correlation test). As cyclophosphamide was used for steroid dependence or for initially steroid-resistant patients and hepatitis C, which represents a serious comorbidity, these findings may be interpreted as secondary to an increase in disease severity. On the other hand, the variables associated with a final HtZ < −2 were the initial HtZ and the THZ.
In our previous study [3], the gain of growth percentiles occurred predominantly in children using lower doses of GC, whereas the loss of growth percentiles occurred in older ages affecting the adolescent stage of growth. It is known that growth in adolescence is controlled by different genetic and hormonal mechanisms than those that control growth during early childhood [26, 27]. In the study presented here, analysis of the influence of cumulative doses of prednisone, time span of prednisone utilization, mean age of discontinuation of prednisone, and age group at discontinuation of prednisone (before or after 12 years of age) did not confirm our previous findings, as none of these factors proved to be influential on defining either gain or loss of growth percentiles during the study period or final HtZ < −2. Also in this study, the main determinants of the final HtZ were initial HtZ score and target height. Patients’ initial and final HtZ scores showed a significant correlation with the THZ score (Figs. 1 and 2).
How can we reconcile the conclusions of our previous study with those of this study? Interestingly, looking back at that moment in time in our patients’ growth curves, it is noteworthy that despite the influence of the disease and its treatment, patients’ HtZ score at that moment was significantly correlated with the target HtZ score, as shown in Fig. 3. Our data agree with the findings of Ruth et al. [17], who demonstrate in their patient series that the final height was similar to the expected value, in both male and female patients, and the favorable outcome could be attributed to the maintenance of alternate-day steroid therapy in the long term. The authors also suggest that after discontinuation of GC, a compensatory growth might occur to recover previous growth retardation periods.
A final word on account of the six patients who achieved final stature Z score < −2: Analysis of our data show that the male patients who reached adulthood with short stature presented lower growth percentiles on admission to our service, which at that time were already in accordance with their target HtZ score, confirming for this small subgroup the findings of the group as a whole that the main determinants of the final HtZ were the initial HtZ and the THZ. Analysis of female patients of group C was not possible due to their small number and the lack of information on parental heights on one of the patients.
In conclusion, the initial mean HtZ score with a mean age of 5.2 years (SD 2.4 years), the HtZ at our previous study with mean age of 11.8 years (SD 3.1 years), and the final HtZ score at a mean age of 20.4 years (SD 3.0 years) were strongly correlated to the THZ. During the study period, there were gains and losses of growth percentiles in comparison to the initial stature Z score, probably related to the severity of the disease, its comorbidities, and periods of growth delay secondary to steroid utilization followed by periods of growth compensation after steroid discontinuation. These fluctuations, however, have not proved to be an impediment for this series of patients with steroid-responsive INS to seek and reach the expected target height in adulthood. Our findings suggest that the genetic background must be the strongest factor influencing the final height of children with INS.
References
Eddy AA, Symond JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639
Crew RJ, Rashakrishnan J, Appel G (2004) Complications of the nephrotic syndrome and their treatment. Clin Nephrol 62:245–249
Donatti TL, Koch VH, Fujimura MD, Okay Y (2003) Growth in steroid-responsive nephrotic syndrome: a study of 85 pediatric patients. Pediatr Nephrol 18:789–795
Tanner JM, Goldstein H, Whitehouse RH (1970) Standards for children’s height at ages 2–9 years allowing for height of parents. Arch Dis Child 45:755–762
WHO Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization, Geneva, p 312
Lam CN, Arneil GC (1968) Long-term dwarfism effects of corticosteroid treatment for childhood nephrosis. Arch Dis Child 43:589–594
Polito C, Oporto MR, Totino SF, La Manna A (1986) Normal growth of nephrotic children during long-term alternate-day prednisone therapy. Acta Paediatr Scand 75:245–250
Sadeghi-Nejad A, Senior B (1969) Adrenal function, growth, and insulin in patients treated with corticoids on alternate days. Pediatrics 43:277–283
Saha MT, Laippala P, Lenko HL (1998) Normal growth of prepubertal nephrotic children during long-term treatment with repeated courses of prednisone. Acta Paediatr 87:545–548
Centers for Disease Control and Prevention, CDC growth charts. Available at www.cdc.gov/growthcharts. Accessed June 9, 2009
Must A, Dallal GE, Dietz WH (1991) Reference data for obesity: 85th and 95th percentiles of body mass index (Wt/Ht2) and triceps skinfold thickness. Am J Clin Nutr 53:839–846
Tanner JM (1986) The use and abuse of growth standards. In: Falkner F, Tanner JM (eds) Human growth, 2nd edn. Plenum, New York, pp 95–112
Rosner B (1995) Fundamentals of biostatistics, 4th edn. Duxbury, New York
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31–41
International Study of Kidney Disease in Children (ISKDC) (1981) The primary nephrotic syndrome in children: identification of patients with minimal change nephrotic syndrome from initial response to prednisone. J Pediatr 98:561–564
International Study of Kidney Disease in Children (ISKDC) (1978) Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics time of diagnosis. Kidney Int 13:159–165
Ruth EM, Kemper MJ, Leumann EP, Laube GF, Thomas J, Neuhaus TJ (2005) Children with steroid-sensitive nephrotic syndrome come of age: long-term outcome. J Pediatr 147:202–207
Martinelli CE Jr, Moreira AC (1994) Relation between growth hormone and cortisol spontaneous secretion in children. Clin Endocrinol (Oxf) 41:117–121
Senaris RM, Lago F, Coya R, Pineda J, Dieguez C (1996) Regulation of hypothalamic somatostatin, growth hormone-releasing hormone, and growth hormone receptor messenger ribonucleic acid by glucocorticoids. Endocrinology 137:5236–5241
Malerba M, Bossoni S, Radaeli A, Mori E, Bonadonna S, Giustina A, Tantucci C (2005) Growth hormone response to growth hormone-releasing hormone is reduced in adult asthmatic patients receiving long-term inhaled corticosteroid treatment. Chest 127:515–521
Iwasaki Y, Morishita M, Asai M, Onishi A, Yoshida M, Oiso Y, Inoue K (2004) Effects of hormones targeting nuclear receptors on transcriptional regulation of the growth hormone gene in the MtT/S rat somatotrope cell line. Neuroendocrinology 79:229–236
Gafni RI, Weise M, Robrecht DT, Meyers JL, Barnes KM, De-Levi S, Baron J (2001) Catch-up growth is associated with delayed senescence of the growth plate in rabbits. Pediatr Res 50:618–623
Elders M, Wingfield BS, McNatt ML, Clarke JS, Hughes ER (1975) Glucocorticoid therapy in children. Am J Dis Child 129:1393–1396
Baron J, Klein KO, Colli MJ, Yanovski JA, Novosad JA, Bacher JD, Cutler GB Jr (1994) Catch-up growth after glucocorticoid excess: a mechanism intrinsic to the growth plate. Endocrinology 135:1367–1371
Gafni RI, Baron J (2000) Catch-up growth: possible mechanisms. Pediatr Nephrol 14:616–619
Tanner JM (1994) Auxology. In: Kappy MS, Blizzard RM, Migeon CJ (eds) The diagnosis and treatment of endocrine disorders. Charles C. Thomas, Springfield, pp 137–192
Rees L, Greene SA, Adlard P, Jones J, Haycock GB, Rigden SPA, Preece M, Chantler C (1988) Growth and endocrine function in steroid sensitive nephrotic syndrome. Arch Dis Child 63:484–490
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donatti, T.L., Koch, V.H. Final height of adults with childhood-onset steroid-responsive idiopathic nephrotic syndrome. Pediatr Nephrol 24, 2401–2408 (2009). https://doi.org/10.1007/s00467-009-1301-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-009-1301-z