Abstract
Preterm birth is associated with decreased nephron mass and obesity that may impact on kidney disease progression in later life. Our objectives were to examine the relative risks of obesity and preterm birth on the progression of kidney disease in children. In a retrospective cohort study, 80 (44 obese and 36 non-obese) patients with proteinuric kidney disease were studied for disease progression and glomerular histomorphometry. Of the obese, 22 had been born at term (Obese-T) and 22 had been preterm (Obese-PT). Seventeen non-obese children with focal glomerular sclerosis, born at term (NO-FSGS), and 19 non-obese preterm (NO-PT) children, served as controls. Insulin resistance as measured by the homeostatic model assessment (HOMA-IR) was elevated in all obese children. Obese-PT patients had increased risk of renal demise during childhood when compared with Obese-T children [hazard ratio 2.4; 95% Confidence interval (95% CI) 1.1 to 7.1; P = 0.04]. In obese children, although proteinuria often exceeded nephrotic range, average levels of serum albumin remained normal. Preterm patients were more likely to have reduced renal mass (odds ratio 4.7; P = 0.006), but obesity was not a factor. Renal histomorphometry showed glomerulomegaly in obese patients, regardless of birth weight. Obesity and preterm birth appear to impose additive risks for progression of kidney disease in childhood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Concomitant with the global obesity epidemic [1], there are a number of reports of obesity-related glomerulopathy (ORG) associated with progression of kidney diseases in adults and adolescents [2–5]. Some of these reports note a decrease in nephron mass by acquired unilateral nephrectomy or established renal disease [2, 4, 6–10]. ORG in adults has been defined as the clinical syndrome of morbid obesity, marked proteinuria without edema and normal serum albumin [3]. Histomorphometry describes glomerulomegaly which is thought to reflect glomerular hyperfiltration [8–10].
In the context of pediatric kidney disease, reduced nephron mass and increased risk for end-stage kidney disease (ESKD) has been associated with individuals born small for gestational age (SGA) as well as those born preterm and appropriate for gestational age (AGA) [11–13]. Epidemiologic studies indicate that low birth weight in conjunction with rapid post-natal growth imposes an increased risk for hypertension, insulin resistance and type 2 diabetes in later life [13, 14]. Some ethnic populations, such as the Aborigines [15], American Indians [16], and African Americans of the southeast United States of America [17], develop proteinuric kidney disease associated with hypertension and glomerulomegaly, presumably related to reduced nephron mass [18]. Our previous clinical observations suggest that early excessive weight gain contributes to progression of kidney disease in patients who have suffered neonatal acute kidney injury (AKI) [19]. It remains unclear whether these manifestations are the results of “developmental programming” induced by adverse environmental events in utero or during the vulnerable periods in early post-natal life [20]. The population of surviving low birth weight individuals born preterm are the focus of much research, since they offer some insight into this phenomenon as regards glucose sensitivity [21, 22], low nephron mass [12, 13] and cardiovascular disease risk [23, 24]. This problem has become increasingly more evident in the multi-ethnic community of South Florida, with a growing population of children with obesity-related non-diabetic kidney disease. We have had an opportunity to examine a cohort of pediatric patients with chronic kidney disease (CKD) born preterm and have compared them with those born of normal birth weight with and without obesity according to renal disease progression and histomorphometry. To our knowledge, this report is the first to describe clinico-pathologic correlations of this kind in children.
Patients and methods
Patient selection and examination
A retrospective analysis was performed on the data of a population of children aged between 1 year and 21 years who were included in a database maintained in the Division of Pediatric Nephrology, University of Miami, Holtz Children’s Hospital, between January 1996 and June 2008. An initial cohort was composed of 285 children with data collected in an investigation to profile proteinuria in a pediatric population [25]. A second cohort consisted of 27 infants who had been referred for neonatal AKI and were followed in the renal clinic for chronic kidney injury. The study was approved by the institutional review board, and all subjects were assured of anonymity in compliance with the Health Insurance Portability and Accountability Act (HIPAA).
In all, 80 children with non-diabetic kidney disease and proteinuria were identified for inclusion in this study. Patients were excluded if they had orthostatic proteinuria or any underlying systemic disease, such as diabetes, systemic lupus erythematosus, human immunodeficiency virus infection, sickle cell disease or membranous nephropathy identified by serology or kidney biopsy. They were also excluded if they had been treated with corticosteroids for the nephrotic syndrome and had shown clinical response to therapy by a significant decrease in proteinuria. The cohort was divided according to gestational age at birth, with preterm (PT) ≤32 weeks’ gestation and term (T) ≥36 weeks’ gestation. Size for gestational age was designated as appropriate if birth weight exceeded the 5th percentile for length of gestation [26].
Of the obese children, 22 had been born at term (Obese-T) and 22 had been born preterm (Obese-PT). A non-obese cohort of 17 patients born at term with steroid-resistant nephrotic syndrome and focal glomerular sclerosis by renal biopsy (NO-FSGS) was selected to serve as a reference group for disease progression and histomorphometry. Similarly, 19 non-obese patients born preterm (NO-PT) who had been followed longitudinally after recovery from neonatal AKI served as controls to the Obese-PT group.
Body mass index [BMI = weight (in kilograms)/height2 (meters squared)] was recorded at each encounter as percentile values for age and standard deviation scores (SDSs) from the reference population [26]. Obesity was considered to be ≥95th percentile for gender and height and/or a z-score ≥1.65 SDS [1, 26, 27].
Casual sitting systolic and diastolic blood pressures were measured by the Dinamap® oscillometric technique at each clinic visit. Reference values were taken from the Fourth Report of the Working Group on Pediatric Hypertension [28].
Socio-economic assessment
An estimate of socio-economic status (SES) was obtained by the percent of individuals living below the poverty level in the postal ZIP code area of each patient’s address as defined by the 2000 United States Census [29]. With the national average of 12.4% for individuals living below poverty level, a ZIP code with >20% was considered a high poverty environment for the purposes of this study.
Renal function and proteinuria
Twenty-four hour and/or random urine samples for protein/creatinine (Upr/cr) and microalbumin/creatinine (Ualb/cr) ratios, levels of serum creatinine and serum albumin, and blood pressures were recorded at the time of first encounter. A Upr/cr <0.2 and Ualb/cr <0.03 were considered to be normal. A Upr/cr > 2.0 and Ualb/cr>1.0 were considered to be within the nephrotic range. Estimated glomerular filtration rate (eGFR) in milliliters per minute per 1.73 m2 body surface area was calculated by the Schwartz height index formula [30]. For the purpose of calculating renal survival, we set renal death at stage 5 chronic kidney disease (CKD) when eGFR ≤ 15 ml/min per 1.73 m2. Urine and serum were assayed in the central hospital clinical laboratory on a multi-channel analyzer or by Quest® referral laboratories.
Estimation of renal mass
Renal mass and function were assessed by renal ultrasound and scintigraphy. Renal mass was estimated from the average renal length recorded by real-time sonography using a mechanical sector scanner with a 3.5–7.5 MHz transducer positioned to image the kidney in its longest dimension. Renal lengths were measured with digital calipers on a freeze-frame image. The average renal length was compared with published population standards according to age at the time of the study to within the nearest 6 months, and the z-score was calculated [31, 32].
Insulin resistance and the metabolic syndrome
In obese patients, the degree of insulin resistance was determined by the homeostatic model assessment (HOMA-IR), calculated as (fasting concentration of glucose in millimoles per liter) × fasting concentration of insulin in milliunits per liter divided by 22.5 [33]. Serum lipids were measured from blood drawn under fasting conditions and included total cholesterol, triglycerides, high density lipoprotein (HDL) and calculated low density lipoprotein (LDL).
The children in our study were classified as having the metabolic syndrome if they met three or more of the following criteria for age and gender: a BMI >95th percentile (z-score ≥1.65), a fasting concentration of glucose ≥100 mg/dl, a total concentration of cholesterol ≥130 mg/dl, a triglyceride level ≥150 mg/dl, an HDL level ≤50 mg/dl, systolic or diastolic blood pressure (BP) ≥ 95th percentile [28].
Renal biopsy and histomorphometry
Renal tissue for morphologic diagnosis was available from 23 obese patients (nine Obese-PT; 14 Obese-T) and all 17 NO-FSGS patients by light microscopy. Histomorphometry was performed by random selection from 17 (six Obese-PT; four Obese-T; seven NO-FSGS) available specimens. Computer-assisted morphometry was performed with an Olympus BH-2® microscope and MetaMorph® imaging system from Universal Imaging Corporation (https://doi.org/www.universal-imaging.com). Microscopic sections were stained with hematoxylin and eosin, periodic acid–Schiff (PAS), Jones’ methenamine silver, and trichrome stains. The PAS-stained slides were used for computer-assisted morphometry. We determined the average dimensions of glomerular area (GA), expressed as micrometers squared × 103 of mesangial tuft area, by photographing with the ×40 lens. Glomerular volume (GV) (micrometers cubed × 106) was calculated from the glomerular area according to the formula of Weibel and Gomez as follows: GV = GA1.5 × β/κ, where β is the shape coefficient of 1.38 and κ is 1.01, the size distribution coefficient of 10% for the variation in glomerular size for a single biopsy specimen [34, 35]. To control for observer bias, the pathologist was unaware of the patient source of the specimen.
Statistical methods
All data sets were analyzed for Gaussian distribution with the D’Agostino–Pearson omnibus test for normality. All results were expressed as the mean ± standard deviation (SD). Intergroup comparisons were analyzed by one-way analysis of variance (ANOVA) using the Tukey–Kramer multiple-comparisons test. Differences between two groups were analyzed by Student’s t-test. Actuarial renal survival was analyzed by the Kaplan–Meier method with comparison of curves by log-rank test. Multiple regression analysis of survival curves between groups was analyzed by proportional hazards regression with calculation of hazards ratios (HR) and 95% CI. Univariate correlations were performed with Pearson’s correlation coefficient (r). Proportional differences were tested with Fisher’s exact test. Values of P < 0.05 were considered significant.
Results
Demographics and anthropometrics
Demographic characteristics of the obese and non-obese patients according to birth weight are shown in Table 1. The majority of preterm patients (39/41 = 95%) had been of extremely low birth weight (<1,000 g). Of the Obese-PT, only three (14%) had been SGA. Of the 19 NO-PT patients, one had been SGA. Each patient group had an African American (AA) and Hispanic (H) ethnic predominance, with AAs composing 51% of the entire cohort.
The average percent poverty for each group exceeded the national average of 12.4% and was not significantly different between the groups (Table 1). Those of African American ethnicity had an odds ratio of 4.2 (95% CI 1.6–11.1; P < 0.01) of living in an area of increased poverty when compared with those of Hispanic or white ethnicity. However, no other medical demographic characteristics in this cohort were significantly different, including the presence of obesity, preterm birth or progression to ESKD.
Anthropometric indices by SDSs, including weight, height and BMI, were compared. Obese-T children had significantly greater weight SDSs (2.2 ± 0.7 versus 1.2 ± 1.0), height SDS (0.5 ± 1.3 versus −1.0 ± 2.2) and BMI SDS (3.8 ± 1.8 versus 2.3 ± 1.0) than the Obese-PT children, respectively (P < 0.001). The body habitus for the Obese-PT was disproportionately short and obese, while the anthropometric characteristics of the Obese-T described a more proportionate habitus as tall and heavy.
Radiological and functional evaluation of renal mass
On final renal sonography and scintigraphy, 16/41 (39%) preterm (eight obese and eight non-obese) patients exhibited at least one small and/or hypofunctioning renal unit compared to 5/39 (13%) of term patients (odds ratio 4.7; P < 0.006). Of the preterm patients, all had had normal sized renal units at birth and most had had documented vascular thrombosis in the newborn period to explain the discrepancy in size and function in later life. Among the term patients, only the obese patients with kidney disease were found to have unilateral renal hypoplasia (four) and agenesis (one).
Average renal length was recorded at 7 ± 4 years in the preterm patients and 11 ± 5 years of age in the term patients. When the z-score for the average length of both kidneys was calculated, the NO-PT patients had significantly less renal tissue than those patients born at term (Table 1). In the entire cohort, renal length SDS correlated significantly to patient height SDS (r = 0.4; P < 0.01), consistent with the reference population [32].
Clinical course and progression of kidney disease
Average longitudinal follow-up for the entire cohort was 7.4 ± 4 years. The group followed the longest was the NO-PT at 10 ± 4 years, since they had been identified at birth. The shortest follow-up was in the Obese-T group at 5 ± 4 years. Of the Obese-T patients, 5/9 (56%) presented with ESKD without prior diagnosis. The remainder presented with asymptomatic proteinuria and hypertension. As in the Obese-T patients, the Obese-PT patients tended to present with fewer symptoms and an inordinate decrease in eGFR.
Twenty-six preterm infants (seven Obese-PT and 19 NO-PT) were followed since birth and had neonatal AKI documented by peak levels of serum creatinine averaging 2.9 ± 1.0 mg/dl (range 1.5-5.3 mg/dl), which had decreased to an average of 0.6 ± 0.4 mg/dl (range 0.3-1.9 mg/dl) by 6 months of age. The differences between the obese and non-obese preterm were not significant (P = 0.07).
Absolute total proteinuria and albuminuria was greater in the NO-FSGS patients with steroid-resistant nephrotic syndrome (Table 1). Despite heavy proteinuria, the obese groups maintained normal levels of serum albumin and manifested no edema, while the NO-FSGS had significantly lower serum albumin levels and symptomatic edema. There was a significant negative correlation between total proteinuria and eGFR (r = −0.5; P < 0.001) in the obese patients. Increasing albuminuria also correlated with loss in kidney function, although the relationship was less significant (r = −0.4; P < 0.05).
Treatment with angiotensin-converting enzyme inhibitors (ACEIs) and/or angiotensin receptor blockers (ARBs) was prevalent in the NO-FSGS control group 13/17 (76%) and the Obese-T group (6/22 = 27%) but rare in the preterm patients (Obese-PT 3/22 = 14%; NO-PT 2/19 = 11%). No effect of these therapies was apparent in the renal outcome of any group.
Insulin resistance and the metabolic syndrome
Insulin resistance and components of the metabolic syndrome are shown in Table 2.
Average age at the time of examination for insulin resistance and the metabolic syndrome for the obese patients was 11.9 ± 4.9 years. Overall, 38/44 (86%) of the obese children met criteria for the metabolic syndrome, with an average score of 4 ± 1. In the Obese-PT group 20/22 (91%) met three or more criteria for the metabolic syndrome compared with 18/22 (82%) of the Obese-T (P = 1.0). Obese patients had similar measures of insulin resistance as measured by HOMA-IR (Table 2). Dyslipidemia was prominent in obese children and was characterized by increased levels of total cholesterol and serum triglycerides as well as low HDL.
Renal survival relative to birth weight
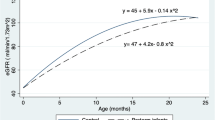
Figure 1 demonstrates the actuarial renal survival curves for the four groups of patients with a significant difference by log rank test (P = 0.02). The median renal survival was 23 years in the Obese-T, 16 years in the NO-FSGS, and 15 years for the Obese-PT. None of the NO-PT patients showed progression to ESKD, although 6/19 (32%) had CKD with decreased eGFR <90 ml/min per 1.73 m2. Obese-PT patients showed increased risk of renal death during childhood compared with Obese-T (HR = 2.4; 95% CI = 1.1 to 7.1; P = 0.04) and NO-PT (P < 0.005) patients. There was also a trend for improved survival in the Obese-T compared with the NO-FSGS patients (HR = 0.4; 95% CI = 0.1 to 1.0; P = 0.06).
Kaplan–Meier actuarial renal survival curves in four groups of children with kidney disease. Obese-PT patients had increased risk of renal demise during childhood compared with Obese-T (hazard ratio 2.4; 95% CI 1.1 to 7.1 P = 0.04) with median renal survival of 15 years of age for Obese-PT compared with 23 years for Obese-T patients
Renal pathology and histomorphometry
All Obese-PT who had renal pathologic diagnoses (9/22) showed findings consistent with FSGS. Of the 14 Obese-T patients who underwent renal biopsies, 12 showed FSGS and two showed mesangial proliferation.
Histomorphometry was performed on ten obese (six O-PT; four Obese-T) and seven NO-FSGS renal tissue specimens. An average of 9.6 ± 8 glomeruli were measured from each biopsy specimen. An average of 86 ± 56 (range 56–106) glomeruli from each group were measured for glomerular tuft area. Glomerulomegaly as measured by glomerular volume was similar in the obese children, regardless of birth weight (Obese-PT 38.3 ± 12.6 µm3 × 106 versus Obese-T 42.0 ± 7.0 µm3 × 106), but was significantly greater than that of the NO-FSGS patients (22.6 ± 7.0 µm3 × 106; P < 0.01) (Fig. 2a).
a Graphic comparison of average glomerular volume (µm3 × 106) by histomorphometry in Obese-PT, Obese-T and NO-FSGS patients. Average glomerular volume was similar in obese patients (Obese-T and Obese-PT), regardless of birth weight, but was significantly less in non-obese patients (NO-FSGS); *P = 0.008 by ANOVA. b Composite photomicrograph. A Obese patient born preterm of low birth weight presenting with proteinuria. The glomerulus is larger than that of the non-obese control, and there is extensive peri-glomerular and interstitial fibrosis. B Obese patient of normal birth weight presenting with heavy proteinuria. The glomerulus is larger than that of the control. C Age-matched non-obese control with FSGS. Observe a normal-sized glomerulus. Hematoxylin and eosin, ×200. Internal scales 100 μm
Figure 2b shows the pathologic comparison on renal biopsy of glomeruli from a non-obese patient with FSGS compared with those from obese patients of normal and low birth weight. This composite provides the histologic picture demonstrating the morphometric measurements.
Discussion
This study brought insight into a growing population of children with obesity-related kidney disease, especially in those born preterm. The lesion of glomerulomegaly, focal and global sclerosis and a more insidious progression to renal failure compared with that in non-obese patients with FSGS has characterized ORG in adults [2–4]. In our cohort of obese children, the pathologic finding of FSGS was the predominant lesion in both groups of obese children, regardless of birth weight. The clinical course in the obese children born at term was typical of the ORG described in adults and adolescents [4, 5] with a protracted course in comparison with that in patients with typical FSGS [3]. In distinction, the condition of obese preterm children deteriorated more rapidly, although their presentation was also characterized by lack of edema and normal serum levels of proteins. A recent report of six adult patients born preterm who developed secondary FSGS provided observations similar to our own, with the caveat that obesity seemed to accelerate the pathogenesis in children [36].
The greatest limitation in this retrospective observational study was the identification of a suitable control group to compare with the preterm obese patients. The longitudinal database at our institution of preterm infants with evidence of chronic kidney injury allowed such a comparison. The demographic characteristics of our cohort were also important, in that ethnic differences might impose an important bias. Despite a 57% Hispanic ethnic predominance in South Florida, African American children composed the majority of our cohort and were more likely to be living in poverty. These disparate characteristics may account for the seemingly large number of patients with obesity, preterm birth and renal disease at this urban medical center.
Previous studies have demonstrated increased blood pressure, salt sensitivity, reduced renal mass, and microalbuminuria in adults born preterm, whether small or appropriate for gestational age [37–39]. Our data support these findings in our preterm patients with kidney disease. Not surprisingly, all the preterm patients showed evidence of significantly smaller renal mass than a reference population and the term patients. Although hypertension and loss of renal mass were common in the non-obese preterm patients, renal function was well preserved and proteinuria was minimal.
Proteinuria as a consequence and perpetrator of renal injury is evident in this and other studies of CKD [2, 5, 15, 19, 25]. The relationship of increasing proteinuria with loss in eGFR was shown in our observations and confirms that of numerous other reports in adults and children [2, 15–17, 19, 25]. An interesting observation, that many of the obese patients had normal levels of serum albumin in the face of heavy proteinuria, may be related to the character of their proteinuria. We have shown previously that the albumin component of proteinuria may be less in children, especially in those of younger age with primarily tubular disease [19]. The mechanisms by which obesity imposes systemic and local cytochemical reactions may also result in a predominance of non-albumin proteinuria which would maintain normal serum proteins until the terminal phases of the disease [23].
In the cohort described here, glomerulomegaly was present and similar in the obese patients, regardless of birth weight, when compared with the non-obese FSGS controls. Glomerulomegaly as a component of obesity-related renal disease has been described in a large number of adults [3]. Total kidney specimens are necessary for the measurement of glomerular number, but histomorphometry by biopsy sampling can give important data regarding glomerulomegaly and suspected glomerular hypertension [3, 7–10, 32]. Some reports indicate that obesity or increased BMI alone may be an independent initiator of glomerular hypertension by various systemic and local mechanisms included in the cascade towards focal glomerulosclerosis [6–10, 23]. Of interest is that there was no apparent difference in glomerulomegaly according to birth weight, suggesting that obesity was the primary offender. This association requires further investigation.
We have previously observed in preterm infants that overweight at 3 years of age resulted in a more rapid progression to renal demise [19]. Preterm birth, regardless of size for gestational age, appears to be a cause of low nephron endowment, since active nephrogenesis is ongoing in utero until 36 weeks’ gestation. After preterm birth, glomerulogenesis ceases within approximately 40 days, and fewer glomeruli are produced in proportion to the length of gestation [12]. Reduced renal mass, whether by acquired renal disease, nephrectomy, ischemic injury, or congenital oligonephronia, may be a major vulnerability factor in progression of kidney disease [2, 6, 7]. Our data indicate that, in obese children born preterm, kidney disease was two-times more likely to advance to ESKD than in obese patients born at term and five-times more likely to progress than in non-obese preterm children. This finding supports the need for prospective cohort studies in this population in an effort to decipher the relative role of ischemic nephropathy versus preterm birth on nephron endowment.
The metabolic syndrome is recognized as a syndrome complex of insulin resistance and dyslipidemia, aggravated by central obesity [23, 24, 33]. It is increasingly described in association with the genetic predisposition to type 2 diabetes and is believed to have its origins in “developmental programming” or the fetal origins of adult disease [14, 22]. All our obese pediatric patients had similar markers of the metabolic syndrome, including significant insulin resistance, compared with a general pediatric population without renal disease [24]. Preterm birth and rapid weight gain during the first years of life are associated with early insulin resistance and hypertension in childhood and adolescence, regardless of size for gestational age [13, 20–22, 37–39].
In summary, obesity is an important modifiable risk factor in the development and progression of renal disease in children, especially those born preterm, whether appropriate or small for gestational age. Individuals of extreme prematurity will have proportionately less nephron mass and, with their improved survival, may emerge as an important population at risk for renal disease progression. If they have genetic predisposition to renal disease, their risk becomes more significant. It is particularly important that we study infants and children in an attempt to recognize those critical windows during early life in which programming of adult diseases occurs. Ultimately, these may become the potential windows for therapeutic interventions aimed to prevent late onset of disease.
References
Hedley A, Ogden CL, Johnson CL, Carrol MD, Curtin LR, Flegal KM (2004) Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA 291:2847–2850
Praga M, Hernández E, Herrero JC, Morales E, Revilla Y, Diax-Gonzalez R, Rodicio JL (2000) Influence of obesity on the appearance of proteinuria and renal insufficiency after unilateral nephrectomy. Kidney Int 58:2111–2118
Kambham N, Markowitz GS, Valeri AM, Lin J, D’Agati VD (2001) Obesity-related glomerulopathy: an emerging epidemic. Kidney Int 59:1498–1509
Praga M, Hernandez E, Morales E, Campos AP, Valero MA, Martinez MA, Leon M (2001) Clinical features and longterm outcome of obesity-associated focal glomerulosclerosis. Nephrol Dial Transplant 16:1790–1798
Adelman RD, Restaino JG, Alon US, Blowley DL (2001) Proteinuria and focal segmental glomerulosclerosis in severely obese adolescents. J Pediatr 138:482–485
Bonnet F, Deprele C, Sassolas A, Moulin P, Alamartine E, Berthezene F, Berthoux F (2001) Excessive body weight as a new independent risk factor for clinical and pathological progression in IgA nephritis. Am J Kidney Dis 37:720–727
González E, Gutiérrez E, Morales E, Hernandez E, Andres A, Bello I, Diaz-Gonzalez R, Leiva O, Praga M (2005) Factors influencing the progression of renal damage in patients with unilateral renal agenesis and remnant kidney. Kidney Int 168:263–270
Ahmed MH, Khalil AA (2007) Obesity-related glomerulopathy: another nail in the coffin of the epidemic of end-stage renal disease. J Clin Pathol 60:582
Rea DJ, Heimbach JK, Grande JP, Textor SC, Taler SJ, Prieto M, Larson TS, Cosio FG, Stegall MD (2006) Glomerular volume and renal histology in obese and non-obese living kidney donors. Kidney Int 70:1636–1641
Tomaszewski M, Charchar FJ, Maric C, McClure C, Crawford L, Grzeszczak W, Sattar N, Zulowska-Szczechowska E, Dominiczak AF, Luyckx VA (2007) Glomerular hyperfiltration: a marker of metabolic risk. Kidney Int 71:816–821
Mañalich R, Reyes L, Herrera M, Melendi C, Fundora I (2000) Relationship between weight at birth and number and size of renal glomeruli in humans: a histomorphometric study. Kidney Int 58:770–773
Rodriguez MM, Gomez AH, Abitbol CL, Chandar JJ, Duara S, Zilleruelo GE (2004) Histomorphometric analysis of postnatal glomerulogenesis in extremely preterm infants. Pediatr Dev Pathol 7:17–25
Vikse BE, Irgens LM, Leivestad T, Hallan S, Iversen BM (2008) Low birth weight increases risk for end stage renal disease. J Am Soc Nephrol 19:151–157
Hershkovitz D, Burbea Z, Skorecki K, Brenner BM (2007) Fetal programming of adult kidney disease: cellular and molecular mechanisms. Clin J Am Soc Nephrol 2:334–342
Singh GR, Hoy WE (2004) Kidney volume, blood pressure and albuminuria: findings in an Australian Aboriginal community. Am J Kidney Dis 43:254–259
Narva AS (2003) The spectrum of kidney disease in American Indians. Kidney Int 83 [Suppl]:53–57
Lackland DT, Bendal HE, Osmond C, Egan BM, Barker DJP (2000) Low birth weight contributes to the high rates of early onset chronic renal failure on the southeast United States. Arch Intern Med 160:1472–1476
Hughson M, Farris AB 3rd, Douglas-Denton R, Hoy WE, Bertram JF (2003) Glomerular number and size in autopsy kidneys: the relationship to birth weight. Kidney Int 63:2113–2122
Abitbol CL, Bauer CR, Montané B, Chandar J, Duara S, Zilleruelo G (2003) Long-term follow-up of extremely low birth weight infants with neonatal renal failure. Pediatr Nephrol 18:887–893
Regan FM, Cutfield WS, Jefferies C, Robinson E, Hofman PL (2006) The impact of early nutrition in premature infants on later childhood insulin sensitivity and growth. Pediatrics 118:1943–1949
Hovi P, Andersson S, Eriksson JG, Järvenpää AL, Strang-Karlsson S, Mäkitie O, Kajantie E (2007) Glucose regulation in young adults with very low birth weight. N Engl J Med 356:2053–2063
Jimenez-Chillaron JC, Patti ME (2007) To catch up or not to catch up: is this the question? Lessons from animal models. Curr Opin Endocrinol Diabetes Obes 14:23–29
Wahba IM, Mak RH (2007) Obesity and obesity-initiated metabolic syndrome: mechanistic links to chronic kidney disease. Clin J Am Soc Nephrol 2:550–562
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J, Sherwin RS, Caprio S (2004) Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 350:2362–2374
Abitbol CL, Chandar J, Onder AM, Nwobi O, Montane B, Zilleruelo G (2006) Profiling proteinuria in pediatric patients. Pediatr Nephrol 21:995–1002
Frisancho AR (1993) Anthropometric standards for the assessment of growth and nutritional status. University of Michigan Press, Ann Arbor, pp 31–36
Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Grummer-Strawn LM, Curtin LR, Roche AF, Johnson CL (2002) Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics 109:45–60
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics 114:555–576
US Census Bureau: American Fact Finder. https://doi.org/factfinder.census.gov. Accessed 22 November 2008
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Rosenbaum DM, Korngold E, Teele RL (1983) Sonographic assessment of renal length in normal children. AJR Am J Roentgenol 142:467–469
Dinkel E, Ertel M, Dittrich M, Peters H, Berres M, Schulte-Wissermann H (1985) Kidney size in childhood: sonographic growth charts for kidney length and volume. Pediatr Radiol 15:38–43
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Chen HM, Liu ZH, Zeng CH, Li SJ, Wang QW, Li LS (2006) Podocyte lesions in patients with obesity-related glomerulopathy. Am J Kidney Dis 48:772–779
Hoy WE, Samuel T, Hughson MD, Nicol JL, Bertram JF (2006) How many glomerular profiles must be measured to obtain reliable estimates of mean glomerular areas in human renal biopsies? J Am Soc Nephrol 17:556–563
Hodgin JB, Rasoulpour M, Markowitz GS, D’Agati VD (2009) Very low birth weight is a risk factor for secondary focal segmental glomerulosclerosis. Clin J Am Soc Nephrol 4:71-76
Simonetti GD, Raio L, Surbek D, Nelle M, Frey FJ, Mohaupt MG (2008) Salt sensitivity of children with low birth weight. Hypertension 52:625–630
Irving RJ, Belton NR, Elton RA, Walker BR (2000) Adult cardiovascular risk factors in premature babies. Lancet 355:2135–2136
Keijzer-Veen MG, Schrevel M, Finken MJ, Dekker FW, Nauta J, Hille ET, Frolich M, van der Heijden BJ (2005) Microalbuminuria and lower glomerular filtration rate at young adult age in subjects born very premature and after intrauterine growth retardation. J Am Soc Nephrol 16:2762–2768
Acknowledgments
This study was supported in part by a grant from Florida’s Department of Health, Children’s Medical Services.
The authors have no conflict of interests referable to the content of the manuscript or financial interest in any of the products or procedures mentioned.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abitbol, C.L., Chandar, J., Rodríguez, M.M. et al. Obesity and preterm birth: additive risks in the progression of kidney disease in children. Pediatr Nephrol 24, 1363–1370 (2009). https://doi.org/10.1007/s00467-009-1120-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-009-1120-2